Complicated Grief: Risk Factors, Interventions, and Resources for Oncology Nurses
Background: When a loved one dies of cancer, complicated grief (CG) may occur because of the trauma associated with family caregivers’ perceptions of their loved one’s suffering, either from advanced cancer or from side effects of cancer treatment.
Objectives: This article provides an overview of CG and existing interventions for family caregivers who may be at risk for CG following the loss of a loved one and the implications for oncology nurses who provide emotional support and guidance.
Methods: Current evidence related to the treatment of CG and information to assist with identification of individuals at risk for CG are presented, as well as resources for oncology nurses who encounter individuals who are at high risk for, or who are experiencing, CG.
Findings: Although therapy interventions for CG have been shown to be effective forms of treatment, these therapies are not widely available and often require an extended treatment period to yield results. Oncology nurses can provide early interventions, such as referrals to supportive care services and mental health professionals to facilitate effective treatment.
Jump to a section
Grief is part of the human experience and a normal reaction to the death of a loved one. Although the pain of loss may never completely subside, most individuals adjust to life without the deceased and develop a new sense of normalcy over time. For others, the grief process becomes prolonged. Individuals who have difficulty accepting the death and assimilating into life without the deceased experience what is known as complicated grief (CG), or prolonged grief disorder (Shear, 2010).
CG may occur in as many as 40% of family caregivers who lose a close family member to cancer (Guldin, Vedsted, Zachariae, Olesen, & Jensen, 2012). For some, symptoms of CG can occur before the patient dies when family members are struggling to accept the cancer diagnosis and impending death (Tomarken et al., 2008). CG disproportionately affects older adults, with more than 25% of older adults experiencing CG, compared to only 5%–7% of the general population (Newson, Boelen, Hek, Hofman, & Tiemeier, 2011; Shear, 2010). CG is associated with numerous psychological problems, including loneliness, social isolation, anxiety, clinical depression, cognitive impairment, and post-traumatic stress disorder (PTSD) (Ghesquiere, Shear, & Duan, 2013; Shear, Ghesquiere, & Glickman, 2013). Compounded losses of multiple close family members and friends, increased likelihood that the deceased will be a spouse or partner, and financial burdens associated with the loss may lead to a higher incidence of CG among older adults (Ghesquiere et al., 2013; Newson et al., 2011).
Oncology nurses often form close relationships with patients and their family caregivers, both of whom depend on them for guidance and emotional support during cancer treatment (Guldin et al., 2012). Therefore, oncology nurses are positioned to direct family caregivers to appropriate grief services, as well as to deliver continued emotional support and guidance. This article provides information to assist with identifying individuals at risk for CG, discusses current evidence related to treatment for CG, and provides resources for oncology nurses who encounter individuals who are at high risk for, or who are experiencing, CG.
Risk Factors
Although anyone can experience CG, certain risk factors may elevate the likelihood of CG occurring. Manifestations of CG include (a) intense longing; (b) loneliness, emptiness, or lack of meaning in life; (c) recurring thoughts of wanting to join the deceased; and (d) intrusive thoughts about the deceased that interfere with functioning (Shear et al., 2011). Individual signs and symptoms of CG also may include feelings of guilt over the death; constantly replaying the circumstances of the death in their mind; imagining that they could have somehow prevented the death if they had done something differently; and feeling numb, shocked, or in disbelief over the death. The nature of the relationship to the deceased, personality traits, coping style, psychiatric history and comorbidities, and socioeconomic factors all contribute to the risk of CG.
Relational Factors
The closer the relationship to the deceased, the more likely it is that the individual will experience CG. Spouses and parents are particularly vulnerable to symptoms of CG. Spouses may be highly inter-dependent on each other and share a close relationship and a lifetime commitment. Widowed parents with young children may face additional stressors that can lead to depression and increased psychological distress (Yopp, Park, Edwards, Deal, & Rosenstein, 2015). Because parents normally do not expect a child to precede them in death, feelings of guilt and existential suffering may ensue. Older adults may experience multiple losses in a short period of time that compound grief and delay recovery (Newson et al., 2011).
Personality Traits and Coping Style
Personality plays a key role in how an individual grieves, internalizes the grief, and integrates understanding and meaning about the loss of a loved one (Piper, Ogrodniczuk, Joyce, & Weideman, 2011). An individual’s psychological adjustment process, combined with attachment style and coping capability, can help determine whether he or she is at a higher or lower risk of experiencing symptoms of CG (Piper et al., 2011). Although more well-adjusted individuals would be expected to cope better with grief and loss, the literature does not clearly support this relationship (Mancini, Sinan, & Bonanno, 2015; Piper et al., 2011). Personality traits identified as correlates for poorer coping strategies and prolonged emotional distress include anxiety, insecurity, lower levels of self-esteem, and higher levels of negative cognition (Boelen, van den Bout, & van den Hout, 2006; Piper et al., 2011).
Despite inconclusive research regarding a causal relationship between personality and severity of grief, personality does factor into the level of distress some individuals experience when dealing with grief and the length of time required for the grief symptoms to resolve (Piper et al., 2011). The literature presents a compelling argument that an individual’s level of worry and anxiety, along with his or her attachment style, plays a role in the ability to effectively adapt after a loss (Schenck, Eberle, & Rings, 2015). For example, securely attached individuals tend to adapt and resolve their grief more effectively than those with a more anxious attachment style (Piper et al., 2011). Those with higher anxiety-related attachment styles may experience difficulty moving through the grief process, managing emotions, and adjusting after a loss (Piper et al., 2011). Individuals with anxious attachment styles are also prone to prolonged emotional distress and display maladaptive avoidant behavior, causing them to suppress emotions that could result in psychosomatic symptoms (Mancini et al., 2015).
The negative cognitions associated with the previously mentioned attachment styles create beliefs of not being able to live without the deceased individual, feeling worthless without the presence of the deceased person, and feeling like life no longer has meaning (Boelen et al., 2006). These negative cognitions cause bereaved individuals to dwell on their loss rather than to focus on problem- or emotion-specific solutions (Mancini et al., 2015). Negative cognitions play a significant role in prolonging emotional distress and serve as the target for therapeutic interventions to help bereaved individuals dispute and restructure their maladaptive thoughts and beliefs (Boelen et al., 2006; Piper et al., 2011). Behavioral interventions that support the lessening of negative cognitions and avoidant behaviors serve as protective factors in resolving grief and loss (Mancini et al., 2015).
Individuals who experience CG during their bereavement tend to exhibit greater dependency behaviors, focus primarily on negative cognitions about the deceased, are highly emotional, experience a greater degree of loneliness, and hold negative perceptions about the support they will receive if they reach out to others for help (Boelen et al., 2006; Mancini et al., 2015; Piper et al., 2011). Individuals who demonstrate greater levels of resilience during their bereavement hold a more favorable view of the support they can expect from others, rely more on their support systems, openly share their feelings, and worry less about available support when needed (Mancini et al., 2015).
Additional protective factors that lead to more adaptive bereavement include spiritual and religious practices or rituals, prior adaptive psychological well-being, personal and financial control, and no co-occurring losses (Mancini et al., 2015; Piper et al., 2011). These protective factors predict less negative cognition and higher rates of perceived wellness (Boelen et al., 2006). However, bereaved individuals with insecure attachment styles may demonstrate unwillingness or inability to engage with community and social support networks (Piper et al., 2011).
Studies conducted by Mancini et al. (2015) and Schenck et al. (2015) concluded that individuals with insecure attachment styles remained more focused on negative cognitions about the deceased than those with secure attachment styles. Findings also revealed a higher level of CG symptoms among bereaved individuals with insecure attachment styles. Those bereaved individuals who displayed CG symptoms demonstrated greater levels of separation distress (Piper et al., 2011; Schenck et al., 2015). Grief integration is necessary to find meaning in the loss and to find ways of maintaining a sense of closeness with the deceased (Schenck et al., 2015), resulting in adaptive coping that strengthens resilience (Mancini et al., 2015).
Psychiatric Comorbidities and Differentiation
As with many primary mental health disorders, comorbidities are common among individuals suffering from CG. This includes when CG is considered the primary disorder, as well as when CG is secondary to mental health disorders that share symptom overlap. For example, individuals presenting for care with a primary diagnosis of CG exhibit elevated rates of comorbid anxiety disorders, especially PTSD (48% current, 52% lifetime) and panic disorder (14% current, 22% lifetime) (Simon, Shear, et al., 2007). In nontreatment settings, approximately 15% of bereaved individuals also meet the diagnostic criteria for PTSD (O’Connor, 2010). Similarly, individuals with CG present with psychological characteristics often found in individuals with anxiety disorders, such as experiential avoidance (Boelen, van den Bout, & van den Hout, 2010) and intolerance of uncertainty (Boelen, 2010). Considering reverse directionality, high rates of comorbid CG have been documented in individuals with a primary diagnosis of major depressive disorder (Kersting et al., 2009; Sung et al., 2011). Consistent with this temporal relationship, a history of prior trauma or loss and a history of mood and anxiety disorders also predict greater likelihood of developing CG (Lobb et al., 2010).
Although significant symptom overlap exists whether CG is primary or secondary to PTSD, each disorder has its own unique features (O’Connor, 2010; O’Connor, Lasgaard, Shevlin, & Guldin, 2010). Whereas PTSD is characterized typically by fear, horror, anger, guilt, or shame, combined with an anxious hyperarousal and exaggerated reactivity, the experience of CG is marked primarily by yearning, loss, or emptiness (Alexander & Litz, 2014). CG symptoms include an intense longing for the deceased and distress over the loss of the relationship, which is not a central component of PTSD (O’Connor et al., 2010). To further differentiate, when experiencing PTSD after a loss, intrusive thoughts fixate on the death event itself, leading individuals to avoid internal and external reminders of the death event specifically, rather than reminders of the deceased. On the other hand, in CG, individuals may experience intrusive and involuntary thoughts about diverse aspects of the relationship with the deceased, including positive content that the bereaved longs for, and avoidance is mostly limited to stimuli that serve as reminders of the reality or permanence of the loss (Alexander & Litz, 2014). However, the cardinal symptom of emotional numbness since the time of the loss is shared by both CG and PTSD (Alexander & Litz, 2014). Common comorbidities and similar symptom overlap between CG and other mental health disorders add to the challenge of identifying optimal treatments.
Psychotherapeutic Interventions
The normal grief process is a fluid process that most individuals can resolve without the intervention of healthcare professionals (Waller et al., 2016). Oncology nurses should consider referring individuals experiencing normal grief to support groups, grief counseling, and spiritual care services (Ghesquiere et al., 2013), which are offered through hospice and palliative care programs throughout the United States (Centers for Medicare and Medicaid Services, n.d.). When grief is prolonged, and the grief-stricken individual is unable to reconcile the grief and adjust to life without his or her deceased loved one, psychotherapeutic interventions are warranted (Wittouck, Van Autreve, De Jaegere, Portzky, & van Heeringen, 2011).
Support groups and bereavement counseling offer psychosocial support throughout the grief process and educate participants about normal grieving patterns; however, little evidence suggests that psychosocial support is effective in preventing or treating CG (Ghesquiere et al., 2015). Because bereavement programs are widely available and facilitated by mental health professionals, they may be helpful in identifying individuals who require treatment for CG.
Despite an abundance of hospice and palliative care programs offering support groups and counseling for grieving individuals, only a small percentage of people use these services (Steiner, 2006). Online groups offer similar benefits, increased access, and lower associated costs (Lubas & De Leo, 2014) which may encourage usage. However, healthcare providers have expressed concerns about the safety, oversight, and confidentiality of online programs (Lubas & De Leo, 2014; Wells, Mitchell, Finkelhor, & Becker-Blease, 2007).
Early palliative care interventions for family caregivers, delivered by advanced practice nurses via telephone while the patient is in advanced stages of malignancy, may reduce depression and CG, but require further study (Dionne-Odom et al., 2016). A writing intervention, called Finding Balance, allows bereaved caregivers of patients with cancer to reflect, process emotions, and find balance through specific writing activities (Holtslander et al., 2016). These promising new interventions, developed and evaluated by nurse scientists, aim to guide nursing practice in specific interventions to alleviate grief; however, more research is needed to evaluate their effectiveness in CG.
A 2011 meta-analysis of interventions for CG, which pooled data from 14 randomized, controlled trials testing interventions to prevent or treat CG, determined that treatment of CG significantly improved grief-related symptoms, whereas prevention interventions have not demonstrated consistent efficacy (Wittouck et al., 2011). The studies of CG interventions presented in the meta-analysis were published from 1990–2007 and included studies of cognitive behavioral therapy, individual interpersonal therapy, and a combination of the two (see Figure 1). The interventions ranged in length from 12–20 weeks and were conducted by trained mental health counselors and therapists.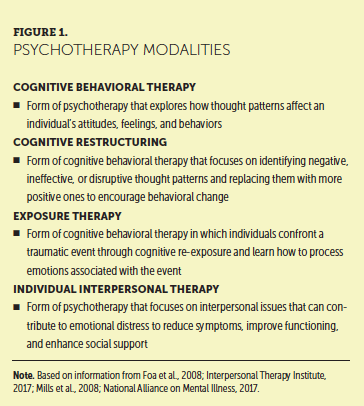
Katherine Shear, MD, a faculty physician in the School of Social Work at Columbia University, has been instrumental in moving the science of grief therapy forward. Shear and her research team developed a 16-session psychotherapeutic intervention for individuals with CG that has demonstrated efficacy in three large randomized, controlled trials involving more than 600 participants (Shear et al., 2014, 2016; Shear, Frank, Houck, & Reynolds, 2005). The Complicated Grief Treatment intervention is a structured psychotherapy program, designed to be implemented by licensed mental health professionals (Shear et al., 2014). Complicated Grief Treatment has also demonstrated efficacy in a group setting, which affords a more economical option and higher access to treatment (Supiano & Luptak, 2014).
Pharmacologic Interventions
Depression and CG frequently co-occur, and preliminary evidence suggests that antidepressants factor into treatment of CG (Bui, Nadal-Vicens, & Simon, 2012; Glickman, Shear, & Wall, 2016; Hensley, Slonimski, Uhlenhuth, & Clayton, 2009; Simon et al., 2008; Simon, Thompson, Pollack, & Shear, 2007; Zisook, Shuchter, Pedrelli, Sable, & Deaciuc, 2001). Pilot studies have demonstrated positive effects of selective serotonin reuptake inhibitors on CG (Hensley et al., 2009; Simon, Thompson, et al., 2007; Zygmont et al., 1998); however, a clinical trial involving 395 people with CG found that providing citalopram (Celexa®) and Complicated Grief Treatment in combination reduced depression-related outcomes, but did not lead to specific improvements in CG when compared to Complicated Grief Treatment plus placebo (Shear et al., 2016).
Implications for Nursing Practice
In practice, except for hospices, family caregivers are not considered targets of oncology nursing care, and healthcare providers and hospitals are not reimbursed for administering care to family caregivers. Therefore, nurses may find providing support to them after the death of the patient to be challenging. Nevertheless, oncology nurses are well positioned to identify family caregivers who are at the greatest risk for CG and should remain alert to the possibility. Oncology nurses should stay abreast of available community resources so that family caregivers experiencing CG, or those at risk for CG, can be referred promptly to support groups, grief counseling, or spiritual support services. Nurses can provide direct support for those struggling with grief by offering condolences, demonstrating concern, and allowing family caregivers to express their feelings. Individuals may be open to discussing feelings and concerns or they may be reluctant. If concerns about the potential for self-harm arise, nurses have an ethical obligation to obtain immediate mental health services for that individual. Figure 2 provides online resources that can help support individuals experiencing CG. Many hospices provide free bereavement services regardless of whether the individual experiencing the loss was involved in that hospice. Often, pastors are trained in managing grief, so referring family caregivers to their local faith community leader may be helpful.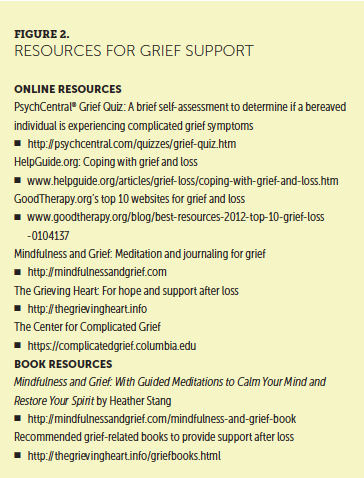
Education
Nursing education has very little focus on the issues of loss and grief for family caregivers and even less focus on CG. Therefore, nursing educators should incorporate assessment and management of CG at all levels of the nursing curriculum and conduct educational research to measure the efficacy of adding CG-related content. Cancer centers and oncology units should offer continuing education focusing on CG to keep practicing nurses up to date on the latest findings from research, as well as to provide education and support to assist nurses who might be experiencing grief themselves.
Research
Although Complicated Grief Treatment has been shown to be an effective treatment for CG symptoms, it is not widely available and typically requires a relatively lengthy treatment period (16 weeks) (Shear et al., 2014). Future studies should focus on efficient ways of delivering treatment for CG and other effective forms of psychotherapy to more individuals. To date, few studies have evaluated psychotherapeutic interventions specifically for CG in loved ones of patients who have died from cancer. The experience of family caregivers and close family or friends during diagnosis and treatment, as well as near the end of life, may influence their response following the loss and have unique effects on the grief process. Targeting psychologic symptoms, like trauma, depression, and loneliness, may be useful for individuals experiencing prolonged or complicated grief. Preliminary evidence suggests that nurse-led interventions may have a role in alleviating CG in caregivers of patients with cancer, but more research is needed to support such interventions (Dionne-Odom et al., 2016; Holtslander et al., 2016). Grief is a culture-bound experience that occurs within an individual’s social-cultural environment. Research studies that inform behavioral health and medical practitioners must include family, social, cultural, and environmental constructs when developing intervention programs (Schenck et al., 2015).
[[{"type":"media","view_mode":"media_original","fid":"32536","field_deltas":{"1":{}},"link_text":null,"fields":{},"attributes":{"height":"212","width":"365","class":"media-image media-element file-media-original","data-delta":"1"}}]]
Conclusion
Oncology nurses often encounter individuals who are suffering with, or who are at risk for, CG. Prompt recognition and referral to supportive services and mental health experts can help facilitate early and effective treatment. Current evidence suggests that psychotherapy and pharmacologic treatments may be helpful in alleviating CG symptoms. Providing effective palliative care, symptom management, and patient and family education during the cancer trajectory may help to prevent CG. Acknowledging the loss, engaging in active listening, and allowing family caregivers to express their feelings and tell their story are important ways that oncology nurses can intervene in CG.
[[{"type":"media","view_mode":"media_original","fid":"32541","field_deltas":{"2":{}},"link_text":null,"fields":{},"attributes":{"height":"281","width":"374","class":"media-image media-element file-media-original","data-delta":"2"}}]]
About the Author(s)
Cindy S. Tofthagen, PhD, ARNP, AOCNP®, FAANP, FAAN, is an associate professor and director of oncology in the College of Nursing and Kevin Kip, PhD, FAHA, is a distinguished professor in the College of Public Health, both at the University of South Florida; Ann Witt, MS, LMHC, NCC, is the president of and a licensed mental health counselor at PieWiseLiving, LLC; and Susan C. McMillan, PhD, ARNP, FAAN, is a distinguished professor in the College of Nursing at the University of South Florida, all in Tampa. The authors take full responsibility for this content and did not receive honoraria or disclose any relevant financial relationships. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Mention of specific products and opinions related to those products do not indicate or imply endorsement by the Oncology Nursing Society. Tofthagen can be reached at ctofthag@health.usf.edu, with copy to CJONEditor@ons.org. (Submitted August 2016. Accepted November 29, 2016.)
References
Alexander, H., & Litz, B.T. (2014). Prolonged grief disorder: Diagnostic, assessment, and treatment considerations. Professional Psychology: Research and Practice, 45(3), 180–187. doi:10.1037/a0036836
Boelen, P. (2010). Intolerance of uncertainty and emotional distress following the death of a loved one. Anxiety, Stress, and Coping, 23, 471–478. doi:10.1080/10615800903494135
Boelen, P.A., van den Bout, J., & van den Hout, M.A. (2010). A prospective examination of catastrophic misinterpretations and experiential avoidance in emotional distress following loss. Journal of Nervous and Mental Disease, 198, 252–257. doi:10.1097/NMD.0b013e3181d619e4
Boelen, P.A., van den Bout, J., & van den Hout, M.A. (2006). Negative cognitions and avoidance in emotional problems after bereavement: A prospective study. Behaviour Research and Therapy, 44, 1657–1672. doi:10.1016/j.brat.2005.12.006
Bui, E., Nadal-Vicens, M., & Simon, N.M. (2012). Pharmacological approaches to the treatment of complicated grief: Rationale and a brief review of the literature. Dialogues in Clinical Neuroscience, 14, 149–157.
Centers for Medicare and Medicaid Services. (n.d.). Medicare benefit policy manual. Chapter 9—Coverage of hospice services under hospital insurance. Retrieved from https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads…
Dionne-Odom, J.N., Azuero, A., Lyons, K.D., Hull, J.G., Prescott, A.T., Tosteson, T., . . . Bakitas, M.A. (2016). Family caregiver depressive symptom and grief outcomes from the ENABLE III randomized controlled trial. Journal of Pain and Symptom Management, 52, 378–385. doi:10.1016/j.jpainsymman.2016.03.014
Foa, E.B., Chrestman, K., & Gilboa-Schechtman, E. (2008). Prolonged exposure therapy for adolescents with PTSD. New York, NY: Oxford University Press.
Ghesquiere, A., Shear, M.K., & Duan, N. (2013). Outcomes of bereavement care among widowed older adults with complicated grief and depression. Journal of Primary Care and Community Health, 4, 256–264. doi:10.1177/2150131913481231
Ghesquiere, A.R., Aldridge, M.D., Johnson-Hurzeler, R., Kaplan, D., Bruce, M.L., & Bradley, E. (2015). Hospice services for complicated grief and depression: Results from a national survey. Journal of the American Geriatric Society, 63, 2173–2180. doi:10.1111/jgs.13656
Glickman, K., Shear, M.K., & Wall, M. (2016). Exploring outcomes related to anxiety and depression in completers of a randomized controlled trial of complicated grief treatment. Clinical Psychology and Psychotherapy, 23, 118–124. doi:10.1002/cpp.1940
Guldin, M.B., Vedsted, P., Zachariae, R., Olesen, F., & Jensen, A.B. (2012). Complicated grief and need for professional support in family caregivers of cancer patients in palliative care: A longitudinal cohort study. Supportive Care in Cancer, 20, 1679–1685. doi:10.1007/s00520-011-1260-3
Hensley, P.L., Slonimski, C.K., Uhlenhuth, E.H., & Clayton, P.J. (2009). Escitalopram: An open-label study of bereavement-related depression and grief. Journal of Affective Disorders, 113, 142–149. doi:10.1016/j.jad.2008.05.016
Holtslander, L., Duggleby, W., Teucher, U., Cooper, D., Bally, J.M., Solar, J., & Steeves, M. (2016). Developing and pilot-testing a Finding Balance Intervention for older adult bereaved family caregivers: A randomized feasibility trial. European Journal of Oncology Nursing, 21, 66–74. doi:10.1016/j.ejon.2016.01.003
Interpersonal Psychotherapy Institute. (2017). About IPT. Retrieved from https://iptinstitute.com/about-ipt
Kersting, A., Kroker, K., Horstmann, J., Ohrmann, P., Baune, B.T., Arolt, V., & Suslow, T. (2009). Complicated grief in patients with unipolar depression. Journal of Affective Disorders, 118, 201–204. doi:10.1016/j.jad.2009.01.033
Lobb, E.A., Kristjanson, L.J., Aoun, S.M., Monterosso, L., Halkett, G.K., & Davies, A. (2010). Predictors of complicated grief: A systematic review of empirical studies. Death Studies, 34, 673–698. doi:10.1080/07481187.2010.496686
Lubas, M., & De Leo, G. (2014). Online grief support groups: Facilitators’ attitudes. Death Studies, 38, 517–521. doi:10.1080/07481187.2013.873840
Mancini, A.D., Sinan, B., & Bonanno, G.A. (2015). Predictors of prolonged grief, resilience, and recovery among bereaved spouses. Journal of Clinical Psychology, 71, 1245–1258. doi:10.1002/jclp.22224
Mills, H., Reiss, N., & Dombeck, M. (2008, June 30). Self-efficacy and the perception of control in stress reduction. Mental Help. Retrieved from https://www.mentalhelp.net/articles/self-efficacy-and-the-perception-of…
National Alliance on Mental Illness. (2017). Psychotherapy. Retrieved from https://www.nami.org/Learn-More/Treatment/Psychotherapy
Newson, R.S., Boelen, P.A., Hek, K., Hofman, A., & Tiemeier, H. (2011). The prevalence and characteristics of complicated grief in older adults. Journal of Affective Disorders, 132, 231–238. doi:10.1016/j.jad.2011.02.021
O’Connor, M. (2010). A longitudinal study of PTSD in the elderly bereaved: [Corrected] prevalence and predictors. Aging and Mental Health, 14, 310–318. doi:10.1080/13607860903228770
O’Connor, M., Lasgaard, M., Shevlin, M., & Guldin, M.B. (2010). A confirmatory factor analysis of combined models of the Harvard Trauma Questionnaire and the Inventory of Complicated Grief-Revised: Are we measuring complicated grief or posttraumatic stress? Journal of Anxiety Disorders, 24, 672–679. doi:10.1016/j.janxdis.2010.04.009
Piper, W.E., Ogrodniczuk, J.S., Joyce, A.S., & Weideman, R. (2011). Risk factors for complicated grief. In W.E. Piper, J.S. Ogrodniczuk, A.S. Joyce, & R. Weideman (Eds.), Short-term group therapies for complicated grief: Two research-based models. (pp. 63–106). Washington, DC: American Psychological Association.
Schenck, L.K., Eberle, K.M., & Rings, J.A. (2015). Insecure attachment styles and complicated grief severity: Applying what we know to inform future directions. Journal of Death and Dying, 73, 231–249. doi:10.1177/0030222815576124
Shear, K., Frank, E., Houck, P.R., & Reynolds, C.F., 3rd. (2005). Treatment of complicated grief: A randomized controlled trial. JAMA, 293, 2601–2608. doi:10.1001/jama.293.21.2601
Shear, M.K. (2010). Complicated grief treatment: The theory, practice and outcomes. Bereavement Care, 29(3), 10–14. doi:10.1080/02682621.2010.522373
Shear, M.K., Ghesquiere, A., & Glickman, K. (2013). Bereavement and complicated grief. Current Psychiatry Reports, 15, 406. doi:10.1007/s11920-013-0406-z
Shear, M.K., Reynolds, C.F., 3rd, Simon, N.M., Zisook, S., Wang, Y., Mauro, C., . . . Skritskaya, N. (2016). Optimizing treatment of complicated grief: A randomized clinical trial. JAMA Psychiatry, 73, 685–694. doi:10.1001/jamapsychiatry.2016.0892
Shear, M.K., Simon, N., Wall, M., Zisook, S., Neimeyer, R., Duan, N., . . . Keshaviah, A. (2011). Complicated grief and related bereavement issues for DSM-5. Depression and Anxiety, 28, 103–117. doi:10.1002/da.20780
Shear, M.K., Wang, Y., Skritskaya, N., Duan, N., Mauro, C., & Ghesquiere, A. (2014). Treatment of complicated grief in elderly persons: A randomized clinical trial. JAMA Psychiatry, 71, 1287–1295. doi:10.1001/jamapsychiatry.2014.1242
Simon, N.M., Shear, K.M., Thompson, E.H., Zalta, A.K., Perlman, C., Reynolds, C.F., . . . Silowash, R. (2007). The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Comprehensive Psychiatry, 48, 395–399. doi:10.1016/j.comppsych.2007.05.002
Simon, N.M., Shear, M.K., Fagiolini, A., Frank, E., Zalta, A., Thompson, E.H., . . . Silowash, R. (2008). Impact of concurrent naturalistic pharmacotherapy on psychotherapy of complicated grief. Psychiatry Research, 159, 31–36. doi:10.1016/j.psychres.2007.05.011
Simon, N.M., Thompson, E.H., Pollack, M.H., & Shear, M.K. (2007). Complicated grief: A case series using escitalopram. American Journal of Psychiatry, 164, 1760–1761. doi:10.1176/appi.ajp.2007.07050800
Steiner, C.S. (2006). Grief support groups used by few—Are bereavement needs being met? Journal of Social Work in End-of-Life and Palliative Care, 2, 29–53. doi:10.1300/J457v02n0104
Sung, S.C., Dryman, M.T., Marks, E., Shear, M.K., Ghesquiere, A., Fava, M., & Simon, N.M. (2011). Complicated grief among individuals with major depression: Prevalence, comorbidity, and associated features. Journal of Affective Disorders, 134, 453–458. doi:10.1016/j.jad.2011.05.017
Supiano, K.P., & Luptak, M. (2014). Complicated grief in older adults: A randomized controlled trial of complicated grief group therapy. Gerontologist, 54, 840–856. doi:10.1093/geront/gnt076
Tomarken, A., Holland, J., Schachter, S., Vanderwerker, L., Zuckerman, E., Nelson, C., . . . Prigerson, H. (2008). Factors of complicated grief pre-death in caregivers of cancer patients. Psycho-Oncology, 17, 105–111. doi:10.1002/pon.1188
Waller, A., Turon, H., Mansfield, E., Clark, K., Hobden, B., & Sanson-Fisher, R. (2016). Assisting the bereaved: A systematic review of the evidence for grief counselling. Palliative Medicine, 30, 132–148. doi:10.1177/0269216315588728
Wells, M., Mitchell, K.J., Finkelhor, D., & Becker-Blease, K.A. (2007). Online mental health treatment: Concerns and considerations. Cyberpsychology and Behavior, 10, 453–459. doi:10.1089/cpb.2006.9933
Wittouck, C., Van Autreve, S., De Jaegere, E., Portzky, G., & van Heeringen, K. (2011). The prevention and treatment of complicated grief: A meta-analysis. Clinical Psychology Review, 31, 69–78. doi:10.1016/j.cpr.2010.09.005
Yopp, J.M., Park, E.M., Edwards, T., Deal, A., & Rosenstein, D.L. (2015). Overlooked and underserved: Widowed fathers with dependent-age children. Palliative and Supportive Care, 13, 1325–1334. doi:10.1017/s1478951514001321
Zisook, S., Shuchter, S.R., Pedrelli, P., Sable, J., & Deaciuc, S.C. (2001). Bupropion sustained release for bereavement: Results of an open trial. Journal of Clinical Psychiatry, 62, 227–230.
Zygmont, M., Prigerson, H.G., Houck, P.R., Miller, M.D., Shear, M.K., Jacobs, S., & Reynolds, C.F., 3rd. (1998). A post hoc comparison of paroxetine and nortriptyline for symptoms of traumatic grief. Journal of Clinical Psychiatry, 59, 241–245.


