Self-Management Coaching: Promoting Postoperative Recovery and Caregiving Preparedness for Patients With Lung Cancer and Their Family Caregivers
Background: Quality of life (QOL) for patients undergoing lung resection and their family caregivers (FCGs) is often affected by surgical treatment for lung cancer.
Objectives: Patients and FCGs have a great deal of distress that affects their QOL. Introducing self-management skills soon after diagnosis improves patient and FCG outcomes.
Methods: This article presents a intervention model for providing patients and FCGs with self-management skills. Patients and FCGs will learn how to identify and overcome challenges, set goals, and address unmet needs throughout the phases of surgery. The model and case examples are presented.
Findings: Patients and FCGs gained self-efficacy. They were able to identify potential stressors that would otherwise become burdensome. Patients remained in control of their preoperative care and recovery, resulting in continued independence. FCGs achieved healthier well-being, which increased positive caregiving experiences.
Jump to a section
Lung cancer is the leading cause of cancer death in the United States for both men and women (Siegel et al., 2020). The incidence of lung cancer remains high in the United States, with many cases diagnosed at more advanced stages of the disease. Common presenting symptoms include cough, colored sputum, hoarseness, chest pain, and appetite loss. Some patients are asymptomatic before diagnosis. Most patients diagnosed with lung cancer are older; the median age at diagnosis is 70 years (Miller et al., 2019). When lung cancer is diagnosed early, the likelihood of surgical removal is higher. During the perioperative phase, both patients and family caregivers (FCGs) feel an increase in stress (Kim et al., 2016). Because most patients diagnosed with lung cancer are older, FCG demands in the perioperative setting can increase because of decreased psychological and physical functioning (Eguchi et al., 2017; Sun et al., 2017). Postoperatively, patients experience an increase in symptoms such as shortness of breath and fatigue (Hino et al., 2018; Tan et al., 2016). Symptom burden and functional declines may affect participation in key postoperative recovery activities, such as ambulation and respiratory exercises. Chest tubes are placed during the procedure to facilitate postoperative drainage and recovery. Postoperative ambulation during hospitalization is often challenging for patients because of the connected drainage system and anticipated pain from the chest tube. After lung resection, the expected course of recovery to baseline is one to two months (Shintani et al., 2018).
Caring for a loved one with lung cancer can be challenging, particularly during postoperative transitions from hospital to home. Both patients and FCGs can feel helpless and experience unmet needs because of a lack of preparation (Sun, Raz, & Kim, 2019). This results in an increased caregiving burden, poor dyadic quality of life (QOL), and poor postoperative outcomes for patients (Johansen et al., 2018; Longacre et al., 2018). Because of the increased responsibility and distress, FCGs are at greater risk of neglecting their own needs (Moss et al., 2019). They may also report symptoms, such as sleep disturbance, related to their caregiving role (Al-Daken & Ahmad, 2018). Despite the multiple caregiving tasks, many FCGs do not receive guidance on their caregiving role and rarely access emotional and social support services (National Alliance for Caregiving, 2016). FCG distress is associated with support in the emotional, psychological, employment, and social well-being domains (Sklenarova et al., 2015). Few interventions address the need for family-centered models of care in surgical oncology.
The purpose of this article is to describe a perioperative self-management multimedia intervention to enhance caregiving preparedness and postoperative recovery for patients with lung cancer undergoing surgery and their FCGs. The article also highlights the oncology nurse’s role in providing self-management coaching to dyads in the perioperative setting.
Methods
The trial and intervention design have been described elsewhere (Sun, Raz, Erhunmwunsee, et al., 2019). This ongoing trial is a five-year, single-site randomized controlled trial of 160 dyads of patients undergoing lung cancer surgery and their FCGs (320 total participants). The trial is conducted at City of Hope in Duarte, California, a National Cancer Institute–designated comprehensive cancer center, and its affiliated community practices. The overall purpose is to test the intervention’s efficacy on patient and FCG outcomes, comparing the intervention and attention control arms. The attention control condition involves videos and associated written materials from the American Cancer Society on clinical trial participation. The standard of perioperative care for patients undergoing lung resection does not include self-management skills training or FCG support. The primary objectives are improvements in FCG outcomes (caregiver burden, psychological distress, self-efficacy, activation, caregiving preparedness, QOL) and patient outcomes (psychological distress, self-efficacy, activation, QOL). An exploratory objective aims to explicate the interrelationship between FCG and patient outcomes. Outcomes are obtained primarily through validated patient- and FCG-reported measures and electronic health records.
Design
The perioperative self-management intervention is based on the Chronic Care Self-Management Model (McCorkle et al., 2011; Salvatore et al., 2015). The Chronic Care Self-Management Model transforms a reactive healthcare system into one that improves outcomes through proactive planning and skills building (Mosen et al., 2007). The nurse coaches dyads using three classic behavioral strategies:
• Employing SMART (specific, measurable, attainable, relevant, timely) goal setting
• Identifying challenges in preparing for surgery, postoperative recovery, and caregiving
• Problem-solving on an action plan to overcome the challenges identified
To promote FCG well-being, self-management skills building includes the development of a self-care plan that addresses the FCG’s QOL needs and promotes the importance of self-care as a strategy to prevent caregiving burden. As self-efficacy grows, dyads are empowered, enabled, and prepared for surgery and caregiving (Lorig & Holman, 2003; McCorkle et al., 2011; Merluzzi et al., 2019).
The intervention is administered through five coaching sessions that begin before surgery and continue for as many as two months after hospital discharge. In addition to the sessions, dyadic coaching content is delivered through a 20-minute video and print resource manuals. Each session includes self-management skills training in the context of preoperative preparation for surgery, postoperative recovery activities in the hospital, and recovery activities after discharge and while healing at home. Detailed intervention coaching content for each session is presented in Figure 1. 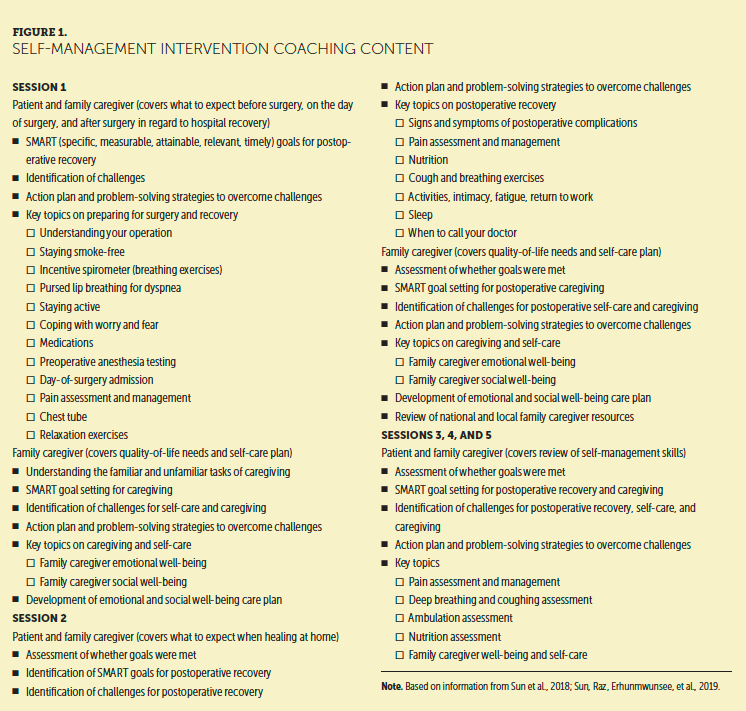
Results
Based on actual experiences, the following cases were identified to demonstrate the integration of self-management coaching to promote dyadic self-efficacy before and after lung cancer surgery.
Case Study 1
Mrs. M is a 71-year-old former smoker with upper left lung adenocarcinoma. She has a history of asthma, hypertension, and arrhythmias, with mild dyspnea on exertion. Her physical activities are limited, secondary to a significant fracture to her right leg and chronic pain. Mrs. M’s FCG is her 71-year-old spouse, a full-time contractor with a history of bipolar disorder. The dyad maintains an active life, but the lung cancer diagnosis and increasing comorbid conditions have forced them to make life adjustments.
Mrs. M’s SMART goal before surgery (session 1) was to practice using the incentive spirometer every day to prepare for postoperative respiratory exercises. Her identified challenge was communicating her needs with Mr. M. The action plan to overcome this challenge was to write down her thoughts and practice what to say beforehand. Mrs. M desired to overcome her challenge before surgery to foster better communication with Mr. M after surgery.
Mr. M’s goal before surgery was to learn new ways to communicate and express his feelings. His challenge was a lack of patience as an FCG. He identified strategies to overcome this challenge by learning to deep breathe, stay calm, and listen to Mrs. M. For his emotional self-care plan, Mr. M identified his sister as a trusted person for support, as well as painting and daily journaling as additional emotional well-being action plans. For his social well-being plan, Mr. M planned on finding time to golf with his friends. This activity helped Mr. M with maintaining his social connections while remaining active.
After surgery and before hospital discharge (session 2), Mrs. M’s goal was to maintain and resume her prediagnosis social activities. She identified her preexisting comorbid conditions as a barrier to postoperative ambulation and activity participation. To overcome this challenge, Mrs. M took her pain medications as instructed. She also practiced deep breathing, coughing, and ambulating to facilitate postdischarge recovery. Mr. M’s goal for after surgery and before discharge was to find a surgeon for Mrs. M’s chronic back pain and hire an aquatic therapist to help with her recovery needs at home. Keeping Mrs. M calm and hearing her needs was Mr. M’s challenge for after surgery and before discharge. Identified strategies to overcome this challenge included practicing communication, remaining calm, and taking a time-out when needed.
Mrs. M’s hospital stay was prolonged because of postoperative complications, and she was readmitted shortly after discharge. During the readmission, the dyad continued to use self-management skills, goals, and strategies, as well as the action plan, to overcome challenges. They maintained their communication goals and encouraged each other to share their needs and emotions.
One week after hospital discharge (sessions 3 and 4), Mrs. M identified her goal and challenge as feeling normal without any additional postoperative complications. To overcome this challenge, Mrs. M maintained physical activity and took her pain medications as instructed. She also consulted with a registered dietitian to help with postoperative nutritional needs. Mr. M’s challenge was postoperative caregiving. He continued to communicate with Mrs. M and reported success with their expressing thoughts and emotions with each other. Two months after discharge (session 5), Mrs. M recovered from her postoperative complications and reported physical improvements. She was traveling and attending social events with friends. Mr. M returned to working full-time and was active socially and physically. He reported good emotional well-being and was able to achieve and maintain his communication plan with Mrs. M.
Case Study 2
Mr. C is a 47-year-old Korean American man diagnosed with adenocarcinoma of the lung. He has no history of tobacco use and otherwise was healthy, except for hypertension. Mr. C lives with his mother, wife, and two children and works full-time as a dentist. Mr. C’s FCG is his spouse, Mrs. C, who is a full-time housewife.
Before surgery (session 1), Mr. C’s goal was to enjoy quality time with his family without distractions from work. He identified his challenge as needing to slow down with his dental practice in preparation for his upcoming surgery. To overcome this challenge and achieve his goal, Mr. C organized coverage for his dental practice. To prepare for the anticipated time away from his practice because of the surgery, Mr. C took additional days off during the week. He also took some weekend vacations before surgery to spend more time with his family.
Mrs. C identified her main challenge before surgery as managing the different roles that she plays at home as a wife and mother. She anticipated difficulties attending to the children’s needs while preparing for Mr. C’s surgery and postoperative needs. To overcome this challenge, Mrs. C created a family calendar of tasks and responsibilities that were reviewed with her children and posted on the refrigerator. To prepare for Mr. C’s recovery at home, Mrs. C’s goal was to organize and clean their bedroom two days before surgery. She also identified a second goal of planning meals ahead of time for Mr. C’s recovery. For her emotional well-being plan, Mrs. C focused on open communication with Mr. C and expressed her emotions about her caregiving role, the diagnosis, and upcoming surgery. Emotional well-being action plans included allowing herself to cry and going to the gym to relieve the emotional burden. For social well-being, Mrs. C used social media to stay socially active and connected with her family in Korea. She also scheduled monthly lunch dates with friends.
Before hospital discharge (session 2), Mr. C identified his postoperative goal as ambulating every hour. The challenge was symptoms (lack of energy, dyspnea), which were barriers to achieving Mr. C’s defined goal. Despite the challenges, Mr. C resolved to continue with hourly ambulation, as tolerated, and completed hourly respiratory exercises and cough using the incentive spirometer. He acknowledged that it takes time to recuperate from lung resection. Mrs. C identified her challenge as a lack of sleep because of Mr. C’s postoperative pain. She was also worried about increasing Mr. C’s pain and discomfort by moving too much in bed at night. Despite the concerns, Mrs. C recognized that pain management was part of Mr. C’s recovery process and that the challenge could be overcome by making sure that Mr. C took his pain medication as instructed to achieve pain control. Another identified strategy was to set a timer on her watch as a reminder to give Mr. C his next dose of pain medication. Mrs. C identified her long-term postoperative goal as supporting Mr. C’s postoperative recovery. For physical well-being, Mrs. C took 20-minute walks with Mr. C to help with his recovery and her daily stress. For spiritual well-being, Mrs. C maintained connection with her religious organization and used prayers and daily Bible readings to maintain hope and positivity.
On day 2 postdischarge (session 3), the dyad reported that their challenges and goals had not changed. Mrs. C felt supported in her role as a wife and mother because her mother-in-law was helping with the children, home duties, and caring for the patient. Mr. C focused on his recovery and took things one day at a time.
On day 7 postdischarge (session 4), Mr. C’s challenge was his mother refusing to allow meat in his postoperative diet because she believed it contributed to the spread of cancer. To overcome this challenge, Mr. C incorporated high-protein shakes and other forms of protein into his diet. His goal was to enjoy eating out with his family when he felt well enough to do so. For his recovery goal, Mr. C gradually increased his walk time and continued with daily deep-breathing exercises. His goal was to walk at least 30 minutes per day in the next two weeks.
Mrs. C identified her challenge as a lack of wound care knowledge. She had concerns about infection, as well as wound color and appearance. To overcome this challenge, Mrs. C contacted the surgical team to address her concerns and questions. The surgical team provided feedback, which allowed Mrs. C to care for Mr. C’s surgical wound with confidence.
For session 5, two months after discharge, Mr. C reported being able to achieve his postoperative goals for recovery. He was able to resume physical activity, such as bike riding with his family. This led to increased quality time with his family, which was a baseline goal. Overall, the lung cancer diagnosis prompted Mr. C to reevaluate his life priorities. Mrs. C reported success in achieving the goal of communicating her emotions. The self-management skills empowered her and allowed her to build self-efficacy in expressing her feelings. Mrs. C also reported that the self-management skills increased her perceived preparedness for the caregiving role by learning what to do before surgery, what to expect on the day of surgery, and how to recover at home. The skills obtained provided her with guidance and knowledge that she did not have previously.
Discussion
Surgery is one of the primary curative intent treatments for lung cancer. However, unmet needs related to postoperative recovery can significantly affect a patient’s QOL and increase the FCG’s burden (Brown et al., 2020; Kim & Yi, 2015). Because of changes in the healthcare environment and advances in surgical care, patients with lung cancer are discharged from the hospital earlier after surgery. This is despite an aging population experiencing more comorbidities, increased symptom burden, decreased physical function, and reduced QOL. As such, a greater proportion of the caregiving burden has fallen on FCGs (Chambers et al., 2010; Fujinami et al., 2015; Grant et al., 2013; Kim et al., 2016).
As cancer care continues to move further into the home setting, FCGs and patients may be ill-prepared for recovery at home. Adequate preparation for surgery and self-management may help to empower patients and their families, as well as decrease distress and increase QOL (Knobf, 2013). The case studies included in this article illustrate that self-management skills building could be successfully incorporated into perioperative and postoperative care. Self-management skills building that begins before surgery is an evidence-based approach that may improve self-efficacy, reduce caregiving burden, and enhance postoperative recovery (Salvatore et al., 2015). According to observational evidence, patients with lung cancer with low self-efficacy who had an FCG with low self-efficacy noted worse physical and psychological well-being; in addition, dyads with high self-efficacy noted better QOL, with low FCG self-efficacy being associated with higher FCG distress and caregiver burden (Porter et al., 2008). Accordingly, these findings suggest that interventions targeted at improving self-efficacy and -management may benefit this population.
Implications for Nursing
Perioperative and postoperative nurses provide most of the care for surgical populations. Although most oncology nurses possess clinical knowledge of the postoperative patient’s physical condition, few have specific self-management skills building and coaching training. Training on self-management principles is possible for nurses (Schulman-Green et al., 2016), and advancing the science of self-management of chronic conditions, including cancer, is a priority of the National Institute of Nursing Research (Moore et al., 2016).
Oncology nurses can use the principles of self-management skills building (setting goals, identifying challenges, formulating action plans through problem-solving) to guide FCGs and patients through surgery and recovery. Self-management interventions are sustainable because all oncology nurses can be trained to provide dyadic coaching. There are few anticipated financial implications for oncology practices to provide self-management interventions, although cost-effectiveness data are needed to confirm this. Nurses who care for patients in the preoperative setting (e.g., preanesthesia testing clinics) can be trained to start self-management skills building for dyads before surgery, with a focus on preparing for the upcoming surgery. They can introduce the principles of self-management skills building early so dyads can begin preparing for their surgery and postoperative recovery. Postoperatively, nurses can continue supporting the dyad’s self-management skills building, focusing on recovery activities (ambulation, respiratory exercises, symptom management) and caregiving and FCG self-care. Armed with preparatory self-management skills, dyads may approach their scheduled surgery and caregiving responsibilities with more ease, taking away fear of the unknown.
Potential limitations of the intervention include the lack of generalizability to patients and FCGs outside of a comprehensive cancer center setting and to dyads who are non–English speaking. Future iterations of the intervention should establish the effectiveness of the intervention in other care settings and in rural communities. Efforts should also be undertaken to develop and test culturally and linguistically sensitive versions of the intervention to establish efficacy in different populations. 
Conclusion
Patients with lung cancer and FCGs have unmet needs, as well as experience caregiving burden and uncertainty associated with recovery in the perioperative setting. This article highlights a perioperative, nurse-led self-management intervention to prepare patients with lung cancer and their FCGs for surgery and postoperative recovery using case studies. Dyads are enabled and empowered through skills building in goal setting, problem-solving, and FCG self-care. Oncology nurses in the perioperative setting can consider building their self-management coaching skills and integrating them into daily patient care. 
About the Author(s)
Rosemary Prieto, BSN, RN, is a clinical research nurse, and Betty Ferrell, PhD, FAAN, is a director and professor, both in the Division of Nursing Research and Education in the Department of Population Sciences; Jae Y. Kim, MD, is an associate professor and chief in the Division of Thoracic Surgery in the Department of Surgery; and Virginia Sun, PhD, RN, is an associate professor in the Division of Nursing Research and Education in the Department of Population Sciences and in the Department of Surgery, all at City of Hope in Duarte, CA. The authors take full responsibility for this content. Research reported in this population is supported by the National Cancer Institute of the National Institutes of Health under award number R01CA217841. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Prieto can be reached at rprieto@coh.org, with copy to CJONEditor@ons.org. (Submitted July 2020. Accepted October 21, 2020.)
References
Al-Daken, L.I., & Ahmad, M.M. (2018). Predictors of burden and quality of sleep among family caregivers of patients with cancer. Supportive Care in Cancer, 26(11), 3967–3973. https://doi.org/10.1007/s00520-018-4287-x
Brown, L.M., Gosdin, M.M., Cooke, D.T., Apesoa-Varano, E.C., & Kratz, A.L. (2020). Health-related quality of life after lobectomy for lung cancer: Conceptual framework and measurement. Annals of Thoracic Surgery, 110(6), 1840–1846. https://doi.org/10.1016/j.athoracsur.2020.05.080
Chambers, A., Routledge, T., Pilling, J., & Scarci, M. (2010). In elderly patients with lung cancer is resection justified in terms of morbidity, mortality and residual quality of life? Interactive CardioVascular and Thoracic Surgery, 10(6), 1015–1021. https://doi.org/10.1510/icvts.2010.233189
Eguchi, T., Bains, S., Lee, M.-C., Tan, K.S., Hristov, B., Buitrago, D.H., . . . Adusumilli, P.S. (2017). Impact of increasing age on cause-specific mortality and morbidity in patients with stage I non-small-cell lung cancer: A competing risks analysis. Journal of Clinical Oncology, 35(3), 281–290. https://doi.org/10.1200/JCO.2016.69.0834
Fujinami, R., Sun, V., Zachariah, F., Uman, G., Grant, M., & Ferrell, B. (2015). Family caregivers’ distress levels related to quality of life, burden, and preparedness. Psycho-Oncology, 24(1), 54–62. https://doi.org/10.1002/pon.3562
Grant, M., Sun, V., Fujinami, R., Sidhu, R., Otis-Green, S., Juarez, G., . . . Ferrell, B. (2013). Family caregiver burden, skills preparedness, and quality of life in non-small cell lung cancer. Oncology Nursing Forum, 40(4), 337–346. https://doi.org/10.1188/13.ONF.337-346
Hino, H., Karasaki, T., Yoshida, Y., Fukami, T., Sano, A., Tanaka, M., . . . Nakajima, J. (2018). Risk factors for postoperative complications and long-term survival in lung cancer patients older than 80 years. European Journal of Cardiothoracic Surgery, 53(5), 980–986. https://doi.org/10.1093/ejcts/ezx437
Johansen, S., Cvancarova, M., & Ruland, C. (2018). The effect of cancer patients’ and their family caregivers’ physical and emotional symptoms on caregiver burden. Cancer Nursing, 41(2), 91–99. https://doi.org/10.1097/ncc.0000000000000493
Kim, H., & Yi, M. (2015). Unmet needs and quality of life of family caregivers of cancer patients in South Korea. Asia-Pacific Journal of Oncology Nursing, 2(3), 152–159. https://doi.org/10.4103/2347-5625.158019
Kim, J.Y., Sun, V., Raz, D.J., Williams, A.C., Fujinami, R., Reckamp, K., . . . Ferrell, B. (2016). The impact of lung cancer surgery on quality of life trajectories in patients and family caregivers. Lung Cancer, 101, 35–39. https://doi.org/10.1016/j.lungcan.2016.08.011
Knobf, M.T. (2013). Being prepared: Essential to self-care and quality of life for the person with cancer. Clinical Journal of Oncology Nursing, 17(3), 255–261. https://doi.org/10.1188/13.CJON.255-261
Longacre, M.L., Applebaum, A.J., Buzaglo, J.S., Miller, M.F., Golant, M., Rowland, J.H., . . . Northouse, L. (2018). Reducing informal caregiver burden in cancer: Evidence-based programs in practice. Translational Behavioral Medicine, 8(2), 145–155. https://doi.org/10.1093/tbm/ibx028
Lorig, K.R., & Holman, H.R. (2003). Self-management education: History, definition, outcomes, and mechanisms. Annals of Behavioral Medicine, 26(1), 1–7. https://doi.org/10.1207/s15324796abm2601_01
McCorkle, R., Ercolano, E., Lazenby, M., Schulman-Green, D., Schilling, L.S., Lorig, K., & Wagner, E.H. (2011). Self-management: Enabling and empowering patients living with cancer as a chronic illness. CA: A Cancer Journal for Clinicians, 61(1), 50–62. https://doi.org/10.3322/caac.20093
Merluzzi, T.V., Pustejovsky, J.E., Philip, E.J., Sohl, S.J., Berendsen, M., & Salsman, J.M. (2019). Interventions to enhance self-efficacy in cancer patients: A meta-analysis of randomized controlled trials. Psycho-Oncology, 28(9), 1781–1790. https://doi.org/10.1002/pon.5148
Miller, K.D., Nogueira, L., Mariotto, A.B., Rowland, J.H., Yabroff, K.R., Alfano, C.M., . . . Siegel, R.L. (2019). Cancer treatment and survivorship statistics, 2019. CA: A Cancer Journal for Clinicians, 69(5), 363–385. https://doi.org/10.3322/caac.21565
Moore, S.M., Schiffman, R., Waldrop-Valverde, D., Redeker, N.S., McCloskey, D.J., Kim, M.T., . . . Grady, P. (2016). Recommendations of common data elements to advance the science of self-management of chronic conditions. Journal of Nursing Scholarship, 48(5), 437–447. https://doi.org/10.1111/jnu.12233
Mosen, D.M., Schmittdiel, J., Hibbard, J., Sobel, D., Remmers, C., & Bellows, J. (2007). Is patient activation associated with outcomes of care for adults with chronic conditions? Journal of Ambulatory Care Management, 30(1), 21–29.
Moss, K.O., Kurzawa, C., Daly, B., & Prince-Paul, M. (2019). Identifying and addressing family caregiver anxiety. Journal of Hospice and Palliative Nursing, 21(1), 14–20. https://doi.org/10.1097/njh.0000000000000489
National Alliance for Caregiving. (2016). Cancer caregiving in the U.S.: An intense, episodic, and challenging care experience. https://www.caregiving.org/wp-content/uploads/2020/05/CancerCaregivingR…
Porter, L.S., Keefe, F.J., Garst, J., McBride, C.M., & Baucom, D. (2008). Self-efficacy for managing pain, symptoms, and function in patients with lung cancer and their informal caregivers: Associations with symptoms and distress. Pain, 137(2), 306–315. https://doi.org/10.1016/j.pain.2007.09.010
Salvatore, A.L., Ahn, S., Jiang, L., Lorig, K., & Ory, M.G. (2015). National study of chronic disease self-management: 6-month and 12-month findings among cancer survivors and non-cancer survivors. Psycho-Oncology, 24(12), 1714–1722. https://doi.org/10.1002/pon.3783
Schulman-Green, D., Jaser, S.S., Park, C., & Whittemore, R. (2016). A metasynthesis of factors affecting self-management of chronic illness. Journal of Advanced Nursing, 72(7), 1469–1489. https://doi.org/10.1111/jan.12902
Shintani, Y., Funaki, S., Ose, N., Kanou, T., Kanzaki, R., Minami, M., & Okumura, M. (2018). Chest tube management in patients undergoing lobectomy. Journal of Thoracic Disease, 10(12), 6432–6435. https://doi.org/10.21037/jtd.2018.11.47
Siegel, R.L., Miller, K.D., & Jemal, A. (2020). Cancer statistics, 2020. CA: A Cancer Journal for Clinicians, 70(1), 7–30. https://doi.org/10.3322/caac.21590
Sklenarova, H., Krümpelmann, A., Haun, M.W., Friederich, H.-C., Huber, J., Thomas, M., . . . Hartmann, M. (2015). When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer, 121(9), 1513–1519. https://doi.org/10.1002/cncr.29223
Sun, V., Burhenn, P.S., Lai, L., & Hurria, A. (2017). The impact of comorbidity on surgical outcomes in older adults with cancer. Seminars in Oncology Nursing, 33(1), 80–86. https://doi.org/10.1016/j.soncn.2016.11.008
Sun, V., Kim, J.Y., Raz, D.J., Chang, W., Erhunmwunsee, L., Uranga, C., . . . McCorkle, R. (2018). Preparing cancer patients and family caregivers for lung surgery: Development of a multimedia self-management intervention. Journal of Cancer Education, 33(3), 557–563. https://doi.org/10.1007/s13187-016-1103-5
Sun, V., Raz, D.J., Erhunmwunsee, L., Ruel, N., Carranza, J., Prieto, R., . . . Kim, J.Y. (2019). Improving family caregiver and patient outcomes in lung cancer surgery: Study protocol for a randomized trial of the multimedia self-management (MSM) intervention. Contemporary Clinical Trials, 83, 88–96. https://doi.org/10.1016/j.cct.2019.07.002
Sun, V., Raz, D.J., & Kim, J.Y. (2019). Caring for the informal cancer caregiver. Current Opinion in Supportive and Palliative Care, 13(3), 238–242. https://doi.org/10.1097/SPC.0000000000000438
Tan, H.-J., Saliba, D., Kwan, L., Moore, A.A., & Litwin, M.S. (2016). Burden of geriatric events among older adults undergoing major cancer surgery. Journal of Clinical Oncology, 34(11), 1231–1238. https://doi.org/10.1200/JCO.2015.63.4592




