Compassion Fatigue and Satisfaction: Influence on Turnover Among Oncology Nurses at an Urban Cancer Center
Background: Oncology nurses are exposed to stressors that may contribute to compassion fatigue (CF), leading to high rates of turnover, potential financial implications for organizations, and concerns for patient safety and employee well-being.
Objectives: The purpose of this study was to explore the relationship among CF, compassion satisfaction (CS), and turnover intention in a sample of 93 inpatient oncology nurses at a 90-bed urban cancer center.
Methods: Data were collected using paper surveys. CS, secondary traumatic stress, and burnout were measured using the Professional Quality of Life–Version 5 scale, and turnover intention was determined using the Turnover Intention Scale–6.
Findings: Burnout and CS were found to be significantly predictive of turnover intention. Strategies to reduce CF individually and organizationally may improve patient and employee well-being.
Jump to a section
Oncology nurses spend significant amounts of time at the bedside of patients who are suffering, which increases their risk for developing compassion fatigue (CF) and decreases compassion satisfaction (CS). Joinson (1992) identified the concept of CF in her study regarding the decrease of nurturing ability in emergency department nurses (Zajac, Moran, & Groh, 2017). Although Joinson coined the term, the concept of CF was expanded on by Figley (2002), who defined it as the cost of caring and, more specifically, a combination of secondary traumatic stress and burnout. According to Figley (2002), secondary traumatic stress is defined as the stress of helping a traumatized or suffering individual. Figley (2002) also described burnout as the physical, emotional, and mental exhaustion caused by chronic involvement in burdensome situations.
Background
Using Figley’s (2002) definition of CF and its constructs, Stamm (2010) developed the Professional Quality of Life–Version 5 (ProQOL-V) CS-CF scale, which was a primary instrument for this study. According to Stamm (2010), professional quality of life is the quality that one perceives in his or her work as a helper, which incorporates components of CF (secondary traumatic stress and burnout). Stamm’s (2010) scale also includes the construct of CS, which is defined as positive feelings that one may have toward helping others.
A study by Wu, Singh-Carlson, Odell, Reynolds, and Su (2016) suggests that, while developing a rapport with patients and consequently developing an emotional involvement in their care, oncology nurses face immense emotional burdens, distress, and grief. Often, nurses experiencing CF tend to report physical symptoms, such as fatigue, muscle tension, headaches, emotional ability, anger, and poor judgment, which can potentially increase their use of sick days, create more situations where errors can occur, and decrease overall productivity (Adimando, 2018; Pfifferling & Gilley, 2000).
In addition, practicing mindfulness and prayer has shown to be efficacious in decreasing the effects of CF and increasing overall satisfaction among nurses (Duarte & Pinto-Gouveia, 2016; Kelly & Tyson, 2017). Mindfulness has also been linked to a reduction in burnout and a greater capacity for empathy (Kelly & Tyson, 2017). Previous studies indicate that nurses who exhibit high levels of resiliency tend to embody optimism, hopefulness, self-efficacy, and flexibility, and can cope more effectively with the symptoms of CF (Gentry, 2018; Rushton, Batcheller, Schroeder, & Donohue, 2015; Tubbert, 2016). According to Gentry (2018), seeking out mentorship, participating in counseling, openly expressing emotions, practicing self-care and assessment, obtaining adequate sleep and exercise, and talking with coworkers after difficult patient encounters are examples of behavioral patterns that have been shown to increase individual nurse resiliency. Therefore, adopting resiliency behaviors may be beneficial for nurses coping with CF.
Stressful work environments may be affected by factors within the organization as a whole rather than by individual influences (Jakimowicz, Perry, & Lewis, 2018; Kelly & Tyson, 2017). Potter et al. (2013) found that implementing a five-week program on resiliency training resulted in lower post-test CF scores, which was an unsurprising finding considering that previous research has shown that resilient nurses cope with CF better than their less resilient counterparts (Rushton et al., 2015; Tubbert, 2016). A study by Wahl, Hultguist, Struwe, and Moore (2018) revealed a statistically significant increase in nurses’ CS scores at post-test following a six-week resiliency training program on mindfulness, gratitude, and breath awareness strategies. In addition, implementing debriefing interventions after poor patient outcomes has been shown to promote group healing and increase morale and resiliency in nurses (Schmidt & Haglund, 2017). At the organizational level, implementation of mindfulness and resiliency training, as well as group debriefing sessions after difficult patient encounters, may be effective strategies to begin mitigating CF (Duarte & Pinto-Gouveia, 2016; Kelly & Tyson, 2017; Schmidt & Haglund, 2017; Wahl et al., 2018).
Turnover Intention
Across the United States, hospitals continue to face a nursing shortage, leading to increased costs for recruitment and the development of staff retention programs (Bakhamis, Paul, Smith, & Coustasse, 2019; Potter et al., 2010). According to Kelly, Baker, and Horton (2017), about 20% of new nurses leave their jobs within the first year of employment. The ongoing stress and feelings of burnout experienced by nurses can contribute to job dissatisfaction and increased turnover rates (Jakimowicz et al., 2018; Leiter & Maslach, 2009; Morrison & Korol, 2014; Russel, 2016). In addition to significant financial burdens for institutions, a high turnover rate raises concerns about the quality of patient care being provided (Leiter & Maslach, 2009; Luu & Hattrup, 2010; Zhang et al., 2014). Therefore, investing in strategies to mitigate CF may reduce turnover, limit organizational costs, and improve patient care (Kelly, Runge, & Spencer, 2015; Luu & Hattrup, 2010; Sung, Seo, & Kim, 2012).
The purpose of this article is to examine the relationships between CS and CF (e.g., secondary traumatic stress, burnout) and turnover intention among oncology nurses. The relationships among these three constructs, as well as the impact of overall experience with nursing and work experience specific to oncology on these relationships, and their influence on turnover intention are also assessed. Recommendations for additional research and interventions focused on decreasing and managing CF in oncology nurses are also suggested.
Methods
This cross-sectional self-report study was conducted at a 90-bed urban for-profit cancer center with four separate inpatient oncology units in the southern United States. Convenience sampling via paper surveys was used to collect data during a three-month period. During data collection, about 150 nurses worked in the inpatient oncology unit. Eligible nurses were working full-time, part-time, or per diem in acute care. Healthcare providers who were not RNs or float nurses were excluded from the sample. Because of contractual agreements with the cancer units, agency nurses were also included in the sample. Ninety-four oncology nurses completed the demographic survey and measurement scales; however, one respondent did not complete the survey on burnout completely and was dropped from the study. The final sample included 93 participants. The study was approved by the institutional review board at Belmont University.
Instruments and Measurements
Demographics, including age, gender, nursing unit, months of overall nursing experience, months of oncology nursing experience, and whether each nurse worked full-time, part-time, or per diem, were collected. The authors developed a survey using the ProQOL-V scale, the Turnover Intention Scale–6 (TIS-6), and some of the questions on the demographic questionnaire. The ProQOL-V is a self-report, 30-item, Likert-type scale with three subscales that assess CS and CF, secondary traumatic stress, and burnout. The ProQOL-V has been demonstrated to have satisfactory reliability and construct validity, with a Cronbach alpha ranging from 0.7 to 0.91 (Sacco, Ciurzynski, Harvey, & Ingersoll, 2015; Stamm, 2010). Of the 30 items, 10 items measure CS and CF, 10 items measure secondary traumatic stress, and 10 items measure burnout. Total scores range from 10 to 50 (22 or less = low, 23–41 = moderate, and 42 or greater = high).
Turnover intention was evaluated in this sample using the TIS-6. The TIS-6 displays satisfactory psychometric properties, with a Cronbach alpha of 0.8 (Bothma & Roodt, 2013). Each item is ranked on a five-point Likert-type scale. A score of 3 or greater indicates an intention to leave, whereas a score of less than 3 indicates an intention to stay. Scores for each item on the TIS-6 scale are totaled, with scores of 18 or greater indicating an intention to leave and scores less than 18 indicating an intention to stay.
Statistical Analysis
A bivariate correlation analysis and a stepwise multivariate linear regression analysis (Cronbach alpha = 0.05) were conducted using IBM SPSS Statistics, version 24.0. Power and sample size were assessed a priori using G*Power, version 3.1, to determine the required sample size. The calculated sample size was 92 (F2 = 0.125, p = 0.8).
Results
Of 150 eligible nurses, 93 completed the survey (overall response rate of 62%). The sample was predominantly women (n = 85) who were employed full-time (n = 79). Demographic characteristics can be found in Table 1. 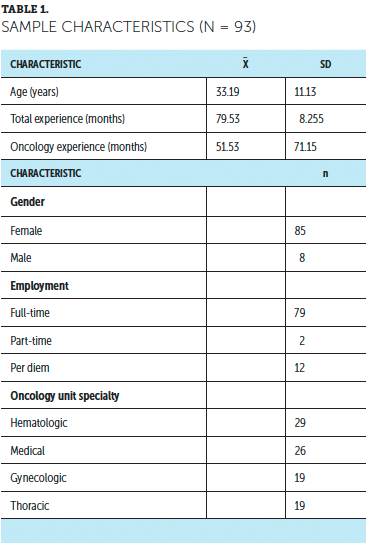
About half of the nurses (n = 47) in this sample exhibited average levels of satisfaction, with total scores ranging from 23 to 41. Forty-five nurses exhibited high levels of satisfaction (scores greater than or equal to 42). Only one participant exhibited a low level of satisfaction (score lower than or equal to 22). The mean raw satisfaction score for the sample was 40.12 (SD = 6.21). Fifty-six participants exhibited low levels of secondary traumatic stress (scores less than or equal to 22), and 37 participants exhibited average levels of secondary traumatic stress, with scores ranging from 23 to 41. No participants exhibited high levels of secondary traumatic stress (score greater than or equal to 42). The average raw score for secondary traumatic stress was 21.93 (SD = 5.26). Thirty-eight participants exhibited low levels of burnout (score less than or equal to 22), and 55 participants exhibited average levels of burnout, with scores ranging from 23 to 41. No participants exhibited high levels of burnout (score greater than or equal to 42). The average raw score for burnout was 23.72 (SD = 5.09).
An examination of the correlations of the dependent and independent variables was conducted (see Table 2). CS negatively correlated with the two dimensions of CF: secondary traumatic stress (r = –0.299) and burnout (r = –0.681). Secondary traumatic stress and burnout were positively correlated (r = 0.577). Total months of nursing experience was not significantly correlated to burnout (r = –0.026, p = 0.808) or secondary traumatic stress (r = 0.004, p = 0.973). Total months of oncology nursing experience was also not significantly correlated to burnout (r = –0.116, p = 0.267) or secondary traumatic stress (r = 0.044, p = 0.677). 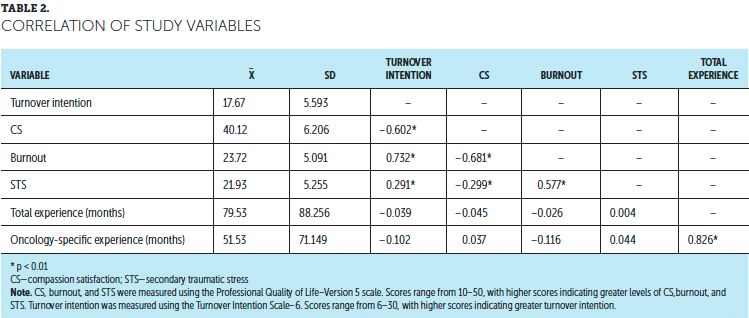
A stepwise linear regression model was constructed and executed to assess the impact of CS, secondary traumatic stress, and burnout on turnover intention (see Table 3). Because secondary traumatic stress and burnout were so highly correlated (r = 0.577), the stepwise entry of the independent variables was performed (Hair, Black, Babin, Anderson, & Tatham, 2006). CS was the first variable entered into the equation, followed by secondary traumatic stress and burnout. Secondary traumatic stress was not significant (beta = 0.13, p = 0.164) and was removed from the model. The final results of the regression analysis indicated significant relationships (F[2, 90] = 58.425, p < 0.001, r2 = 0.555). CS (beta = –0.234, p = 0.016) and burnout (beta = 0.573, p < 0.001) were also significant predictors of turnover intention. The coefficient of CS negatively indicated a significant protective influence against turnover intention. All variance inflation factors in both regression models were below 2.6. 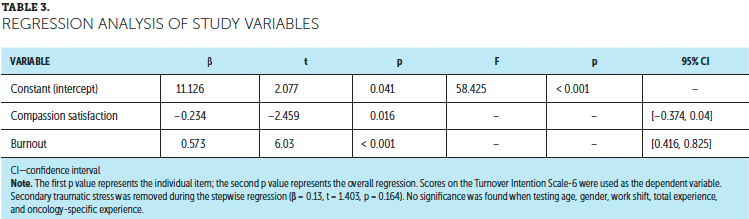
Discussion
Because oncology nurses care for patients with cancer and offer support to families coping with emotionally and physically burdensome illnesses, they are consistently exposed to a variety of stressors and execute decision making in ethically complex situations (Cañadas-De la Fuente et al., 2017). This environment places oncology nurses at a higher risk for developing burnout and subsequently leaving their job (Aycock and Boyle, 2009; Gentry, 2018; Scanlan & Still, 2019; Wu et al., 2016). The results of this study indicate that burnout significantly predicts turnover intention, which is consistent with the results of previous studies (Austin, Saylor, & Finley, 2017; Leiter & Maslach, 2009; Perry, Toffner, Merrick, & Dalton, 2011; Scanlan & Still, 2019; Sung et al., 2012; Zhang et al., 2014). Previous studies have shown that nurses who experience secondary traumatic stress have higher levels of turnover intention (Austin et al., 2017; Leiter & Maslach, 2009; Perry et al., 2011; Scanlan & Still, 2019; Sung et al., 2012; Zhang et al., 2014). However, the results of this study did not indicate that secondary traumatic stress is significantly predictive of turnover intention. Although secondary traumatic stress was not significantly predictive in this sample, the results do reveal a correlation supporting the belief that nurses with higher stress scores also have higher turnover intention scores. In addition, compassion satisfaction indicated a significant lack of turnover intention in this sample, which is consistent with results reported in previous studies (Jakimowicz et al., 2018; Kelly et al., 2015).
Overall, nurses who reported higher scores on the burnout ProQOL-V subscale also had higher secondary traumatic stress and turnover intention scores on the TIS-6. In contrast, nurses who had higher satisfaction scores reported lower scores on the secondary traumatic stress and burnout subscales and had lower turnover intention, indicating that nurses who experience greater satisfaction in their caregiving role will likely experience less feelings of burnout and stress and have less desire to leave their place of employment.
Although the results of this study are similar to those reported in the literature, some differences were determined. In this study, demographics, such as age, gender, and experience, did not have significant relationships with CS, secondary traumatic stress, or burnout. Other studies reported no significant relationships between age and CF (Frey, Robinson, Wong, & Gott, 2018; Kelly & Lefton, 2017); however, prior studies found that more months of nursing experience were significantly predictive of CF (Kelly et al., 2015; Wijdenes, Badger, & Sheppard, 2019). The generalizability of the study results are concerning because of the large percentage of inexperienced nurses, which could also explain the lack of significance between experience and CF in this sample.
Limitations
Although the sample size (N = 93) was moderate, this study was limited by its cross-sectional design and its use of convenience sampling. The design of this study precludes an evaluation of temporal precedence and causality of the observed associations among CF and satisfaction and secondary traumatic stress and burnout. Because of the homogeneity of the sample, generalizability is limited. Future studies should include more diverse demographics (age and experience levels) across multiple locations. In addition, this study only used the ProQOL-V scale to measure CF, whereas other studies may include tools that measure additional influential factors, such as job satisfaction.
Implications for Nursing
CF has commonly been associated with increased turnover intention and, therefore, holds financial implications for healthcare organizations (Kelly et al., 2015; Roney & Acri, 2018; Wijdenes et al., 2019). According to Nursing Solutions (2019), the turnover rate for bedside nurses is 19.1%, which significantly affects operational costs for hospitals in the United States. The average cost of turnover for a bedside nurse is $52,100, resulting in an average-sized hospital losing an average of $4.4–$6.9 million per year (Nursing Solutions, 2019). Although high clinical staff turnover is a well-recognized problem in health care, 81% of hospitals do not track clinical staff turnover costs regularly (Nursing Solutions, 2019). These statistics indicate a need for healthcare organizations to implement strategies that promote nurse retention. Interventions aimed at the prevention of secondary traumatic stress and burnout in bedside nurses can be a starting point for strategy development.
CF also has implications for patient safety (Kelly et al., 2015; Lumpkin, 2014; Wijdenes et al., 2019). Nurses who suffer from CF are more likely to struggle to show empathy for their patients, thereby reducing the overall effectiveness of their care (Christodoulou-Fella, Middleton, Papathanassoglou, & Karanikola, 2017). In addition, CF has been associated with an increase in medical errors (Kelly & Tyson, 2017; Tawfik et al., 2017; Wijdenes et al., 2019). Nurses experiencing CF have also been reported as having low patient safety standards and productivity in the workplace (Branch & Klinkenberg, 2015; Christodoulou-Fella et al., 2017). These findings suggest that the quality of patient care can be compromised when nurses are experiencing CF. It may be beneficial for healthcare organizations to explore the patient safety concerns associated with CF so that policies and procedures to limit its effects on nurses can be implemented.
CF can also compromise the safety of nurses on an individual level by causing physical and emotional side effects (Lumpkin, 2014; Matey, 2016). Physically, CF can manifest as an increase in somatic complaints, such as headache, sleep disturbance, concentration issues, and fatigue. These physical symptoms can contribute to increased absences and medical errors and decreased productivity (Adimando, 2018). According to Hegney et al. (2014), secondary traumatic stress and burnout are significantly predictive of psychological symptoms in nurses, such as anxiety, stress, and depression, suggesting that nurses experiencing CF are at an increased risk for developing anxiety and depression.
When examining the influence of CF on turnover intention, it is also important for healthcare organizations to develop interventions to reduce CF in nurses, which can lead to improvements in costs, patient safety, and overall employee well-being. The results of this study support the findings of other studies that suggest that efforts to mitigate the effects of CF are beneficial in multiple dimensions, such as nurse well-being and retention, which can save costs for healthcare organizations (Duarte & Pinto-Gouveia, 2016; Potter et al., 2013; Rushton et al., 2015; Tubbert, 2016). Although additional studies on the efficacy of interventions and recommendations for mitigating CF are needed, implementing mindfulness and resiliency training, as well as providing routine debriefing sessions for nurses, can be a starting point in addressing the complexity of CF (Duarte & Pinto-Gouveia, 2016; Kelly & Tyson, 2017; Rushton et al., 2015; Schmidt & Haglund, 2017; Tubbert, 2016). 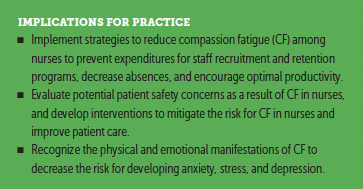
Conclusion
CF can contribute to turnover intention among oncology nurses, increase financial issues for healthcare organizations, and create safety concerns for patients and nurses. Addressing CF interprofessionally can improve understanding of the factors that lead to its development. In addition, recognition of the implications of CF and proactive implementation of strategies to mitigate the emotional and physical stressors associated with the nursing profession can be beneficial for institutions and nurses alike. Additional multisite studies are warranted to further explore the contributing factors of CF and its influence on turnover intention, as well as to establish effective interventions to alleviate CF among nurses. Implementing mindfulness and resiliency training, as well as offering regular debriefing opportunities for nurses after difficult patient encounters, is recommended to address CF issues among oncology nurses. [[{"fid":"53216","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
About the Author(s)
Diana Wells-English, DNP, FNP-BC, is an adjunct professor, and Jeannie Giese, DNP, FNP-BC, is an assistant professor, both in the School of Nursing at Belmont University in Nashville, TN; and Joseph Price, PhD, is a principal consultant at JPriceAnalytics in Brentwood, TN. The authors take full responsibility for this content and did not receive honoraria or disclose any relevant financial relationships. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Wells-English can be reached at dianawellsenglish@gmail.com, with copy to CJONEditor@ons.org. (Submitted December 2018. Accepted April 23, 2019.)
References
Adimando, A. (2018). Preventing and alleviating compassion fatigue through self-care: An educational workshop for nurses. Journal of Holistic Nursing, 36, 304–317. https://doi.org/10.1177/0898010117721581
Austin, C.L., Saylor, R., & Finley, P.J. (2017). Moral distress in physicians and nurses: Impact on professional quality of life and turnover. Psychological Trauma, 9, 399–406. https://doi.org/10.1037/tra0000201
Aycock, N., & Boyle, D. (2009). Interventions to manage compassion fatigue in oncology nursing. Clinical Journal of Oncology Nursing, 13, 183–191. https://doi.org/10.1188/09.CJON.183-191
Bakhamis, L., Paul, D.P., III, Smith, H., & Coustasse, A. (2019). Still an epidemic: The burnout syndrome in hospital registered nurses. Health Care Manager, 38, 3–10. https://doi.org/10.1097/HCM.0000000000000243
Bothma, C.F.C., & Roodt, G. (2013). The validation of the Turnover Intention Scale. SA Journal of Human Resource Management, 11, 1–12. https://doi.org/10.4102/sajhrm.v11.i1.507
Branch, C., & Klinkenberg, D. (2015). Compassion fatigue among pediatric healthcare providers. Maternal Child Nursing, 40, 160–165. https://doi.org/10.1097/NMC.0000000000000133
Cañadas-De la Fuente, G.A., Gómez-Urquiza, J.L., Ortega-Campos, E.M., Cañadas, G.R., Albendín-García, L., & De la Fuente-Solana, E.I. (2017). Prevalence of burnout syndrome in oncology nursing: A meta analytic study. Psycho-Oncology, 27, 1426–1433. https://doi.org/10.1002/pon.4632
Christodoulou-Fella, M., Middleton, N., Papathanassoglou, E.D.E., & Karanikola, M.N.K. (2017). Exploration of the association between nurses’ moral distress and secondary traumatic stress syndrome: Implications for patient safety in mental health services. BioMed Research International, 1908712. https://doi.org/10.1155/2017/1908712
Duarte, J., & Pinto-Gouveia, J. (2016). Effectiveness of mindfulness-based intervention on oncology nurses’ burnout and compassion fatigue symptoms: A non-randomized study. International Journal of Nursing Studies, 64, 98–107. https://doi.org/10.1016/j.ijnurstu.2016.10.002
Figley, C.R. (Ed.) (2002). Treating compassion fatigue. New York, NY: Brunner-Routledge.
Frey, R., Robinson, J., Wong, C., & Gott, M. (2018). Burnout, compassion fatigue and psychological capital: Findings from a survey of nurses delivering palliative care. Applied Nursing Research, 43, 1–9. https://doi.org/10.1016/j.apnr.2018.06.003
Gentry, E. (2018). Fighting compassion fatigue and burnout by building emotional resilience. Journal of Oncology Navigation and Survivorship, 9, 12.
Hair, J.F., Black, W.C., Babin, B.J., Anderson, R.E., & Tatham, R.L. (2006). Multivariate data analysis (6th ed.). Upper Saddle River, NJ: Pearson-Prentice Hall.
Hegney, D.G., Craigie, M., Hemsworth, D., Osseiran-Moisson, R., Aoun, S., Francis, K., & Drury, V. (2014). Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: Study 1 results. Journal of Nursing Management, 22, 506–518. https://doi.org/10.1111/jonm.12160
Jakimowicz, S., Perry, L., & Lewis, J. (2018). Compassion satisfaction and fatigue: A cross sectional survey of Australian intensive care nurses. Australian Critical Care, 31, 396–405. https://doi.org/10.1016/j.aucc.2017.10.003
Joinson, C. (1992). Coping with compassion fatigue. Nursing, 22, 116–121.
Kelly, L.A., Baker, M.E., & Horton, K.L. (2017). Code compassion: A caring fatigue reduction intervention. Nursing Management, 48(5), 18–22. https://doi.org/10.1097/01.NUMA.0000515800.02592.d4
Kelly, L.A., & Lefton, C. (2017). Effect of meaningful recognition on critical care nurses’ compassion fatigue. American Journal of Critical Care, 26, 438–444. https://doi.org/10.4037/ajcc2017471
Kelly, L., Runge, J., & Spencer, C. (2015). Predictors of compassion fatigue and compassion satisfaction in acute care nurses. Journal of Nursing Scholarship, 47, 522–528. https://doi.org/10.1111/jnu.12162
Kelly, M., & Tyson M. (2017). Can mindfulness be an effective tool in reducing stress and burnout, while enhancing self-compassion and empathy in nursing? Mental Health Nursing, 36, 12–17.
Leiter, M.P., & Maslach, C. (2009). Nurse turnover: The mediating role of burnout. Journal of Nursing Management, 17, 331–339. https://doi.org/0.1111/j.1365-2834.200901004.x
Lumpkin, E. (2014). Educating oncology nurses on compassion fatigue. Journal of Gynecologic Oncologic Nursing, 24(2), 4–7.
Luu, L., & Hattrup, K. (2010). An investigation of country differences in the relationship between job satisfaction and turnover intentions. Applied H.R.M. Research, 12, 17–39.
Matey, L. (2016). Compassion fatigue is a safety concern. ONS Connect, 31, 20.
Morrison, K.B., & Korol, S.A. (2014). Nurses’ perceived and actual caregiving roles: Identifying factors that can contribute to job satisfaction. Journal of Clinical Nursing, 23, 3468–3477. https://doi.org/10.1111/jocn.12597
Nursing Solutions. (2019). 2019 national healthcare retention and RN staffing report. Retrieved from http://www.nsinursingsolutions.com/Files/assets/library/retention-insti…
Perry, B., Toffner, G., Merrick, T., & Dalton. J. (2011). An exploration of the experience of compassion fatigue in clinical oncology nurses. Canadian Oncology Nursing Journal, 21, 95–105.
Pfifferling, J.H., & Gilley, K. (2000). Overcoming compassion fatigue. Family Practice Management, 7, 39–44. Retrieved from http://www.aafp.org/fpm/20000400/39over.html
Potter, P., Deshields, T., Berger, J.A., Clarke, M., Olsen, S., & Chen, L. (2013). Evaluation of a compassion fatigue resiliency program for oncology nurses. Oncology Nursing Forum, 40, 180–187. https://doi.org/0.1188/13.ONF.180-187
Potter, P., Deshields, T., Divanbeigi, J., Berger, J., Cipriano, D., Norris, L., & Olsen, S. (2010). Compassion fatigue and burnout: Prevalence among oncology nurses [Online exclusive]. Clinical Journal of Oncology Nursing, 14, E56–E62. https://doi.org/10.1188/10.CJON.E56-E62
Roney, L.N., & Acri, M.C. (2018). The cost of caring: An exploration of compassion fatigue, compassion satisfaction, and job satisfaction in pediatric nurses. Journal of Pediatric Nursing, 40, 74–80. https://doi.org/10.1016/j.pedn.201801.016
Rushton, C.H., Batcheller, J., Schroeder, K., & Donohue, P. (2015). Burnout and resilience among nurses practicing in high-intensity settings. American Journal of Critical Care, 24, 412–421. https://doi.org/10.4037/ajcc2015291
Russell, K. (2016). Perceptions of burnout, its prevention, and its effect on patient care as described by oncology nurses in the hospital setting. Oncology Nursing Forum, 43, 103–109. https://doi.org/10.1188/16.ONF.103-109
Sacco, T.L., Ciurzynski, S.M., Harvey, M.E., & Ingersoll, G.L. (2015). Compassion satisfaction and compassion fatigue among critical care nurses. Critical Care Nurse, 35, 32–43. https://doi.org/10.4037/ccn2015392
Scanlan, J.N., & Still, M. (2019). Relationships between burnout, turnover intention, job satisfaction, job demands and job resources for mental health personnel in an Australian mental health service. BMC Health Services Research, 19, 62. https://doi.org/10.1186/s12913-018-3841-z
Schmidt, M., & Haglund, K. (2017). Debrief in emergency departments to improve compassion fatigue and promote resiliency. Journal of Trauma Nursing, 24, 317–322. https://doi.org/10.1097/JTN.0000000000000315
Stamm, B.H. (2010). The concise ProQOL manual (2nd ed.). Pocatello, ID: ProQOL.org
Sung, K., Seo, Y., & Kim, J.H. (2012). Relationships between compassion fatigue, burnout, and turnover intention in Korean hospital nurses. Journal of Korean Academic Nursing, 42, 1087–1094. https://doi.org/10.4040/jkan.2012.42.7.1087
Tawfik, D.S., Sexton, J.B., Kan, P., Sharek, P.J., Nisbet, C.C., Rigdon, J., . . . Profit, J. (2017). Burnout in the neonatal intensive care unit and its relation to healthcare-associated infections. Journal of Perinatology, 37, 315–320. https://doi.org/10.1038/jp.2016.211
Tubbert, S.J. (2016). Resiliency in emergency nurses. Journal of Emergency Nursing, 42, 47–52. https://doi.org/10.1016/j.jen.2015.05.016
Wahl, C., Hultguist, T.B., Struwe, L., & Moore, J. (2018). Implementing a peer support network to promote compassion without fatigue. Journal of Nursing Administration, 48, 615–621. https://doi.org/10.1097/NNA.0000000000000691
Wijdenes, K.L., Badger, T.A., & Sheppard, K.G. (2019). Assessing compassion fatigue risk among nurses in a large urban trauma center. Journal of Nursing Administration, 49, 19–23. https://doi.org/10.1097/NNA.0000000000000702
Wu, S., Singh-Carlson, S., Odell, A., Reynolds, G., & Su, Y. (2016). Compassion fatigue, burnout, and compassion satisfaction among oncology nurses in the United States and Canada [Online exclusive]. Oncology Nursing Forum, 43, E161–E169. https://doi.org/10.1188/16.ONF.E161-E169
Zajac, L.M., Moran, K.J., & Groh, C.J. (2017). Confronting compassion fatigue: Assessment and intervention in inpatient oncology. Clinical Journal of Oncology Nursing, 21, 446–453. https://doi.org/10.1188/17.CJON.446-453
Zhang, L.F., You, L.M., Liu, K., Zheng, J., Fang, J.B., Lu, M.M., . . . Bu, X.Q. (2014). The association of Chinese hospital work environment with nurse burnout, job satisfaction, and intention to leave. Nursing Outlook, 62, 128–137. https://doi.org/10.1016/j.outlook.2013.10.010




