How Do You Deal With Death and Dying?
Oncology nursing is a rewarding, challenging, and ever-changing specialty. Oncology affords the nurse an opportunity to care for individuals with unique, complex issues during his or her cancer journey. I assumed that, at some point, I would care for a patient who may not have a positive outcome. It became clear to me that I would be there during the dying process and, subsequently, face issues related to the death of a patient. I really thought I knew what I was getting into; however, I now understand that I was not sufficiently prepared.
Jump to a section
Oncology nursing is a rewarding, challenging, and ever-changing specialty. Oncology affords the nurse an opportunity to care for individuals with unique, complex issues during his or her cancer journey. I assumed that, at some point, I would care for a patient who may not have a positive outcome. It became clear to me that I would be there during the dying process and, subsequently, face issues related to the death of a patient. I really thought I knew what I was getting into; however, I now understand that I was not sufficiently prepared.
We learn to care for patients across their lifespan and learn the stages of death and dying in our curriculum. I still have them committed to memory: denial, anger, bargaining, depression, and acceptance. Psychology, human growth and development, and physiology courses were simply not adequate to prepare me for my first patient death. That first experience with death as a new oncology nurse was difficult and has stayed with me to this day.
I remember the patient’s name, his wife, and his family as if it were yesterday. My patient was suffering from graft-versus-host disease of the liver. The liver enzymes, total bilirubin, and ammonia levels were seemingly rising by the minute. The patient became very disoriented, drowsy, and increasingly confused. The clinical team and the family had made the difficult decision regarding the patient’s do-not-resuscitate order. I was youthful, naive, and eager to do everything I could for the patient to ensure his comfort. I was in the room with the family when the patient took his final breath, which was heartbreaking.
My peers walked me through the postmortem care procedures, documentation, and paperwork. They helped me care for the family as they grieved the loss of their loved one. I thought I had it under control, but the overwhelming feeling of sadness came over me when I least expected it. At that time, the institution did not have a significant support system available for nursing grief and loss. I relied on my more-experienced coworkers, who provided emotional support and shared their personal experiences with me. They reassured me that it was OK to take a moment to process the situation, encouraged me to discuss my feelings with them, and coached me on self-care.
Acknowledging your grief and identifying resources for support is important. Some healthcare organizations offer employee assistance programs with counseling services, pastoral care, and spiritual care for nurses. Special interventions and tools are available that can be used after a challenging or emotional situation to help restore emotional balance for the nurse. An example of this at my institution is the use of Code Lavender, a rapid-response service for well-being. Developed through a partnership between the Office of Patient Experience and the spiritual care chaplains, the Code Lavender team provides supportive, holistic services to help clinical team members, patients, and their family members during stressful events. Some of the holistic services include guided imagery, mind–body exercises, Reiki, and spiritual and emotional support. Once a Code Lavender is called, support services are available for 72 hours.
Several years ago, when I was managing an oncology infusion suite, we had a terminal patient who died in the ambulatory setting. This is extremely rare. The clinical team was shocked, and I called the Code Lavender team to assist. They came to the unit, met with the clinical team, and offered support to the patient’s family. The clinical team debriefed and paused collectively for a moment of silence to honor the patient. This brief, shared experience gave us the time to reflect and relieve stress.
In addition to personal self-care and post-crisis intervention, training resources are available to new and experienced nurses regarding end-of-life care. These resources can provide in-depth information on caring for patients at the end of life. I cannot say that dealing with the death of a patient gets easier over time, but the ability to cope and maintain self-care can be somewhat improved by seeking out and using available resources. 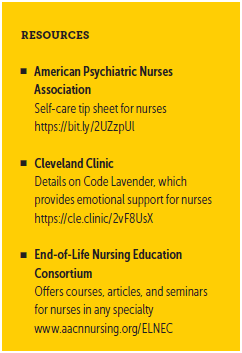
About the Author(s)
Georgina T. Rodgers, BSN, RN, OCN®, NE-BC, is the director of Clinical Cancer Services at the Cleveland Clinic Taussig Cancer Institute in Ohio. Rodgers can be reached at rodgersg@ccf.org, with copy to CJONEditor@ons.org.




