Transitions of Male Partners of Women With Breast Cancer: Hope, Guilt, and Quality of Life
Purpose/Objectives: To (a) describe the types of transitions experienced by male spousal caregivers of women with breast cancer and the strategies used by male spouses to deal with these transitions and (b) examine factors related to their quality of life, including demographic variables, self-efficacy, caregiver guilt, hope, the quality of life of their partner with breast cancer, and transitions.
Design: Cross-sectional, transformational, mixed-methods approach.
Setting: Participants’ homes.
Sample: 105 dyads of male spouses and their female partners diagnosed with stages I–III breast cancer.
Methods: 600 surveys were mailed to women with breast cancer and their male partners. Significant variables were entered into a multivariate model.
Main Research Variable: Male caregiver quality of life.
Findings: The quality of life of male spouse participants was positively influenced by hope (p < 0.01). It was negatively influenced by caregiver guilt scores (p < 0.01) and the method of dealing with their transitions by “doing what needs to be done” (p = 0.04).
Conclusions: The male caregivers with higher quality-of- life scores reported higher hope and lower caregiver guilt scores. They reported lower quality-of-life scores if they dealt with transitions by “doing what needs to be done.”
Implications for Nursing: Strategies to support male spouses of women with breast cancer should involve ways to foster hope, reduce feelings of guilt, and encourage male caregivers to engage more in supporting their spouses.
Jump to a section
Breast cancer is the second most prevalent type of cancer in the world, with more than one million new cases of breast cancer diagnosed every year (World Health Organization, 2014). Men frequently provide physical and psychological care and support to their partners with breast cancer (American Cancer Society, 2014; Canadian Cancer Society’s Advisory Committee on Cancer Statistics, 2014). A diagnosis of breast cancer affects not only the women with breast cancer, but also their male partners, resulting in considerable changes to their lives (Zahlis & Lewis, 2010). How family caregivers deal with these transitions has an impact on their quality of life (Duggleby, Swindle, Peacock, & Ghosh, 2011). Significant changes or transitions are disruptive to the individual, and they often result in distress and feelings of loss (Meleis, Sawyer, Im, Hilfinger Messias, & Schumacher, 2010). Male spouses of women with breast cancer experience significant levels of distress and disruptions in their sleep, eating habits, and ability to work (Fitch & Allard, 2007). Although a growing body of literature that describes factors influencing the quality of life of male spouses exists, no published study has specifically considered how their quality of life is affected by the types of transitions that accompany caregiving for a spouse with breast cancer, as well as how they deal with these transitions.
Studies exploring the experience of male spouses of women with breast cancer suggest that they undergo multiple concurrent transitions. For example, in a qualitative study involving 48 spouses of newly diagnosed women with breast cancer, the spouses described changes in their relationships with their wives, as well as in their communication, roles, and hope (Zahlis & Lewis, 2010). Participants described how the diagnosis either brought the couple closer or made their relationship more difficult. The diagnosis also affected their communication (positively and negatively) and their physical relationship, and it changed their relationships with their children. Significant changes in relationships were also reported in other qualitative studies of male spouses of women with breast cancer (Northouse, 1989; Zahlis & Shands, 1991).
Another transition experienced by male spouses of women with breast cancer was that of changes in roles. Following the diagnosis, male spouses often took on unfamiliar physical and caregiving tasks for their wives in addition to changing their work schedules, performing more child care, and assuming management of the household (Northouse, 1989; Zahlis & Lewis, 2010). Participants in a qualitative study of the hope experience of male spouses of women with breast cancer described the loss of hope as a significant transition. They described their loss of hope in relation to their relationships with their wives and their goals for the future (Duggleby, Bally, Cooper, Doell, & Thomas, 2012). This loss of hope resulted in feelings of helplessness, lack of control, and distress.
Few studies have examined specific factors that influence the quality of life of male spouses (Alacacioglu, Yavuzsen, Dirioz, & Yilmaz, 2009; Awadalla et al., 2007; Duggleby, Doell, Cooper, Thomas, & Ghosh, 2014; Kim et al., 2008; Northouse et al., 2002; Wagner, Bigatti, & Storniolo, 2006). In a study of 110 male spouses of women with breast cancer, predictor variables of quality of life included age, hope, feelings of guilt, general self-efficacy (confidence in their ability to deal with difficult situations), and the quality of life of their family members with breast cancer (Duggleby et al., 2014). Male spouses with higher quality-of-life scores were older, and they had more hope and general self-efficacy and less guilt. In addition, their partners had higher quality-of-life scores.
Findings from other studies also address factors influencing the quality of life of male spouses. For example, Awadalla et al. (2007) found, in a study of family caregivers of outpatients with breast or gynecologic cancers, that older male caregivers had higher quality-of-life scores than their younger counterparts. In addition, Northouse et al. (2002) determined, in a study of 189 patient-family dyads, that family caregivers with more self-efficacy reported less hopelessness and negative appraisal of their caregiving, as well as better quality of life. Mental health was also significantly related to caregivers’ quality of life in a study of 168 couples dealing with breast or prostate cancer (Kim et al., 2008). As such, the few existing studies suggest that multiple factors influence the quality of life of male spouses of women with breast cancer, but that significant gaps exist in the knowledge of transitions and quality of life.
The purpose of this study was to examine the quality of life of male spouses of women with breast cancer and its relationship to (a) the types of transitions male spouses experienced and the strategies they used to deal with these changes and (b) demographic variables, self-efficacy, caregiver guilt and hope, and the quality of life of their partners with breast cancer.
Methods
A cross-sectional, transformational, mixed-methods approach, in which the emphasis was on quantitative and qualitative data, was adopted (Creswell & Plano Clark, 2007). Data were collected concurrently using quantitative questionnaires and an open-ended qualitative survey. Qualitative data were analyzed separately using content analysis, then transformed into quantitative measures using Krippendorff’s (2004) content analysis technique. All data were combined and analyzed. This study received ethical approval from the Alberta Cancer Research Ethics Board.
Inclusion criteria for the study were women with breast cancer (stages I–III) and male partners (spouses or common-law partners) who were living with and had a legal relationship with women with breast cancer. All participants were required to be aged 18 years or older and able to read English.
The study required a sample size of 98 for six independent variables (i.e., quality of life of women with breast cancer, and male spouses’ general self-efficacy, guilt, hope, age, and transitions) (Cohen, 1977). The dependent variable was participants’ quality of life, which was measured on a continuous scale.
Alberta Cancer Registry personnel mailed 600 survey packages in December 2012. Women with breast cancer (stages I–III) who had listed a man as their next of kin on their admission form when they were admitted to a cancer facility in 2012 were randomly selected for the mail-out. Packages included a letter of introduction to the study; demographic forms; questionnaires; an open-ended, qualitative transitions survey; and a $5 coffee gift certificate. The study package was addressed to women with breast cancer and contained instructions for them to ask their male partners to complete the demographic forms, questionnaires, and surveys. The following survey instruments were used: (a) Herth Hope Index (HHI) to measure hope, (b) General Self-Efficacy Scale (GSES) to measure self-efficacy, (c) Caregiver Guilt Questionnaire (CGQ) to measure guilt, (d) Caregiver Quality of Life–Cancer (CQOL-C) to measure the quality of life of male spouses, and (e) Functional Assessment of Cancer Therapy–Breast (FACT-B) to measure the quality of life of women with breast cancer. Study participants were asked to return their survey materials using the prepaid envelope included in the package. To facilitate a higher response rate, reminder cards were distributed four and eight weeks after the initial mail-out (Dillman, 2007). The return of surveys implied informed consent.
Caregiver Guilt Questionnaire: The CGQ measures the guilt experienced by male spouse caregivers (Losada, Márquez-González, Peñacoba, & Romero-Moreno, 2010). This 22-item scale measures guilt on a five-point Likert-type scale that ranges from 0 (never) to 4 (always), with total scores ranging from 0–88. A higher score indicates that the respondent experienced more feelings of guilt related to his caregiving. The CGQ has a reported internal consistency of r = 0.88 and a convergent validity of r = 0.65 (p < 0.001) (Roach, Laidlaw, Gillanders, & Quinn, 2013). The Cronbach alpha, measuring internal consistency, was 0.93.
Caregiver Quality of Life–Cancer: The CQOL-C is a 35-item questionnaire measuring subjective quality of life on a five-point Likert-type scale that ranges from 0 (not at all) to 4 (very much); total scores range from 0–140 (Weitzner, Jacobsen, Wagner, Friedland, & Cox, 1999). The CQOL-C measures respondents’ perception of burden, disruptiveness, and financial concerns, as well as their positive adaptation in the face of spousal illness. A higher score on the CQOL-C indicates a higher quality of life. The test-retest reliability of the CQOL-C was found to be r = 0.95, with an internal consistency of r = 0.91 (Weitzner et al., 1999). The Cronbach alpha was 0.91.
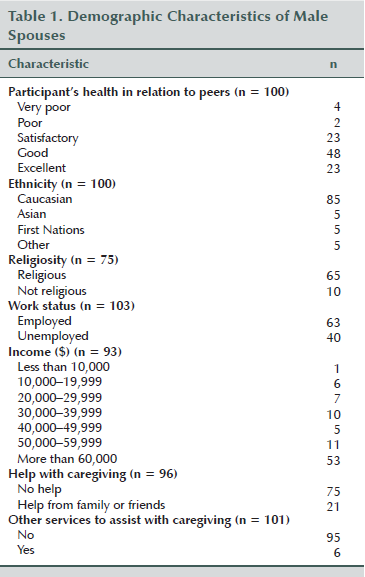
Demographics
Demographic characteristics obtained from the male spouse included age, years of education, years of marriage, ethnicity, religious affiliation, occupation, income, and number and type of medical conditions. Male spouses were also asked if they had received help with caregiving from family or friends, whether they had used other services to assist with caregiving, and about their relative health in comparison to their peers. Women with breast cancer also filled out a demographic form to measure their age, date of diagnosis, specifics of breast cancer diagnosis, stage of disease, whether they were in treatment, other medical diagnoses, and occupational status.
Functional Assessment of Cancer Therapy–Breast: The FACT-B, a 44-item scale, assesses the multidimensional nature of quality of life of patients with breast cancer using a five-point Likert-type scale ranging from 0 (not at all) to 4 (very much) (Brady et al., 1997). The FACT-B measures physical, social, emotional, and functional components of well-being, as well as items specific to quality of life in breast cancer with a breast cancer subscale. A higher score indicates a higher quality of life. The FACT-B has been reported to be a reliable (internal consistency of r = 0.9 and test-retest reliability of r = 0.85) and valid (construct validity of r = 0.87, p < 0.01) measure of quality of life in women with breast cancer (Brady et al., 1997). The Cronbach alpha was 0.93.
General Self-Efficacy Scale: The GSES is an instrument that focuses on the perceived self-efficacy of one’s ability to perform difficult tasks or, in the case of the current study, to care for and cope with the adversity of having a spouse with breast cancer (Schwarzer & Jerusalem, 1995). This scale consists of 10 questions measured on a four-point Likert-type scale ranging from 1 (not true at all) to 4 (exactly true); total scores range from 10–40. A higher score on the GSES indicates that the participant is confident in his ability to cope with unexpected events and in the efficacy of his problem-solving strategies. The internal consistency of the GSES has been reported to be r = 0.88 and its test-retest reliability to be r = 0.82 (Leganger, Kraft, & Røysamb, 2000). Construct validity was reported as r = 0.29 (p < 0.01). The Cronbach alpha was 0.89.
Herth Hope Index: The HHI measures the subjective feelings of hope in adults in the clinical setting (Herth, 1992). This 12-item questionnaire uses a four-point Likert-type scale that ranges from 1 (strongly disagree) to 4 (strongly agree) to measure the multifaceted characteristics of hope as a concept with consistency, validity, and reliability across variable ages, backgrounds, and genders (Herth, 1992). The HHI assesses hope across three factors: temporality and the future, positive readiness and expectancy, and interconnectedness. Total scores range from 12–48, with a higher score indicating a higher level of reported hope. HHI has reported reliability (test-retest is r = 0.91, p < 0.05) and validity (concurrent, r = 0.84; p < 0.05; criterion, r = 0.92, p < 0.05; divergent, r = –0.73, p < 0.05) (Herth, 1992). The Cronbach alpha was 0.89.
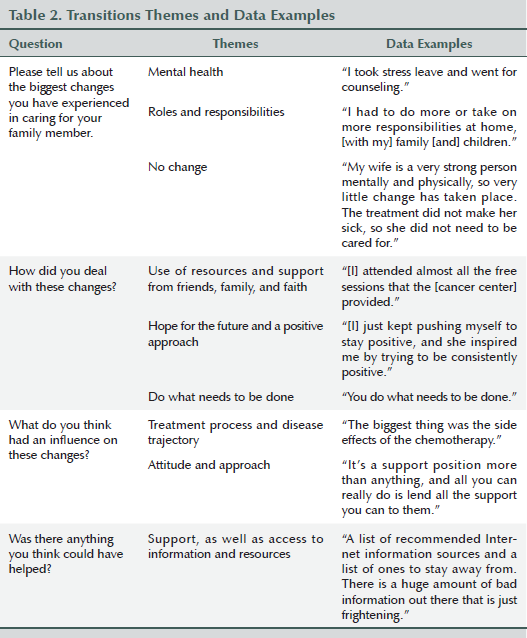
The study package also included an open-ended transitions survey for male caregivers. This survey had been used in a previous study regarding transitions (Duggleby et al., 2011) and was developed based on questions used in a qualitative research study about transitions. Survey prompts were, “Please tell us about the biggest changes you have experienced in caring for your family member,” “How did you deal with these changes?”, “What do you think had an influence on these changes?”, and, “Was there anything you think could have helped?” The qualitative survey concluded with space for participants to write additional comments about their experiences.
Qualitative data from the transitions survey were transcribed. Data were analyzed for each question separately using Krippendorff’s (2004) content analysis technique. Themes were then developed for each question. The themes reflected the responses to the questions and were assigned a value in SPSS®, version 18.0. For each participant, the main theme reflected in his answer was entered into SPSS alongside the other quantitative measures. For example, in response to the first question—“Please tell us about the biggest challenges you have experienced in caring for your family member”—two themes were identified using content analysis: (a) transitions in mental health and (b) transitions in roles and responsibilities. In the SPSS file, the variable transitions was assigned two codes (1 = mental health; 2 = roles and responsibilities). The researchers then went back to each participant survey and coded the response to that question based on the most prevalent answer.
Quantitative data also were entered into SPSS. Scores for quality of life, hope, caregiver guilt, general self-efficacy, and quality of life of women with breast cancer were described using descriptive statistics. Variables were then assessed for linearity, normal distribution, and homoscedasticity by examining bivariate scatterplots, histograms, and measures of skewness and kurtosis (Tabachnick & Fidell, 2007). The correlation matrix indicated no issues related to multicollinearity. The dependent variable was quality of life (CQOL-C). Independent variables were demographic variables (e.g., age); male partners’ hope, caregiver guilt, and general self-efficacy; and quality of life of women with breast cancer. To determine relationships between independent variables and the outcome variable of CQOL-C total scores, a general linear model (GLM) was used. GLM, an extension of the linear regression method, can handle categorical, count, and continuous data as the response variable (Nelder & Wedderburn, 1972). First, each independent variable was entered separately for the univariate analysis. Those variables that were significant at the p < 0.1 level were included in the multivariate model analysis. In the multivariate analysis, statistical significance was set at p < 0.05. Statistical data analysis was performed by the principal investigator and a co-investigator who is a biostatistician.
Findings
One hundred and five participant dyads took part in the current study (18% response rate). Male spouse participants were generally older, with an average age of 61.12 years (SD = 11.9), whereas their female partners were slightly younger, with an average age of 58.75 years (SD = 11.34). The couples had been married an average of 31.64 years (SD = 15). Thirty-four of the participating women with breast cancer (34%) were receiving treatment, and 67 women (66%) were not. At the time of diagnosis, 29% of women (n = 20) were diagnosed as stage I, 42% (n = 29) were diagnosed as stage II, and 29% (n = 20) were diagnosed as stage III. The average time since diagnosis was 32.32 months (SD = 55.15), with a range of 9–339 months. Table 1 presents additional demographic information about the male spouse participants.
Transitions
Although some male spouses (n = 10) did not perceive any changes following their wife’s diagnosis, many described significant transitions, including changes in their roles and responsibilities (n = 41) and to their mental health (n = 21). Changes in roles and responsibilities included taking on more household activities and becoming a caregiver. The male spouses described changes in their mental health after the diagnosis prompted feelings of fear, sadness, and uncertainty. They dealt with these changes by using available resources (n = 27), maintaining hope and a positive approach (n = 18), and “doing what needs to be done,” or focusing only on essential caregiving tasks (n = 22). The biggest influences on their transitions were their wives’ disease trajectory and treatment process (n = 31) and their own attitude and approach (n = 23). Some participants (n = 34) said they felt that more support for male spouses (e.g., access to information and resources) would have helped, whereas others said nothing would have helped them (n = 11). Table 2 presents data examples for these findings. Chi-square analysis was used to determine if any significant relationships existed among the types of transitions experienced and how participants dealt with the transitions, as well as what they felt influenced them and what would have helped them. No significant associations were found.
Main Variables
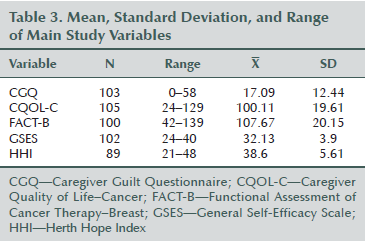
Table 3 presents the means, standard deviations, and ranges of the current study’s main variables. The univariate analysis results suggested the quality of life of women with breast cancer (FACT-B) (p < 0.01) was significantly positively associated with their male partners’ quality-of-life scores (CQOL-C). Hope (HHI) (p < 0.01) and general self-efficacy (GSES) (p < 0.01) were also found to have significant positive relationships. Caregiver guilt (CGQ) (p < 0.01) and dealing with transitions by “doing what needs to be done” (p = 0.04) had a significant negative association. These variables were included in the multivariate analysis. Other transition themes and demographic variables did not produce statistically significant relationships in the univariate analysis and, as a result, were not included in the multivariate analysis.
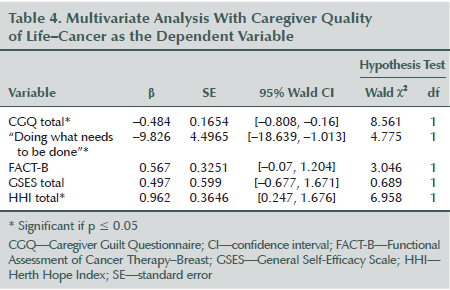
Using GLM, significant factors influencing CQOL-C scores for male study participants included caregiver guilt (p < 0.01), hope (p < 0.01), and “doing what needs to be done” (p = 0.03) (see Table 4). The quality of life of male caregivers increased as their hope increased and their guilt decreased. It also decreased when they dealt with significant transitions by “doing what needs to be done.” GSES and FACT-B scores did not have a statistically significant association with quality of life in the multivariate analysis.
Discussion
Male partners of women with breast cancer reported they had a higher quality of life when they reported feeling more hope and less guilt. They reported a lower quality of life when they dealt with their significant changes by “doing what needs to be done.” As a model predicting the quality of life of male partners of women with breast cancer, these findings are unique and have not been reported elsewhere.
A significant association between male spouses’ hope and perceptions of guilt has also been reported in a quality-of-life study that involved 110 male spouses of women with breast cancer (Duggleby et al., 2014). In that study, significant predictors of the male spouses’ quality of life included hope, general self-efficacy, perceptions of guilt, and the quality of life of the women with breast cancer for whom they cared. However, in this study, general self-efficacy and the quality of life of the women with breast cancer were significant at the univariate level, but these associations were not found in the multivariate analysis. These differences in findings may be related to sample differences. For example, FACT-B scores in Duggleby et al.’s (2014) study were slightly higher (114.9, SD = 17.7) than in the current study (107.24, SD = 3.35). The differences may also be related to sample size. Although the sample size of the current study was adequate for the number of variables, a larger sample size may have found significance at the multivariate level for FACT-B and general self-efficacy. In addition, Duggleby et al. (2014) did not include transitions as a variable. The addition of the transitions survey answers may have affected interactions in the model.
The significant influence of caregiver guilt on the quality of life of male spouses of women with breast cancer has been reported on in only one other study (Duggleby et al., 2014). Feelings of guilt have also been reported as a factor contributing to quality of life in other populations (Losada et al., 2010; Spillers, Wellisch, Kim, Matthews, & Baker, 2008). Spillers et al. (2008) reported an inverse relationship of caregiving competence and caregiver guilt in family caregivers of survivors of cancer. Losada et al. (2010) found a significant positive association between caregiver guilt and burden, depression, and distress in family caregivers of individuals with Alzheimer disease. Caregivers may feel guilt when they think they have not done enough and cannot deal with caregiving demands (Erlingsson, Magnusson, & Hanson, 2012). Future research should explore further the concept of caregiver guilt with male spouses of women with breast cancer.
The positive influence of hope on the quality of life of male spouses is part of the growing evidence that supports the importance of hope in this population. Hope has been found to have a significant positive association with caregiver quality of life in (a) male spouses of women with breast cancer (Duggleby et al., 2014), (b) family caregivers of individuals with dementia (Acton, 2002; Duggleby et al., 2011), and (c) rural women caregivers of individuals with advanced cancer (Duggleby et al., 2014). In a qualitative study of the experience of hope of male spouses of women with breast cancer, participants described hope as a psychosocial resource essential to their continued support of their wives (Duggleby et al., 2012). Hope gave them courage and confidence in their ability to deal with difficult situations associated with caregiving.
Of importance in the current study was the finding that dealing with transitions by “doing what needs to be done” had a negative association with male spouses’ quality of life. “Doing what needs to be done” may be a reflection of a minimal engagement in caregiving. This strategy may appear on the surface to be a practical way of coping, but the authors’ findings suggest otherwise. More specifically, these findings suggest that minimal engagement in caregiving may result in a reduction of quality of life. In a qualitative study of male spouses of women with breast cancer within the first six months after diagnosis, study participants described “doing what needs to be done and what could be done” (Zahlis & Lewis, 2010). An important distinction is that this statement describes not only “doing what needs to be done” but also possibly a more engaged approach of “doing what could be done.” Zahlis and Lewis’s (2010) participants described needing to make adjustments to deal with and move through their experience. The current study did not determine whether participants were able to make adjustments to deal with their experience. Future research should explore how encouraging male spouses to be more engaged with their partner’s experience positively influences their quality of life.
Limitations
The results of this study should be considered in the light of several limitations regarding sample and methodology. The sample was older, as well as in relatively good health and with middle-class incomes (i.e., 50% had incomes greater than $60,000). Therefore, male spouses with poorer health and lower incomes may have produced different results. Most of the women had been diagnosed with stage II breast cancer. Taken together, these sample characteristics and the poor response rate affect the generalizability of the data. Although the sample size was adequate, other variables may have been significant in the analysis had the sample size been larger. Future studies with larger and more representative samples should be conducted. In addition, the study design was cross-sectional; therefore, changes in transitions and quality of life over time were not determined. Because the significant predictors of quality of life could change over time, future studies should be longitudinal in nature.
Implications for Nursing
The findings of this study have significant implications for nursing practice. For example, they suggest that identifying spouses who are at a higher risk for having difficulty dealing with their transitions is important. The current study’s data indicate that spouses at a higher risk are those who perceive loss of hope, feel guilty, and are less engaged in the care of their spouses with breast cancer. Creating assessments of guilt and hope would be a first step in establishing the demand for psychosocial support. Next, developing various strategies to decrease feelings of guilt and foster hope would also enhance psychosocial care and may improve quality of life. Some interventions for hope exist, but they are not yet widely implemented. Further explorations of the complexity of transitions for male spouses across a variety of social strata, as well as the impact of transitions on quality of life, would also be beneficial. In addition, new interventions and support programs need to be developed that support male spouses; these must reflect their unique needs and recognize the range in responses to their spouses’ experiences with breast cancer.
[[{"type":"media","view_mode":"media_original","fid":"19596","attributes":{"alt":"","class":"media-image","height":"218","typeof":"foaf:Image","width":"365"}}]]
Conclusions
This study was a first step toward gaining an understanding of transitions experienced by male spouses of women with breast cancer and their influence on quality of life. The suggestion that male spouses have a better quality of life by being more engaged with the care of their spouses, and that they feel less guilt and have more hope, provides insight into how best to develop ways to support this population. The findings also provide a foundation for future research to further understand transitions and feelings of guilt in this population.
References
Acton, G.J. (2002). Health-promoting self-care in family caregivers. Western Journal of Nursing Research, 24, 73–86. doi:10.1177/01939450222045716
Alacacioglu, A., Yavuzsen, T., Dirioz, M., & Yilmaz, U. (2009). Quality of life, anxiety and depression in Turkish breast cancer patients and in their husbands. Medical Oncology, 26, 415–419. doi:10.1007/s12032-008-9138-z
American Cancer Society. (2014). Cancer facts and figures 2014. Retrieved from http://www.cancer.org/acs/groups/content/@research/documents/webcontent…
Awadalla, A.W., Ohaeri, J.U., Gholoum, A., Khalid, A.O., Hamad, H.M., & Jacob, A. (2007). Factors associated with quality of life of outpatients with breast cancer and gynecologic cancers and their family caregivers: A controlled study. BMC Cancer, 7, 102. doi:10.1186/1471-2407-7-102
Brady, M.J., Cella, D.F., Mo, F., Bonomi, A.E., Tulsky, D.S., Lloyd, S.R., . . . Shiomoto, G. (1997). Reliability and validity of the Functional Assessment of Cancer Therapy–Breast quality-of-life instrument. Journal of Clinical Oncology, 15, 974–986.
Canadian Cancer Society’s Advisory Committee on Cancer Statistics (2014). Canadian cancer statistics 2014. Retrieved from http://www.cancer.ca/~/media/cancer.ca/CW/cancer%20information/cancer%2…
Cohen, J. (1977). Statistical power analysis for the behavioral sciences. New York, NY: Academic Press.
Creswell, J.W., & Plano Clark, V.L. (2007). Designing and conducting mixed methods research. Thousand Oaks, CA: Sage.
Dillman, D.A. (2007). Mail and Internet surveys: The tailored design method. New York, NY: John Wiley and Sons.
Duggleby, W., Bally, J., Cooper, D., Doell, H., & Thomas, R. (2012). Engaging hope: The experiences of male spouses of women with breast cancer. Oncology Nursing Forum, 39, 400–406. doi:10.1188/12.ONF.400-406
Duggleby, W., Doell, H., Cooper, D., Thomas, R., & Ghosh, S. (2014). The quality of life of male spouses of women with breast cancer: Hope, self-efficacy and perceptions of guilt. Cancer Nursing, 37, E28–E35. doi:10.1097/NCC.0b013e31827ca807
Duggleby, W.D., Swindle, J., Peacock, S., & Ghosh, S. (2011). A mixed methods study of hope, transitions, and quality of life in family caregivers of persons with Alzheimer’s disease. BMC Geriatrics, 11, 88. doi:10.1186/1471-2318-11-88
Erlingsson, C.L., Magnusson, L., & Hanson, E. (2012). Family caregivers’ health in connection with providing care. Qualitative Health Research, 22, 640–655. doi:10.1177/1049732311431247
Fitch, M.I., & Allard, M. (2007). Perspectives of husbands of women with breast cancer: Impact and response. Canadian Oncology Nursing Journal, 17, 66–78. doi:10.5737/1181912x1726671
Herth, K. (1992). Abbreviated instrument to measure hope: Development and psychometric evaluation. Journal of Advanced Nursing, 17, 1251–1259. doi:10.1111/j.1365-2648.1992.tb01843.x
Kim, Y., Kashy, D.A., Wellisch, D.K., Spillers, R.L., Kaw, C.K., & Smith, T.G. (2008). Quality of life of couples dealing with cancer: Dyadic and individual adjustment among breast and prostate cancer survivors and their spousal caregivers. Annals of Behavioral Medicine, 35, 230–238. doi:10.1007/s12160-008-9026-y
Krippendorff, K. (2004). Content analysis: An introduction to its methodology (2nd ed.). Thousand Oaks, CA: Sage.
Leganger, A., Kraft, P., & Røysamb, E. (2000). Perceived self-efficacy in health behavior research: Conceptualization, measurement and correlates. Psychology and Health, 15, 51–69. doi:10.1080/08870440008400288
Losada, A., Márquez-González, M., Peñacoba, C., & Romero-Moreno, R. (2010). Development and validation of the caregiver guilt questionnaire. International Psychogeriatrics, 22, 650–660. doi:10.1017/S1041610210000074
Meleis, A.I., Sawyer, L.M., Im, E.O., Hilfinger Messias, D.K., & Schumacher, K. (2010). Experiencing transitions: An emerging middle-range theory. In A.I. Meleis (Ed.), Transitions theory: Middle-range and situation-specific theories in nursing research and practice (pp. 52–65). New York, NY: Springer.
Nelder, J.A., & Wedderburn, R.W.M. (1972). Generalized linear models. Journal of Royal Statistical Society. Series A (General), 135, 370–384.
Northouse, L. (1989). A longitudinal study of the adjustment of patients and husbands to breast cancer. Oncology Nursing Forum, 16, 511–516.
Northouse, L.L., Mood, D., Kershaw, T., Schafenacker, A., Mellon, S., Walker, J., . . . Decker, V. (2002). Quality of life of women with recurrent breast cancer and their family members. Journal of Clinical Oncology, 20, 4050–4064. doi:10.1200/JCO.2002.02.054
Roach, L., Laidlaw, K., Gillanders, D., & Quinn, K. (2013). Validation of the Caregiver Guilt Questionnaire (CGQ) in a sample of British dementia caregivers. International Psychogeriatrics, 25, 2001–2010. doi:10.1017/S1041610213001506
Schwarzer, R., & Jerusalem, M. (1995). Generalized Self-Efficacy scale. In J. Weinman, S. Wright, & M. Johnston (Eds.), Measures in health psychology: A user’s portfolio. Causal and control beliefs (pp. 35–37). Windsor, UK: NFER-NELSON.
Spillers, R.L., Wellisch, D.K., Kim, Y., Matthews, B.A., & Baker, F. (2008). Family caregivers and guilt in the context of cancer care. Psychosomatics, 49, 511–519. doi:10.1176/appi.psy.49.6.511
Tabachnick, B.G., & Fidell, L.S. (2007). Using multivariate statistics (5th ed.). Boston, MA: Pearson Education.
Wagner, C.D., Bigatti, S.M., & Storniolo, A.M. (2006). Quality of life of husbands of women with breast cancer. Psycho-Oncology, 15, 109–120. doi:10.1002/pon.928
Weitzner, M.A., Jacobsen, P.B., Wagner, H., Jr., Friedland, J., & Cox, C. (1999). The Caregiver Quality of Life Index–Cancer (CQOLC) scale: Development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Quality of Life Research, 8, 55–63. doi: 10.1023/A:1026407010614
World Health Organization. (2014). Cancer. Retrieved from http://www.who.int/mediacentre/factsheets/fs297/en
Zahlis, E.H., & Lewis, F.M. (2010). Coming to grips with breast cancer: The spouse’s experience with his wife’s first six months. Journal of Psychosocial Oncology, 28, 79–97. doi:10.1080/07347330903438974
Zahlis, E.H., & Shands, M.E. (1991). Breast cancer: Demands of the illness on the patient’s partner. Journal of Psychosocial Oncology, 9, 75–93. doi:10.1300/J077v09n01_04
About the Author(s)
Wendy Duggleby, PhD, RN, AOCN®, is a professor and nursing research chair of aging and quality of life in the Faculty of Nursing at the University of Alberta in Edmonton; Jasmine Thomas, MA, and Kelly Struthers Montford, MA, are doctoral candidates in the Department of Sociology at the University of Alberta; Roanne Thomas, PhD, is a professor in the School of Rehabilitation Sciences at the University of Ottawa in Ontario and a Canada Research chair in qualitative health research with marginalized populations; Cheryl Nekolaichuk, PhD, is a counseling psychologist at Covenant Health and an associate professor in the Department of Medicine and Dentistry at the University of Alberta; Sunita Ghosh, PhD, is a research scientist at Alberta Health Services; and Ceiwen Cumming, PhD, is a clinical professor and psychologist, and Katia Tonkin, MBBS, FRCP(UK), MD, FRCPC, is a professor, both in the Department of Medicine and Dentistry at the University of Alberta, all in Canada. No financial relationships to disclose. Duggleby can be reached at wendy.duggleby@ualberta.ca, with copy to editor at ONFEditor@ons.org. (Submitted July 2014. Accepted for publication October 1, 2014.)

