Fear of Cancer Progression: Findings From Case Studies and a Nurse-Led Intervention
Background: Fear of cancer recurrence or progression (FOP) is a significant concern for cancer survivors. With the advent of new targeted therapies and immunotherapy, many patients with advanced cancer are living longer while dealing with uncertainty and fears related to cancer progression. Although some level of FOP is normal and adaptive, high levels adversely affect quality of life and healthcare costs.
Objectives: This article describes a nurse-led intervention for managing FOP in two patients with advanced gynecologic cancer. The intervention teaches skills for managing worry, challenging unhelpful beliefs, and modifying unhelpful coping behaviors.
Methods: Preliminary findings from the two case studies are presented, including a comparison of post-treatment FOP scores to baseline scores.
Findings: The participants reported feeling more focused, less overwhelmed, and more in control of their worries. Both participants achieved statistically reliable improvements in FOP scores.
Jump to a section
Fear of cancer recurrence or progression (FOP) is the fear, worry, or concern about cancer returning or progressing (Lebel et al., 2016). Among cancer survivors, FOP is a prevalent unmet need associated with high levels of distress, anxiety, and depression (Sharpe et al., 2018; Thewes et al., 2014). About 49% of cancer survivors and as many as 70% of patients with advanced cancer experience moderate to high FOP (Butow et al., 2018), including intrusive thoughts, unhelpful coping behaviors, and difficulty making future plans (Lebel et al., 2016). Healthcare providers lack training in managing FOP (Butow et al., 2018). Providers may be unaware of FOP because patients may hesitate sharing their worries, particularly when family members are present (Economou & Reb, 2017). Nurses are well placed to discuss FOP with their patients (Dawson et al., 2016). This article describes a nurse-led intervention to manage FOP. Preliminary findings from two case studies are presented, including the change in FOP score from baseline to postintervention.
Background
FOP is a common reaction following an advanced cancer diagnosis (Ozga et al., 2015). Although some FOP is normal and even adaptive, some patients retain high FOP levels across time (Simard et al., 2013). Risk factors for clinically significant FOP include being newly diagnosed, being of a younger age, having cancer- or treatment-related side effects, and experiencing anxiety (Simard et al., 2013). FOP is problematic when poorly managed; high levels adversely affect quality of life (Lengacher et al., 2016; Tauber et al., 2019) and increase healthcare costs (Lebel et al., 2013). Patient behaviors include being hypervigilant about minor symptoms, requesting unnecessary tests, and constantly browsing the Internet for cancer-related information (Butow et al., 2018), which reinforces worry-driven behavior (Heathcote et al., 2018).
FOP may be an even greater concern in patients with advanced cancer (Lutgendorf et al., 2017; Mehnert et al., 2013). Targeted therapies and immunotherapies have increased patient survival. Treatment for extended durations and frequent monitoring contributes to FOP vulnerability (Thewes et al., 2017). Screening for FOP is not routinely done; however, screening for general distress is more common. FOP can be assessed by validated questionnaires with cutoff scores identifying those with dysfunctional FOP levels. Butow et al. (2018) suggest screening for FOP in clinical practice. According to a systematic review (Thewes et al., 2012), two measures are recommended: the Fear of Cancer Recurrence Inventory–Severity subscale (Simard & Savard, 2009) and the FOP Short Form (SF) questionnaire (Mehnert et al., 2006).
Nurses are well positioned to ask patients about FOP and about coping strategies they are using to manage their fears. One approach is to normalize FOP by asking if the patient feels that their worries are excessive, overwhelming, or interfering with their life (Butow et al., 2018).
Overview of Interventions
Two meta-analyses confirmed the overall efficacy of FOP interventions (Hall et al., 2018; Tauber et al., 2019). In a review of mind-body interventions by Hall et al. (2018), FOP trials were categorized as mindfulness-based (n = 3), cognitive-behavioral therapy (CBT) (n = 4), communication skills (n = 2), and a gratitude intervention (n = 1). At postintervention, small to medium effects were found (Hedges’ g = 0.36, p < 0.001). In Tauber et al. (2019), some studies used traditional CBT, in which the content of beliefs about FOP are challenged. Other studies used more contemporary CBT, where the process of worry and rumination are targeted, not thought content. Tauber et al. (2019) found that contemporary CBTs were more efficacious than traditional CBTs for FOP. However, several gaps in the studies were highlighted, including a focus on breast cancer and patients with early-stage disease. Most interventionists were psychologists. A report by Brebach et al. (2016) found that nurse-led FOP interventions have been effective, with uptake rates higher than non-nursing interventions. Training nurses to provide psychoeducational interventions is an efficient and cost-effective way to increase access to these services (McCarthy et al., 2018).
This article describes a nurse-led FOP intervention and preliminary findings from two patients with advanced gynecologic cancer. The Day-by-Day (DBD) intervention is adapted from Conquer Fear, an intervention found more efficacious than relaxation training in a large randomized trial of patients with early-stage cancer (Butow et al., 2017). Conquer Fear is based on a model that worry about cancer is normal, but some people have beliefs that worry is dangerous (i.e., the stress will bring the cancer back) or helpful (i.e., a recurrence will be identified more quickly). In addition, patients may become hypervigilant to physical sensations, which increases worry about recurrence (Sharpe et al., 2017). This FOP preoccupation makes it hard for people to engage in other life goals (Fardell et al., 2016). Using a case study approach, this article describes the intervention components and results.
Methods
Intervention Development
Adaptations to Conquer Fear were made to reflect the increased risk of recurrence among women with advanced gynecologic cancer and to shorten individual sessions to accommodate patients with advanced cancer. In addition, case studies, surveillance guidelines, and resources were revised to be relevant to advanced cancer; threat monitoring behaviors were revised to reflect unhelpful coping strategies exhibited by the patients; and more emphasis was placed on values-based goal setting.
Nurse Training Intervention
The study team, consisting of two advanced practice nurses (APNs) (interventionists), the principal investigator (PI), a psychologist, and a senior research coordinator (a certified health education specialist), participated in a two-day training workshop led by Louise Sharpe, PhD, one of the Conquer Fear developers. The intervention components were explained, and the goals and content of each session and key skills for managing FOP were reviewed. Role-play was used to practice these skills.
Patient Sample
Using a convenience sample, two patients with stage III or IV gynecologic cancer were recruited from the outpatient medical oncology clinic at a free-standing comprehensive cancer center in southern California. Patients were eligible if they were at least three months after initial diagnosis and had a score of 34 or greater on the FOP-SF (Mehnert et al., 2006) or 24 or greater on the Impact of Event Scale–Revised (Sundin & Horowitz, 2002). The Impact of Event Scale–Revised measures cancer-related distress. Items are categorized into three subscales: intrusion, avoidance, and hyperarousal. Scores range from 0 to 88, and a score of 24 or greater indicates significant distress (Sundin & Horowitz, 2002).
The DBD intervention included components from the Conquer Fear curriculum (Butow et al., 2013) including (a) comprehensive psychosocial assessment; (b) values-based goal setting exercise; (c) worry management skills; (d) challenging unhelpful beliefs about worry; (e) modifying threat monitoring behaviors; (f) educating patients about follow-up guidelines and healthy lifestyle behaviors, and (g) developing a relapse prevention plan. The goals were to identify triggers, teach skills for managing worries, and promote values-based goal setting (Smith et al., 2015). Unhelpful beliefs about worry frequently underlie excessive threat monitoring behaviors (Sharpe et al., 2019) (see Table 1). The intent was to help patients find a middle ground between vigilance and hypervigilance for recurrence symptoms. The skills addressed problematic metacognitions (i.e., beliefs about worry) and associated behaviors contributing to FOP. Experiential exercises and home practice were used to reinforce session content. 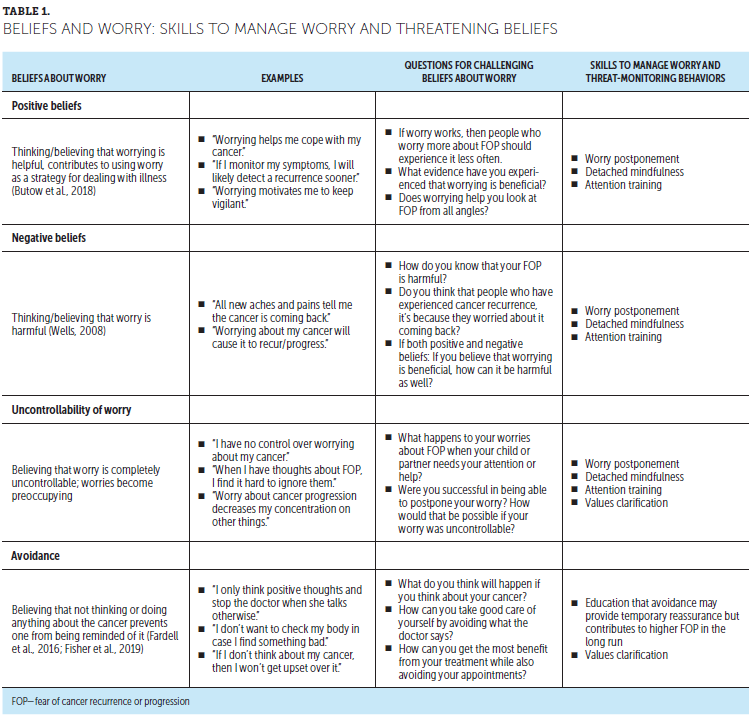
Procedures
FOP (DBD) Intervention Sessions: The intervention consisted of seven nurse-led, one-on-one sessions delivered during eight weeks (see Table 2). Patients were given videoconferencing instructions and emailed a session link for home participation. Session 1 consisted of a comprehensive psychosocial assessment, including prior losses and trauma, which can increase FOP. During session 2, patients reflected on how past experiences influenced their cancer response. Session 3 focused on values-based goal setting and attention training technique (ATT), which trains patients to focus their attention by noticing but not engaging in worrying thoughts (Butow et al., 2017) (see Table 3). Session 4 focused on other detached mindfulness and worry postponement skills. Detached mindfulness involves accepting one’s thoughts while relating to them in a detached way (Gu et al., 2016). Worry postponement helps to challenge unhelpful beliefs about the uncontrollability of worry. Sessions 5 and 6 focused on modifying threat-monitoring behaviors and challenging unhelpful beliefs about worries. The final session, session 7, summarized goal-setting progress and helped patients develop a response plan for worries or triggers. 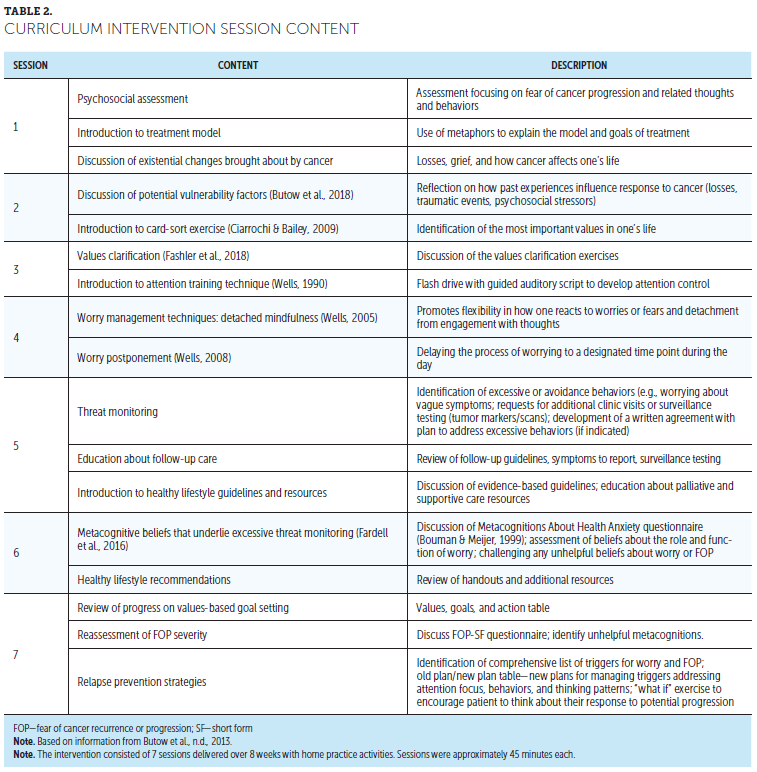
The APNs audiorecorded each session and completed session checklists to document covered content. During team meetings, the APNs reviewed cases with the PI and the team psychologist, who provided feedback on challenging cases. Patients completed the FOP-SF at baseline, 8 weeks, and 12 weeks. 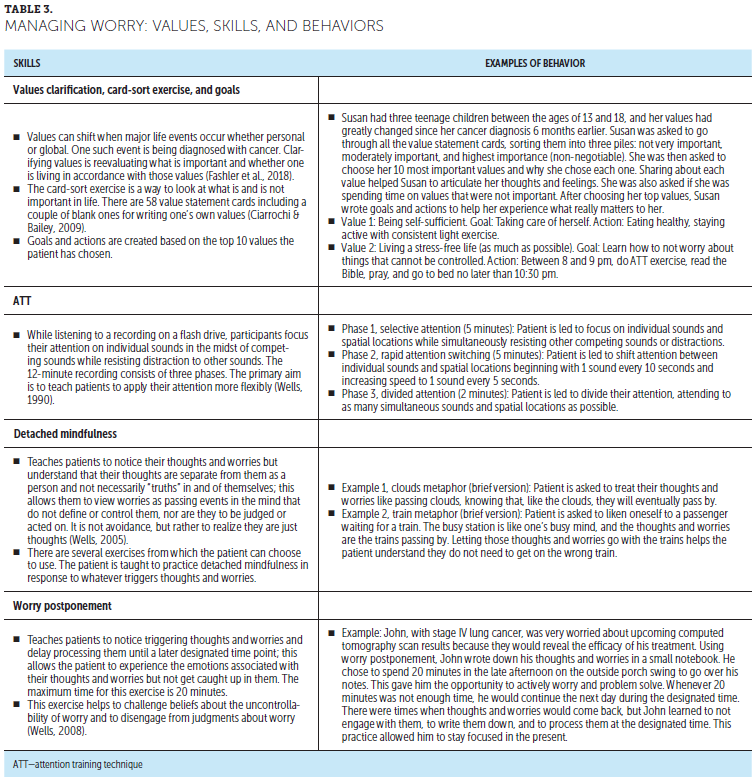
Measures
FOP was measured using the FOP-SF, with 12 items selected from the original 43-item questionnaire (FOP-Q) (Herschbach et al., 2005). Items are scored from 1 (never) to 5 (very often). Total scores ranged from 12 to 60; a cutoff score of 34 or greater indicates dysfunctional levels of FOP (Herschbach et al., 2010). The FOP-SF was comprehensively validated in a large sample of patients with breast cancer (Hinz et al., 2015; Mehnert et al., 2006).
Analysis
To determine if a meaningful change occurred between baseline and postintervention FOP scores, the Reliable Change Index (RCI) was calculated (Jacobson et al., 1984). The RCI indicates whether the patient has made a reliable symptom change over the course of treatment (Ferguson et al., 2002). To calculate the RCI, the difference in raw scores from baseline to postintervention is divided by the standard error of the differences between scores. A score greater than 1.96 shows a reliable change (Jacobson & Truax, 1991).
Findings
Case Study 1
Gail is a 50-year-old woman with recurrent BRCA1-positive stage IV ovarian cancer. A single mother with two grown children, Gail has a strong faith and social support system. Following the card-sort exercise (Ciarrochi & Bailey, 2009), Gail identifies healthy eating and independence as non-negotiable values. The APN helps Gail identify specific goals, including diet maintenance, walking more, and furthering her education. Gail states that she is constantly preoccupied with thoughts of recurrence. She frequently calls her nurse about her tumor marker results and experiences anxiety whenever scans are due. She frequently examines her breasts and scans her body for new pains that might represent a cancer recurrence. Gail experiences both positive and negative beliefs about worry, believing that being alert to and investigating new symptoms keeps her safe. Alternatively, she states that this worry will make her sick. Although Gail keeps busy to try to avoid cancer thoughts, she states that she experiences intrusive thoughts, making it difficult for her to concentrate. Although Gail initially remained preoccupied with recurrence, with ATT practice, she states that she feels less self-focused and more relaxed. The APN reviews detached mindfulness exercises. Gail states that the cloud metaphor was most helpful. Gail uses a journal to record her worries to reference during her worry time. She states that journaling helps her feel more in control over her worries, allowing her to attend to more meaningful events at other times. Gail also reviews previous responses to triggers and creates a new plan for managing unhelpful coping behaviors. The detached mindfulness and ATT skills helped her notice worrying thoughts but not get caught up in them. She calls less frequently and has cut back on the frequency of body scanning. Gail said she feels inspired by her progress and motivated to continue skills practice.
Analysis: Gail endorsed positive and negative beliefs about worry, distress around follow-up scans, and threat-monitoring behaviors, including frequent tumor marker inquiries and breast self-examinations. Her self-focused attention and intrusive thoughts interfered with her concentration. With skills practice, Gail reports less intrusive thoughts and threat-monitoring behaviors. She states that she feels calmer and more in control over her thoughts and worries.
At baseline, Gail had a clinically significant FOP level, as measured by the FOP-SF (Mehnert et al., 2006). The post-treatment FOP-SF score was compared with the baseline score using the RCI procedure (Jacobson & Truax, 1991) (see Table 4), and Gail’s FOP-SF score was significantly reduced, indicating that she had made a statistically reliable improvement (RCI = 4.35, p < 0.05). In addition, at eight weeks follow-up, Gail was in the normal FOP-SF score range. 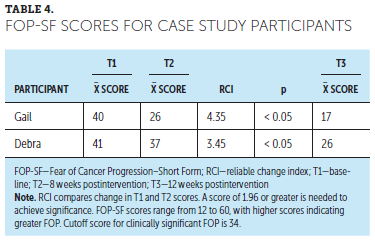
Case Study 2
Debra is a 65-year-old woman with stage III uterine cancer diagnosed two years prior. She completed neoadjuvant radiation therapy and chemotherapy, followed by surgery. Her husband recently died from colorectal cancer. Debra reveals she is most afraid of being alone and is depressed and lonely since her husband’s death. In the past, she had been active in her church but now finds it stressful. The APN discussed the impact of Debra’s grief and recent loss as contributing to her fears. Using the card-sort exercise, Debra states that her top values were her faith, having close relationships and feeling supported, and being there for her family. The nurse encourages Debra to set small but attainable goals consistent with her values and explores ways in which she might seek support. Debra agrees to set a monthly social activity goal, such as attending a book club and volunteering at church. Focusing on these goals helps Debra deal with her grief and fears.
Debra states that she has intrusive thoughts about the possibility of cancer progression. She is particularly fearful at night, which affects her sleep. Triggers for intrusive thoughts include concerns about her family and follow-up scans. Debra endorses negative beliefs about worry, expressing that she could make herself sick if she continues to worry. Although she said she tries to avoid these thoughts, she finds it difficult to control her worries. Although the ATT was challenging initially, with practice it helped Debra to focus her thinking. Debra reports that the cloud metaphor helped her to let go of worrying thoughts. Debra would go to her worry room around 4 pm to think about her concerns. Postponing worries helps her feel less overwhelmed and more in control of her thoughts. Both ATT and detached mindfulness skills help Debra break the worry cycle. Although she states that she has some residual fears at night, her sleep has become more restful. To manage triggers, Debra plans to use ATT to reinforce focused thinking as well as detached mindfulness and worry postponement to manage intrusive thoughts.
Analysis: Debra’s grief over the loss of her husband contributed to increased FOP. She endorsed mainly negative beliefs about worry. Although she tried to avoid negative thoughts, worry overwhelmed her. Debra did not exhibit threat monitoring behaviors, reassured by her close medical surveillance. However, her self-focused attention and intrusive thoughts interfered with her concentration and sleep. With skills practice, Debra learned to manage intrusive thoughts. Postintervention, she stated she felt calmer, more focused, and her sleep improved.
At baseline, Debra had a clinically significant FOP level, as measured by the FOP-SF (Mehnert et al., 2006). The post-treatment FOP-SF score was compared with a baseline score using the RCI procedure (Jacobson & Truax, 1991). Her FOP-SF score was significantly reduced, indicating that she had made a statistically reliable improvement (RCI = 3.45, p < 0.05). In addition, at 12 weeks follow-up, she was in the normal FOP-SF score range.
Discussion
FOP is a prevalent unmet need in patients with advanced cancer (Ozga et al., 2015; Sharpe et al., 2017). The findings from the case studies support the benefits of a nurse-led intervention to help patients manage FOP. The DBD intervention helps patients reflect on their most important values and targets unhelpful beliefs about worry and related coping behaviors. When confronted with a life-threatening illness, patients may lose sight of what gives their life meaning, spending time on less important activities. Helping patients reflect on their primary values provides direction and meaning in life (Fashler et al., 2018). Patients with FOP are often burdened with worry, which may underlie unhelpful coping behaviors. Some patients may avoid cancer reminders, increasing FOP (Fardell et al., 2016). Although frequent self-examination or requests for additional surveillance tests may provide temporary reassurance, these behaviors ultimately increase FOP (Butow et al., 2018). The DBD intervention teaches patients skills to manage intrusive thoughts and worries that they can use in their daily lives. The skills practice promotes focused attention, flexibility in response to worry, and thought detachment.
Nurses and other healthcare providers may not recognize FOP in patients or may be reluctant to discuss it (Curran et al., 2017; Thewes et al., 2014). These patients may be known to the clinical team because they call frequently with minor complaints or seek unnecessary tests for reassurance. Many providers are uncertain how to manage FOP (Thewes et al., 2014). Rather than ordering unnecessary tests, providers who carefully listen to the patient’s concerns and discuss the evidence-based rationale for surveillance decisions communicate understanding and confidence (Butow et al., 2018).
Lessons Learned
Based on the case studies describing the patients’ experience receiving the DBD intervention, patients requested more flexibility related to intervention sessions and practicing skills. One patient preferred phone delivery, whereas the other preferred in-person sessions. One patient found it difficult to access a computer to listen to the ATT flash drive during the day and suggested having a smartphone app. Although the patients found the card-sort exercise very helpful, they reported difficulty narrowing down their top values. The APNs learned to explain the goal of the value cards up front and ask patients to choose their top 10 non-negotiable values.
Implications for Nursing
This article describes a nurse-led intervention for managing FOP in patients with advanced gynecologic cancer. If patients are experiencing FOP, a nurse can encourage patients to express their fears. Nurses can assess how FOP affects the patient’s daily life, considering prior losses or trauma that may heighten FOP. By incorporating intervention techniques, nurses can help patients identify triggers, teach practical skills for managing triggers and worries, and challenge beliefs that contribute to unhelpful coping behaviors. The card-sort exercise can help patients identify their most important values and set goals aligned with those values. Teaching patients about recurrence symptoms, follow-up care, and healthy lifestyles equips them with ways to take control of their health.
Oncology nurses provide much of the emotional and psychosocial support for patients with advanced cancer and their family members (Wittenberg et al., 2018). APNs and many clinical nurses have expertise in managing symptoms and psychosocial concerns, but few have specific FOP training. Nurses are in a unique position to provide this care because they routinely interact with patients. With focused training, oncology nurses have successfully used CBT and related techniques (Melton, 2017; Zhang et al., 2018). Partnering with psychologists and social workers will help provide guidance to patients with more complex needs. Patients with preexisting mental health conditions or history of unresolved trauma may require specialized psychosocial treatment. 
Conclusion
FOP is a significant concern for patients with advanced cancer. This article highlights a nurse-led intervention for managing FOP. The case studies illustrate the intervention components, which teach skills for managing worry and help patients modify unhelpful coping behaviors. Skills include attention training, detached mindfulness, and worry postponement. After the intervention, patients reported feeling more focused and in control of their worries. Both achieved reliable improvements in FOP-SF scores.
About the Author(s)
Anne M. Reb, PhD, NP, is an assistant professor in the Beckman Research Institute, Tami Borneman, RN, MSN, CNS, FPCN, is a senior research specialist, and Denice Economou, RN, PhD, CHPN, is a senior research specialist, all in the Division of Nursing Research and Education, Marissa A. Cangin, PsyD, is an assistant clinical professor and licensed psychologist in the Department of Supportive Care Medicine, and Sunita K. Patel, PhD, is an associate professor in the Departments of Population Sciences and Supportive Care Medicine, all at City of Hope National Medical Center in Duarte, CA; and Louise Sharpe, PhD, is a professor of clinical psychology in the School of Psychology at the University of Sydney in New South Wales, Australia. The authors gratefully acknowledge the patients who generously contributed their time and supported this study. The authors also thank Nancy Guerrero-Llamas, MPH, CHES, for assistance with data management and adapting the intervention manual and patient workbook; Maribel Tejada, BS, for assistance with data management and technical support; and Betty Ferrell, PhD, and Judith Baggs, PhD, for review and comments on the manuscript. The authors take full responsibility for this content. This project is supported by the Palliative Care Research Cooperative Group funded by National Institute of Nursing Research (U2CNR014637). The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Reb can be reached at areb@coh.org, with copy to CJONEditor@ons.org. (Submitted July 2019. Accepted February 13, 2020.)
References
Bouman, T.K., & Meijer, K.J. (1999). A preliminary study of worry and metacognitions in hypochondriasis. Clinical Psychology and Psychotherapy, 6(2) 96–101. https://doi.org/ 10.1002/(sici)1099-0879(199905)6:2<96::Aid-cpp190>3.0.Co;2-g
Brebach, R., Sharpe, L., Costa, D.S.J., Rhodes, P., & Butow, P. (2016). Psychological intervention targeting distress for cancer patients: A meta-analytic study investigating uptake and adherence. Psycho-Oncology, 25(8), 882–890. https://doi.org/10.1002/pon.4099
Butow, P., Sharpe, L., Thewes, B., Turner, J., Gilchrist, J., & Beith, J. (2018). Fear of cancer recurrence: A practical guide for clinicians. Oncology, 32(1), 32–38.
Butow, P., Thewes, B., Gilchrist, J., Turner, J., & the Conquer Fear authorship group. (n.d.). A psychological and educational intervention for fear of cancer recurrence. Therapist Treatment Manual. Unpublished manuscript.
Butow, P.N., Bell, M.L., Smith, A.B., Fardell, J.E., Thewes, B., Turner, J., . . . Mihalopoulos, C. (2013). Conquer Fear: Protocol of a randomised controlled trial of a psychological intervention to reduce fear of cancer recurrence. BMC Cancer, 13, 201. https://doi.org/10.1186/1471-2407-13-201
Butow, P.N., Turner, J., Gilchrist, J., Sharpe, L., Smith, A.B., Fardell, J.E., . . . Thewes, B. (2017). Randomized trial of ConquerFear: A novel, theoretically based psychosocial intervention for fear of cancer recurrence. Journal of Clinical Oncology, 35(36), 4066–4077. https://doi.org/10.1200/JCO.2017.73.1257
Ciarrochi, J., & Bailey, A. (2009). A CBT-practitioner’s guide to ACT: How to bridge the gap between cognitive behavioral therapy and acceptance and commitment therapy. New Harbinger Publications.
Curran, L., Sharpe, L., & Butow, P. (2017). Anxiety in the context of cancer: A systematic review and development of an integrated model. Clinical Psychology Review, 56, 40–54. https://doi.org/10.1016/j.cpr.2017.06.003
Dawson, G., Madsen, L.T., & Dains, J.E. (2016). Interventions to manage uncertainty and fear of recurrence in female breast cancer survivors: A review of the literature. Clinical Journal of Oncology Nursing, 20(6), E155–E161. https://doi.org/10.1188/16.CJON.E155-E161
Economou, D., & Reb, A. (2017). Communication concerns when transitioning to cancer survivorship care. Seminars in Oncology Nursing, 33(5), 526–535. https://doi.org/10.1016/j.soncn.2017.10.001
Fardell, J.E., Thewes, B., Turner, J., Gilchrist, J., Sharpe, L., Smith, A.B., . . . Butow, P. (2016). Fear of cancer recurrence: A theoretical review and novel cognitive processing formulation. Journal of Cancer Survivorship, 10(4), 663–673. https://doi.org/10.1007/s11764-015-0512-5
Fashler, S.R., Weinrib, A.Z., Azam, M.A., & Katz, J. (2018). The use of acceptance and commitment therapy in oncology settings: A narrative review. Psychological Reports, 121(2), 229–252. https://doi.org/10.1177/0033294117726061
Ferguson, R.J., Robinson, A.B., & Splaine, M. (2002). Use of the Reliable Change Index to evaluate clinical significance in SF-36 outcomes. Quality of Life Research, 11(6), 509–516.
Fisher, P.L., Byrne, A., Fairburn, L., Ullmer, H., Abbey, G., & Salmon, P. (2019). Brief metacognitive therapy for emotional distress in adult cancer survivors. Frontiers in Psychology, 10, 162. https://doi.org/10.3389/fpsyg.2019.00162
Gu, J., Strauss, C., Crane, C., Barnhofer, T., Karl, A., Cavanagh, K., & Kuyken, W. (2016). Examining the factor structure of the 39-item and 15-item versions of the Five Facet Mindfulness Questionnaire before and after mindfulness-based cognitive therapy for people with recurrent depression. Psychological Assessment, 28(7), 791–802.
Hall, D.L., Luberto, C.M., Philpotts, L.L., Song, R., Park, E.R., & Yeh, G.Y. (2018). Mind-body interventions for fear of cancer recurrence: A systematic review and meta-analysis. Psycho-Oncology, 27(11), 2546–2558. https://doi.org/10.1002/pon.4757
Heathcote, L.C., Goldberg, D.S., Eccleston, C., Spunt, S.L., Simons, L.E., Sharpe, L., & Earp, B.D. (2018). Advancing shared decision making for symptom monitoring in people living beyond cancer. Lancet Oncology, 19(10), e556–e563. https://doi.org/10.1016/s1470-2045(18)30499-6
Herschbach, P., Berg, P., Dankert, A., Duran, G., Engst-Hastreiter, U., Waadt, S., . . . Henrich, G. (2005). Fear of progression in chronic diseases: Psychometric properties of the Fear of Progression Questionnaire. Journal of Psychosomatic Research, 58(6), 505–511. https://doi.org/10.1016/j.jpsychores.2005.02.007
Herschbach, P., Berg, P., Waadt, S., Duran, G., Engst-Hastreiter, U., Henrich, G., . . . Dinkel, A. (2010). Group psychotherapy of dysfunctional fear of progression in patients with chronic arthritis or cancer. Psychotherapy and Psychosomatics, 79(1), 31–38.
Hinz, A., Mehnert, A., Ernst, J., Herschbach, P., & Schulte, T. (2015). Fear of progression in patients 6 months after cancer rehabilitation—A validation study of the Fear of Progression Questionnaire FoP-Q-12. Supportive Care in Cancer, 23(6), 1579–1587. https://doi.org/10.1007/s00520-014-2516-5
Jacobson, N.S., Follette, W.C., & Revenstorf, D. (1984). Psychotherapy outcome research: Methods for reporting variability and evaluating clinical significance. Behavior Therapy, 15(4), 336–352. https://doi.org/10.1016/S0005-7894(84)80002-7
Jacobson, N.S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. https://doi.org/10.1037/0022-006x.59.1.12
Lebel, S., Ozakinci, G., Humphris, G., Mutsaers, B., Thewes, B., Prins, J., . . . Butow, P. (2016). From normal response to clinical problem: Definition and clinical features of fear of cancer recurrence. Supportive Care in Cancer, 24(8), 3265–3268. https://doi.org/10.1007/s00520-016-3272-5
Lebel, S., Tomei, C., Feldstain, A., Beattie, S., & McCallum, M. (2013). Does fear of cancer recurrence predict cancer survivors’ health care use? Supportive Care in Cancer, 21(3), 901–906.
Lengacher, C.A., Reich, R.R., Paterson, C.L., Ramesar, S., Park, J.Y., Alinat, C., . . . Kip, K.E. (2016). Examination of broad symptom improvement resulting from mindfulness-based stress reduction in breast cancer survivors: A randomized controlled trial. Journal of Clinical Oncology, 34(24), 2827–2834. https://doi.org/10.1200/jco.2015.65.7874
Lutgendorf, S.K., Shinn, E., Carter, J., Leighton, S., Baggerly, K., Guindani, M., . . . Sood, A.K. (2017). Quality of life among long-term survivors of advanced stage ovarian cancer: A cross-sectional approach. Gynecologic Oncology, 146(1), 101–108.
McCarthy, M.S., Matthews, E.E., Battaglia, C., & Meek, P.M. (2018). Feasibility of a telemedicine-delivered cognitive behavioral therapy for insomnia in rural breast cancer survivors. Oncology Nursing Forum, 45(5), 607–618. https://doi.org/10.1188/18.ONF.607-618
Mehnert, A., Herschbach, P., Berg, P., Henrich, G., & Koch, U. (2006). Fear of progression in breast cancer patients—Validation of the short form of the Fear of Progression Questionnaire (FoP-Q-SF). Zeitschrift for Psychosomatische Medizin und Psychotherapie, 52(3), 274–288. https://doi.org/10.13109/zptm.2006.52.3.274
Mehnert, A., Koch, U., Sundermann, C., & Dinkel, A. (2013). Predictors of fear of recurrence in patients one year after cancer rehabilitation: A prospective study. Acta Oncologica, 52(6), 1102–1109. https://doi.org/10.3109/0284186x.2013.765063
Melton, L. (2017). Brief introduction to cognitive behavioral therapy for the advanced practitioner in oncology. Journal of the Advanced Practitioner in Oncology, 8(2), 188–193.
Ozga, M., Aghajanian, C., Myers-Virtue, S., McDonnell, G., Jhanwar, S., Hichenberg, S., & Sulimanoff, I. (2015). A systematic review of ovarian cancer and fear of recurrence. Palliative and Supportive Care, 13(6), 1771–1780. https://doi.org/10.1017/s1478951515000127
Sharpe, L., Curran, L., Butow, P., & Thewes, B. (2018). Fear of cancer recurrence and death anxiety. Psycho-Oncology, 27(11), 2559–2565. https://doi.org/10.1002/pon.4783
Sharpe, L., Thewes, B., & Butow, P. (2017). Current directions in research and treatment of fear of cancer recurrence. Current Opinion in Supportive and Palliative Care, 11(3), 191–196.
Sharpe, L., Turner, J., Fardell, J.E., Thewes, B., Smith, A.B., Gilchrist, J., . . . Butow, P. (2019). Psychological intervention (ConquerFear) for treating fear of cancer recurrence: Mediators and moderators of treatment efficacy. Journal of Cancer Survivorship, 13(5), 695–702.
Simard, S., & Savard, J. (2009). Fear of Cancer Recurrence Inventory: Development and initial validation of a multidimensional measure of fear of cancer recurrence. Supportive Care in Cancer, 17(3), 241–251. https://doi.org/10.1007/s00520-008-0444-y
Simard, S., Thewes, B., Humphris, G., Dixon, M., Hayden, C., Mireskandari, S., & Ozakinci, G. (2013). Fear of cancer recurrence in adult cancer survivors: A systematic review of quantitative studies. Journal of Cancer Survivorship, 7(3), 300–322.
Smith, A.B., Thewes, B., Turner, J., Gilchrist, J., Fardell, J., Sharpe, L., . . . Butow, P. (2015). Pilot of a theoretically grounded psychologist-delivered intervention for fear of cancer recurrence (Conquer Fear). Psycho-Oncology, 24(8), 967–970. https://doi.org/10.1002/pon.3775
Sundin, E.C., & Horowitz, M.J. (2002). Impact of Event Scale: Psychometric properties. British Journal of Psychiatry, 180(3), 205–209. https://doi.org/10.1192/bjp.180.3.205
Tauber, N.M., O’Toole, M.S., Dinkel, A., Galica, J., Humphris, G., Lebel, S., . . . Zachariae, R. (2019). Effect of psychological intervention on fear of cancer recurrence: A systematic review and meta-analysis. Journal of Clinical Oncology, 37(31), 2899–2915.
Thewes, B., Brebach, R., Dzidowska, M., Rhodes, P., Sharpe, L., & Butow, P. (2014). Current approaches to managing fear of cancer recurrence; a descriptive survey of psychosocial and clinical health professionals. Psycho-Oncology, 23(4), 390–396. https://doi.org/10.1002/pon.3423
Thewes, B., Butow, P., Zachariae, R., Christensen, S., Simard, S., & Gotay, C. (2012). Fear of cancer recurrence: A systematic literature review of self-report measures. Psycho-Oncology, 21(6), 571–587. https://doi.org/10.1002/pon.2070
Thewes, B., Husson, O., Poort, H., Custers, J.A.E., Butow, P.N., McLachlan, S.A., & Prins, J.B. (2017). Fear of cancer recurrence in an era of personalized medicine. Journal of Clinical Oncology, 35(29), 3275–3278. https://doi.org/10.1200/jco.2017.72.8212
Wells, A. (1990). Panic disorder in association with relaxation induced anxiety: An attentional training approach to treatment. Behavior Therapy, 21(3), 273–280.
Wells, A. (2005). Detached mindfulness in cognitive therapy: A metacognitive analysis and ten techniques. Journal of Rational-Emotive and Cognitive-Behavior Therapy, 23(4), 337–355.
Wells, A. (2008). Metacognitive therapy: Cognition applied to regulating cognition. Behavioural and Cognitive Psychotherapy, 36(6), 651–658. https://doi.org/10.1017/S1352465808004803
Wittenberg, E., Reb, A., & Kanter, E. (2018). Communicating with patients and families around difficult topics in cancer care using the COMFORT communication curriculum. Seminars in Oncology Nursing, 34(3), 264–273. https://doi.org/10.1016/j.soncn.2018.06.007
Zhang, Q., Li, F., Zhang, H., Yu, X., & Cong, Y. (2018). Effects of nurse-led home-based exercise and cognitive behavioral therapy on reducing cancer-related fatigue in patients with ovarian cancer during and after chemotherapy: A randomized controlled trial. International Journal of Nursing Studies, 78, 52–60. https://doi.org/10.1016/j.ijnurstu.2017.08.010


