Effect of a Nurse-Led Psychoeducational Intervention on Healthcare Service Utilization Among Adults With Advanced Cancer
Purpose/Objectives: To examine differences in healthcare service utilization among patients with advanced cancer participating in a nurse-led psychoeducational intervention.
Design: Secondary analysis of trial data.
Setting: Four Michigan cancer centers.
Sample: 484 patients with advanced cancer.
Methods: Patients were randomized to three groups: brief intervention, extensive intervention, or control. Medical chart review took place at baseline, three months, and six months to measure patients’ healthcare service utilization, defined as emergency department (ED) visits or inpatient hospitalizations. Multivariable logistic regression was used to examine the odds, by study arm, of visiting the ED and being hospitalized, controlling for patient sociodemographic and health status factors, as well as baseline health-related quality of life (QOL).
Main Research Variables: Study arm (brief, extensive, or control), ED visitation (one or more times versus none), inpatient hospitalizations (one or more times versus none), and covariates.
Findings: No significant differences in ED visits or inpatient hospitalizations were observed among study arms. ED visits were more frequent for patients with lung or colorectal cancer, more comorbidities, and lower baseline QOL. Baseline QOL was associated with inpatient hospitalizations in the adjusted analysis.
Conclusions: The psychoeducational intervention, either in brief or extensive format, is unlikely to increase healthcare service utilization.
Implications for Nursing: Efficacious nurse-led psychoeducational interventions to improve QOL do not place undue burdens on the healthcare system and may improve care.
Jump to a section
Healthcare costs in the United States that are attributed to cancer, particularly in the final year of life, are substantial and projected to climb (Mariotto, Yabroff, Shao, Feuer, & Brown, 2011). Expenditures directly associated with cancer treatments (e.g., surgery, chemotherapy, radiation therapy) constitute a large part of these increasing costs, estimated to exceed $100 billion annually (Roehrig, Miller, Lake, & Bryant, 2009). Greater healthcare service utilization, including emergency department (ED) visits and inpatient hospitalizations, are also significant contributors to the growing costs of cancer care (Alemayehu, Buysman, Parry, Becker, & Nathan, 2010; Kutikova et al., 2005; Lang et al., 2009; Vera-Llonch, Weycker, Glass, Gao, Borker, Barber, & Oster, 2011; Vera-Llonch, Weycker, Glass, Gao, Borker, Qin, & Oster, 2011). ED visitation is particularly common among patients with advanced cancer (Barbera, Taylor, & Dudgeon, 2010). ED visits and inpatient hospitalizations can place substantial financial and emotional burdens on patients and families.
Healthcare service utilization among patients is often attributable to the diverse challenges patients face with regard to health-related quality of life (HRQOL) (Barbera et al., 2010). Functional status deficits and symptoms (e.g., pain, dyspnea) are common triggers for patients to seek care through the ED or urgent care (Barbera et al., 2013). Depression and emotional distress are also common in this population (Carlson et al., 2004; Zabora, BrintzenhofeSzoc, Curbow, Hooker, & Piantadosi, 2001) and have been independently associated with excessive healthcare service utilization in prior studies (Himelhoch, Weller, Wu, Anderson, & Cooper, 2004; Unützer et al., 1997).
The report Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis (National Research Council, 2013) emphasized the need for improved management of physical and psychological symptoms for patients with cancer, as well as optimization of care-associated costs. Psychoeducational and psychosocial interventions intended to improve HRQOL have demonstrated favorable efficacy among individuals with advanced cancer (Bakitas et al., 2009; Faller et al., 2013; Northouse et al., 2007; Rehse & Pukrop, 2003). However, despite the large number of these interventions (Faller et al., 2013), their impact on healthcare service utilization among patients with cancer has not been widely studied (Owen, Klapow, Hicken, & Tucker, 2001). Because of this lack of empirical data, understanding of the likely direction of their effect, if any, on healthcare service utilization remains limited.
In the small body of literature that has examined the effect of psychoeducational interventions on healthcare service utilization among patients with cancer, findings are mixed. Some studies have documented decreased healthcare service utilization among patients who received a psychoeducational intervention (Kurtz, Kurtz, Given, & Given, 2006; Rosenberg et al., 2002). Kurtz et al. (2006) found that newly diagnosed patients who received an intervention consisting of 10 contacts with a nurse and focusing on symptom control had fewer ED visits and a trend toward fewer inpatient hospitalizations than control patients.
Other studies have found no effect of psychoeducational interventions on healthcare service utilization (Arving, Brandberg, Feldman, Johansson, & Glimelius, 2014; Bakitas et al., 2009; Björneklett et al., 2013; Lemieux, Topp, Chappell, Ennis, & Goodwin, 2006). Björneklett et al. (2013) offered a one-week residential support intervention to newly diagnosed patients with breast cancer, with a four-day follow-up two months later, and found no difference in the number of primary care visits or medical consultations among patients in the intervention versus control group. Bakitas et al. (2009) observed no effect in use of the intensive care unit or ED by patients undergoing palliative care, compared to controls, following a four-week educational telephone intervention offered by advanced practice nurses (APNs). However, Bakitas et al. (2009) suggested that a more robust in-person intervention may have been needed to see significant effects of the intervention on utilization.
Demonstrating the potential bidirectionality of intervention effects on healthcare service utilization, McCorkle, Jeon, Ercolano, and Schwartz (2011) found that patients with suspected ovarian cancer who received a 16-contact intervention from APNs had significantly fewer primary care visits than patients who received a nine-contact attention-control intervention. Patients who had more sustained contact with APNs may have had their concerns addressed, lessening the need to visit their primary care provider. However, McCorkle et al. (2011) also observed a trend toward increased ED visits among intervention patients versus controls. In addition, McCorkle et al. (2011) reported that APNs instructed patients to follow up on troubling symptoms rather than ignore or minimize them; doing so may have influenced patients’ utilization of the ED.
Taken together, this small group of heterogeneous studies suggests that psychoeducational interventions show potential for attenuating healthcare service utilization among some patients. However, evidence also indicates that interventions have the potential to increase certain types of utilization. Given that patients with advanced cancer tend to use a higher volume of healthcare resources than most other groups (Alemayehu et al., 2010; Lang et al., 2009), further understanding of patterns of healthcare service utilization resulting from psychoeducational interventions in this group is critical.
A randomized, controlled trial (RCT) conducted in 2012 examined psychosocial outcomes of patients with advanced cancer following receipt of a nurse-led intervention offered jointly to patients and their family caregivers (the family involvement, optimistic attitude, coping effectiveness, uncertainty reduction, and symptom management [FOCUS] intervention) compared to a control condition (Northouse et al., 2013). An important aspect of this trial was the evaluation of whether a brief and less resource intensive intervention consisting of three sessions compared favorably with a more extensive six-session version of the intervention. Ultimately, Northouse et al. (2013) found that the brief and extensive interventions demonstrated positive HRQOL outcomes and improved coping behaviors for patients and their caregivers. However, differences in patient healthcare service utilization by intervention arm were not assessed in the original analyses.
To learn more about the effects of the brief and extensive interventions on healthcare service utilization, the current authors conducted a secondary analysis of study data. The specific aims of the current study were (a) to examine differences in healthcare service utilization (i.e., ED visits and inpatient hospitalizations) during a six-month period among patients with advanced cancer who had been randomized to the Brief FOCUS Program, Extensive FOCUS Program, or control condition (usual care) and (b) to assess the association between patient sociodemographic and health-related factors and healthcare service utilization during this six-month period. Because the FOCUS Program was associated with improved HRQOL and coping outcomes, the current authors were particularly interested in evaluating whether the FOCUS Program, in either brief or extensive format, may have led to greater healthcare service utilization compared to controls to achieve those outcomes.
The stress-coping framework that guided the development of the FOCUS intervention also guided the variables that were examined in this study (Folkman & Lazarus, 1980). This framework has been used extensively to explore the impact of serious illness on the psychological state of patients and families (Kim, Han, Shaw, McTavish, & Gustafson, 2010; Yoo et al., 2014). In addition, the framework posits that positive coping behaviors influence downstream outcomes (e.g., emotional well-being, QOL). The primary aim of the current study was to examine the association between FOCUS study arm (an intervention to improve coping) and healthcare service utilization (health behavior). Congruent with the framework, the current authors included several important antecedent variables, including patient demographics, baseline comorbidities, and baseline patient-reported HRQOL.
Methods
Design and Sample
Data for this secondary analysis are from a three-armed RCT of a nurse-led psychoeducational intervention for patients with advanced cancer and their family caregivers. More detailed information about the study, including recruitment, retention, intervention, and primary outcomes, can be found in Northouse et al. (2013).
Study participants consisted of individuals diagnosed with advanced (stage III or IV) breast, colorectal, lung, or prostate cancer. They were eligible for the study if they had a new diagnosis of advanced cancer, progression of their advanced cancer, or a change in the treatment for their cancer in the six months prior to enrollment. Patients were ineligible if their anticipated life expectancy was less than six months (determined by their oncologist), if they were aged 21 years or younger, or if they lived farther than 75 miles from a participating cancer center. Patients also had to have a family caregiver (spouse or nonspouse) who was aged 18 years or older and had not been diagnosed with cancer within the past year.
Procedures
Study participants were informed about the study by clinic staff at four cancer centers in Michigan (University of Michigan Comprehensive Cancer Center in Ann Arbor, Barbara Ann Karmanos Cancer Institute in Detroit, St. Joseph Mercy Cancer Center in Ypsilanti, and Providence Cancer Center in Southfield); they were then contacted by research staff if interested in the study. Data collection occurred in the home after patients and caregivers completed consent forms approved by the institutional review boards at the University of Michigan (coordinating site) and each patient’s cancer center. Patients and caregivers completed instruments separately at baseline (Time 1) prior to the intervention. Patient-caregiver dyads were stratified by patients’ risk for distress (high versus low) based on scores from the Risk for Distress Scale from the Omega Clinical Screening Interview (Worden, 1993). Dyads were also stratified by type of cancer (four types) and cancer center (four sites), and then randomized to one of the study arms (Brief FOCUS, Extensive FOCUS, control). Participants were assessed at baseline (Time 1), at three months (Time 2), and at six months (Time 3). The brief and extensive programs were delivered primarily by master’s-prepared nurses during the three-month interval between Time 1 and Time 2.
Intervention
The FOCUS Program is a home-based intervention that provides education and support to patients with cancer and their family caregivers as a dyad (Northouse, Kershaw, Mood, & Schafenacker, 2005; Northouse et al., 2007). The purpose of the original RCT was to test the relative efficacy of a brief versus extensive version of the FOCUS Program and a control group that received usual care. The Brief FOCUS Program consisted of three nurse-led contacts (two 90-minute home visits and one 30-minute telephone session), whereas the Extensive FOCUS Program consisted of six nurse-led contacts (four 90-minute home visits and two 30-minute telephone sessions).
Instruments
Healthcare service utilization: Healthcare service utilization was assessed in two domains from baseline to six months following study inception: ED visits and inpatient hospitalizations. Utilization data was extracted from each patient’s medical chart by trained research staff members who were blinded to study arm. Appropriate analytic treatment of the utilization variables was determined based on the distributions of each event within the sample. For ED visits, 74% of patients (n = 346) had none, 18% (n = 85) had one, 6% (n = 29) had two, and 2% (n = 10) had three or more. For inpatient hospitalizations, 76% (n = 356) of patients had none, 18% (n = 82) had one, 5% (n = 23) had three, and 2% (n = 9) had four or more. Based on these distributions, ED visits and inpatient hospitalizations were dichotomized separately as “none” versus “one or more times” for analysis.
Demographic and medical information: The Omega Screening Questionnaire (Worden, 1993) was used to obtain demographic and health history information, whereas a researcher-designed questionnaire was used to obtain cancer-related information. Data were categorized as age (aged 64 years or younger versus aged 65 years or older), education (high school diploma or less versus some college or more), marital status (married or partnered versus not married or partnered), annual income ($30,000 or less, $30,001 to $74,999, $75,000 or greater, and no response), race (white, black, other), and gender (male or female). To account for noncancer-related health status, adjusted analyses controlled for number of self-reported comorbidities at baseline. This was categorized as none, one, or two or more.
Health-related quality of life: The Functional Assessment of Cancer Therapy–General (FACT-G), version 4, was administered to measure overall HRQOL at baseline. The FACT-G is a widely validated measure of HRQOL that has been specifically designed for use among patients with cancer, with a Cronbach alpha of 0.89 (Cella et al., 1993). Scores were dichotomized at the mean of the sample as higher versus lower HRQOL. The Distress Thermometer, a numerical rating scale for assessing psychosocial distress in patients with cancer (Jacobsen et al., 2005), was administered at baseline. Scores ranged from 0 (least possible distress) to 10 (most possible distress). Responses were dichotomized as greater than or equal to 4 as high distress versus less than or equal to 3 as average to low distress (Ma et al., 2014). Sensitivity was 0.82, whereas specificity was 0.73. The Center for Epidemiologic Studies Depression Scale (CES-D), a 20-item measure, was used to assess participant depressive symptoms at baseline. Possible scores ranged from 0 (no depressive symptoms) to 60 (most depressive symptoms) (Beekman et al., 1997). The Cronbach alpha was 0.88. Sensitivity (past month) was 1, whereas specificity was 0.87. Scores were dichotomized at greater than or equal to 16 as clinically meaningful depressive symptoms versus less than or equal to 15 as no clinically significant depressive symptoms, based on prior literature (Radloff, 1977).
Statistical Analysis
Distributions for sample characteristics, overall and by study arm, were generated. Equivalence of study arms by sample characteristics (to ensure appropriate randomization) was assessed using the chi-square test. Bivariate distributions of healthcare service utilization (i.e., ED visits and inpatient hospitalizations) by study arm and sample characteristics were then evaluated. Unadjusted differences in healthcare service utilization by study arm were assessed using the chi-square test. Multivariable logistic regression was then used to examine the adjusted associations between study arms and the odds of visiting the ED one or more times versus none and the odds of being hospitalized one or more times versus none. Covariates included cancer type, gender, age, race, marital status, education, annual income, and number of comorbidities. Models also controlled for baseline patient-reported HRQOL factors, including depressive symptoms and emotional distress. As a sensitivity analysis, all adjusted models were also estimated using Poisson regression, treating the number of ED visits and inpatient hospitalizations as count data rather than dichotomous outcomes. Although not reported in the current article, preliminary analyses also examined differences by study arm for other types of utilization, including ambulatory visits, use of home health services, and hospice enrollment. No significant differences were found by study arm with respect to these types of utilization. All analyses were conducted in Stata®, version 13.0.
Results
The mean age of study participants was 60.5 years (range = 26–95 years); additional participant characteristics are presented in Table 1. With respect to the sample, no significant differences were noted by study arm. No statistically significant differences in healthcare service utilization for ED visits or inpatient hospitalizations by FOCUS study arm were noted in unadjusted analyses. 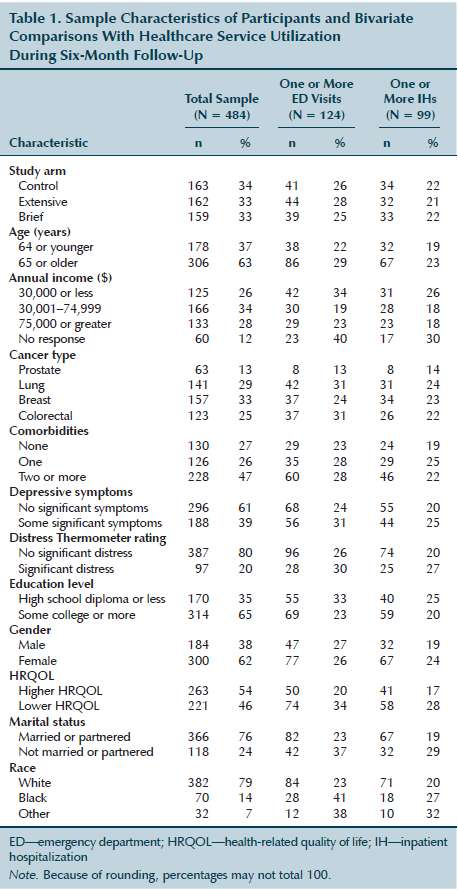
Table 2 presents the results of two multivariable logistic regression models: (a) the odds of ED visit (one or more times versus none) and (b) the odds of inpatient hospitalization (one or more times versus none) by study arm (Brief FOCUS, Extensive FOCUS, control), adjusting for participant sociodemographic, health status, and HRQOL factors. No significant association between study arm and ED visits was observed in the adjusted model. Patients with lung cancer or colorectal cancer were significantly more likely to visit the ED one or more times than patients with prostate cancer. Having two or more comorbidities versus none was also significantly associated with higher odds of ED visits. Patients reporting lower baseline HRQOL on the FACT-G were significantly more likely to visit the ED one or more times, compared to patients reporting higher baseline FACT-G scores. 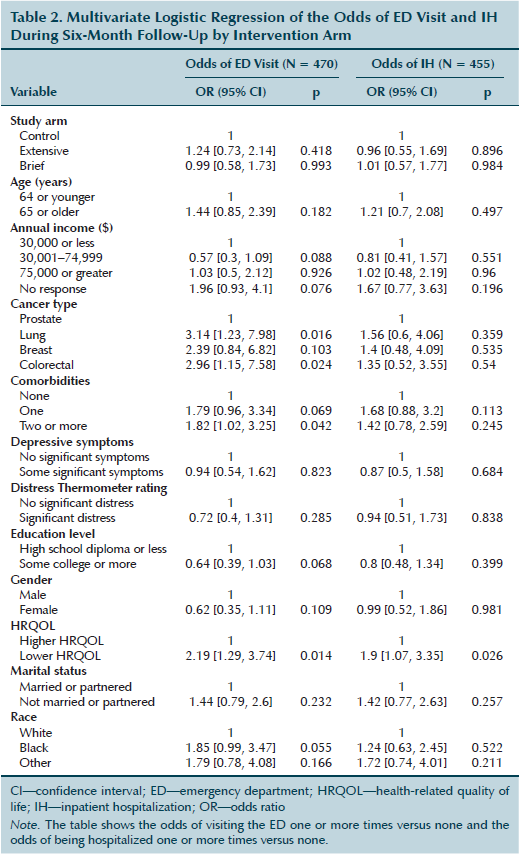
In the multivariable logistic regression model of odds of inpatient hospitalization (one or more times during the six-month follow-up period versus none) by FOCUS study arm, no significant association was found between study arm and odds of inpatient hospitalization. Of the other model covariates, baseline HRQOL, as measured by the FACT-G, was significantly associated with odds of inpatient hospitalization. Patients with lower baseline FACT-G scores were significantly more likely to be hospitalized during the six-month follow-up period compared to those with higher baseline scores. Results from the Poisson regression did not differ from results generated by the logistic regressions.
Discussion
In the RCT of patients with advanced cancer and their family caregivers who received a nurse-led psychoeducational intervention, the current authors found no difference in the odds of patients visiting the ED or being hospitalized by study arm. These findings suggest that the FOCUS Program, either in a brief or extensive format, is unlikely to influence patients’ healthcare service utilization.
During a time of rising healthcare costs, the FOCUS Program shows promise in improving psychosocial outcomes for patients and their caregivers without increasing patients’ use of costly healthcare services, such as the ED or hospitalization. However, the FOCUS Program also did not reduce healthcare service utilization in the current study’s population. This may be the result of the overall low intensity of both the brief (three sessions) and extensive (six sessions) versions of the program, which were delivered over a relatively short period of time (two months). To keep implementation costs low and to increase the feasibility of community-based implementation, the FOCUS Program was developed intentionally as a time- and resource-limited program. To reduce ED visits and hospital stays, a more extended or intense intervention with ongoing case management may be necessary.
As noted earlier, prior studies that examined the effect of psychoeducational interventions on healthcare service utilization have shown mixed results. Some of this variability may be because of the heterogeneity of studies in regard to type of intervention offered (e.g., symptom management, residential support, psychoeducational), number of intervention sessions (3–18), duration of intervention (two to six months), length of follow-up (six months to two years), and differences in patients’ type and stage of cancer. Although the number of studies is limited, interventions that focused primarily on symptom management (Kurtz et al., 2006) appear to have had more effect on healthcare service utilization than interventions that primarily provided support (Björneklett et al., 2013). Studies that offered more intervention sessions during a longer period of time, such as Kurtz et al.’s (2006) 10-session intervention and McCorkle et al.’s (2011) 16-session intervention, had more effect on decreasing healthcare service utilization than interventions that offered fewer sessions. Similarly, studies with longer periods of follow-up may be better suited to detecting differences in healthcare service utilization than those with shorter analytic windows.
Reduction in avoidable or unnecessary healthcare service utilization, including ED visitation, has been specified by the Institute of Medicine as an important target for controlling costs associated with cancer care (National Research Council, 2013). However, patients with cancer may be at risk for a number of disease- or treatment-related complications for which emergency medical care may be appropriate. McCorkle et al. (2011) noted a trend toward greater utilization of the ED among women who received the nurse-led intervention, particularly those who were depressed. Björneklett et al. (2013) found that utilization was significantly higher in the intervention arm of their psychosocial intervention among women newly diagnosed with breast cancer who had received chemotherapy. Both studies concluded that individuals receiving the intervention may have been more motivated to notice physical symptoms and changes in health status, and then seek care when needed. In these cases, the interventions may have increased appropriate ED visits among patients who otherwise may have ignored important symptoms. Although the FOCUS intervention did not increase ED visitation, these findings from prior studies underscore the need for psychoeducational interventions to examine the possibility of increased healthcare service utilization as a positive outcome.
To date, the majority of research that has examined the impact of nurse-led interventions on healthcare service utilization has focused on patients with cancer with localized disease (Arving et al., 2014; Björneklett et al., 2013; McCorkle et al., 2011). The current study’s population consisted of patients with advanced disease (stage III or IV cancer) but anticipated life expectancies of six months or longer. To the current authors’ knowledge, only a few studies (Bakitas et al., 2009; Lemieux et al., 2006; Northouse et al., 2013) have examined the association between a nurse-led psychoeducational intervention and healthcare service utilization among this growing subset of patients with advanced disease, none of which observed increased healthcare service utilization as a result of the intervention.
The current study identified a number of patient characteristics that were associated with greater healthcare service utilization. Study participants with lung cancer had a high likelihood of ED visitation, which is consistent with previous findings (Mayer, Travers, Wyss, Leak, & Waller, 2011). Greater burden of comorbidities were also associated with higher ED visitation in the current study and others, including Kurtz et al. (2006). Although the current authors found significant differences by cancer type and comorbidities for ED visitation, no differences by cancer type for the odds of subsequent inpatient hospitalizations were observed. This is perhaps unsurprising, given that inpatient hospitalizations are generally preceded by more serious health events, the distribution of which may be fairly heterogeneous within this population (Kurtz, Kurtz, Given, & Given, 2005). Consistent with research in noncancer populations (Dominick, Ahern, Gold, & Heller, 2002), worse baseline HRQOL was also strongly associated with ED visitation and inpatient hospitalizations in the current study, suggesting that baseline HRQOL is an independent predictor of subsequent healthcare service utilization, even among patients with similar sociodemographic characteristics and burden of disease.
Limitations
The current study had some limitations. Patients who lacked an involved caregiver were not eligible for this study, and they may have different patterns of utilization. Although a major strength of this study was the assessment of utilization using medical chart data versus participant self-report, the current authors were unable to measure the particular health problem or condition for which patients sought help. Consequently, differentiating between appropriate versus inappropriate utilization of the ED and between planned versus unplanned inpatient hospitalizations was not possible and needs to be assessed in future research. In addition, because medical chart data were specific to study sites, the current authors were unable to account for any ED visit or inpatient hospitalization that took place at a nonparticipating institution. Compared to other studies in this domain (Arving et al., 2014), the current study had a fairly short follow-up window of six months. Healthcare service utilization may differ by FOCUS study arm beyond the six-month follow-up period. The FOCUS intervention also is a specific psychoeducational intervention for patient-caregiver dyads, and the lack of effect found on healthcare service utilization cannot be generalized to other nurse-led psychoeducational interventions.
Implications for Practice and Conclusion
Psychosocial support for patients with advanced cancer is a major priority area for improving the cancer care delivery system (National Research Council, 2013). The number of patients with cancer is projected to rise in the coming decade, yet available healthcare resources will likely remain relatively static (Smith, Smith, Hurria, Hortobagyi, & Buchholz, 2009). Patients with worse baseline HRQOL may be at greater risk of using healthcare resources. These patients may require more intense interventions and longer-term follow-up by health professionals. Psychoeducational interventions that demonstrate favorable patient outcomes without increasing economic burden on the healthcare system are needed. The FOCUS intervention, either in brief or extensive format, is an effective strategy to improve the HRQOL of patients with advanced cancer without increasing healthcare service utilization.
Nurse-led psychoeducational interventions are an important aspect of patient-centered nursing care in the oncology setting. A number of nurse-led psychoeducational interventions, including the FOCUS Program, have shown promise in empowering patients and caregivers to appropriately address symptoms and manage psychosocial distress without placing undue strain on the healthcare system. As new nurse-led interventions for patients with cancer and their caregivers are developed and tested, continued investigation regarding the impact of these interventions on healthcare service utilization is needed.
References
Alemayehu, B., Buysman, E., Parry, D., Becker, L., & Nathan, F. (2010). Economic burden and healthcare utilization associated with castration-resistant prostate cancer in a commercial and Medicare Advantage US patient population. Journal of Medical Economics, 13, 351–361. doi:10.3111/13696998.2010.491435
Arving, C., Brandberg, Y., Feldman, I., Johansson, B., & Glimelius, B. (2014). Cost-utility analysis of individual psychosocial support interventions for breast cancer patients in a randomized controlled study. Psycho-Oncology, 23, 251–258. doi:10.1002/pon.3411
Bakitas, M., Lyons, K.D., Hegel, M.T., Balan, S., Barnett, K.N., Brokaw, F.C., . . . Ahles, T.A. (2009). The project ENABLE II randomized controlled trial to improve palliative care for rural patients with advanced cancer: Baseline findings, methodological challenges, and solutions. Palliative and Supportive Care, 7, 75–86. doi:10.1017/S1478951509000108
Barbera, L., Atzema, C., Sutradhar, R., Seow, H., Howell, D., Husain, A., . . . Dudgeon, D. (2013). Do patient-reported symptoms predict emergency department visits in cancer patients? A population-based analysis. Annals of Emergency Medicine, 61, 427–437, e5. doi:10.1016/j.annemergmed.2012.10.010
Barbera, L., Taylor, C., & Dudgeon, D. (2010). Why do patients with cancer visit the emergency department near the end of life? Canadian Medical Association Journal, 182, 563–568. doi:10.1503/cmaj.091187
Beekman, A.T., Deeg, D.J., Van Limbeek, J., Braam, A.W., De Vries, M.Z., & Van Tilburg, W. (1997). Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): Results from a community-based sample of older subjects in The Netherlands. Psychological Medicine, 27, 231–235. doi:10.1017/s0033291796003510
Björneklett, H.G., Rosenblad, A., Lindemalm, C., Ojutkangas, M.L., Letocha, H., Strang, P., & Bergkvist, L. (2013). A randomized controlled trial of support group intervention after breast cancer treatment: Results on sick leave, health care utilization and health economy. Acta Oncologica, 52, 38–47. doi:10.3109/0284186X.2012.734921
Carlson, L.E., Angen, M., Cullum, J., Goodey, E., Koopmans, J., Lamont, L., . . . Bultz, B.D. (2004). High levels of untreated distress and fatigue in cancer patients. British Journal of Cancer, 90, 2297–2304. doi:10.1038/sj.bjc.6601887
Cella, D.F., Tulsky, D.S., Gray, G., Sarafian, B., Linn, E., Bonomi, A., . . . Brannon, J. (1993). The Functional Assessment of Cancer Therapy scale: Development and validation of the general measure. Journal of Clinical Oncology, 11, 570–579.
Dominick, K.L., Ahern, F.M., Gold, C.H., & Heller, D.A. (2002). Relationship of health-related quality of life to health care utilization and mortality among older adults. Aging Clinical and Experimental Research, 14, 499–508. doi:10.1007/bf03327351
Faller, H., Schuler, M., Richard, M., Heckl, U., Weis, J., & Küffner, R. (2013). Effects of psycho-oncologic interventions on emotional distress and quality of life in adult patients with cancer: Systematic review and meta-analysis. Journal of Clinical Oncology, 31, 782–793. doi:10.1200/JCO.2011.40.8922
Folkman, S., & Lazarus, R.S. (1980). An analysis of coping in a middle-aged community sample. Journal of Health and Social Behavior, 21, 219–239.
Himelhoch, S., Weller, W.E., Wu, A.W., Anderson, G.F., & Cooper, L.A. (2004). Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Medical Care, 42, 512–521. doi:10.1097/01.mlr.0000127998.89246.ef
Jacobsen, P.B., Donovan, K.A., Trask, P.C., Fleishman, S.B., Zabora, J., Baker, F., & Holland, J.C. (2005). Screening for psychologic distress in ambulatory cancer patients. Cancer, 103, 1494–1502. doi:10.1002/cncr.20940
Kim, J., Han, J.Y., Shaw, B., McTavish, F., & Gustafson, D. (2010). The roles of social support and coping strategies in predicting breast cancer patients’ emotional well-being: Testing mediation and moderation models. Journal of Health Psychology, 15, 543–552. doi:10.1177/1359105309355338
Kurtz, M.E., Kurtz, J.C., Given, C.W., & Given, B. (2006). Effects of a symptom control intervention on utilization of health care services among cancer patients. Medical Science Monitor, 12, CR319–CR324.
Kurtz, M.E., Kurtz, J.C., Given, C.W., & Given, B.A. (2005). Utilization of services among elderly cancer patients—Relationship to age, symptoms, physical functioning, comorbidity, and survival status. Ethnicity and Disease, 15(Suppl. 2), S17–S22.
Kutikova, L., Bowman, L., Chang, S., Long, S.R., Obasaju, C., & Crown, W.H. (2005). The economic burden of lung cancer and the associated costs of treatment failure in the United States. Lung Cancer, 50, 143–154. doi:10.1016/j.lungcan.2005.06.005
Lang, K., Lines, L.M., Lee, D.W., Korn, J.R., Earle, C.C., & Menzin, J. (2009). Trends in healthcare utilization among older Americans with colorectal cancer: A retrospective database analysis. BMC Health Services Research, 9, 227. doi:10.1186/1472-6963-9-227
Lemieux, J., Topp, A., Chappell, H., Ennis, M., & Goodwin, P.J. (2006). Economic analysis of psychosocial group therapy in women with metastatic breast cancer. Breast Cancer Research and Treatment, 100, 183–190. doi:10.1007/s10549-006-9249-1
Ma, X., Zhang, J., Zhong, W., Shu, C., Wang, F., Wen, J., . . . Liu, L. (2014). The diagnostic role of a short screening tool—The Distress Thermometer: A meta-analysis. Supportive Care in Cancer, 22, 1741–1755. doi:10.1007/s00520-014-2143-1
Mariotto, A.B., Yabroff, K.R., Shao, Y., Feuer, E.J., & Brown, M.L. (2011). Projections of the cost of cancer care in the United States: 2010–2020. Journal of the National Cancer Institute, 103, 117–128. doi:10.1093/jnci/djq495
Mayer, D.K., Travers, D., Wyss, A., Leak, A., & Waller, A. (2011). Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. Journal of Clinical Oncology, 29, 2683–2688. doi:10.1200/JCO.2010.34.2816
McCorkle, R., Jeon, S., Ercolano, E., & Schwartz, P. (2011). Healthcare utilization in women after abdominal surgery for ovarian cancer. Nursing Research, 60, 47–57. doi:10.1097/NNR.0b013e3181ff77e4
National Research Council. (2013). Delivering high-quality cancer care: Charting a new course for a system in crisis. Washington, DC: National Academies Press.
Northouse, L., Kershaw, T., Mood, D., & Schafenacker, A. (2005). Effects of a family intervention on the quality of life of women with recurrent breast cancer and their family caregivers. Psycho-Oncology, 14, 478–491. doi:10.1002/pon.871
Northouse, L.L., Mood, D.W., Schafenacker, A., Kalemkerian, G., Zalupski, M., LoRusso, P., . . . Kershaw, T. (2013). Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psycho-Oncology, 22, 555–563. doi:10.1002/pon.3036
Northouse, L.L., Mood, D.W., Schafenacker, A., Montie, J.E., Sandler, H.M., Forman, J.D., . . . Kershaw, T. (2007). Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer, 110, 2809–2818. doi:10.1002/cncr.23114
Owen, J.E., Klapow, J.C., Hicken, B., & Tucker, D.C. (2001). Psychosocial interventions for cancer: Review and analysis using a three-tiered outcomes model. Psycho-Oncology, 10, 218–230. doi:10.1002/pon.509.abs
Radloff, L.S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi:10.1177/014662167700100306
Rehse, B., & Pukrop, R. (2003). Effects of psychosocial interventions on quality of life in adult cancer patients: Meta analysis of 37 published controlled outcome studies. Patient Education and Counseling, 50, 179–186. doi:10.1016/s0738-3991(02)00149-0
Roehrig, C., Miller, G., Lake, C., & Bryant, J. (2009). National health spending by medical condition, 1996–2005. Health Affairs, 28, w358–w367. doi:10.1377/hlthaff.28.2.w358
Rosenberg, H.J., Rosenberg, S.D., Ernstoff, M.S., Wolford, G.L., Amdur, R.J., Elshamy, M.R., . . . Pennebaker, J.W. (2002). Expressive disclosure and health outcomes in a prostate cancer population. International Journal of Psychiatry in Medicine, 32, 37–53. doi:10.2190/agpf-vb1g-u82e-ae8c
Smith, B.D., Smith, G.L., Hurria, A., Hortobagyi, G.N., & Buchholz, T.A. (2009). Future of cancer incidence in the United States: Burdens upon an aging, changing nation. Journal of Clinical Oncology, 27, 2758–2765. doi:10.1200/JCO.2008.20.8983
Unützer, J., Patrick, D.L., Simon, G., Grembowski, D., Walker, E., Rutter, C., & Katon, W. (1997). Depressive symptoms and the cost of health services in HMO patients aged 65 years and older. A 4-year prospective study. JAMA, 277, 1618–1623. doi:10.1001/jama.277.20.1618
Vera-Llonch, M., Weycker, D., Glass, A., Gao, S., Borker, R., Barber, B., & Oster, G. (2011). Healthcare costs in patients with metastatic lung cancer receiving chemotherapy. BMC Health Services Research, 11, 305. doi:10.1186/1472-6963-11-305
Vera-Llonch, M., Weycker, D., Glass, A., Gao, S., Borker, R., Qin, A., & Oster, G. (2011). Healthcare costs in women with metastatic breast cancer receiving chemotherapy as their principal treatment modality. BMC Cancer, 11, 250. doi:10.1186/1471-2407-11-250
Worden, J.W. (1993). Psychosocial screening of cancer patients. Journal of Psychosocial Oncology, 1, 1–10. doi:10.1300/J077v01n04_01
Yoo, W., Shah, D.V., Shaw, B.R., Kim, E., Smaglik, P., Roberts, L.J., . . . Gustafson, D.H. (2014). The role of the family environment and computer-mediated social support on breast cancer patients’ coping strategies. Journal of Health Communication, 19, 981–998. doi:10.1080/10810730.2013.864723
Zabora, J., BrintzenhofeSzoc, K., Curbow, B., Hooker, C., & Piantadosi, S. (2001). The prevalence of psychological distress by cancer site. Psycho-Oncology, 10, 19–28. doi:10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.3.co;2-y
About the Author(s)
Kathryn A. Martinez, PhD, MPH, is a postdoctoral fellow at the VA Center for Clinical Management Research in Ann Arbor, MI; Christopher Friese, PhD, RN, AOCN®, FAAN, is an assistant professor in the School of Nursing at the University of Michigan in Ann Arbor; Trace Kershaw, PhD, is an associate professor in the School of Public Health at Yale University in New Haven, CT; Charles W. Given, PhD, is a professor in the Department of Family Medicine at Michigan State University in East Lansing; A. Mark Fendrick, MD, is a professor in the Division of General Medicine at the University of Michigan; and Laurel Northouse, PhD, RN, FAAN, is professor emerita in the School of Nursing at the University of Michigan. No financial relationships to disclose. Martinez can be reached at makathry@med.umich.edu, with copy to editor at ONFEditor@ons.org. (Submitted December 2014. Accepted for publication January 27, 2015.)

