The Teachable Moment After Cancer Diagnosis: Perceptions From Oncology Nurses
Purpose/Objectives: To determine oncology nurses’ perspectives of the receptiveness of survivors to receiving health behavior guidance, with secondary purposes to (a) explore other elements of oncology nurses’ perceptions of the teachable moment and (b) examine differences in outcomes between American and Canadian nurses.
Design: Cross-sectional survey.
Setting: In- and outpatient oncology nursing departments in the United States and Canada.
Sample: 310 members of the Canadian Association of Nurses in Oncology (CANO/ACIO) and the Oncology Nursing Society (ONS) who currently care for patients.
Methods: Oncology nurses recruited through emails distributed through the CANO/ACIO and ONS Listservs completed online investigator-developed surveys.
Main Research Variables: Measures related to oncology nurses’ perceptions of survivors’ receptiveness to health behavior change counseling and the teachable moment (i.e., general receptiveness, perceived benefits, guidance and referral seeking, long- and short-term effectiveness, best time, and best resources).
Findings: Oncology nurses reported that survivors were receptive to receiving guidance on health behaviors, particularly during teachable moments after diagnosis and during treatment. They also perceived that a fairly low percentage of survivors asked for guidance about health behavior change; relatively few made improvements to their health behaviors.
Conclusions: Survivors are reported to be interested in receiving guidance concerning health behavior change during key teachable moments. Oncology nurses may need to initiate conversations with survivors, offer education regarding the benefits of positive health behavior change, and provide ongoing support throughout the cancer trajectory.
Implications for Nursing: Oncology nurses may use findings from the current study to guide their health behavior change counseling with survivors.
Jump to a section
Being treated for cancer and living as a survivor comes with an increased likelihood of ongoing quality-of-life (QOL) concerns and incidence of chronic disease, as well as the risk of cancer recurrence and the possibility of secondary tumors (Cowens-Alvarado et al., 2013). In many cases, the risk of poor QOL, recurrence, and comorbidities is exacerbated by the practice of unhealthy behaviors, such as lack of physical activity, poor nutritional choices, and tobacco use (Cowens-Alvarado et al., 2013). Consequently, an increasing level of interest has been focused on improving health behaviors in survivors as a means of enhancing QOL, reducing chronic disease, and increasing longevity.
In an attempt to effectively foster health behavior change in survivorship, researchers and practitioners have become interested in the teachable moment, or a time after naturally occurring circumstances or events that may lead individuals to make positive changes to their health behaviors (McBride, Emmons, & Lipkus, 2003). In survivors, a teachable moment has been identified during the time after cancer diagnosis when individuals may be receptive to behavior change interventions (Demark-Wahnefried, Aziz, Rowland, & Pinto, 2005). Cancer and its treatments may create challenges to making improvements in behaviors, but a cancer diagnosis may also act as a catalyst for change if individuals see the potential harm associated with unhealthy behaviors as being related to the cancer diagnosis and subsequent prognosis (McBride & Ostroff, 2003).
Although a cancer diagnosis has the potential to trigger positive lifestyle changes, most research suggests that the majority of individuals do not improve health behaviors following diagnosis (Broderick, Hussey, Kennedy, & O’Donnell, 2014; Patterson et al., 2010; Sabiston, Brunet, Vallance, & Meterissian, 2014). For example, Sabiston et al. (2014) found that, when using accelerometers to objectively measure physical activity levels in a sample of breast cancer survivors, moderate to vigorous physical activity levels significantly decreased in the year after diagnosis. Similarly, Broderick et al. (2014) discovered that a sample of breast cancer survivors remained equally sedentary in the first year after completion of chemotherapy and experienced a significant gain in body weight. In longer-term survivors, large cohort studies also indicated a lack of positive changes in health behaviors, reporting that, compared to cancer-free controls, cancer survivors several years into survivorship do not significantly differ in body mass index (BMI) and alcohol and tobacco consumption (Bidstrup et al., 2013; Patterson et al., 2010). Most cancer survivors are seemingly unable to self-initiate or maintain changes in health behaviors by themselves.
Despite the lack of changes that survivors initiate in their behaviors, survey research consistently indicates that this population reports interest in receiving support and guidance regarding making positive changes in the areas of physical activity (Szymlek-Gay, Richards, & Egan, 2011), tobacco cessation (Berg, Carpenter, Jardin, & Ostroff, 2013), and health behaviors (Cooley et al., 2011, 2013; Demark-Wahnefried, Peterson, McBride, Lipkus, & Clipp, 2000). In addition, when provided with counseling or other intervention strategies, cancer survivors generally can make positive improvements in fruit and vegetable consumption (Campbell et al., 2009), smoking cessation (Sharp, Johansson, Fagerström, & Rutqvist, 2008), weight loss (Vitolins et al., 2014), and physical activity levels (Demark-Wahnefried et al., 2012). For example, Demark-Wahnefried et al. (2012) found that in a wait-list control, crossover trial of 641 colorectal, breast, and prostate cancer survivors, those who received a physical activity and diet intervention consisting of mailed print materials and telephone counseling for one year were able to make significant improvements in diet quality, physical activity, and BMI compared to those in the control condition. Likewise, a nurse-led tobacco cessation intervention with head and neck cancer survivors (N = 50) receiving radiation therapy was able to demonstrate significant reductions in smoking, with 74% (n = 37) of participants testing smoke-free during the course of the intervention and 68% (n = 28) testing smoke-free one year later (Sharp et al., 2008).
The teachable moment has the potential to decrease cancer survivors’ risks associated with unhealthy behaviors, but it remains relatively underexplored. To date, no research has specifically examined the teachable moment from the perspective of oncology nurses, even though nurses can likely provide a unique viewpoint on survivors’ interest and receptiveness to making positive changes to their health behaviors. Oncology nurses frequently care for survivors following diagnosis, allowing them to obtain a good idea of survivors’ ability to improve health behaviors across the cancer trajectory.
The overall aim of the current study was to explore the teachable moment following a cancer diagnosis from an oncology nursing perspective. The primary purpose was to determine oncology nurses’ perspectives of the receptiveness of cancer survivors to receiving health behavior guidance and support. Secondary purposes were to (a) further explore other elements of oncology nurses’ perceptions of the teachable moment and (b) explore differences in oncology nurses’ perceptions of the receptiveness of cancer survivors to receiving health behavior guidance and support between the United States and Canada. The current authors hypothesized that oncology nurses would report cancer survivors being generally receptive to receiving health behavior guidance and support. In addition, the current authors expected to see differences between the United States and Canada in perceived receptiveness of cancer survivors to health behavior change guidance because of dissimilarities in health behaviors (e.g., higher physical activity and lower smoking rates in Canada as compared to the United States) (Jones, Gulbis, & Baker, 2010; Zhang et al., 2010) and healthcare systems (e.g., health care in the United States is mostly privately funded as compared to health care in Canada, which is publicly funded) (Buhr, 2013; O’Neill & O’Neill, 2007). No other hypotheses were developed, given the primarily exploratory nature of the study.
Methods
The study design was a cross-sectional exploratory online survey. The Nipissing University Research Ethics Board provided ethics approval for the study and allowed informed consent to be waived. Eligibility criteria included (a) being a practicing oncology nurse, (b) residing in the United States or Canada, and (c) currently seeing cancer survivors in a clinical capacity. Email Listservs of the memberships of the Canadian Association of Nurses in Oncology (CANO/ACIO) and the Oncology Nursing Society (ONS) were used for sending recruitment emails. A total of 4,000 randomly selected eligible ONS members were sent emails, and about 1,000 emails were sent to the entire email list of CANO/ACIO. The anonymous, Internet-based survey was created using Qualtrics online survey software (www.qualtrics.com), and a link to it, embedded within a brief description of the study, was included in the recruitment emails. All emails featured an opt-out option. All participants were given the opportunity to enter a drawing for one of 10 $30 gift cards. The current authors received two emails from nurses indicating ineligibility because both no longer cared for patients in a clinical capacity. The survey was conducted from May 2013 to January 2014, and a total of 310 completed surveys were received from the 5,000 emails that were sent out (response rate = 6%).
Instrument
The survey consisted of eight closed-ended items that assessed variables related to the teachable moment and were developed by the current authors. Items were independently evaluated by the authors for face validity. Perceptions of the teachable moment were assessed by items that asked about oncology nurses’ observations regarding the receptiveness of cancer survivors to health behavior change counseling. 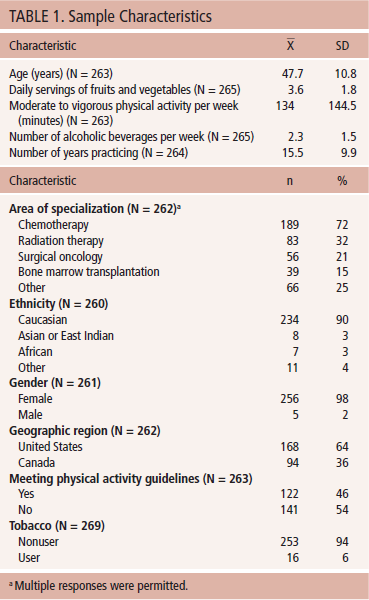 These items consisted of (a) general receptiveness (how receptive survivors are to receiving guidance and support regarding positive health behavior change with responses ranging from 1 [not at all interested] to 5 [very interested]); (b) perceived benefits (the degree to which survivors recognize health and QOL benefits of positive health behavior change, with responses ranging from 1 [not at all] to 5 [very much]); (c) guidance and referral seeking (the percentage of survivors who ask for guidance and referrals for making positive changes in health behaviors); (d) long- and short-term effectiveness (the percentage of survivors who make positive improvements in the long and short term after receiving health behavior change counseling); (e) best time (the time when survivors are the most receptive to receiving guidance and support for positive health behavior change); and (f) best resources (the effectiveness of services and resources for helping survivors improve health behaviors). Details of the specific items are displayed in Tables 1, 2, and 3.
These items consisted of (a) general receptiveness (how receptive survivors are to receiving guidance and support regarding positive health behavior change with responses ranging from 1 [not at all interested] to 5 [very interested]); (b) perceived benefits (the degree to which survivors recognize health and QOL benefits of positive health behavior change, with responses ranging from 1 [not at all] to 5 [very much]); (c) guidance and referral seeking (the percentage of survivors who ask for guidance and referrals for making positive changes in health behaviors); (d) long- and short-term effectiveness (the percentage of survivors who make positive improvements in the long and short term after receiving health behavior change counseling); (e) best time (the time when survivors are the most receptive to receiving guidance and support for positive health behavior change); and (f) best resources (the effectiveness of services and resources for helping survivors improve health behaviors). Details of the specific items are displayed in Tables 1, 2, and 3.
[[{"type":"media","view_mode":"media_original","fid":"19211","attributes":{"alt":"","class":"media-image","height":"252","typeof":"foaf:Image","width":"576"}}]]
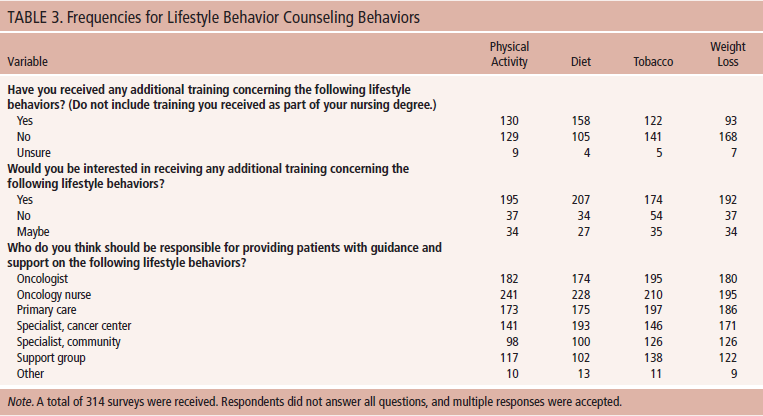
A final section consisted of nine additional open- and closed-ended items assessing demographic and professional information. These items queried age, gender, ethnicity, geographic region, area of specialization, types of cancer specialization, and years practicing nursing (see Table 4).
[[{"type":"media","view_mode":"media_original","fid":"19246","attributes":{"alt":"","class":"media-image","height":"723","typeof":"foaf:Image","width":"355"}}]]
Statistical Analyses
SPSS®, version 21.0, was used for statistical analyses. A significant p value was set at alpha = 0.05. Descriptive statistics—including means, standard deviations, frequencies, and percentages—were used to analyze data. Differences between the primary outcome (i.e., general receptiveness to physical activity, diet, tobacco cessation, and weight-loss counseling) and country of residence (i.e., United States or Canada) were determined using independent samples t tests.
Results
Descriptive statistics of demographic and professional information revealed an average age of 47.7 years. The majority of participants were female (98%) and Caucasian (90%), and 64% resided in the United States. The sample reported active clinical practice for an average of 15.5 years, with the most common area of specialization being chemotherapy (72%) and the most frequently reported type of cancer specialization being breast cancer (36%).
In brief, oncology nurses perceived that, although cancer survivors scored high on general receptiveness (mean = 3.2–4.05, SD = 0.71–0.96), they scored only moderately on perceived benefits (mean = 2.46–2.63, SD = 0.53–0.67) and fairly low on guidance seeking (mean = 20.4%–54.6%, SD = 22.9–28.6), long-term effectiveness (mean = 24.7%–37.3%, SD = 23.8–24.8), and short-term effectiveness (mean = 27.2%–45.3%, SD = 24.3–25.4). When oncology nurses were asked when they felt cancer survivors are most receptive to receiving guidance and support concerning health behaviors, the most frequent answer was “during treatment” for physical activity (n = 130 of 267), diet (n = 148 of 266), and weight loss (n = 75 of 264). For tobacco cessation, the most frequent answer was “during diagnosis” (n = 129 of 260). For best resources, oncology nurses rated support groups (mean = 4.15, SD = 0.64) and counseling (mean = 4.12, SD = 0.57) as the most effective.
Results of the independent t tests indicated a significant difference in perceived receptiveness of cancer survivors to physical activity guidance and support between American (mean = 3.9, SD = 0.74) and Canadian (mean = 3.69, SD = 0.74) nurses (t [257] = 2.25, p = 0.025 with a small effect size [Cohen’s d = 0.28]). No significant differences were found in perceived receptiveness to guidance and support for diet, tobacco cessation, or weight loss between nurses from the United States and Canada (see Table 5). 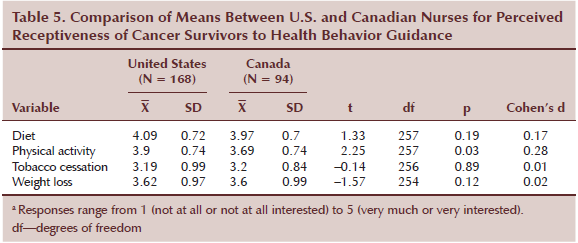
Discussion
The current study reports on novel data from a survey of oncology nurses’ perceptions of the teachable moment for health behavior promotion in cancer survivors. The current authors found partial support for their hypotheses.
As expected, the current authors found that oncology nurses perceived that survivors were generally receptive to guidance and support for making positive changes to their health behaviors. This finding is important because it validates previous survey research that has consistently indicated that cancer survivors report a strong interest in receiving health behavior change guidance (Berg et al., 2013; Cooley et al., 2011, 2013; Demark-Wahnefried et al., 2000; Szymlek-Gay et al., 2011). However, these previous surveys have been limited because of the high possibility of a social desirability bias in which cancer survivors offer responses that they feel are the most favorable (Karvinen, Raedeke, Arastu, & Allison, 2011). As such, the findings from the current study, which potentially lacks the social desirability bias of research with cancer survivors, supports previous surveys and further highlights the need for additional supportive care services for survivors for improving health behaviors.
Similar to the current study, past research has suggested that cancer survivors report being most interested in receiving guidance and support concerning diet (Green, Steinnagel, Morris, & Laakso, 2014) and physical activity (Green et al., 2014; Philip et al., 2014) during the teachable moment (shortly after diagnosis or during treatment). For tobacco cessation, the most common time in the current study during which oncology nurses felt cancer survivors were the most receptive to guidance was at diagnosis, possibly because of the connection that many survivors make with a cancer diagnosis and tobacco use. These findings provide additional evidence of a teachable moment after cancer diagnosis; the diagnosis of cancer may cue individuals to be more interested in making positive changes to their health behaviors.
Contrary to past research, oncology nurses in the current study’s sample reported that they perceive cancer survivors to not generally recognize the health and QOL benefits of practicing positive health behaviors. Past research surveying cancer survivors generally indicates that survivors are well aware of the benefits of positive health behaviors, at least in the physical activity domain (Bulmer, Howell, Ackerman, & Fedric, 2012; Craike, Hose, Courneya, Harrison, & Livingston, 2013). For example, survivors report recognizing the benefits of physical activity for recovery from the side effects of therapy, psychological and social well-being, and enjoyment (Craike et al., 2013), and they are able to make connections between good QOL indices and participation in exercise (Bulmer et al., 2012). This discrepancy may be because oncology nurses are possibly not aware of what survivors find to be the benefits of positive health behaviors. Alternatively, survivors may over-report the perceived benefits of health behavior change because of social desirability bias.
In the current study, oncology nurses indicated that relatively few survivors requested guidance or asked for a referral to a specialist concerning health behavior change support. However, previous surveys suggest strong interest by survivors in health behavior guidance (Berg et al., 2013; Cooley et al., 2011, 2013; Demark-Wahnefried et al., 2000; Szymlek-Gay et al., 2011). These findings suggest that, although survivors may be interested in receiving guidance concerning health behavior change, they may not initiate discussions to ask for additional support. In addition, opportunities to focus on health promotion discussions in the efficiency-driven, disease-focused cancer care system may leave little time or opportunity for survivors to ask for support, or for healthcare providers to assess and offer support for health-promoting behaviors (Arora, 2009; Feuerstein & Ganz, 2011; Roundtree, Giordano, Price, & Suarez-Almazor, 2011). Given the mounting evidence for the benefits of adopting healthy behaviors (e.g., physical activity, diet, weight maintenance, smoking cessation) for cancer survivors, oncology nurses must initiate the dialogue and offer ongoing support for adopting these behaviors at teachable moments throughout the cancer trajectory.
The majority of past research suggests that, without support, few survivors make positive changes to their health behaviors after a cancer diagnosis (Broderick et al., 2014; Patterson et al., 2010; Sabiston et al., 2014). From data gathered in the current study, oncology nurses overall indicated that a fairly low percentage of cancer survivors actually made positive changes to their health behaviors in the short or long term, even after receiving guidance and support from nurses. These findings suggest that more effective counseling or different intervention strategies may be required to make positive changes in health behaviors among cancer survivors. In addition, as identified by the oncology nurses in the current study, teachable moments may exist throughout the cancer trajectory; during these times, specific health behaviors may optimally be targeted for intervention. Shifting the model of care to create intentional opportunities at specific time points (e.g., diagnosis, during treatment, throughout the survivorship phase) for oncology nurses to provide information, counseling, and ongoing health behavior change support for survivors is imperative.
Contrary to the current authors’ hypotheses, minimal differences were found between oncology nurses in the United States and Canada in terms of cancer survivors’ general receptiveness to health behavior change guidance. The current authors did find that nurses from the United States rated cancer survivors as being slightly more receptive to receiving physical activity guidance than did Canadian nurses; the difference was small but still statistically significant. That larger differences did not emerge is surprising, considering discrepancies between the two countries regarding healthcare systems (the United States’ multi-payer, mostly privately funded system versus Canada’s single-payer, publicly funded system) (O’Neill & O’Neill, 2007). As a result, in general, Canadians experience longer wait times for services, whereas costs sometimes result in lack of access for some individuals in the United States (O’Neill & O’Neill, 2007). Canadians, compared to Americans, have been found in previous research to indicate better access to needed medicine and are more likely to have a regular doctor; however, they are less likely to have experienced cancer screening and are more likely to have perceptions of unmet healthcare needs (Buhr, 2013; O’Neill & O’Neill, 2007). Differences in health behaviors have also been found between the two countries, with higher physical activity levels (Zhang et al., 2010) and lower smoking rates (Jones et al., 2010) reported among Canadians than Americans.
Strengths and Limitations
One strength of the current study was the fairly large sample size that is representative of oncology nurses from disparate regions throughout the United States and Canada. A prominent weakness is a possible social desirability bias involving oncology nurses’ wish to present their patients and the effectiveness of their interactions with them in a favorable way. In addition, given the small survey response rate (6%), oncology nurses with an affinity for providing health behavior change guidance and support or care for populations where health behavior change is more readily taken up (e.g., women with breast cancer as compared to patients with lung cancer) may have self-selected to respond, thereby biasing results. In addition, the instrument used in the study was developed by the current authors and has not been validated.
Future studies using qualitative approaches may extend and provide context to the current study’s survey results to explore oncology nurses’ perspectives regarding what helps survivors to be ready for a teachable moment, as well as which health behavior change strategies are likely to be effective in which situations across the cancer trajectory. Similarly, gaining an understanding of the complex survivor perspectives regarding triggers and helpful strategies to support short- and long-term health behavior change is necessary to fully appreciate how to successfully support survivors to achieve optimal health. Studies incorporating an experimental design that examine the effectiveness of nurse-initiated discussions with cancer survivors concerning health behavior change may also be warranted.
Implications for Nursing and Conclusion
Results of the current study indicate that oncology nurses perceive that survivors were receptive to receiving guidance concerning health behavior change, particularly during teachable moments (e.g., shortly after diagnosis, during treatment). However, according to oncology nurses, many survivors did not generally ask nurses for help or for referrals regarding health behavior change. In addition, oncology nurses felt that the majority of survivors to whom they provided guidance concerning health behaviors did not make positive changes in the short or long term. Very small differences were found between oncology nurses in the United States and in Canada regarding their perceptions of survivors’ receptiveness to receiving health behavior change guidance.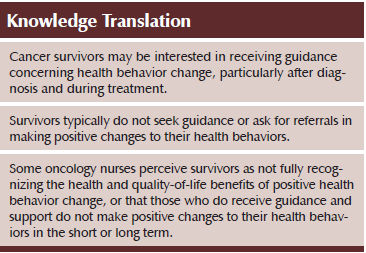
Oncology nurses may use these findings to guide their health behavior change counseling with survivors. Nurses should recognize that the perception of cancer survivors being receptive to receiving health behavior counseling of all types contrasts with their typically not asking for guidance or making short- or long-term changes. Consequently, oncology nurses should regularly inquire about survivors’ health behaviors and provide guidance and support for positive health behavior change as needed. Oncology nurses also should provide information to survivors concerning the advantages of making positive changes to their health behaviors because many survivors may not fully recognize the benefits. In addition, oncology nurses may find the provision of positive health behavior change guidance to survivors to be particularly effective if initiated during diagnosis or treatment because survivors may be most receptive during those times. Oncology nurses must advocate to shift the model of care to include opportunities to focus on and provide ongoing support for health promotion in the context of cancer treatment and care across the cancer trajectory.
References
Arora, N.K. (2009). Importance of patient-centered care in enhancing patient well-being: A cancer survivor’s perspective. Quality of Life Research, 18, 1–4. doi:10.1007/s11136-008-9415-5
Berg, C.J., Carpenter, M.J., Jardin, B., & Ostroff, J.S. (2013). Harm reduction and cessation efforts and interest in cessation resources among survivors of smoking-related cancers. Journal of Cancer Survivorship, 7, 44–54. doi:10.1007/s11764-012-0243-9
Bidstrup, P.E., Dalton, S.O., Christensen, J., Tjonneland, A., Larsen, S.B., Karlsen, R., . . . Johansen, C. (2013). Changes in body mass index and alcohol and tobacco consumption among breast cancer survivors and cancer-free women: A prospective study in the Danish Diet, Cancer and Health Cohort. Acta Oncologica, 52, 327–335. doi:10.3109/0284186X.2012.746466
Broderick, J.M., Hussey, J., Kennedy, M.J., & O’Donnell, D.M. (2014). Testing the ‘teachable moment’ premise: Does physical activity increase in the early survivorship phase? Supportive Care in Cancer, 22, 989–997. doi:10.1007/s00520-013-2064-4
Buhr, K. (2013). Access to medical care: How do women in Canada and the United States compare? Preventive Medicine, 56, 345–347. doi:10.1016/j.ypmed.2013.02.010
Bulmer, S.M., Howell, J., Ackerman, L., & Fedric, R. (2012). Women’s perceived benefits of exercise during and after breast cancer treatment. Women and Health, 52, 771–787. doi:10.1080/03630242.2012.725707
Campbell, M.K., Carr, C., Devellis, B., Switzer, B., Biddle, A., Amamoo, M.A., . . . Sandler, R. (2009). A randomized trial of tailoring and motivational interviewing to promote fruit and vegetable consumption for cancer prevention and control. Annals of Behavioral Medicine, 38, 71–85. doi:10.1007/s12160-009-9140-5
Cooley, M.E., Emmons, K.M., Haddad, R., Wang, Q., Posner, M., Bueno, R., . . . Johnson, B.E. (2011). Patient-reported receipt of and interest in smoking-cessation interventions after a diagnosis of cancer. Cancer, 117, 2961–2969. doi:10.1002/cncr.25828
Cooley, M.E., Finn, K.T., Wang, Q., Roper, K., Morones, S., Shi, L., . . . Hayman, L.L. (2013). Health behaviors, readiness to change, and interest in health promotion programs among smokers with lung cancer and their family members: A pilot study. Cancer Nursing, 36, 145–154. doi:10.1097/NCC.0b013e31825e4359
Cowens-Alvarado, R., Sharpe, K., Pratt-Chapman, M., Willis, A., Gansler, T., Ganz, P.A., . . . Stein, K. (2013). Advancing survivorship care through the National Cancer Survivorship Resource Center: Developing American Cancer Society guidelines for primary care providers. CA: A Cancer Journal for Clinicians, 63, 147–150. doi:10.3322/caac.21183
Craike, M.J., Hose, K., Courneya, K.S., Harrison, S.J., & Livingston, P.M. (2013). Perceived benefits and barriers to exercise for recently treated patients with multiple myeloma: A qualitative study. BMC Cancer, 13, 319. doi:10.1186/1471-2407-13-319
Demark-Wahnefried, W., Aziz, N.M., Rowland, J.H., & Pinto, B.M. (2005). Riding the crest of the teachable moment: Promoting long-term health after the diagnosis of cancer. Journal of Clinical Oncology, 23, 5814–5830. doi:10.1200/JCO.2005.01.230
Demark-Wahnefried, W., Morey, M.C., Sloane, R., Snyder, D.C., Miller, P.E., Hartman, T.J., & Cohen, H.J. (2012). Reach out to enhance wellness home-based diet-exercise intervention promotes reproducible and sustainable long-term improvements in health behaviors, body weight, and physical functioning in older, overweight/obese cancer survivors. Journal of Clinical Oncology, 30, 2354–2361.doi:10.1200/JCO.2011.40.0895
Demark-Wahnefried, W., Peterson, B., McBride, C., Lipkus, I., & Clipp, E. (2000). Current health behaviors and readiness to pursue life-style changes among men and women diagnosed with early stage prostate and breast carcinomas. Cancer, 88, 674–684. doi:10.1002/(SICI)1097-0142(20000201)88:3<674::AID-CNCR26>3.0.CO;2-R
Feuerstein, M., & Ganz, P.A. (2011). Quality health care for cancer survivors. In M. Feuerstein & P. Ganz (Eds.), Health services for cancer survivors: Practice, policy and research (pp. 373–383). New York, NY: Springer.
Green, H.J., Steinnagel, G., Morris, C., & Laakso, E.L. (2014). Health behaviour models and patient preferences regarding nutrition and physical activity after breast or prostate cancer diagnosis. European Journal of Cancer Care, 23, 640–652. doi:10.1111/ecc.12190
Jones, A., Gulbis, A., & Baker, E.H. (2010). Differences in tobacco use between Canada and the United States. International Journal of Public Health, 55, 167–175. doi:10.1007/s00038-009-0101-3
Karvinen, K.H., Raedeke, T.D., Arastu, H., & Allison, R.R. (2011). Exercise programming and counseling preferences of breast cancer survivors during or after radiation therapy [Online exclusive]. Oncology Nursing Forum, 38, E326–E334. doi:10.1188/11.ONF.E326-E334
McBride, C.M., Emmons, K.M., & Lipkus, I.M. (2003). Understanding the potential of teachable moments: The case of smoking cessation. Health Education Research, 18, 156–170. doi:10.1093/her/18.2.156
McBride, C.M., & Ostroff, J.S. (2003). Teachable moments for promoting smoking cessation: The context of cancer care and survivorship. Cancer Control, 10, 325–333.
O’Neill, J.E., & O’Neill, D.M. (2007). Health status, health care and inequality: Canada vs. the U.S. Retrieved from http://bit.ly/1RCh8FE
Patterson, F., Wileyto, E.P., Segal, J., Kurz, J., Glanz, K., & Hanlon, A. (2010). Intention to quit smoking: Role of personal and family member cancer diagnosis. Health Education Research, 25, 792–802. doi:10.1093/her/cyq033
Philip, E.J., Coups, E.J., Feinstein, M.B., Park, B.J., Wilson, D.J., & Ostroff, J.S. (2014). Physical activity preferences of early-stage lung cancer survivors. Supportive Care in Cancer, 22, 495–502. doi:10.1007/s00520-013-2002-5
Roundtree, A.K., Giordano, S.H., Price, A., & Suarez-Almazor, M.E. (2011). Problems in transition and quality of care: Perspectives of breast cancer survivors. Supportive Care in Cancer, 19, 1921–1929. doi:10.1007/s00520-010-1031-6
Sabiston, C.M., Brunet, J., Vallance, J.K., & Meterissian, S. (2014). Prospective examination of objectively assessed physical activity and sedentary time after breast cancer treatment: Sitting on the crest of the teachable moment. Cancer Epidemiology, Biomarkers and Prevention, 23, 1324–1330. doi:10.1158/1055-9965.EPI-13-1179
Sharp, L., Johansson, H., Fagerström, K., & Rutqvist, L.E. (2008). Smoking cessation among patients with head and neck cancer: Cancer as a ‘teachable’ moment. European Journal of Cancer Care, 17, 114–119. doi:10.1111/j.1365-2354.2007.00815.x
Szymlek-Gay, E.A., Richards, R., & Egan, R. (2011). Physical activity among cancer survivors: A literature review. New Zealand Medical Journal, 124, 77–89.
U.S. Census Bureau. (n.d.). Census regions and divisions of the United States. Retrieved from http://1.usa.gov/1LqCdlu
Vitolins, M.Z., Milliron, B.J., Hopkins, J.O., Fulmer, A., Lawrence, J., Melin, S., & Case, D. (2014). Weight loss intervention in survivors of ER/PR-negative breast cancer. Clinical Medicine Insights. Women’s Health, 7, 17–24. doi:10.4137/CMWH.S13955
Zhang, X., Geiss, L.S., Caspersen, C.J., Cheng, Y.J., Engelgau, M.M., Johnson, J.A., . . . Gregg, E.W. (2010). Physical activity levels and differences in the prevalence of diabetes between the United States and Canada. Preventive Medicine, 50, 241–245. doi:10.1016/j.ypmed.2010.02.015
About the Author(s)
Kristina Karvinen, PhD, and Brenda Bruner, PhD, are associate professors in the School of Physical and Health Education at Nipissing University in North Bay, Ontario, and Tracy Truant, RN, MSN, PhD, is an adjunct professor in the School of Nursing at the University of British Columbia in Vancouver, all in Canada. No financial relationships to disclose. Karvinen can be reached at kristinak@nipissingu.ca, with copy to editor at ONFEditor@ons.org. (Submitted December 2014. Accepted for publication May 5, 2015.)

