Oncology Volunteers: The Effect of a Personal Cancer History on Compassion and Psychological Well-Being
Background: The impact of support work on volunteers with a personal history of cancer has rarely been examined, despite the possibility that supporting distressed individuals may become a psychological burden for someone who has faced a life-threatening disease themselves.
Objectives: The purpose of this study is to compare compassion, self-compassion, self-coldness, and psychological well-being of oncology volunteers to the general population and clinical samples.
Methods: Volunteers completed questionnaires on demographic and volunteer work–related characteristics, the Compassion Toward Others Scale, the Self-Compassion Scale, and the Psychological General Well-Being Index.
Findings: Overall, volunteers indicated higher levels of self-compassion and psychological well-being and lower levels of self-coldness than clinical and community samples. Peer volunteers were less satisfied with their volunteer work and reported worse general health and psychological well-being than volunteers without a cancer history.
Jump to a section
Social support plays a significant role for patients adapting to a cancer diagnosis and in mitigating treatment-related distress (Luszczynska, Pawlowska, Cieslak, Knoll, & Scholz, 2013; Tedeschi & Calhoun, 2004). Cancer survivors who share similar experiences may be ideally positioned to provide information and support to individuals undergoing treatment (i.e., peers) to decrease social isolation and facilitate adaptive coping (Brunet, Love, Ramphal, & Sabiston, 2014; Pistrang, Jay, Gessler, & Barker, 2012). Peer support involves a survivor providing emotional or informational support to a patient at an earlier stage of the cancer trajectory (Pistrang, Jay, Gessler, & Barker, 2013). Because survivors possess firsthand knowledge of the experience of living with cancer, they offer a unique perspective that may be unavailable to individuals without a personal history of cancer.
Patients newly diagnosed with cancer and their families often are paired with cancer survivors and caregivers through volunteer organizations (Schulman-Green, Wagner, & McCorkle, 2015; Wagner & McCorkle, 2010). Systematic reviews of the psychosocial literature suggest that volunteer support programs are beneficial for patients with cancer who require information, stress management, and empowerment (Campbell, Phaneuf, & Deane, 2004; Hoey, Ieropoli, White, & Jefford, 2008; Macvean, White, & Sanson-Fisher, 2008). However, studies may lack rigorous research design and methodologies (Meyer, Coroiu, & Körner, 2015; Wagner & McCorkle, 2010), and a knowledge gap exists regarding the impact of the support work on volunteers themselves (Pistrang et al., 2013). The broader literature indicates that support providers experience benefits from their work (e.g., enhance self-esteem, self-efficacy, and feelings of social usefulness) (Brown, Hoye, & Nicholson, 2012). However, supporting distressed individuals also can lead to the supporters experiencing mood disturbances (Pistrang et al., 2013) and triggering the supporters’ own anxieties, such as fear of recurrence. Given the potential vulnerability of peer volunteers, healthcare providers may need to monitor volunteers for potentially negative psychosocial effects, prompted by their support of those in distress (Embuldeniya et al., 2013; Giese-Davis et al., 2006; Pistrang et al., 2012, 2013). Nurses are at the forefront of supportive cancer care but also play a leading role in the establishment, maintenance, and integration of volunteer programs into the larger network of psychosocial oncology services. Of concern are risks when volunteers provide peer-based psychosocial care without proper support for them.
Compassion for others and compassion for oneself (i.e., self-compassion) are two related concepts that are important characteristics of volunteers providing direct services to patients with cancer. Compassion consists of recognizing, understanding, and feeling another’s suffering, while also acting to alleviate it (Strauss et al., 2016). Self-compassion is defined as extending kindness to oneself, seeing one’s experience as part of human experience, and being aware of painful thoughts and feelings (Neff, 2003). In contrast, self-coldness (a counterpart to self-compassion) corresponds to feelings of self-judgment, isolation from others, and overidentification with negative thoughts and emotions (Gilbert, McEwan, Matos, & Rivis, 2011). A strong imbalance between compassion toward others and toward oneself may lead oncology volunteers to become emotionally overinvolved in the lives of the patients they serve, leading to unhelpful and even harmful behavior. This behavior may include blaming patients for their problems and for their need for support and offering false reassurance and unsolicited advice (Gottlieb & Wachala, 2007). In addition, the widely demonstrated positive relationship between self-compassion and psychological well-being suggests that self-compassion can act as a coping strategy to prevent compassion fatigue and burnout (Boellinghaus, Jones, & Hutton, 2014; Klimecki & Singer, 2011). Ultimately, the mental health of volunteers is not only important for their own well-being, but also for the success of oncology volunteer programs.
The purpose of this study was to examine volunteer work characteristics, compassion, self-compassion, self-coldness, and psychological well-being in oncology volunteers with a personal cancer history (i.e., peer volunteers) and volunteers who have never been diagnosed with cancer. The following research questions were addressed:
• What are the levels of compassion, self-compassion, self-coldness, and psychological well-being in oncology volunteers?
• Do oncology volunteers, with or without a history of cancer, have different levels of compassion, self-compassion, self-coldness, and psychological well-being compared to general and clinical populations?
• Do peer volunteers and volunteers without a personal cancer history differ in demographic and volunteer work–related characteristics, as well as in compassion, self-compassion, self-coldness, and psychological well-being?
Methods
Data were collected at a well-established community cancer support program, Hope and Cope, and its cancer wellness center in Montreal, Canada, with more than 450 volunteers (340 provide direct patient service). Professional staff and a volunteer executive provide leadership and program administration. Most volunteers have a personal history of cancer, and others have family members or friends diagnosed with the disease. Oncology volunteers provide many services, including mentoring, maintaining the library, transporting patients, sharing information, leading self-support groups, welcoming patients at the reception, presenting workshops, making hospital visits, providing bereavement support, conducting research, and maintaining a newsletter. Oncology volunteers are screened, selected, and assigned to roles that correspond to their interests and to the needs of the organization (Remmer, Edgar, & Rapkin, 2001). They receive a 15-hour orientation program as well as ongoing training, support, and educational opportunities.
Participants and Data Collection
The authors included oncology volunteers aged 18 years or older who were fluent in English and who have direct contact with patients with newly diagnosed cancer (e.g., face-to-face and telephone counseling, hospital visits, group support and workshops). Volunteers with a personal cancer diagnosis were labeled peer volunteers. Volunteers who never were diagnosed with cancer were labeled volunteers without cancer. The term oncology volunteers refers to both groups (i.e., peer volunteers and volunteers without cancer). The study protocol was approved by the ethics board of the hospital associated with the cancer support program, and informed consent was obtained from all participants included in the study. Study invitation, questionnaires, and consent forms were mailed to all eligible oncology volunteers. Participants received as many as three reminder telephone calls to complete the study materials. Data collection took place from April to June 2012.
Measures
Demographic information included age, sex, marital status, occupation, first language, ethnic background, education, and personal or family cancer history.
Volunteer work–related information included the specific domains of volunteer work at the cancer support program, the duration of the volunteering, and the average hours of volunteering per week. Volunteer work satisfaction was assessed with one item rated from 1 (not at all satisfied) to 5 (maximum satisfaction).
Compassion was measured using the total score of the 24-item Compassion Toward Others Scale (CS) (Pommier, 2010) addressing kindness versus indifference, common humanity versus disengagement, and mindfulness versus separation (alpha of the total sample = 0.81).
Self-compassion and self-coldness were assessed with the 26-item Self-Compassion Scale (SCS) (Neff, 2003) addressing self-kindness versus self-judgment, common humanity versus isolation, and mindfulness versus overidentification. In line with research on the psychometric properties of SCS, two composite subscale scores were computed and termed self-compassion for the mean of the three positive subscales and self-coldness for the mean of the three negative subscales (alpha of self-compassion = 0.87, alpha of self-coldness = 0.89) (Brenner, Heath, Vogel, & Credé, 2017; Coroiu et al., 2018; Gilbert et al., 2011; Pfattheicher, Geiger, Hartung, Weiss, & Schindler, 2017).
Psychological well-being was assessed with the 22-item Psychological General Well-Being Index (PGWBI) (Dupuy, 1984) capturing anxiety, depression, positive well-being, self-control, general health, and vitality. The PGWBI has good psychometric properties in clinical samples with chronic physical illness and in general population samples (alpha of total sample = 0.9) (Chassany et al., 2004).
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics, version 20.0, and GraphPad Prism. Descriptive analyses were conducted on demographic characteristics and volunteer work–related information, as well as on compassion, self-compassion, self-coldness, and psychological well-being variables. Peer volunteers and volunteers without cancer were compared on outcome measures using nonparametric methods (Mann–Whitney U test and Kruskal–Wallis test, chi-square test, significance levels Bonferroni correction, Cohen’s d effect sizes).
To address the second study objective, study outcomes were compared to published clinical samples and non-student samples with similar demographic and illness-related characteristics using unpaired t tests with Bonferroni corrections for multiple comparisons. Compassion scores were compared with participant data from a Mindful Self-Compassion (MSC) Program (Pommier, 2010) because the authors could not locate a published study with CS in patients with cancer. Self-compassion and self-coldness subscale scores were compared to data from patients with cancer (Crane-Okada et al., 2012; K. Sherman, personal communication, June 7, 2017; Nakamura, Lipschitz, Kuhn, Kinney, & Donaldson, 2013; Przezdziecki et al., 2013; R. Crane-Okada, personal communication, June 14, 2017; Y. Nakamura, personal communication, June 22, 2017) and community samples (Neff, Whittaker, & Karl, 2017). Psychological well-being scores (PGWBI) were compared to data from patients with colorectal cancer and community adults (Chassany et al., 2004).
Results
A total of 147 (43%) of 340 eligible oncology volunteers completed questionnaires. The majority of the oncology volunteers were Caucasian women aged 55 years or older with an average of 15.67 years of education (SD = 3.22, range = 7–24) (see Table 1). Other ethnic backgrounds included Asian, African American, and Hispanic. 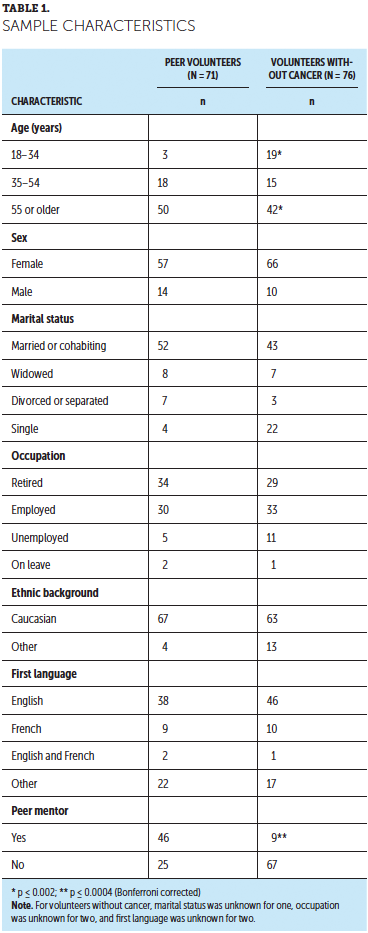
Almost all oncology volunteers had experiences related to cancer. About half of the sample (n = 71, 48%) had a cancer diagnosis (i.e., peer volunteers), and most had a family member (n = 99, 67%) or friend (n = 52, 35%) with cancer. The most common cancer diagnosis among peer volunteers was breast cancer (n = 25, 35%), followed by hematologic cancers (n = 11, 16%). On average, the most recent cancer diagnosis and treatment completion date occurred 10.9 (SD = 6.6, range = 1–32) and 8.25 (SD = 5.58, range = 0–26) years prior to study enrollment, respectively. Participants had been active volunteers at the community cancer support program for an average of six years (mean = 6.27, SD = 6.29, range = 0.5–31), volunteering for four hours a week (mean = 4.01, SD = 2.59, range = 1–15). Study participants reported high satisfaction with their volunteer work (mean = 4.35, SD = 0.68, range = 2–5).
Data Analysis
To provide context, the current findings were compared to those from clinical and community studies. The authors identified one study examining compassion using CS, three studies reporting on self-compassion using SCS, and two studies on psychological well-being using PGWBI. The current authors contacted authors who conducted studies using SCS but did not report subscale scores for self-compassion and self-coldness in their published reports.
Information about these comparative samples (e.g., age, gender, diagnosis, intervention program) is presented in Table 2. No significant differences were found between CS scores in the current study’s volunteer sample and a community sample of participants of an MSC program (Neff & Germer, 2013). The current study’s oncology volunteers reported significantly higher self-compassion subscale scores than breast cancer survivors and community adults did, but they did not differ significantly from baseline data of patients with breast cancer who were enrolled in a Mindful Movement Program intervention. Self-coldness subscale scores were significantly lower in oncology volunteers than in all identifiable samples of patients with breast cancer and community adults. The current study participants reported more psychological well-being (PGWBI) than a general population sample and a sample of patients with colorectal cancer. 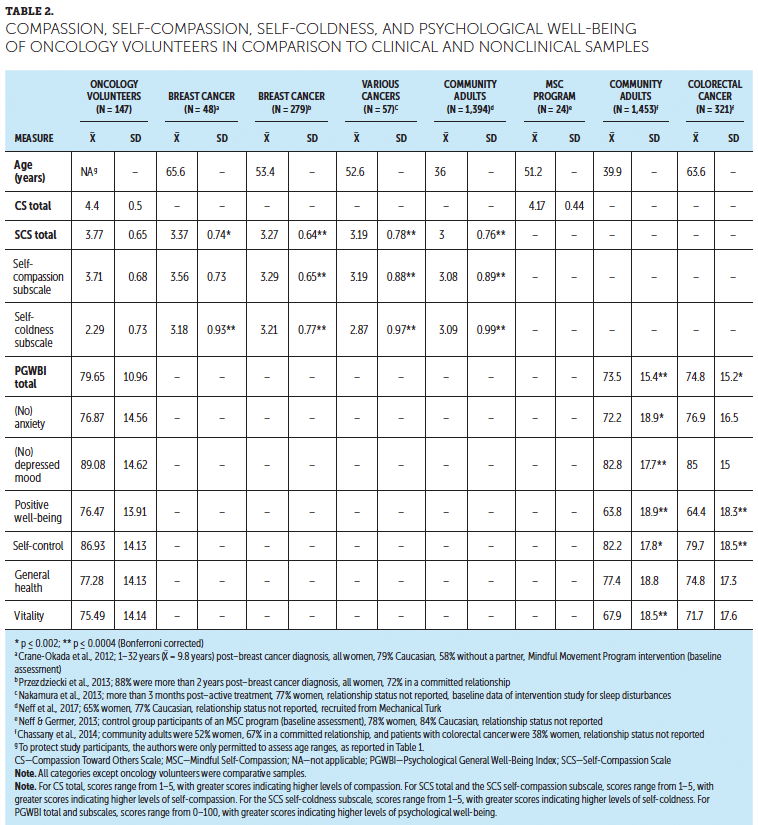
When comparing volunteers without cancer to peer volunteers, the latter were significantly older and were more likely to act as mentors for patients with cancer and their loved ones. In addition, peer volunteers were less satisfied with their volunteering job (mean = 4.2, SD = 0.69 versus mean = 4.49, SD = 0.64; U[df] = 2,067.5 [145], p < 0.01) and had served as volunteers for a longer time (mean = 7.61 years, SD = 6.01 versus mean = 5.05 years, SD = 6.34; U[df] = 1,659 [141], p < 0.001). Finally, peer volunteers did not differ from volunteers without cancer regarding compassion, self-compassion, and self-coldness. However, peer volunteers felt less psychological well-being and reported worse general health (see Table 3). 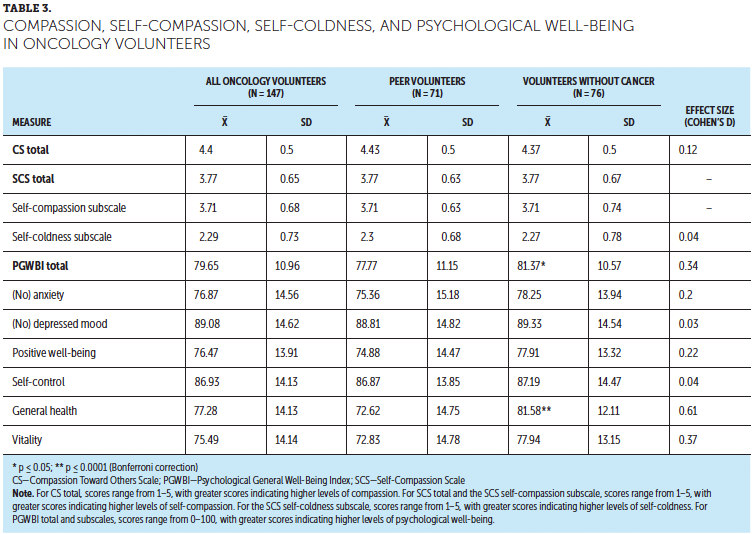
Discussion
The purpose of the current study was to examine demographics; work-related characteristics; and levels of compassion, self-compassion, self-coldness, and psychological well-being in volunteers at an oncology support program consisting of individuals with and without a personal history of cancer. The authors also compared the sample’s CS, SCS, and PWBGI scores to published findings for patients with cancer and the general population (i.e., North American community samples).
The results suggests that volunteer work within a community cancer support program can be experienced as highly satisfactory, with participants in the current study completing, on average, more than six years of service. Mirrielees et al. (2017) evaluated a peer support program for patients with breast cancer and also found high satisfaction and a sense of accomplishment in support providers. Satisfaction with the volunteer experience in the current sample also was similar to that in a study by Remmer et al. (2001), who examined the same cancer support program more than 16 years ago. Despite overall high satisfaction, peer volunteers felt significantly less satisfied with their volunteer work when compared to their colleagues without a personal history of cancer. This difference may be attributed to the nature of the volunteer work, but it is also possible that volunteers without cancer can keep some emotional distance from their work while feeling less burdened or less discouraged by the limitations of the support they can provide.
Overall, the current sample of oncology volunteers fared well when compared to community samples and patients with cancer. Study participants reported less anxiety and depression and more psychological well-being, self-control, and vitality than a large community sample (Dupuy, 1984). Although both samples included similar proportions of married or cohabiting individuals (n = 95, 65% of oncology volunteers and n = 974, 67% of community adults), the older age of the study participants may have contributed to these findings; 92 participants (63%) were at least 55 years of age, and the mean age in the comparison sample was 40 years. Higher life satisfaction and better psychological well-being have been reported in studies of participants from Western countries (Carr, Freedman, Cornman, & Schwarz, 2014; Steptoe, Deaton, & Stone, 2015; Stone, Schwartz, Broderick, & Deaton, 2010; Van Willigen, 2000), oncology volunteers (Wittenberg et al., 2010), older adults (Steptoe et al., 2015; Van Willigen, 2000), and those who are married (Carr et al., 2014; Wittenberg et al., 2010). In addition, participants in the current study experienced less self-coldness and more self-compassion than clinical and nonclinical samples, regardless of whether they had a personal history of cancer. However, the cross-sectional design does not allow for determining causality. The current study’s results suggest that oncology volunteers are a self-selected group of individuals who dealt well enough with adversity related to their cancer experience to be capable of lending a helping hand to others in need. It is also possible that providing support to others may further enhance one’s experience of meaning in life (Frazier et al., 2013) and increase feelings of compassion and self-compassion (Konrath & Brown, 2013). Finally, volunteer work can provide additional opportunities for sharing of emotions, social support, and cognitive and emotional processing of the cancer experience, and it can promote posttraumatic growth (Calhoun & Tedeschi, 2006; Cohen & Numa, 2011).
When comparing volunteers with and without a history of cancer, the participants did not differ significantly regarding compassion, self-compassion, self-coldness, and several indicators of psychological well-being. However, cancer survivors in the current sample reported worse general health than their colleagues without a personal history of cancer. This result is not surprising given the older age of the peer volunteer group and their medical history. Still, the lower overall psychological well-being of peer volunteers may not have been exclusively driven by age and medical history, because peer volunteers also reported less positive well-being, less vitality, and more symptoms of anxiety (after correcting for type 1 error, these differences were not statistically significant). Because most cancer survivors live with a lifelong risk of recurrence associated with psychological distress, the current findings speak to the need to be sensitive to potential support needs of those who volunteer to provide support.
Limitations and Future Directions
The results of the current study may be limited by self-selection bias, given the study participation rate of 44%. Oncology volunteers who were less satisfied and experienced lower compassion, self-compassion, or psychological well-being may not have responded to the study invitation. Nevertheless, this is one of the few studies addressing psychological characteristics of support providers in the context of cancer care. Future research may benefit from also assessing the perceived quality and quantity of the peer support in support recipients compared to providers; it has been shown that the psychological state of both parties could influence the effectiveness and perception of the support interaction (Embuldeniya et al., 2013; Giese-Davis et al., 2006; Pistrang et al., 2013; Pistrang, Solomons, & Barker, 1999). It would also be valuable to extend this work toward examining the satisfaction, well-being, and compassion of healthcare professionals, particularly nurses who interact with patients most closely and are major supportive care providers in oncology. This may further the authors’ insight into the challenges and protective factors across different groups that are facing the task of supporting individuals and families touched by a life-threatening medical condition. 
Implications for Practice
As leaders in hospitals and care centers, nurses play an important role in the training and management of oncology volunteers. The results of the current study confirm the importance of proper psychoeducation and training for oncology volunteers. Volunteer program coordinators and nurses working alongside peer volunteers can be particularly sensitive to the well-being of oncology volunteers with a personal history of cancer. Training for these positions may include content specifically tailored to the potential needs of peer volunteers, such as modules on self-care. Exercises aimed at increasing self-compassion and decreasing self-coldness may be appropriate because this may be a protective factor for oncology volunteers (Körner et al., 2015). Continued formal or informal monitoring of peer volunteer well-being also may prove beneficial. Nurses are an integral part of supportive cancer care and could play a leading role in this movement. Oncology nurses must advance care while being sensitive to volunteers’ well-being, as well as practicing self-care and self-compassion (see Figure 1) and addressing their own signs of early burnout. 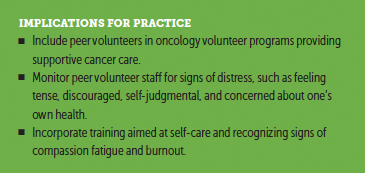
Conclusion
Oncology volunteers, including those with a personal history of cancer, indicated higher levels of self-compassion and psychological well-being than patients with cancer and even community samples. This speaks for including peer volunteers when expanding volunteer programs as part of supportive care services in oncology and when establishing such programs where they do not exist yet. [[{"fid":"44366","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"height":"586","width":"366","style":"font-size: 13.008px;","class":"media-element file-default","data-delta":"1"}}]]
The authors gratefully acknowledge Hope and Cope staff members Hinda Goodman, BSc, MSW, Suzanne O’Brien, MA, and Mara Laura Leimanis, PhD, for their assistance with volunteer recruitment, and undergraduate students Melanie Mulligan-Pittarelli and Cong Zhang for their assistance with data collection and data entry.
About the Author(s)
Alexandra Meyer, PhD, is a postdoctoral fellow in the Department of Medical Psychology and Medical Sociology at the University Medical Center in Leipzig, Germany; Chelsea Moran, BSc, is a master’s student in the Department of Educational and Counseling Psychology at McGill University in Montreal, Canada; Tanya Fitzpatrick, PhD, MSW, RN, is a professor emerita in the School of Social Work at Arizona State University in Phoenix; Jochen Ernst, PhD, is a research assistant in the Department of Medical Psychology and Medical Sociology at the University Medical Center; and Annett Körner, PhD, is an associate professor in the Department of Educational and Counseling Psychology at McGill University. The authors take full responsibility for this content. This research was supported by grants from German Cancer Aid. Fitzpatrick has received honorarium from Springer Publishing for a previous publication. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Meyer can be reached at meyeralexandra@web.de, with copy to CJONEditor@ons.org. (Submitted September 2017. Accepted December 8, 2017.)
References
Boellinghaus, I., Jones, F.W., & Hutton, J. (2014). The role of mindfulness and loving-kindness meditation in cultivating self-compassion and other-focused concern in health care professionals. Mindfulness, 5, 129–138. https://doi.org/10.1007/s12671-012-0158-6
Brenner, R.E., Heath, P.J., Vogel, D.L., & Credé, M. (2017). Two is more valid than one: Examining the factor structure of the Self-Compassion Scale (SCS). Journal of Counseling Psychology, 64, 696–707. https://doi.org/10.1037/cou0000211
Brown, K.M., Hoye, R., & Nicholson, M. (2012). Self-esteem, self-efficacy, and social connectedness as mediators of the relationship between volunteering and well-being. Journal of Social Service Research, 38, 468–483. https://doi.org/10.1080/01488376.2012.687706
Brunet, J., Love, C., Ramphal, R., & Sabiston, C.M. (2014). Stress and physical activity in young adults treated for cancer: The moderating role of social support. Supportive Care in Cancer, 22, 689–695. https://doi.org/10.1007/s00520-013-2023-0
Calhoun, L.G., & Tedeschi, R.G. (2006). The foundations of posttraumatic growth: An expended framework. In L.G. Calhoun & R.G. Tedeschi (Eds.), Handbook of posttraumatic growth: Research and practice (pp. 3–23). Mahwah, NJ: Lawrence Erlbaum Associates.
Campbell, H.S., Phaneuf, M.R., & Deane, K. (2004). Cancer peer support programs—Do they work? Patient Education and Counseling, 55, 3–15. https://doi.org/10.1016/j.pec.2003.10.001
Carr, D., Freedman, V.A., Cornman, J.C., & Schwarz, N. (2014). Happy marriage, happy life? Marital quality and subjective well-being in later life. Journal of Marriage and the Family, 76, 930–948. https://doi.org/10.1111/jomf.12133
Chassany, O., Dimenäs, E., Zeneca, A., Dubois, D., Wu, A., & Dupuy, H. (2004). The Psychological General Well-Being Index (PGWBI) user manual. Lyone, France: MAPI Research Institute.
Cohen, M., & Numa, M. (2011). Posttraumatic growth in breast cancer survivors: A comparison of volunteers and non-volunteers. Psycho-Oncology, 20, 69–76. https://doi.org/10.1002/pon.1709
Coroiu, A., Kwakkenbos, L., Moran, C., Thombs, B., Albani, C., Bourkas, S., . . . Körner, A. (2018). Structural validation of the self-compassion scale with a German general population. PLOS One, 13(2), e0190771. https://doi.org/10.1371/journal.pone.0190771
Crane-Okada, R., Kiger, H., Sugerman, F., Uman, G.C., Shapiro, S.L., Wyman-McGinty, W., & Anderson, N.L. (2012). Mindful movement program for older breast cancer survivors: A pilot study. Cancer Nursing, 35, E1–E13. https://doi.org/10.1097/NCC.0b013e3182280f73
Dupuy, H.J. (1984). The Psychological General Well-Being (PGWB) Index. In N.K. Wenger, M.E. Mattson, C.D. Furburg, & J. Elinson (Eds.), Assessment of quality of life in clinical trials of cardiovascular therapies (pp. 170–183). New York, NY: Le Jacq Publishing.
Embuldeniya, G., Veinot, P., Bell, E., Bell, M., Nyhof-Young, J., Sale, J.E., & Britten, N. (2013). The experience and impact of chronic disease peer support interventions: A qualitative synthesis. Patient Education and Counseling, 92, 3–12. https://doi.org/10.1016/j.pec.2013.02.002
Frazier, P., Greer, C., Gabrielsen, S., Tennen, H., Park, C., & Tomich, P. (2013). The relation between trauma exposure and prosocial behavior. Psychological Trauma, 5, 286–294. https://doi.org/10.1037/a0027255
Giese-Davis, J., Bliss-Isberg, C., Carson, K., Star, P., Donaghy, J., Cordova, M.J., . . . Spiegel, D. (2006). The effect of peer counseling on quality of life following diagnosis of breast cancer: An observational study. Psycho-Oncology, 15, 1014–1022. https://doi.org/10.1002/pon.1037
Gilbert, P., McEwan, K., Matos, M., & Rivis, A. (2011). Fears of compassion: Development of three self-report measures. Psychology and Psychotherapy, 84, 239–255. https://doi.org/10.1348/147608310X526511
Gottlieb, B.H., & Wachala, E.D. (2007). Cancer support groups: A critical review of empirical studies. Psycho-Oncology, 16, 379–400. https://doi.org/10.1002/pon.1078
Hoey, L.M., Ieropoli, S.C., White, V.M., & Jefford, M. (2008). Systematic review of peer-support programs for people with cancer. Patient Education and Counseling, 70, 315–337. https://doi.org/10.1016/j.pec.2007.11.016
Klimecki, O.M., & Singer, T. (2011). Empathic distress fatigue rather than compassion fatigue? Integrating findings from empathy research in psychology and social neuroscience. In B. Oakley, A. Knafo, G. Madhavan, & D.S. Wilson (Eds.), Pathological altruism (pp. 368–383). New York, NY: Oxford University Press.
Konrath, S., & Brown, S. (2013). The effects of giving on givers. In M.L. Newman, & N.A. Roberts (Eds.), Health and social relationships: The good, the bad, and the complicated (pp. 39–64). Washington, DC: American Psychological Association.
Körner, A., Coroiu, A., Copeland, L., Gomez-Garibello, C., Albani, C., Zenger, M., & Brähler, E. (2015). The role of self-compassion in buffering symptoms of depression in the general population. PLOS One, 10(10), e0136598. https://doi.org/10.1371/journal.pone.0136598
Luszczynska, A., Pawlowska, I., Cieslak, R., Knoll, N., & Scholz, U. (2013). Social support and quality of life among lung cancer patients: A systematic review. Psycho-Oncology, 22, 2160–2168. https://doi.org/10.1002/pon.3218
Macvean, M.L., White, V.M., & Sanson-Fisher, R. (2008). One-to-one volunteer support programs for people with cancer: A review of the literature. Patient Education and Counseling, 70, 10–24. https://doi.org/10.1016/j.pec.2007.08.005
Meyer, A., Coroiu, A., & Körner, A. (2015). One-to-one peer support in cancer care: A review of scholarship published between 2007 and 2014. European Journal of Cancer Care, 24, 299–312. https://doi.org/10.1111/ecc.12273
Mirrielees, J.A., Breckheimer, K.R., White, T.A., Denure, D.A., Schroeder, M.M., Gaines, M.E., . . . Tevaarwerk, A.J. (2017). Breast cancer survivor advocacy at a university hospital: Development of a peer support program with evaluation by patients, advocates, and clinicians. Journal of Cancer Education, 32, 97–104. https://doi.org/10.1007/s13187-015-0932-y
Nakamura, Y., Lipschitz, D.L., Kuhn, R., Kinney, A.Y., & Donaldson, G.W. (2013). Investigating efficacy of two brief mind-body intervention programs for managing sleep disturbance in cancer survivors: A pilot randomized controlled trial. Journal of Cancer Survivorship, 7, 165–182. https://doi.org/10.1007/s11764-012-0252-8
Neff, K.D. (2003). The development and validation of a scale to measure self-compassion. Self and Identity, 2, 223–250. https://doi.org/10.1080/15298860390209035
Neff, K.D., & Germer, C.K. (2013). A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology, 69, 28–44. https://doi.org/10.1002/jclp.21923
Neff, K.D., Whittaker, T.A., & Karl, A. (2017). Examining the factor structure of the self-compassion scale in four distinct populations: Is the use of a total scale score justified? Journal of Personality Assessment, 99, 596–607. https://doi.org/10.1080/00223891.2016.1269334
Pfattheicher, S., Geiger, M., Hartung, J., Weiss, S., & Schindler, S. (2017). Old wine in new bottles? The case of self-compassion and neuroticism. European Journal of Personality, 31, 160–169. https://doi.org/10.1002/per.2097
Pistrang, N., Jay, Z., Gessler, S., & Barker, C. (2012). Telephone peer support for women with gynaecological cancer: Recipients’ perspectives. Psycho-Oncology, 21, 1082–1090. https://doi.org/10.1002/pon.2005
Pistrang, N., Jay, Z., Gessler, S., & Barker, C. (2013). Telephone peer support for women with gynaecological cancer: Benefits and challenges for supporters. Psycho-Oncology, 22, 886–894. https://doi.org/10.1002/pon.3080
Pistrang, N., Solomons, W., & Barker, C. (1999). Peer support for women with breast cancer: The role of empathy and self-disclosure. Journal of Community and Applied Social Psychology, 9, 217–229.
Pommier, E.A. (2010). The compassion scale [Doctoral disseration]. Retrieved from https://repositories.lib.utexas.edu/handle/2152/ETD-UT-2010-12-2213
Przezdziecki, A., Sherman, K.A., Baillie, A., Taylor, A., Foley, E., & Stalgis-Bilinski, K. (2013). My changed body: Breast cancer, body image, distress and self-compassion. Psycho-Oncology, 22, 1872–1879. https://doi.org/10.1002/pon.3230
Remmer, J., Edgar, L., & Rapkin, B. (2001). Volunteers in an oncology support organization: Motivations, stress and satisfactions. Journal of Psychosocial Oncology, 19, 63–83. https://doi.org/10.1300/J077v19n01_05
Schulman-Green, D., Wagner, E.H., & McCorkle, R. (2015). Self-management support. In J.C. Holland, W.S. Breitbart, P.B. Jacobsen, M.L. Loscalzo, R. McCorkle, & P.N. Butow (Eds.), Psycho-Oncology (3rd ed., pp. 464–470). New York, NY: Oxford University Press.
Steptoe, A., Deaton, A., & Stone, A.A. (2015). Subjective wellbeing, health, and ageing. Lancet, 385, 640–648. https://doi.org/10.1016/S0140-6736(13)61489-0
Stone, A.A., Schwartz, J.E., Broderick, J.E., & Deaton, A. (2010). A snapshot of the age distribution of psychological well-being in the United States. Proceedings of the National Academy of Sciences of the United States of America, 107, 9985–9990. https://doi.org/10.1073/pnas.1003744107
Strauss, C., Lever Taylor, B., Gu, J., Kuyken, W., Baer, R., Jones, F., & Cavanagh, K. (2016). What is compassion and how can we measure it? A review of definitions and measures. Clinical Psychology Review, 47, 15–27. https://doi.org/10.1016/j.cpr.2016.05.004
Tedeschi, R.G., & Calhoun, L.G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15, 1–18.
Van Willigen, M. (2000). Differential benefits of volunteering across the life course. Journals of Gerontology Series B, 55, S308–S318.
Wagner, E.H., & McCorkle, R. (2010). Self-management support. In J.C. Holland, W.S. Breitbart, P.B. Jacobsen, M.S. Lederberg, M.J. Loscalzo, & R. McCorkle (Eds.), Psycho-Oncology (2nd ed., pp. 464–469). New York, NY: Oxford University Press.
Wittenberg, L., Yutsis, M., Taylor, S., Giese-Davis, J., Bliss-Isberg, C., Star, P., & Spiegel, D. (2010). Marital status predicts change in distress and well-being in women newly diagnosed with breast cancer and their peer counselors. Breast Journal, 16, 481–489. https://doi.org/10.1111/j.1524-4741.2010.00964.x




