Psychological Distress and Work-Related Quality of Life Among Oncology Nurses During the COVID-19 Pandemic: A Cross-Sectional Study
Background: Oncology nurses are at disproportionate risk for psychological distress because they often encounter ethical challenges and deaths while providing care. Exposures to emergent suffering during the COVID-19 pandemic compound their chronic distress, which likely increased their vulnerability to psychological distress and may increase their risk for reduced work-related quality of life (WRQOL).
Objectives: This study examined the association between psychological distress and WRQOL among oncology nurses during the COVID-19 pandemic.
Methods: A cross-sectional analysis of psychological distress and WRQOL among oncology nurses (N = 63) was conducted.
Findings: The mean Depression, Anxiety and Stress Scale score was 33.4, showing low depression levels, mild anxiety, and mild stress. The mean PTSD score was 29.3, and the mean WRQOL Scale score was 78.8. Depression, anxiety, and stress were strongly correlated to PTSD, and WRQOL was negatively correlated to PTSD, depression, anxiety, and stress.
Jump to a section
Earn free contact hours: Click here to connect to the evaluation. Certified nurses can claim no more than 1 total ILNA point for this program. Up to 1 ILNA point may be applied to Oncology Nursing Practice OR Professional Practice/Performance OR Psychosocial Dimensions of Care OR Roles of the APRN. See www.oncc.org for complete details on certification.
The COVID-19 pandemic triggered psychological distress among healthcare workers (HCWs), increasing negative affective states and work-related stress (Shahrour & Dardas, 2020; Shechter et al., 2020). The prevalence of psychological distress was 41%–54% among HCWs prior to the pandemic (Ghawadra et al., 2019; Melnyk et al., 2018) and rose to 95.9% during the pandemic (Zhang et al., 2020). Exposure to psychological distress may lead to lower work-related quality of life (WRQOL) (Melnyk et al., 2018). Significant reductions in WRQOL are correlated with poor nursing care and healthcare outcomes and can affect nurse retention rates, productivity, and job satisfaction (Labrague & de Los Santos, 2021; Wang et al., 2020). Poor nursing care and associated suboptimal healthcare outcomes suggest acts of avoidable incompetence or harm in nursing that extend to patients, compromising their overall safety (World Health Organization, 2021).
During the COVID-19 pandemic, HCWs providing direct care to patients with COVID-19 have been at the greatest risk for psychological distress (Shaukat et al., 2020; Zhao et al., 2020). Specifically, nurses have an increased risk for post-traumatic stress disorder (PTSD), depression, and anxiety compared to other HCWs (Si et al., 2020; Song et al., 2020). Nurses have not only developed PTSD, but also have had greater risk for psychological dysfunction during the pandemic (Wang et al., 2020). Oncology nurses’ chronic stress, which has been compounded by exposures to patients’ emergent suffering during this pandemic, has made them particularly vulnerable to burnout. Burnout is associated with depression and suicidal ideation among HCWs (Hakanen & Schaufeli, 2012), and about 32% of nurses cite burnout as the reason for resignation (Shah et al., 2021). Burnout, among other work stressors, contributes to lower WRQOL and diminished quality of nursing care (Rosa et al., 2020).
Oncology nurses have intrinsic exposure to psychological distress because they frequently encounter multiple ethical challenges and deaths while providing cancer care (Rezaee et al., 2019). Chronic distress experienced by oncology nurses is well documented globally and is linked to job dissatisfaction, high workload, and lack of organizational support (Nwozichi et al., 2020). Chronicity of cancer care, exposure to harmful treatments, and extension of life without concern for quality, particularly when treating patients with poor prognoses, may be psychologically disruptive for oncology nurses, increasing the likelihood of lower WRQOL (Tsehay et al., 2020).
Patients with cancer also encounter significant psychological distress throughout the care trajectory (Pitman et al., 2018; Tsaras et al., 2018), which has been exacerbated by disrupted and fragmented care since the COVID-19 pandemic began (Karacin et al., 2020). Untreated psychological distress in patients may exacerbate their overall health, posing additional challenges to oncology nursing care (Paterson et al., 2020). In this context, oncology nurses may deal with significant work-related stress and may feel ill-equipped to address multiple patient-level psychological difficulties.
Although nurses are more prone to psychological distress during the pandemic, there is a paucity of data examining whether an association between psychological distress and WRQOL exists among oncology nurses (Shahrour & Dardas, 2020; Si et al., 2020; Wang et al., 2020). Characterizing this association could inform the development of psychosocial interventions to improve coping, increase resilience against psychological distress, and improve WRQOL among oncology nurses. Finding measures to improve psychological functioning in oncology nurses is important because quality nursing care is linked to better patient care and outcomes.
This study addresses this research gap by (a) evaluating oncology nurses’ psychological distress (depression, anxiety, stress, and PTSD) and (b) examining the association between psychological distress and WRQOL among inpatient oncology nurses during the COVID-19 pandemic.
Methods
Design, Sample, and Setting
A descriptive, cross-sectional study was conducted using an internet-based survey to examine whether oncology nurses’ self-reported psychological distress was associated with WRQOL. Psychological distress was measured with assessments of depression, anxiety, stress, and PTSD. The sample was drawn from a population of nurses (N = 140) who worked on the solid, hematologic malignancy and bone marrow transplant units at the Beth Israel Deaconess Medical Center in Boston, Massachusetts.
This setting was chosen for study because like all direct patient care providers, oncology nurses have been regularly exposed to COVID-19 at work. Patients suspected of COVID-19 remained on these units pending a rule out, which involved collection of two COVID-19 tests by respiratory therapists. If patients tested positive, they were transferred to a dedicated COVID-19 unit pending bed availability. If they required intensive care, oncology nurses were deployed for critical oncology-specific interventions, such as administering chemotherapy, although these were deferred until clinical stability. Patients with negative COVID-19 test results or clinical concerns suggestive of COVID-19 were monitored using appropriate precautions on the units but were not transferred to a dedicated COVID-19 unit. Although efforts were made to seclude patients with a confirmed or suspected COVID-19 infection, nurses working on both units had exposures via direct care of patients with cancer who were also diagnosed with or suspected to have COVID-19.
Data Collection
All nurses on the inpatient units were contacted by email to participate in an online survey. The principal investigator sent email invitations containing a link to the study information sheet and survey. A reminder email was sent one week after the initial email invitation. The study information sheet outlined the objectives and risks, emphasizing that participation was voluntary and anonymous. The survey took 20–30 minutes to complete. Survey data were collected between June 1, 2020, and July 27, 2020 via REDCap (Harris et al., 2009), a secure, Health Insurance Portability and Accountability Act–protected electronic database. The institutional review board of the participating institution approved an informed consent waiver because this was a minimal risk study. Survey completion implied consent.
Measures
Demographic variables: Nurse-level characteristics including age, sex, years of nursing experience, years of oncology experience, oncology certification, race, ethnicity, marital status, employment status, educational level, and primary language, were collected. The covariates were predicted a priori to contribute to nurses’ WRQOL based on the literature.
Predictor variables: The 21-item Depression, Anxiety and Stress Scale (DASS-21), a shorter version of the DASS-42, measures depression, anxiety, and stress using a four-point Likert-type scale ranging from 0 (did not apply to me at all) to 3 (applied to me very much) (Lovibond & Lovibond, 1995). Total scores range from 0 to 126, with higher scores indicating more severe negative emotional distress. The DASS-21 has high internal consistency and reliability in assessments of HCWs (Hammond et al., 2021; Sarapultseva et al., 2021). The Impact of Events Scale–Revised is a 22-item scale that measures PTSD symptoms using a five-point Likert-type scale (Weiss & Marmar, 1996). Total scores range from 0 to 88, with higher scores indicating the presence of severe PTSD symptoms. The Impact of Events Scale–Revised has high internal consistency and reliability in HCWs (Sarapultseva et al., 2021).
Primary outcome: The 23-item WRQOL Scale measures WRQOL in HCWs using a five-point Likert-type scale (Easton & Van Laar, 2018). Total scores range from 23 to 115, with higher scores indicating greater perceived quality of work life. It has strong internal consistency (Shukla et al., 2017).
Data Analysis
Descriptive statistics were used to examine nurse-level characteristics. Pearson correlation was used to examine the association between continuous variables, and a chi-square test was used to examine associations between categorical variables. WRQOL as the primary outcome was modeled as a continuous variable in a multivariable linear regression analysis to see whether depression, anxiety, stress, PTSD, and nurse-level characteristics had independent effects. Covariates with independent effects were included in the final model. Statistical significance was set at p < 0.05. Using G*Power, version 3.1, it was determined that the study had 80% power to detect a statistically significant association with a sample size of 55. All analyses were conducted using STATA, version 16.0.
Results
Sample Characteristics
The demographics of the sample (N = 63) were similar to the 2018 National Sample Survey of Registered Nurses (U.S. Department of Health and Human Services, 2019) in terms of educational level, sex, race, and ethnicity. The mean age of respondents was 34.8 years (SD = 9.8). Most respondents were White (n = 60), non-Hispanic (n = 65), female (n = 66), and worked full-time (n = 65). Most had a bachelor’s degree (n = 61), followed by a master’s degree (n = 5) or associate degree (n = 2). More than half were not married (n = 39). The mean nursing and oncology experience was 9.3 years (SD = 8.4) and 7.9 years (SD = 7.3), respectively, with a range of 0–32 years. Twenty-eight nurses had oncology certification. Of note, surveys were sent to 140 oncology nurses, 68 responded, and only 63 completed the survey in its entirety, demonstrating a 45% response rate. Although five nurses completed only the demographic portion of the survey and were excluded from the final analysis, the demographic data they provided did not differ from the study respondents and were included in the demographics of the sample. The Response Rate 1 formula was used to calculate the response rate (American Association for Public Opinion Research, 2015). This study’s response rate of 45% is higher than the average response rate of 33% for studies using web-based surveys (Shih & Fan, 2008).
Study Variables
The mean DASS-21 score was 33.4 (SD = 21.9, range = 0–104). The subscales revealed low levels of depression (mean = 9, SD = 7.4), mild anxiety (mean = 9.09, SD = 7.8), and mild stress (mean = 15.3, SD = 9.4). Regarding PTSD, the mean score was 29.3 (SD = 15.94, range = 4–69). WRQOL was negatively correlated to PTSD (r = –0.5, p < 0.001), as well as anxiety, depression, and stress (r = –0.59, p < 0.001). Nurses’ anxiety, depression, and stress were strongly correlated to PTSD (r = 0.81, p < 0.001).
The mean WRQOL Scale score was 78.8 (SD = 10.5, range = 54–110). Independent significant effect was shown for depression, anxiety, and stress (β = –0.498, 95% CI [–0.767, –0.229], p < 0.001). The multivariate regression analysis is detailed in Table 1. 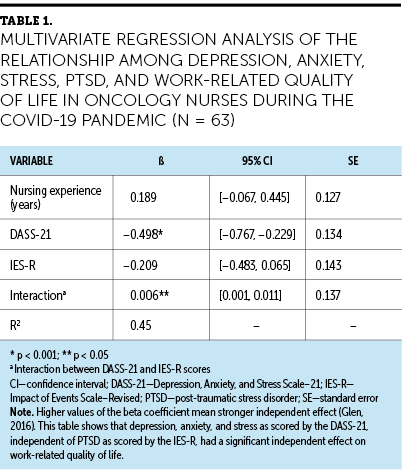
Pearson chi-square tests showed statistically significant associations between nurses’ educational level and employment status (chi-square = 12.9, p = 0.011). Ethnicity was found to be significantly associated with language (chi-square = 16.2, p < 0.01) and race (chi-square = 52.1, p < 0.01). Race was found to be significantly associated with marital status (chi-square = 24.3, p = 0.018). WRQOL was correlated to years of nursing experience (r = 0.36, p < 0.01). Anxiety, depression, and stress were negatively correlated with years of nursing experience (r = –0.26, p < 0.05). Age was correlated to years of nursing experience (r = 0.86, p < 0.05). Years of oncology experience and years of nursing experience were collinear, so years of oncology experience was excluded from the regression model. No other significant associations were observed.
Discussion
The COVID-19 pandemic caused significant stress, disruptions, and challenges in healthcare settings, resulting in psychological distress for oncology nurses. This cross-sectional analysis examined the association between psychological distress (depression, anxiety, stress, and PTSD) and WRQOL among inpatient oncology nurses during the COVID-19 pandemic. Nurses in this study cohort described their WRQOL as average. Furthermore, they reported lower levels of depression, anxiety, and stress with their mean PTSD score suggesting partial PTSD. Studies specifically examining the association between psychological distress and WRQOL among oncology nurses are lacking. Findings from studies that focused on nurses’ WRQOL were consistent with the results of the current study (Abbasi et al., 2017; Saygili et al., 2020), but overlaps in WRQOL scores may be explained by variations in personal factors and work conditions.
For example, a study by Baykal et al. (2009) found that Turkish oncology nurses are overworked, do not receive proper compensation, and face gender discrimination in the workplace (i.e., while breastfeeding or when pregnant). Nurses in non-oncology settings have also reported lack of organizational commitment, poor work conditions, communication breakdowns, and low compensation as significant stressors contributing to poor WRQOL (Aliwalas et al., 2016). These stressors likely worsened during the COVID-19 pandemic because nurses have been increasingly faced with patients’ emergent and evolving suffering in addition to limited resources, such as lack of personal protective equipment, augmenting work-related stress (Arnetz et al., 2020).
Although results from other studies support the findings from this study, variations in practice settings or personal, social, and cultural influences may have accounted for differences in self-reported WRQOL. Perceptions of work may also differ depending on cultural values, particularly for studies based outside of the United States (Abbasi et al., 2017; Lebni et al., 2020). A global perspective matters because shared cultural assumptions may shape how nurses respond, cope, or adapt to stressors in the work environment. Differences in WRQOL scores may also be related to occupational competence and/or perceptions of working conditions (e.g., high number of patients, high patient acuity, high work pressure), which may influence nurses’ commitment to organizational goals and mission (Abbasi et al., 2017).
Patients with cancer have a 3.5 times higher risk of developing severe COVID-19 disease compared to patients with other conditions (Liang et al., 2020). Oncology nurses’ awareness of their patients’ vulnerability to infections is constant, and the pressure to protect their patients from infections can be stressful. The threat of COVID-19 has likely compounded this chronic stress. Patients with cancer also experienced delays and disruptions in care during the COVID-19 pandemic, which increased work-related demands for already overworked nurses. Interruptions to patient-level mental health interventions limited much needed psychological support for patients with cancer (Connolly et al., 2020). Psychological distress in patients with cancer is associated with stress among oncology nurses (Nwozichi et al., 2020). This distress likely heightened during the pandemic. Early identification and management of distress may reduce maladaptive coping strategies, enhancing oncology nurses’ resilience against work-related stress. Nurses who are resilient in stressful situations are less likely to experience lower WRQOL (Tsehay et al., 2020).
Although oncology nurses are expected to appropriately assess and identify patients’ psychosocial needs, evidence suggests otherwise. In routine practice, oncology nurses lack confidence in assessing, managing, and communicating with patients about their psychosocial difficulties (Güner et al., 2018). In addition, oncology nurses’ exposures to providing psychosocial care are limited, even at end of life (Blaževičienė et al., 2017), which makes addressing patients’ psychosocial needs challenging (Güner et al., 2018). The confluence of these factors may make oncology nurses more vulnerable to psychological distress, which increases the likelihood of lower WRQOL.
The post-hoc analysis showed a significant interaction effect between psychological distress (depression, anxiety, and stress) and PTSD. Depression, anxiety, and stress, independent of PTSD, significantly predicted WRQOL (β = 0.006, 95% CI [0.001, 0.011], p = 0.02). These post-hoc analysis results suggest that depression, anxiety, and stress correlate with nurses’ WRQOL and should be the focus of future nurse-level psychosocial interventions.
Limitations
This cross-sectional analysis has several limitations. The study assessed psychosocial distress using self-reporting, which is prone to a social desirability bias and may lead to systematic misreporting. Causal inferences between psychological distress and WRQOL cannot be drawn, which is an inherent limitation of cross-sectional examination. It is important to understand the range of factors (e.g., personal, contextual) and predictors of professional quality of life (e.g., loneliness, moral distress, self-compassion) (Eche et al., 2022) that may influence negative emotional states and WRQOL among nurses (Phillips et al., 2021). These factors may also be better examined through the lens of a conceptual framework theory.
The lower psychological distress in the study cohort may have been because of the timing of study, which occurred between surges of the COVID-19 pandemic in the United States. Longitudinal assessments of progression or improvements in psychological distress once the imminent threat of COVID-19 subsides are important. Nurses’ distress could also fluctuate and may have been missed cross-sectionally; future studies should investigate this prospectively. This study did not measure nurses’ overall responses to the pandemic. This is important because it may affect nurses’ experiences related to work-related stressors and quality of life. The sample was predominantly White, non-Hispanic females drawn from a single academic cancer center. There may be racial and ethnic, as well as practice setting differences relating to the stress experiences of COVID-19, which future studies should investigate.
Implications for Practice
Oncology nurses experience chronic stress, which may make them more vulnerable to distress during the COVID-19 pandemic. Early recognition and targeted nurse-level psychosocial interventions may preserve WRQOL (Melnyk et al., 2018). Well-adjusted nurses are more likely to contribute to their patients’ lives and environments safely and meaningfully. Organizational efforts to minimize additional psychological burden can expand oncology nurses’ cognitive capacity to better navigate stressful events. Work demands are negatively correlated with resilience, so reductions in work-related stress may minimize impairments to WRQOL by improving resilience (Yu et al., 2019). Specifically, nurses may proactively achieve some degree of resilience to mitigate their distress if their organizations are committed to their success, bolstering their continued professional growth and commitment to their profession (Yu et al., 2019).
Oncology nurses should also pay particular attention to their patients’ psychosocial experiences and difficulties. Recognizing patients’ sources of stress and identifying strategies to address them may help to provide better holistic care (Rosa et al., 2021). In addition, enhancing nurses’ ability to assess and manage patients’ psychosocial distress through a psychosocial training program has been shown to increase nurses’ confidence and knowledge about psychosocial care (Kubota et al., 2016). Nurses who have completed palliative care training are also more likely to have greater self-confidence and knowledge as compared to nurses who have not completed such training (Shipman et al., 2008). They may feel emboldened to use their knowledge to navigate the difficulties they face while managing patients’ care. Self-confidence and knowledge may lessen the chronic distress oncology nurses face while providing care, and working to minimize psychosocial difficulties for patients with cancer may in turn mitigate oncology nurses’ own poor psychosocial health, particularly during the pandemic. 
Conclusion
The COVID-19 pandemic triggered significant stressors in the healthcare system that can lead to impairments in WRQOL among oncology nurses. Particular attention should be paid to oncology nurses because they are already prone to chronic stress. Despite lower levels of psychological distress, oncology nurses in this study experienced alterations to WRQOL. Early integration of nurse-level psychosocial interventions may mitigate distress and improve coping, allowing oncology nurses to better adapt to work stressors. Psychological adaptation in oncology nurses may increase their resilience and improve their WRQOL. 
About the Author(s)
Ijeoma Julie Eche, PhD, MPH, FNP-BC, AOCNP®, CPHON®, BMTCN®, is a postdoctoral research fellow at the Dana Farber Cancer Institute and a family nurse practitioner in the Bone Marrow Transplantation and Hematologic Malignancy Program at Beth Israel Deaconess Medical Center, both in Boston, MA; Ifeoma Mary Eche, PharmD, BCCCP, CACP, FCCM, is a clinical pharmacy manager in the Department of Pharmacy at Beth Israel Deaconess Medical Center; and Teri B. Aronowitz, PhD, FNP-BC, FAAN, is a professor in the Tan Chingfen Graduate School of Nursing at the University of Massachusetts Medical School in Worcester and is the editor-in-chief of the Journal of American College Health. The authors take full responsibility for this content and did not receive honoraria or disclose any relevant financial relationships. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. I.J. Eche can be reached at ijeche@bidmc.harvard.edu, with copy to CJONEditor@ons.org. (Submitted December 2021. Accepted February 24, 2022.)
References
Abbasi, M., Zakerian, A., Akbarzade, A., Dinarvand, N., Ghaljahi, M., Poursadeghiyan, M., & Ebrahimi, M.H. (2017). Investigation of the relationship between work ability and work-related quality of life in nurses. Iranian Journal of Public Health, 46(10), 1404–1412.
Aliwalas, K.A.N., Briones, T.J.M., Carabit, Q.M.M, Huyo, J.M.F, Mugol, H.K.L., Samantha, A., . . . Tamayo, R.L.J. (2016). Professional quality of life of staff nurses in the Cancer Institute of the Philippine General Hospital. Journal of Oncology Navigation and Survivorship, 7(9), 32.
American Association for Public Opinion Research. (2015). Standard definitions: Final dispositions of case codes and outcome rates for surveys (8th ed.). https://www.aapor.org/AAPOR_Main/media/MainSiteFiles/Standard-Definitio…
Arnetz, J.E., Goetz, C.M., Arnetz, B.B., & Arble, E. (2020). Nurse reports of stressful situations during the COVID-19 pandemic: Qualitative analysis of survey responses. International Journal of Environmental Research and Public Health, 17(21), 8126. https://doi.org/10.3390/ijerph17218126
Baykal, U., Seren, S., & Sokmen, S. (2009). A description of oncology nurses’ working conditions in Turkey. European Journal of Oncology Nursing, 13(5), 368–375. https://doi.org/10.1016/j.ejon.2009.04.004
Blaževičienė, A., Newland, J.A., Čivinskienė, V., & Beckstrand, R.L. (2017). Oncology nurses’ perceptions of obstacles and role at the end-of-life care: Cross sectional survey. BMC Palliative Care, 16, 74. https://doi.org/10.1186/s12904-017-0257-1
Connolly, S.L., Miller, C.J., Lindsay, J.A., & Bauer, M.S. (2020). A systematic review of providers’ attitudes toward telemental health via videoconferencing. Clinical Psychology: Science and Practice, 27(2), e12311. https://doi.org/10.1111/cpsp.12311
Easton, S., & Van Laar, D. (2018). User manual for the Work-Related Quality of Life (WRQOL) Scale: A measure of quality of working life (2nd ed.). University of Portsmouth. https://doi.org/10.17029/EASTON2018
Eche, I.J., Phillips, C.S., Alcindor, N., & Mazzola, E. (2022). A systematic review and meta-analytic evaluation of moral distress in oncology nursing. Cancer Nursing. Advance online publication. https://doi.org/10.1097/NCC.0000000000001075
Ghawadra, S.F., Abdullah, K.L., Choo, W.Y., & Phang, C.K. (2019). Psychological distress and its association with job satisfaction among nurses in a teaching hospital. Journal of Clinical Nursing, 28(21–22), 4087–4097. https://doi.org/10.1111/jocn.14993
Güner, P., Hiçdurmaz, D., Kocaman Yıldırım, N., & İnci, F. (2018). Psychosocial care from the perspective of nurses working in oncology: A qualitative study. European Journal of Oncology Nursing, 34, 68–75. https://doi.org/10.1016/j.ejon.2018.03.005
Hakanen, J.J., & Schaufeli, W.B. (2012). Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. Journal of Affective Disorders, 141(2–3), 415–424. https://doi.org/10.1016/j.jad.2012.02.043
Hammond, N.E., Crowe, L., Abbenbroek, B., Elliott, R., Tian, D.H., Donaldson, L.H., . . . Delaney, A. (2021). Impact of the coronavirus disease 2019 pandemic on critical care healthcare workers’ depression, anxiety, and stress levels. Australian Critical Care, 34(2), 146–154. https://doi.org/10.1016/j.aucc.2020.12.004
Harris, P.A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J.G. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Karacin, C., Bilgetekin, I., Basal, F.B., & Oksuzoglu, O.B. (2020). How does COVID-19 fear and anxiety affect chemotherapy adherence in patients with cancer. Future Oncology, 16(29), 2283–2293. https://doi.org/10.2217/fon-2020-0592
Kubota, Y., Okuyama, T., Uchida, M., Umezawa, S., Nakaguchi, T., Sugano, K., . . . Akechi, T. (2016). Effectiveness of a psycho-oncology training program for oncology nurses: A randomized controlled trial. Psycho-Oncology, 25(6), 712–718. https://doi.org/10.1002/pon.4000
Labrague, L.J., & de Los Santos, J.A.A. (2021). Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. Journal of Nursing Management, 29(3), 395–403. https://doi.org/10.1111/jonm.13168
Lebni, J.Y., Toghroli, R., Abbas, J., Kianipour, N., NeJhaddadgar, N., Salahshoor, M.R., . . . Ziapour, A. (2020). Nurses’ work-related quality of life and its influencing demographic factors at a public hospital in western Iran: A cross-sectional study. International Quarterly of Community Health Education, 42(1), 37–45. https://doi.org/10.1177/0272684X20972838
Liang, W., Guan, W., Chen, R., Wang, W., Li, J., Xu, K., . . . He, J. (2020). Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncology, 21(3), 335–337. https://doi.org/10.1016/S1470-2045(20)30096-6
Lovibond, P.F., & Lovibond, S.H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. https://doi.org/10.1016/0005-7967(94)00075-u
Melnyk, B.M., Orsolini, L., Tan, A., Arslanian-Engoren, C., Melkus, G.D., Dunbar-Jacob, J., . . . Lewis, L.M. (2018). A national study links nurses’ physical and mental health to medical errors and perceived worksite wellness. Journal of Occupational and Environmental Medicine, 60(2), 126–131. https://doi.org/10.1097/JOM.0000000000001198
Nwozichi, C.U., Guino-o, T.A., Madu, A.M., Hormazabal-Salgado, R., Jimoh, M.A., & Arungwa, O.T. (2020). The troubled nurse: A qualitative study of psychoemotional effects of cancer care on nurses in a Nigerian care setting. Asia-Pacific Journal of Oncology Nursing, 7(4), 328–335. https://doi.org/10.4103/apjon.apjon_25_20
Paterson, C., Gobel, B., Gosselin, T., Haylock, P.J., Papadopoulou, C., Slusser, K., . . . Pituskin, E. (2020). Oncology nursing during a pandemic: Critical reflections in the context of COVID-19. Seminars in Oncology Nursing, 36(3), 151028. https://doi.org/10.1016/j.soncn.2020.151028
Phillips, C.S., Becker, H., & Gonzalez, E. (2021). Psychosocial well-being: An exploratory cross-sectional evaluation of loneliness, anxiety, depression, self-compassion, and professional quality of life in oncology nurses. Clinical Journal of Oncology Nursing, 25(5), 530–538. https://doi.org/10.1188/21.CJON.530-538
Pitman, A., Suleman, S., Hyde, N., & Hodgkiss, A. (2018). Depression and anxiety in patients with cancer. BMJ, 361, k1415. https://doi.org/10.1136/bmj.k1415
Rezaee, N., Mardani-Hamooleh, M., & Ghaljeh, M. (2019). Ethical challenges in cancer care: A qualitative analysis of nurses’ perceptions. Research and Theory for Nursing Practice, 33(2), 169–182. https://doi.org/10.1891/1541-6577.33.2.169
Rosa, W.E., Dahlin, C., Battista, V., Finlayson, C.S., Wisniewski, R.E., Greer, K., & Ferrell, B.R. (2021). Primary palliative care clinical implications: Oncology nursing during the COVID-19 pandemic. Clinical Journal of Oncology Nursing, 25(2), 119–125. https://doi.org/10.1188/21.CJON.119-125
Rosa, W.E., Schlak, A.E., & Rushton, C.H. (2020). A blueprint for leadership during COVID-19. Nursing Management, 51(8), 28–34. https://doi.org/10.1097/01.NUMA.0000688940.29231.6f
Sarapultseva, M., Zolotareva, A., Kritsky, I., Nasretdinova, N., & Sarapultsev, A. (2021). Psychological distress and post-traumatic symptomatology among dental healthcare workers in Russia: Results of a pilot study. International Journal of Environmental Research and Public Health, 18(2). https://doi.org/10.3390/ijerph18020708
Saygili, M., Avci, K., & Sönmez, S. (2020). Quality of work life and burnout in healthcare workers in Turkey. Journal of Health Management, 22(3), 317–329. https://doi.org/10.1177/0972063420938562
Shah, M.K., Gandrakota, N., Cimiotti, J.P., Ghose, N., Moore, M., & Ali, M.K. (2021). Prevalence of and factors associated with nurse burnout in the US. JAMA Network Open, 4(2), e2036469. https://doi.org/10.1001/jamanetworkopen.2020.36469
Shahrour, G., & Dardas, L.A. (2020). Acute stress disorder, coping self-efficacy and subsequent psychological distress among nurses amid COVID-19. Journal of Nursing Management, 28(7), 1686–1695. https://doi.org/10.1111/jonm.13124
Shaukat, N., Ali, D.M., & Razzak, J. (2020). Physical and mental health impacts of COVID-19 on healthcare workers: A scoping review. International Journal of Emergency Medicine, 13(1), 40. https://doi.org/10.1186/s12245-020-00299-5
Shechter, A., Diaz, F., Moise, N., Anstey, D.E., Ye, S., Agarwal, S., . . . Abdalla, M. (2020). Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. General Hospital Psychiatry, 66, 1–8. https://doi.org/10.1016/j.genhosppsych.2020.06.007
Shih, T.-H., & Fan, X. (2008). Comparing response rates from web and mail surveys: A meta-analysis. Field Methods, 20(3), 249-271. https://doi.org/10.1177/1525822X08317085
Shipman, C., Burt, J., Ream, E., Beynon, T., Richardson, A., & Addington-Hall, J. (2008). Improving district nurses’ confidence and knowledge in the principles and practice of palliative care. Journal of Advanced Nursing, 63(5), 494–505. https://doi.org/10.1111/j.1365-2648.2008.04729.x
Shukla, K., Shahane, S., & D’Souza, W. (2017). Role of demographic and job-related variables in determining work-related quality of life of hospital employees. Journal of Postgraduate Medicine, 63(1), 4–10. https://doi.org/10.4103/0022-3859.192794
Si, M.-Y., Su, X.-Y., Jiang, Y., Wang, W.-J., Gu, X.-F., Ma, L., . . . Qiao, Y.-L. (2020). Psychological impact of COVID-19 on medical care workers in China. Infectious Diseases of Poverty, 9, 113. https://doi.org/10.1186/s40249-020-00724-0
Song, X., Fu, W., Liu, X., Luo, Z., Wang, R., Zhou, N., . . . Lv, C. (2020). Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain, Behavior, and Immunity, 88, 60–65. https://doi.org/10.1016/j.bbi.2020.06.002
Tsaras, K., Papathanasiou, I.V., Mitsi, D., Veneti, A., Kelesi, M., Zyga, S., & Fradelos, E.C. (2018). Assessment of depression and anxiety in breast cancer patients: Prevalence and associated factors. Asian Pacific Journal of Cancer Prevention, 19(6), 1661–1669. https://doi.org/10.22034/APJCP.2018.19.6.1661
Tsehay, M., Belete, A., & Necho, M. (2020). Factors associated with psychological distress and brief resilient coping level during the COVID-19 pandemic among health-care professionals in Dessie, Ethiopia. Psychology Research and Behavior Management, 13, 1213–1221. https://doi.org/10.2147/PRBM.S288562
U.S. Department of Health and Human Services. (2019). 2018 National Sample Survey of Registered Nurses: Brief summary of results. Rockville, MD. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-r…
Wang, Y.-X., Guo, H.-T., Du, X.-W., Song, W., Lu, C., & Hao, W.-N. (2020). Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine (Baltimore), 99(26), e20965. https://doi.org/10.1097/MD.0000000000020965
Weiss, D.S., & Marmar, C.R. (1996). The Impact of Event Scale-Revised. In J. Wilson & T.M. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 399-411). Guilford.
World Health Organization. (2021). Global patient safety action plan 2021–2030. https://www.who.int/publications/i/item/9789240032705
Yu, F., Raphael, D., Mackay, L., Smith, M., & King, A. (2019). Personal and work-related factors associated with nurse resilience: A systematic review. International Journal of Nursing Studies, 93, 129–140. https://doi.org/10.1016/j.ijnurstu.2019.02.014
Zhang, C., Peng, D., Lv, L., Zhuo, K., Yu, K., Shen, T., . . . Wang, Z. (2020). Individual perceived stress mediates psychological distress in medical workers during COVID-19 epidemic outbreak in Wuhan. Neuropsychiatric Disease and Treatment, 16, 2529–2537. https://doi.org/10.2147/NDT.S266151
Zhao, F., Ahmed, F., & Faraz, N.A. (2020). Caring for the caregiver during COVID-19 outbreak: Does inclusive leadership improve psychological safety and curb psychological distress? A cross-sectional study. International Journal of Nursing Studies, 110, 103725. https://doi.org/10.1016/j.ijnurstu.2020.103725

