Adolescent Cancer Survivors: A Literature Review of Psychological Effects Following Remission
Background: The psychological distress caused by cancer can remain long after remission. With advanced curative treatments, many pediatric patients continue to have late complications that interfere with neurologic, physical, and social development.
Objectives: The aim of this article is to analyze nine published articles that focus on adolescent cancer survivors (ACSs) and the incidence and risk factors of post-traumatic stress disorder (PTSD) and post-traumatic stress symptoms (PTSSs).
Methods: A search of published articles including pediatric and adolescent oncology and PTSD was performed. The search was narrowed to peer-reviewed articles published after 2010 that presented empirical data and were specific to post-trauma or post-traumatic stress.
Findings: Significant findings for PTSD and PTSSs were reported in ACSs. ACSs suffering from PTSD and PTSSs should be identified and treated appropriately based on age, diagnosis, treatment, and comorbid symptoms.
Jump to a section
A pediatric patient becoming a patient with cancer is a life-altering event. Type and staging, imaging, chemotherapy, treatments, and short- and long-term complications determine how a child progresses from childhood to adolescence. With continuing medical advancements and improved prognosis, research in pediatric psycho-oncology has shifted to long-term survivor adaptation and an increased effort to identify psychological symptoms early (Wenninger et al., 2013). A significant portion of adolescent cancer survivors (ACSs) experience psychological stressors clinically related to the diagnosis of post-traumatic stress disorder (PTSD) and post-traumatic stress symptoms (PTSSs) (Bellizzi et al., 2012; Brinkman et al., 2013; Kwak et al., 2013; Stuber et al., 2010; Wenninger et al., 2013; Zebrack et al., 2013). Conversely, research defines post-traumatic growth (PTG) as positive changes and outcomes emerging from a cancer diagnosis and treatment (Turner-Sack, Menna, Setchell, Maan, & Cataudella, 2012). This article aims to synthesize the literature to determine PTSD and PTSSs in ACSs to increase awareness for pediatric providers, specialists, patients, and parents affected by PTSD and PTSSs to ultimately develop interventions.
PTSSs include re-experiencing an event and completely avoiding emotions related to trauma (American Psychiatric Association [APA], 2013). The definition of PTSD includes one occurrence of re-experiencing, three avoidance symptoms, and two symptoms of increased arousal (APA, 2013). Also, the definition of PTSD includes PTSSs that last for at least one month after a traumatic event and PTSSs that ultimately become physical symptoms that lead to a decline in overall function (APA, 2013). PTG is a psychological construct. When an individual has a traumatic, life-changing experience, this experience eventually can lead to beneficial changes in outlook, priorities, and relationships (Turner-Sack et al., 2012). Focus in pediatric cancer has shifted significantly, from high mortality rates to an increasing number of survivors who are learning to cope and adapt. The paradigm opens doors for research to develop and enforce interventions for ACS.
Background
The ongoing psychological distress caused by cancer can remain long after remission. The Children’s Oncology Group (COG) implemented long-term follow-up guidelines for childhood, adolescent, and young adult cancer survivors. These guidelines promote healthy lifestyles, arrange continual monitoring of health conditions, expedite early identification of possible late symptomatology, and provide a prompt intervention for potential late effects (COG, 2013). According to COG (2013), these guidelines provide standards of practice for follow-up care for pediatric patients with cancer and their providers. COG recommends annual psychological evaluations and continual monitoring. A baseline neurologic evaluation for patients at increased risk for cognitive comorbidities also is recommended. High-risk ACSs should have frequent reevaluations (COG, 2013). Because of resource limitations, most notably lower income, these guidelines are not smoothly executed (Kahalley et al., 2013). For example, in a study by Kahalley et al. (2013), some families chose not to follow through on referrals recommended by their providers because of income level. Parents may be forced to choose between a day of pay and taking their child to a clinic. In addition, when children are referred for psychological services in a nearby area or community, the provider’s survivorship expertise could have limitations. Even when healthcare providers and patients’ families are proactive, operational barriers in the medical field limit necessary school or mental health resources in many settings (Kahalley et al., 2013).
With advanced curative treatments, many pediatric patients continue to have late complications that interfere with neurologic, physical, and social development. In the Childhood Cancer Survivor Study (CCSS), 9,126 ACSs and 2,968 siblings completed an assessment of their suicide ideation within the past week (Recklitis et al., 2010). Results indicated that 8% of ACSs reported suicide ideation, compared to 5% of sibling controls. These findings correlated to the physical health of the patients (Recklitis et al., 2009). Unfortunately, the processes to identify PTSD symptoms and other mental health issues in ACSs are suboptimal (Hahn, Hays, Kahn, Litwin, & Ganz, 2015).
Allostatic Load
Allostatic load is defined as physiological consequences of chronic stress on the body (Hahn et al., 2015). Examples of allostatic load may include high blood pressure, increased cholesterol, and increased cortisol levels. These physiologic implications can increase with the chronic stress associated with cancer and may be elevated in individuals experiencing PTSD symptomatology (Hahn et al., 2015). The effect of allostatic load on individuals can negatively affect their overall health status and lead to potentially life-altering repercussions. Similarly, in a study by Schwartz et al. (2010), 156 cancer survivors and 138 controls completed the Health Knowledge Inventory. Results confirmed that cancer survivors have almost double the number of health problems when compared with healthy controls (5.6 versus 2.6). Significantly more comorbid symptoms could lead to enhanced psychological distress, including PTSD and PTSSs (Schwartz et al., 2010).
Risk Factors for PTSD and PTSSs
Table 1 lists several characteristics of a diagnosis of PTSD or PTSSs that lead to differences in overall psychological stress. These risk factors should be used to stratify adolescent patients for targeted screening. 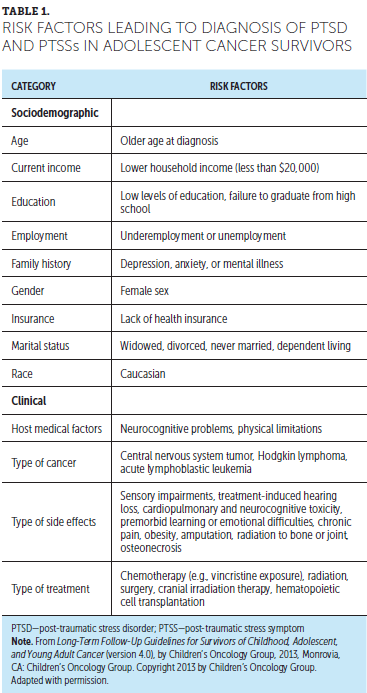
Significance of Adolescent Developmental Stage
Cancer affects developmental milestone potential. Children are at a heightened risk for mental distress because cancer can interfere with development (e.g., social aspects, emotional aspects, language, learning, thinking, problem solving, gross motor movement) (Zebrack et al., 2013). Research is limited on ACSs as they begin to decipher medical information and responsibilities; manage treatment hardships; maintain everyday activities with family, friends, and school; and cope with the diagnosis of cancer (Zebrack et al., 2013). Given the complexity of the developmental stage and increased pressure in terms of education, employment, and independence, a cancer diagnosis adds severe stress (Zebrack et al., 2013). Changes in physical appearance, a premature encounter with possible mortality, interruptions in work or school, increased dependence on parents, increased insurance or financial troubles, potential loss of reproductive means, late effects of treatments, and questions or concerns about health pose difficulties for ACSs (D’Agostino, Penney, & Zebrack, 2011; Zebrack et al., 2013).
Screening for PTSD and PTSSs
Screening can identify and measure which stressors determine psychological distress, functional impairment, and response to trauma. Table 2 shows screening tools that assess these three categories. Most ACSs are psychologically healthy (Brinkman et al., 2013). Specific ACS subgroups are at an increased risk for severe emotional distress, such as depression, somatization, and anxiety (Brinkman et al., 2013). Screening efforts during adolescence could help identify survivors for whom interventions may work to counter psychological symptoms and potentially neutralize the worsening of symptoms into adulthood (Brinkman et al., 2016). Screening tools should include both parent and survivor report of symptoms (Brinkman et al., 2016). 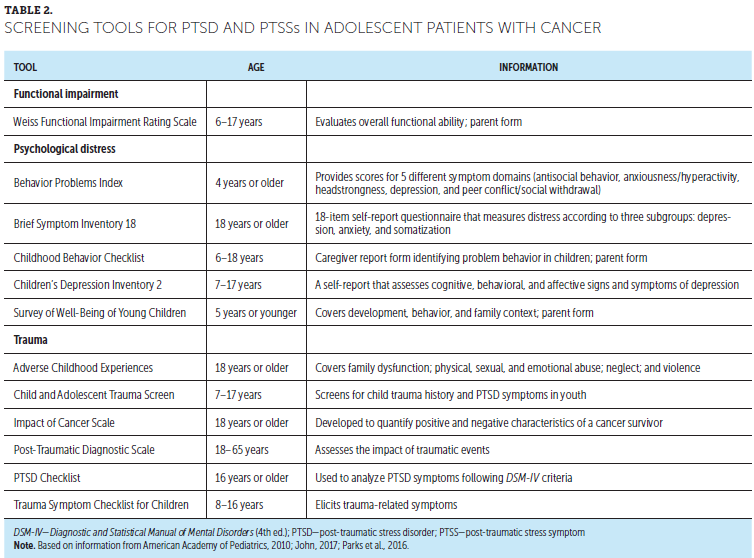
Literature Review
Most studies evaluating adolescent PTSD and PTSSs use CCSS, which is a subdivision of COG’s long-term follow-up study. CCSS is a study of childhood cancer survivors aged 5 years or older and diagnosed before age 21 years (Brinkman et al., 2013, 2016). The cohort has been assembled from 31 centers in the United States and represents 35,923 childhood cancer survivors and more than 5,000 siblings (Brinkman et al., 2013, 2016). Other cohorts include the Cancer Survivor Registry and the St. Jude Lifetime Cohort study.
A search of published studies including pediatric and adolescent oncology and PTSD was performed using PubMed, Google Scholar, and CINAHL®. The search was narrowed to peer-reviewed articles published after 2010. For studies to be included, they had to present empirical data and be specific to post-trauma or post-traumatic stress. The results had to be specific to post-trauma in ACSs in the United States who were either diagnosed at adolescence or were adolescents at the time of the baseline survey. Keyword stems included adolescent, adolescence, AYA, pediatrics, and pediatric, followed by oncology and cancer, and last, post-trauma, post-traumatic stress disorder, and post-traumatic stress symptoms. From the combined search, 100 articles were identified from 2010–2017. Using the inclusion criteria previously stated, nine articles were analyzed.
Results
Table 3 summarizes the nine included articles. The results contained clinically relevant findings related to PTSD and PTSSs in ACSs. According to the results, ACSs were more likely to be diagnosed with clinically significant PTSSs compared to PTSD, but a greater percentage of participants were at increased risk for developing PTSD. [[{"fid":"46656","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
Post-Traumatic Stress Disorder
Significant findings for PTSD ranged from 9%–29% (Kwak et al., 2013; Stuber et al., 2010; Wenninger et al., 2013). At the 12-month follow-up, using Diagnostic and Statistical Manual of Mental Disorders (4th ed.) (DSM-IV) criteria, 29% of adolescents and young adults were at increased risk for developing PTSD (Kwak et al., 2013). This study identified risk for PTSD, not a confirmed diagnosis of PTSD. In a study by Stuber et al. (2010), 9% of patients reported having functional impairment, clinical distress, and symptoms related to PTSD, compared to 2% of siblings. On the Post-Traumatic Diagnostic Scale, 14% of the sample had raw scores that were clinically significant for PTSD (Wenninger et al., 2013). Of this 14%, 50% of the patients had a propensity to suppress negative thoughts and decreased levels of optimism (Wenninger et al., 2013). Although most ACSs seemingly are well-adjusted, a clinically significant number reported markedly high levels of psychological distress (Wenninger et al., 2013).
Post-Traumatic Stress Symptoms
Findings significant for PTSSs ranged from 12%–44% (Brinkman et al., 2013, 2016; Kazak et al., 2010; Kwak et al., 2013; Schwartz et al., 2012; Seitz et al., 2010; Stuber et al., 2011). In the study by Kwak et al. (2013), the prevalence of PTSSs was significantly higher compared to that in similar studies. At 12 months post-diagnosis, 39% of ACSs manifested PTSSs as early as six months post-diagnosis, and 44% demonstrated PTSSs (Kwak et al., 2013). The level did not shift significantly during a six-month period. At least 3% of ACSs reported severe levels of PTSSs (Kwak et al., 2013). In the study by Schwartz et al. (2012), PTSSs evaluated with the PTSD Checklist–civilian version ranged from 17–84. From these findings, 12% had a score above 40, indicating clinically significant PTSSs (Schwartz et al., 2012). Accordingly, in the study by Seitz et al. (2010), 22% of ACSs experienced symptoms of post-traumatic stress, including anxiety or depression, in contrast to only 14% of controls.
Overall, in comparison to sibling controls, ACSs experienced greater rates of post-traumatic stress as defined within DSM-IV criteria (Stuber et al., 2011). Findings in the studies by Brinkman et al. (2013), Brinkman et al. (2016), and Kazak et al. (2010) identified subgroups of ACSs who experienced greater levels of depression, anxiety, and somatization related to increased treatment intensity and cranial radiation therapy.
Discussion
ACSs have an increased risk of developing long-term psychological effects based on their diagnosis, treatment, and support system. Evaluation and treatment are crucial in long-term survivorship care.
Unmet Needs
Mental health issues of ACSs are distinct from those of younger children and adult populations. In addition, ACSs may be treated inappropriately or inadequately by psychological cancer services (Zebrack et al., 2013). Of note, studies suggest that the unmet need for professional psychological services increased as ACSs reported negative health-related symptoms from treatments (Zebrack et al., 2013). Similarly, in a study by Kahalley et al. (2013), ACSs experienced mental health hardships that were not adequately managed by appropriate psychological services.
Comorbid post-treatment symptoms contribute to high levels of distress. These findings indicate a crucial deficiency of psychosocial support (Zebrack et al., 2013). According to Zebrack et al. (2013), almost half of ACSs within the first four months of diagnosis reported an unmet need for information regarding exercise and nutrition. In addition, half of the ACS sample stated an unmet need for adequate mental health services (Zebrack et al., 2013).
Post-Traumatic Growth
PTG is positive change following a cancer diagnosis and treatment (Smith, Samsa, Ganz, & Zimmerman, 2014). The term post-traumatic indicates that this growth occurs after an extreme or life-changing event. This phenomenon is not caused by other minor stresses, nor is it considered a natural process of development (Sumalla, Ochoa, & Blanco, 2009). In connection to PTG, studies define resilience as a positive psychological event, despite direct exposure to traumatic experiences (Phipps et al., 2014). In a study exploring the relationship between PTSSs and PTG, researchers found no association between PTSSs and PTG at 12 months following diagnosis (Zebrack et al., 2015). Zebrack et al. (2015) also reported a relationship among a specific post-traumatic stress symptom, re-experiencing it, and two signs of PTG (new possibilities and personal strengths). The results suggested that re-experiencing may be psychologically adaptive for survivors. With this knowledge, the need to foster a line of open communication with family, friends, other survivors, or healthcare providers to discuss fears, worries, or concerns can help enhance understanding of the diagnosis and lead to positive outcomes in life after cancer (Zebrack et al., 2015).
Similarly, six months after completing treatment, survivors aged 11–21 years from three different pediatric cancer centers reported PTG (Arpawong, Oland, Milam, Ruccione, & Meeske, 2013). PTG was positively associated with higher psychosocial functioning and PTSSs. Physical functioning and depressive symptoms were found to be inversely associated and, therefore, counterproductive in PTG (Arpawong et al., 2013).
Although providers may observe PTG in adolescents as clinically significant, a provider must understand that high levels of PTG are independent of distress (Arpawong et al., 2013; Smith et al., 2014). The presence of psychosocial distress is not entirely avoidable because positive and negative outcomes occur in the adjustment to cancer (Arpawong et al., 2013). Survivors who experience substantial PTG also may be highly distressed (Smith et al., 2014). Therefore, screening for PTSSs is critical, independent of the identified growth.
Role of the Advanced Practice Nurse
Clinical
Providers can best address unmet needs of ACSs by determining and assessing their risk. Proactive care includes a plan for prevention and guidance based on risks associated with ACSs (McCabe et al., 2013). Many ACSs are lost to follow-up when services with their interprofessional oncology team are discontinued because of age (McCabe et al., 2013). Patients should continue to be followed into adulthood by an interprofessional team, including an oncology advanced practice nurse (APN), who is in the best position to evaluate coping and psychological status. APNs should be aware of adolescent adherence to care throughout the transition into adult survivorship.
Regarding counseling, APNs should focus on evidence about adolescent coping strategies. Studies show that cognitive strategies are associated with psychological distress (Wenninger et al., 2013). More specifically, mental health counseling should address the lack of positive future expectations and avoidance of negative thoughts for patients suffering from psychological distress (Wenninger et al., 2013). Healthcare providers should encourage ACSs to use less avoidant coping strategies and instead strengthen coping acceptance strategies (Turner-Sack et al., 2012). ACSs who are more susceptible to relapse use more acceptance coping strategies and, therefore, are more likely to have high PTG (Turner-Sack et al., 2012).
APNs can advocate for their patients by securing health insurance and access to care. The socioeconomic impact of cancer on ACSs is considerable (Zebrack & Isaacson, 2012). As adults, ACSs have been reported to be six times more likely than siblings to report health-related unemployment and almost twice as likely to be unemployed but actively seeking work (Zebrack & Isaacson, 2012). ACSs in the United States are more likely to be uninsured as adults compared to other age groups (Zebrack & Isaacson, 2012). ACSs’ higher risk for unemployment contributes to a higher risk for lacking health insurance, limiting access to appropriate follow-up care. Advocacy does not stop at guaranteeing proper insurance for this patient population but can continue in the form of policy and institutional changes, as identified in Figure 1. 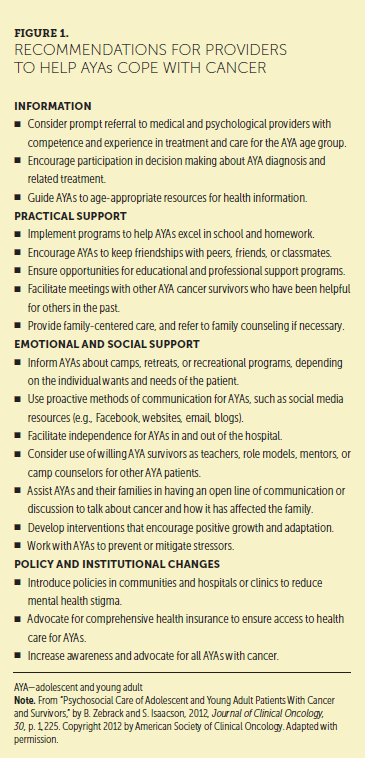
Education
For many ACSs, a cancer diagnosis may be their first experience with a life-threatening illness and, therefore, their first encounter with the world of health care. Patient education should be age-appropriate. Resources for ACSs stress a sense of normalcy (D’Agostino et al., 2011). Figure 2 provides a list of appropriate resources specific to ACSs. Providers can use the Internet as a source of information because younger patients with cancer are more likely to access the Internet for information compared to older adult patients with cancer (D’Agostino et al., 2011). Although a multitude of educational materials can help adolescent patients with cancer navigate their diagnosis and treatment, face-to-face contact with the healthcare team remains important (D’Agostino et al., 2011). Ultimately, the goal of care for ACSs is to encourage and help promote self-sustaining, independent, and proactive adolescents in society (D’Agostino et al., 2011). 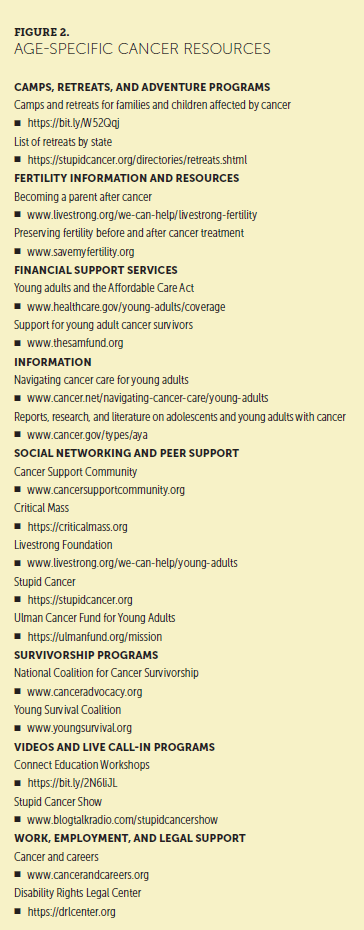
Childhood camps specifically for ACSs give continuous social and emotional support and access to information (Beckwitt, 2014). Themes of cancer camps include normalcy, meaningful camp experiences, and access to resources (Beckwitt, 2014). Recommendations to promote the abilities of ACSs to cope with cancer include information, practical support, emotional and social support, and policy and institutional changes.
Research
Despite studies acknowledging PTSD and PTSSs in ACSs following cancer remission, a small number of studies have explored the prevalence and predictors of distress and mental health issues in this population (Kwak et al., 2013). Future research should examine the etiology of prevalence and predictors of PTSD and PTSSs and how it affects the road to recovery and the stability of ACSs in the long-term. Monitoring the developmental course of specific comorbid symptoms (e.g., the effects of central nervous system tumors) can help introduce individualized therapy and improve functional outcomes to ultimately reduce the long-term impact for ACSs (Brinkman et al., 2016). Future research should identify and implement clinical steps to help transition ACSs to experience higher levels of PTG and continue to investigate individual attributes that explain PTG after cancer remission (Smith et al., 2014). 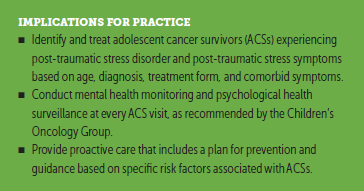
Conclusion
COG guidelines recommend mental health monitoring and psychological surveillance for all ACSs at every visit. A subset of ACSs reports clinically significant mental health difficulties, including PTSD and PTSSs after being diagnosed with cancer. As providers, involving ACSs in their health care, encouraging self-reliance, and promoting autonomy can lead to positive mental health. Advocacy for ACSs in the hospital and clinic settings sets the stage for further outreach and collaboration between provider entities. Psychological screenings with links to appropriate health services are essential in supporting vulnerable ACSs in this developmental chapter and their transition to adulthood. 
About the Author(s)
Brianna I. Katzman, BSN, RN, MSN, CPNP, is a pediatric nurse practitioner and Rita John, EdD, DNP, CPNP, PMHS, FAANP, is an associate professor, both in the School of Nursing at Columbia University in New York, NY. The authors take full responsibility for this content and did not receive honoraria or disclose any relevant financial relationships. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Katzman can be reached at bkatzman8@gmail.com, with copy to CJONEditor@ons.org. (Submitted February 2018. Accepted March 25, 2018.)
References
American Academy of Pediatrics. (2010). Supplemental appendix s12: Mental health screening and assessment tools for primary care. Retrieved from http://pediatrics.aappublications.org/content/125/Supplement_3/S173.ful…
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Arpawong, T.E., Oland, A., Milam, J.E., Ruccione, K., & Meeske, K.A. (2013). Post-traumatic growth among an ethnically diverse sample of adolescent and young adult cancer survivors. Psycho-Oncology, 22, 2235–2244. https://doi.org/10.1002/pon.3286
Beckwitt, A.E. (2014). Childhood cancer camps: Their role in adults surviving childhood cancers lives. Journal of Pediatric Oncology Nursing, 31, 34–40. https://doi.org/10.1177/1043454213515335
Bellizzi, K.M., Smith, A., Schmidt, S., Keegan, T.H., Zebrack, B., Lynch, C.F., . . . Simon, M. (2012). Positive and negative psychosocial impact of being diagnosed with cancer as an adolescent or young adult. Cancer, 118, 5155–5162. https://doi.org/10.1002/cncr.27512
Brinkman, T.M., Li, C., Vannatta, K., Marchak, J.G., Lai, J.S., Prasad, P.K., . . . Krull, K.R. (2016). Behavioral, social, and emotional symptom comorbidities and profiles in adolescent survivors of childhood cancer: A report from the childhood cancer survivor study. Journal of Clinical Oncology, 34, 3417–3425. https://doi.org/10.1200/jco.2016.66.4789
Brinkman, T.M., Zhu, L., Zeltzer, L.K., Recklitis, C.J., Kimberg, C., Zhang, N., . . . Krull, K.R. (2013). Longitudinal patterns of psychological distress in adult survivors of childhood cancer. British Journal of Cancer, 109, 1373–1381. https://doi.org/10.1038/bjc.2013.428
Children’s Oncology Group. (2013). Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancer [v.4.0]. Retrieved from http://www.survivorshipguidelines.org/pdf/LTFUGuidelines_40.pdf
D’Agostino, N.M., Penney, A., & Zebrack, B. (2011). Providing developmentally appropriate psychosocial care to adolescent and young adult cancer survivors. Cancer, 117, 2329–2334. https://doi.org/10.1002/cncr.26043
Hahn, E.E., Hays, R.D., Kahn, K.L., Litwin, M.S., & Ganz, P.A. (2015). Post-traumatic stress symptoms in cancer survivors: Relationship to the impact of cancer scale and other associated risk factors. Psycho-Oncology, 24, 643–652. https://doi.org/10.1002/pon.3623
John, R.M. (2017). Lecture on development and culture. Personal collection of R.M. John, Columbia University School of Nursing, New York, NY.
Kahalley, L.S., Wilson, S.J., Tyc, V.L., Conklin, H.M., Hudson, M.M., Wu, S., . . . Hinds, P.S. (2013). Are the psychological needs of adolescent survivors of pediatric cancer adequately identified and treated? Psycho-Oncology, 22, 447–458. https://doi.org/10.1002/pon.3021
Kazak, A.E., Derosa, B.W., Schwartz, L.A., Hobbie, W., Carlson, C., Ittenbach, R.F., . . . Ginsberg, J.P. (2010). Psychological outcomes and health beliefs in adolescent and young adult survivors of childhood cancer and controls. Journal of Clinical Oncology, 28, 2002–2007. https://doi.org/10.1200/jco.2009.25.9564
Kwak, M., Zebrack, B.J., Meeske, K.A., Embry, L., Aguilar, C., Block, R., . . . Cole, S. (2013). Prevalence and predictors of post-traumatic stress symptoms in adolescent and young adult cancer survivors: A 1-year follow-up study. Psycho-Oncology, 22, 1798–1806. https://doi.org/10.1002/pon.3217
McCabe, M.S., Bhatia, S., Oeffinger, K.C., Reaman, G.H., Tyne, C., Wollins, D.S., & Hudson, M.M. (2013). American Society of Clinical Oncology statement: Achieving high-quality cancer survivorship care. Journal of Clinical Oncology, 31, 631–640. https://doi.org/10.1200/jco.2012.46.6854
Parks, E.P., Maqbool, A., Shaikhkhalil, A., Groleau, V., Dougherty, K.A., & Stallings, V.A. (2016). Developmental-behavioral screening and surveillance. In R.E. Behram (Ed.), Nelson textbook of pediatrics (20th ed., p. 90). Philadelphia, PA: Elsevier.
Phipps, S., Klosky, J.L., Long, A., Hudson, M.M., Huang, Q., Zhang, H., & Noll, R.B. (2014). Posttraumatic stress and psychological growth in children with cancer: Has the traumatic impact of cancer been overestimated? Journal of Clinical Oncology, 32, 641–646. https://doi.org/10.1200/jco.2013.49.8212
Recklitis, C.J., Diller, L.R., Li, X., Najita, J., Robison, L.L., & Zeltzer, L. (2010). Suicide ideation in adult survivors of childhood cancer: A report from the childhood cancer survivor study. Journal of Clinical Oncology, 28, 655–661. https://doi.org/10.1200/jco.2009.22.8635
Schwartz, L.A., Kazak, A.E., Derosa, B.W., Hocking, M.C., Hobbie, W.L., & Ginsberg, J.P. (2012). The role of beliefs in the relationship between health problems and posttraumatic stress in adolescent and young adult cancer survivors. Journal of Clinical Psychology in Medical Settings, 19, 138–146. https://doi.org/10.1007/s10880-011-9264-1
Schwartz, L.A., Mao, J.J., Derosa, B.W., Ginsberg, J.P., Hobbie, W.L., Carlson, C.A., . . . Kazak, A.E. (2010). Self-reported health problems of young adults in clinical settings: Survivors of childhood cancer and healthy controls. Journal of the American Board of Family Medicine, 23, 306–314. https://doi.org/10.3122/jabfm.2010.03.090215
Seitz, D.C., Besier, T., Debatin, K.M., Grabow, D., Dieluweit, U., Hinz, A., . . . Goldbeck, L. (2010). Posttraumatic stress, depression and anxiety among adult long-term survivors of cancer in adolescence. European Journal of Cancer, 46, 1596–1606. https://doi.org/10.1016/j.ejca.2010.03.001
Smith, S.K., Samsa, G., Ganz, P.A., & Zimmerman, S. (2014). Is there a relationship between posttraumatic stress and growth after a lymphoma diagnosis? Psycho-Oncology, 23, 315–321. https://doi.org/10.1002/pon.3419
Stuber, M.L., Meeske, K.A., Krull, K.R., Leisenring, W., Stratton, K., Kazak, A.E., . . . Zeltzer, K. (2010). Prevalence and predictors of posttraumatic stress disorder in adult survivors of childhood cancer. Pediatrics, 125, e1124–e1134. https://doi.org/10.1542/peds.2009-2308
Stuber, M.L., Meeske, K.A., Leisenring, W., Stratton, K., Zeltzer, L.K., Dawson, K., . . . Krull, K.R. (2011). Defining medical posttraumatic stress among young adult survivors in the childhood cancer survivor study. General Hospital Psychiatry, 33, 347–353.
Sumalla, E.C., Ochoa, C., & Blanco, I. (2009). Posttraumatic growth in cancer: Reality or illusion? Clinical Psychology Review, 29, 24–33. https://doi.org/10.1016/j.cpr.2008.09.006
Turner-Sack, A.M., Menna, R., Setchell, S.R., Maan, C., & Cataudella, D. (2012). Posttraumatic growth, coping strategies, and psychological distress in adolescent survivors of cancer. Journal of Pediatric Oncology Nursing, 29, 70–79. https://doi.org/10.1177/1043454212439472
Wenninger, K., Helmes, A., Bengel, J., Lauten, M., Völkel, S., & Niemeyer, C.M. (2013). Coping in long-term survivors of childhood cancer: Relations to psychological distress. Psycho-Oncology, 22, 854–861. https://doi.org/10.1002/pon.3073
Zebrack, B., & Isaacson, S. (2012). Psychosocial care of adolescent and young adult patients with cancer and survivors. Journal of Clinical Oncology, 30, 1221–1226. https://doi.org/10.1200/JCO.2011.39.5467
Zebrack, B., Kwak, M., Salsman, J., Cousino, M., Meeske, K., Aguilar, C., . . . Cole, S. (2015). The relationship between posttraumatic stress and posttraumatic growth among adolescent and young adult cancer (AYA) patients. Psycho-Oncology, 24, 162–168.
Zebrack, B.J., Block, R., Hayes-Lattin, B., Embry, L., Aguilar, C., Meeske, K.A., . . . Cole, S. (2013). Psychosocial service use and unmet need among recently diagnosed adolescent and young adult cancer patients. Cancer, 119, 201–214. https://doi.org/10.1002/cncr.27713




