Cross-Cultural Communication in Oncology: Challenges and Training Interests
Purpose/Objectives: To survey oncology nurses and oncologists about difficulties in taking care of culturally and linguistically diverse patients and about interests in cross-cultural training.
Design: Descriptive, cross-sectional.
Setting: Web-based survey.
Sample: 108 oncology nurses and 44 oncologists.
Methods: 31-item questionnaire derived from preexisting surveys in the United States and Switzerland.
Main Research Variables: Self-rated difficulties in taking care of culturally and linguistically diverse patients and self-rated interests in cross-cultural training.
Findings: All respondents reported communication difficulties in encounters with culturally and linguistically diverse patients. Respondents considered the absence of written materials in other languages, absence of a shared common language with patients, and sensitive subjects (e.g., end of life, sexuality) to be particularly problematic. Respondents also expressed a high level of interest in all aspects of cross-cultural training (task-oriented skills, background knowledge, reflexivity, and attitudes). Nurses perceived several difficulties related to care of migrants as more problematic than physicians did and were more interested in all aspects of cross-cultural training.
Conclusions: The need for cross-cultural training is high among oncology clinicians, particularly among nurses.
Implications for Nursing: The results reported in the current study may help nurses in decision-making positions and educators in introducing elements of cross-cultural education into oncology curricula for nurses. Cross-cultural training should be offered to oncology nurses.
Jump to a section
Communication is a key issue in oncology, in which complex content must be discussed, serious diagnoses announced, and crucial decisions made (Stiefel, 2006). Consequently, communication skills training (CST) for oncology clinicians has been developed over the past three decades (Stiefel et al., 2010). The aim of such training is to enable clinicians to provide effective and patient-centered communication (Razavi et al., 2000). CST is proven to have a beneficial impact on not only clinicians’ communication behavior, but also on their levels of professional stress (Delvaux et al., 2004; Fallowfield et al., 2002; Libert et al., 2007).
Intense global migrations have resulted in specific challenges for oncology clinicians. Factors potentially confusing cancer-related communication may be linguistic, cultural, social, and organizational in nature (Pergert, Ekblad, Enskär, & Björk, 2007, 2008; Surbone, 2010; Swinglehurst, Roberts, Li, Weber, & Singy, 2014). Clinicians face specific communication difficulties related to cultural preferences for truth telling (Arraras et al., 2013; Catania et al., 2014; Cherny, 2011; Faysman, 2002; Mitchison et al., 2012; Surbone, 2006) and patient involvement in decision making (de Graaff, Francke, van den Muijsenbergh, & van der Geest, 2012; Kai, Beavan, & Faull, 2011; Surbone, 2008). Other potential communication difficulties result from language barriers, the use of interpreters (particularly if they are relatives of the patient), and the lack of written material in migrants’ languages (Pergert et al., 2007; Richardson, Thomas, & Richardson, 2006). Along with stereotypes and racial or ethnic biases, migrants’ health beliefs, living conditions, and limited health resources can obstruct clinicians’ communication with patients with cancer from an immigrant background (de Graaff et al., 2012; Pergert et al., 2007; Richardson et al., 2006; Surbone, 2008).
To deal with the difficulties of communicating with patients from diverse linguistic and cultural backgrounds, oncology clinicians need adequate cultural sensitivity and competency. Experience in other medical specialties has shown that clinicians can acquire cultural sensitivity and competency in courses and trainings, many of which are conceived in terms of the cultural competency framework (Beach et al., 2006; Betancourt, 2003; Betancourt, Green, Carrillo, & Ananeh-Firempong, 2003; Boyle, Sheridan, McClary, & White, 2002; Seeleman, Suurmond, & Stronks, 2009). According to this framework, cultural competency is primarily an institutional goal; hospital policies should provide clinicians, among others, with access to community interpreter services and experts in cross-cultural care who provide counsel and supervision to staff (Betancourt et al., 2003; Boyle et al., 2002). However, achieving this goal of cultural competency also requires that clinicians acquire specific knowledge, skills, and attitudes to help them provide quality care to culturally diverse patients (Althaus, Hudelson, Domenig, Green, & Bodenmann, 2010; Powell Sears, 2012).
Awareness that courses and training in cultural competency should be adapted to the specificities of the major fields of medicine is increasing (Butler et al., 2011; Schell, Green, Tulsky, & Arnold, 2013; Shields et al., 2009). In oncology, a few pilot projects have been carried out to design and implement cultural competency training (Maccioni, Etienne, & Efira, 2012; Quinn et al., 2011), but much work remains to be done. Several articles have elaborated on possible difficulties in oncology-related encounters between clinicians (mainly physicians and nurses) and patients from diverse backgrounds (Gibson, 2008; Pergert et al., 2007; Surbone, 2008, 2010; Yeo, Phillips, Delengowski, Griffiths, & Purnell, 2011), but an obvious need exists for exploratory empirical work in the field.
The current study aimed to establish (a) whether oncology clinicians experience specific difficulties when caring for patients from linguistically and culturally diverse backgrounds and, if so, which of those difficulties they consider to be more or less important than others; (b) whether clinicians already have taken courses or training in cross-cultural competency and which aspects of training they consider to be more or less interesting; and (c) whether oncology clinicians’ profession, gender, age, and work setting affect their perceived difficulties in cross-cultural care and their interest in receiving training in this field.
The current study took place in French-speaking Switzerland. Immigration to all linguistic regions of Switzerland has been strong for more than 50 years (Federal Statistical Office, 2015). Among the population aged older than 15 years, 28% are first-generation immigrants (Federal Statistical Office, 2015). The migrant population of Switzerland is highly diversified in terms of countries of origin, first language, proficiency in the local language, legal and immigrant status, and socioeconomic level (Federal Statistical Office, 2015). In the French-speaking part of Switzerland, a large proportion of non-natives are citizens of Southern European Latin countries, namely Portugal, Spain, and Italy. However, the immigrant population coming from geographically, linguistically, and culturally distant societies also is growing; about one-sixth of the non-natives living in Switzerland stem from African, Asian, or South American countries (Federal Statistical Office, 2015). Despite national specificities, most Western and Northern European and North American countries have been through similar demographic evolutions in their recent past (i.e., a steadily high or growing immigration with an increasing diversification of origins) (International Organization for Migration, 2015). Accordingly, the researchers’ results should be of interest to a large range of clinicians, teachers, and decision makers in various countries of the Western world.
Methods
Elaboration of the Inquiry Tool
The researchers created a questionnaire specifically focused on the current study aims. Three types of resources were used as bases for questionnaire items: other questionnaires used outside of oncology to investigate clinicians’ difficulties and training needs in cross-cultural care (Bodenmann, Faucherre, Diserens, Paroz, & Weber, 2011; Casillas et al., 2014; Hudelson, Dominice Dao, Perneger, & Durieux-Paillard, 2014; Park, Chun, Betancourt, Green, & Weissman, 2009), literature on cross-cultural communication in oncology (Maccioni et al., 2012; Quinn et al., 2011; Surbone, 2008), and a preparatory qualitative study the researchers conducted with training experts and clinicians in oncology. In the preparatory study, nine in-depth interviews (30–60 minutes) were conducted on the difficulties clinicians face with migrant patients and their training needs in the field of cultural competency. In this process, four oncology nurses—two clinic nurses and two senior nurses training other oncology nurses—actively contributed to the choice of the questionnaire items. A small multidisciplinary work group of sociolinguists and physicians then reviewed the formulation of the questionnaire items. The final version of the questionnaire was tested in a pilot group of oncology and psycho-oncology physicians and nurses.
Questionnaire
The questionnaire was in French and contained three parts. The first part investigated the frequency and degree to which difficulties that oncology clinicians encountered with migrant patients created problems. The initial question asked how frequently in their practice clinicians experienced communication difficulties related to the linguistic and cultural diversity of migrant patients. The response format was a four-point scale, with 1 indicating never, 2 rarely, 3 sometimes, and 4 often. In addition, 15 items measured the degree to which difficulties in three domains were problematic: (a) language (absence of a shared common language, collaboration with interpreters, and translation by relatives), (b) sociocultural background (patients’ level of understanding, patients’ perceptions of illness and the healthcare system, patient involvement in decision making, discussion of sensitive subjects, relatives’ roles in care, and clinicians’ stereotypes about groups of patients), and (c) missing institutional resources and background knowledge (access to interpreters, required efforts, availability of written materials in other languages, referent individuals in cross-cultural clinical work, knowledge on health and support networks for migrants, and knowledge of living conditions and residence status of migrants).
The second part of the questionnaire investigated clinicians’ past courses or training in cultural competency and aspects of training that they considered to be more or less interesting. This part started with a dichotomous yes or no question that asked whether clinicians had received any training in cultural competency. This question was followed by 15 items evaluating clinicians’ degree of interest in three domains: (a) communication issues (how to collaborate with interpreters, adapt nonverbal communication, and adjust speech to patients’ levels of comprehension), (b) a sociocultural background different from that of the clinician (how to explore patients’ expectations, investigate perceptions of disease and treatments, involve patients in decision making, introduce religion and spirituality to the discussion, share bad news, discuss sensitive subjects, collaborate with relatives, and cope with one’s own stereotypes about groups of patients), and (c) knowledge about migrant populations (historical and socioeconomic conditions of migrants, inequality in access to care, epidemiologic aspects of migration, and health and support networks for migrants). For both 15-item sections, responses were on a four-point scale, with 1 indicating not at all, 2 a little, 3 quite a bit, and 4 very much problematic or interested.
The third part of the questionnaire contained sociodemographic items on respondents’ gender, profession, work setting, age, country of birth, number of languages for potential use in consultations, and first language.
Data Collection Procedures
No exact statistical information is available on the population of physicians and nurses working in the field of oncology in French-speaking Switzerland. The researchers sent the questionnaire to all oncology clinicians in French-speaking Switzerland that they could identify. The researchers first established a complete inventory of the hospitals, clinics, and private practices offering oncology care from telephone directories, Google, and lists provided by professional associations. In every clinic and hospital, one or more people were then contacted and asked to send the email addresses of all of their oncology staff members. The questionnaire was sent to about 300–340 clinicians; the approximation is because in a few clinics, staff members could be reached only through collective email addresses, so the researchers could not establish the exact number of recipients. Respondents were invited by email to participate in the survey, and a link led them to the online questionnaire. Two email reminders were sent over a three-month period in 2013. The study protocol was approved by the Human Research Ethics Committee of Canton Vaud, Switzerland.
Data Analyses
The data obtained through the researchers’ questionnaire were subjected to statistical analysis. Because of the nominal nature of the collected data, two descriptive methods were used: frequency analysis and comparative analysis. An ordered dependent variable model was employed to check the statistical significance of the relationship between clinician characteristics and responses of the survey, using F-test in EViews. The variables with a 5% level of statistical significance are considered for additional analysis in this article.
Results
Sample
The approximate 300–340 respondents completed and returned 152 questionnaires, for a response rate of 45%–51%. This is acceptable in comparison to other surveys of clinicians on similar topics (Casillas et al., 2014; Hudelson et al., 2014). The majority of respondents were nurses, and responding clinicians were mostly women. The largest proportion of respondents worked in university hospitals or other hospitals or clinics. Most of the clinicians were able to conduct clinical interviews in two or more languages. Table 1 presents respondents’ sociodemographic characteristics.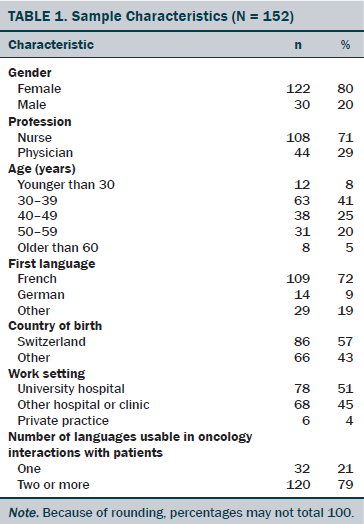
Difficulties in Clinical Communication With Migrant Patients
Responses for the item related to frequency of communication difficulties with migrant patients were distributed as follows: often, sometimes, and rarely. No clinicians answered that they had never had difficulties communicating with migrant patients.
Table 2 presents items and responses for the problems the difficulties posed. Based on the distribution of responses, the 15 items were grouped into three clusters. In cluster I, more than 80% of clinicians responded quite a bit or very problematic. In cluster II, 50%–80% of clinicians responded quite a bit or very problematic. In cluster III, less than 40% of clinicians responded “quite a bit” or “very” problematic.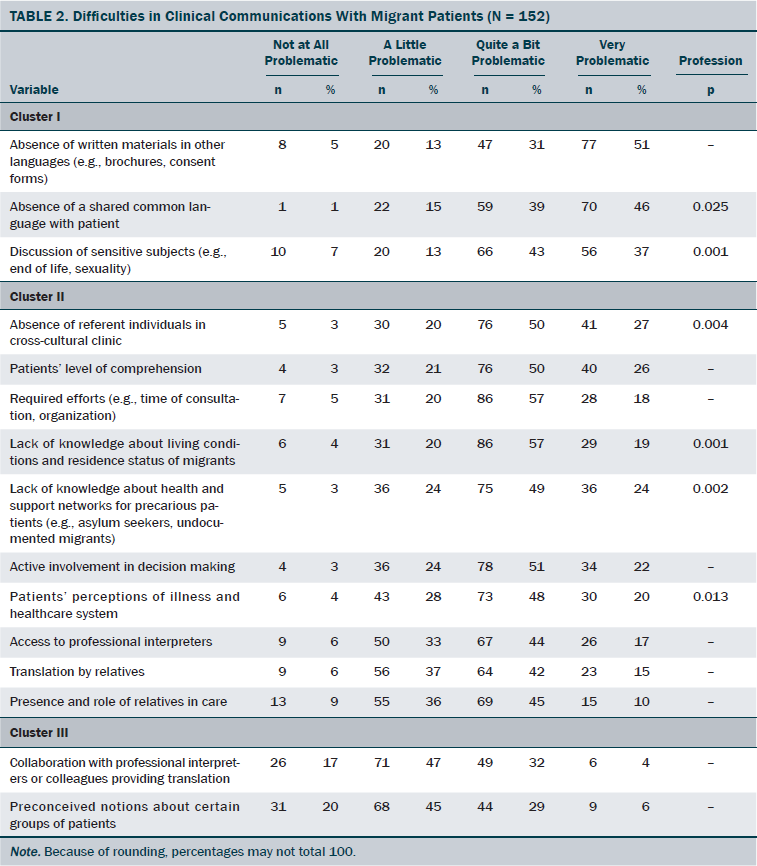
Only three difficulties appeared to be highly problematic (i.e., cluster I): absence of written materials in other languages, absence of a shared common language with patient, and discussion of sensitive subjects.
Ten items appeared to be problematic (cluster II): absence of referent individuals in cross-cultural clinical work, patients’ level of comprehension, required efforts (e.g., time of consultation, organization), lack of knowledge about living conditions and residence status of migrants in Switzerland, lack of knowledge about health and support networks for precarious patients, active involvement in decision making, patients’ perceptions of illness and the healthcare system, access to professional interpreters, translation by relatives, and the presence and role of relatives in care.
Two aspects appeared to be less problematic (cluster III): clinicians’ own preconceived notions about certain groups of patients and collaboration with interpreters.
No differences were found for subgroups based on age, work setting, training, or gender; only the profession was significant. Seven items were judged as more problematic by nurses than by physicians (p ≤ 0.025): absence of a shared common language with patients, absence of written materials in other languages, absence of a referent person in cross-cultural clinical work, lack of knowledge about living conditions of migrants, lack of knowledge about health and support networks for precarious patients, discussion of sensitive subjects, and patients’ perceptions of illness and the healthcare system.
Training Interests in Cultural Competency
The responses to the question of whether clinicians had received any training (e.g., courses, seminars) to improve their care for migrant patients were distributed as follows: no (n = 130, 85%); yes (n = 22, 15%). Therefore, a vast majority of clinicians had not yet received any training in this field.
Table 3 presents respondents’ interest in receiving training in the field of cultural competency. The respondents all expressed high levels of interest for all items. The lowest cumulative score for quite a bit and very interested was 87 (57%). In this article, the researchers describe the results according to the percentage of respondents who stated that they were very interested. The 15 items under scrutiny were clustered into three groups: cluster I (greater than 50% of clinicians responded very interested); cluster II (40%–50% responded very interested); and cluster III (less than 40% responded very interested).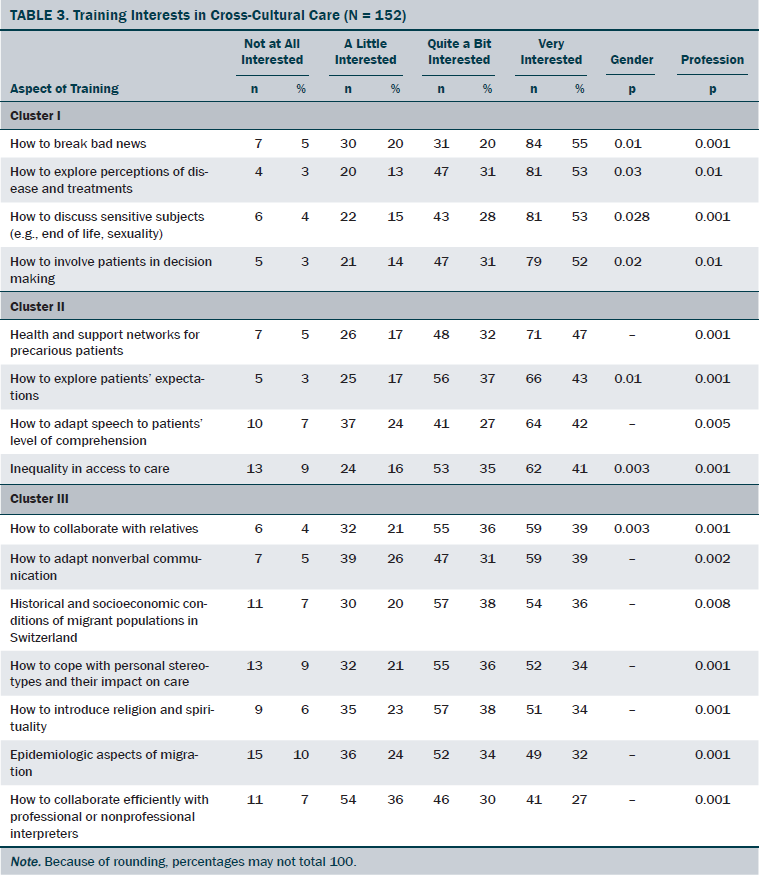
In cluster I, more than 50% of clinicians reported being very interested in four items: how to break bad news, how to explore perceptions of disease and treatments, how to discuss sensitive subjects, and how to involve patients in decision making.
In cluster II, 40%–50% of clinicians rated four training items as very interesting: health and support networks for precarious patients, how to explore patients’ expectations, how to adapt speech to the patients’ level of comprehension, and inequality in access to care.
In cluster III, less than 40% of clinicians reported that seven training items were very interesting: collaboration with relatives, nonverbal communication, historical and socioeconomic conditions of migrant populations in Switzerland, clinicians’ personal stereotypes and their impact on care, the introduction of religion and spirituality to discussions, epidemiologic aspects of migration, and efficient collaboration with interpreters.
Significant differences were found for profession and gender. Nurses are significantly more interested than physicians in all training items (p < 0.005 and p < 0.001, respectively). In addition, women expressed more interest than men for seven items (p < 0.03 and p < 0.01, respectively): breaking bad news, exploring perceptions of disease and treatments, discussing sensitive subjects, involving patients in decision making, exploring patients’ expectations, collaborating with relatives, and learning about inequalities in access to care.
Discussion
The current study is the first systematic investigation of the importance of various difficulties that oncology clinicians experience in their practice with patients from diverse linguistic and cultural backgrounds. Thanks to new insights into oncology clinicians’ training interests, the current study also offers important information for teaching staff members who are planning to introduce training in cross-cultural clinical competency.
Most clinician respondents (n = 115, 76%) reported at least occasional communication difficulties related to the linguistic, cultural, and social diversity of their migrant patients. Therefore, communication difficulties related to diversity are everything but marginal in oncology clinicians’ perception of their daily practice.
Among the 15 items on potential difficulties in cross-cultural care, 84 clinician respondents (55%) evaluated 13 items as problematic or highly problematic, which confirms the findings of previous studies on the difficulties faced in working with migrant patients in oncology (Maccioni et al., 2012; Pergert et al., 2007, 2008).
In practical terms, the difficulties oncology clinicians consider to be problematic call not only for the implementation of training in cultural competency, but also for institutional changes in hospitals, such as policies that foster access to professional interpreters, referent individuals in cross-cultural clinical work, and informational leaflets in multiple languages.
Respondents found only two potential sources of difficulties to be less problematic: collaboration with professional and nonprofessional interpreters, and the impact of the clinicians’ own preconceived notions about certain groups of patients. Respondents clearly consider collaboration with interpreters to be less of a problem than translation by relatives. This is probably because many oncology clinicians rarely call on interpreter services because patients with cancer often consult with bilingual relatives (Surbone, 2008). Regarding clinicians’ stereotypes and biases, many clinicians reported that their own perceptions of groups of patients did not matter as much compared to other barriers to qualitative cross-cultural care. This may be a result of social desirability effects (Nederhof, 1985), but this also may be the expression of relatively low self-reflection among oncology clinicians. Precisely because self-reflection is deemed so difficult, the literature on the cultural competency approach considers it to be the foundation of cross-cultural care (Althaus et al., 2010; Betancourt et al., 2003), with courses on stereotypes and bias being a primary step toward cultural competency education.
This study provides insights into the interests of oncology clinicians in various domains of cross-cultural training. Above all, the data show a high level of interest in all aspects proposed in the questionnaire. This is probably closely related to the fact that only a small number of clinicians (n = 22, 15%) reported having prior training in cross-cultural care. The high interest in all items seems to confirm the central idea of existing cross-cultural competency frameworks: that courses in cross-cultural competency in oncology (Surbone, 2010) and in other fields of medicine (Betancourt et al., 2003) should focus on cultural sensitivity and awareness (e.g., work on prejudice and stereotypes), background knowledge about migrants (e.g., healthcare inequalities, living conditions), and particular task-oriented communication skills for cross-cultural oncology care (e.g., breaking bad news, exploring perceptions of disease and treatment, discussing sensitive subjects, involving patients in decision making). This study’s sample validates the relevance of cross-cultural competency training frameworks for oncology. However, if all aspects of training appear to be a high priority for clinicians, then of note is that clinicians are particularly interested in specific communication skills for cross-cultural oncology care.
A striking finding of the current study is that interest in training is high even for the two aspects considered to be less problematic in clinical work (collaboration with interpreters other than relatives and clinicians’ own stereotypes about certain patient groups). This finding is difficult to interpret.
Other interesting findings of the current study are related to the impact of profession and gender on the distribution of responses. Nurses perceived several difficulties as more problematic than physicians did, and they were significantly more interested in all aspects of training. Casillas et al. (2014) also documented that nurses judge themselves lower on self-assessed cross-cultural skillfulness than physicians. This discrepancy may be because nurses are more critical of themselves or have higher expectations of themselves than physicians do, perhaps because they are often more familiar with cross-cultural care.
In addition, the results of the current study show that women are more interested in several training items than men. A link can be established with previous results on gender and clinician–patient interaction, which suggests that female clinicians are more sensitive to communication issues than their male colleagues are (Roter & Hall, 2004; Singy, 2005).
Limitations
As an exploratory study, the current research has several limitations. First, as in other comparable studies (Casillas et al., 2014; Hudelson et al., 2014), self-selection biases cannot be excluded. Namely, respondents of the survey are likely to be more sensitive and interested in cross-cultural difficulties and education than the nonrespondents are.
The current study was conducted by sending oncology nurses and oncologists a link to an online survey. For structural reasons, the researchers had access to neither exact data on the population of oncology clinicians in the current study area nor full data on the clinicians who received the questionnaire. Therefore, the researchers cannot establish precisely the representativeness of the sample. For this same reason, the researchers could calculate participation only approximately, but this approximate rate was satisfactory.
With respect to the impact of gender and profession on training interests, the comparatively small size of the sample did not allow for fully reliable multivariate analyses. Additional studies with a larger sample are needed to grasp the extent to which gender effects and profession effects are mutually independent or connected and, if the latter, which variable is predominant.
Implications for Nursing
In Western healthcare systems, oncology nurses are assuming growing responsibilities in the treatment and accompaniment of patients with cancer (e.g., nurse navigators, case managers). As a consequence, they have to handle increasingly complex clinical interactions. The current study in French-speaking Switzerland shows that many aspects of communication with linguistically and culturally diverse migrant patients are perceived as problematic by oncology nurses. These results emphasize that the linguistic and cultural diversity in patients may render already complex nurse–patient interactions even more complex.
The surveyed oncology nurses are also highly interested in education on cross-cultural communication, particularly in comparison to physicians. In practice, this means that oncology nurses may be easier to reach than physicians with offers of voluntary cross-cultural training.
Strong similarities between the context of the current survey and other European and North American contexts (e.g., steadily high or increasing immigration, diversification of origins in migrants, absence of coherent curricula in cross-cultural training for oncology clinicians, limited access to professional interpreters) make the researchers’ findings largely transferable to other Western oncology settings. The findings suggest that oncology nurses in decision-making positions have good reasons to promote and organize educational initiatives in cross-cultural clinical communication and other cultural competency measures (e.g., referent people in cross-cultural care, information leaflets in various languages, professional interpreters). Both types of development should not only lead to higher quality care, but also to less difficult clinical encounters for the nursing workforce. Even though the current study focused specifically on clinical communication with migrant patients, cultural competency measures also should address other dimensions of social and cultural diversity in patients (e.g., socioeconomic disparities, nonmigrant ethnicities like African Americans or Native Americans in North America, gender, sexual orientation).
Conclusion
The current study provides new insights into the largely unexplored domain of cross-cultural care in oncology. It shows that oncology clinicians experience difficulties in caring for patients from linguistically and culturally diverse backgrounds, and it provides information on which difficulties they perceive as more and less important than others. It also shows that a large majority of the clinicians have never had courses or training in cultural competency, and they are highly interested in all aspects of such training. Nurses are significantly more interested in cross-cultural training than physicians, and they perceive several aspects of care as more problematic. Other qualitative and quantitative studies should follow this work, including projects aimed to implement cultural competency measures in oncology settings. 
References
Althaus, F., Hudelson, P., Domenig, D., Green, A.R., & Bodenmann, P. (2010). Compétences cliniques transculturelles et pratique médicale: Quels besoins, quels outils, quel impact? Forum Medical Suisse, 10(5), 79–83.
Arraras, J.I., Greimel, E., Chie, W.C., Sezer, O., Bergenmar, M., Costantini, A., . . . Velikova, G. (2013). Cross-cultural differences in information disclosure evaluated through the EORTC questionnaires. Psycho-Oncology, 22, 268–275. doi:10.1002/pon.2088
Beach, M.C., Gary, T.L., Price, E.G., Robinson, K., Gozu, A., Palacio, A., . . . Cooper, L.A. (2006). Improving health care quality for racial/ethnic minorities: A systematic review of the best evidence regarding provider and organization interventions. BMC Public Health, 6, 104. doi:10.1186/1471-2458-6-104
Betancourt, J.R. (2003). Cross-cultural medical education: Conceptual approaches and frameworks for evaluation. Academic Medicine, 78, 560–569. doi:10.1097/00001888-200306000-00004
Betancourt, J.R., Green, A.R., Carrillo, J.E., & Ananeh-Firempong, O., II. (2003). Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Reports, 118, 293–302. doi:10.1016/S0033-3549(04)50253-4
Bodenmann, P., Faucherre, F., Diserens, E.-A., Paroz, S., & Weber, O. (2011). Projet pilote Migrant Friendly Hospitals. Phase A: Evaluation des acquis et des besoins. Retrieved from http://www.reiso.org/IMG/pdf/MFH_phase_A_Analyse_situation_initiale.pdf
Boyle, D.A., Sheridan, A., McClary, J., & White, J. (2002). A multifocal education strategy to enhance hospital-based cultural competency in professional staff. Oncology Nursing Forum, 29, 764–768. doi:10.1188/02.ONF.764-768
Butler, P.D., Swift, M., Kothari, S., Nazeeri-Simmons, I., Friel, C.M., Longaker, M.T., & Britt, L.D. (2011). Integrating cultural competency and humility training into clinical clerkships: Surgery as a model. Journal of Surgical Education, 68, 222–230.
Casillas, A., Paroz, S., Green, A.R., Wolff, H., Weber, O., Faucherre, F., . . . Bodenmann, P. (2014). Cultural competency of health-care providers in a Swiss University Hospital: Self-assessed cross-cultural skillfulness in a cross-sectional study. BMC Medical Education, 14, 19. doi:10.1186/1472-6920-14-19
Catania, C., Radice, D., Spitaleri, G., Adamoli, L., Noberasco, C., Delmonte, A., . . . De Pas, T. (2014). The choice of whether to participate in a phase I clinical trial: Increasing the awareness of patients with cancer. An exploratory study. Psycho-Oncology, 23, 322–329. doi:10.1002/pon.3424
Cherny, N.I. (2011). Factors influencing the attitudes and behaviors of oncologists regarding the truthful disclosure of information to patients with advanced and incurable cancer. Psycho-Oncology, 20, 1269–1284. doi:10.1002/pon.1853
de Graaff, F.M., Francke, A.L., van den Muijsenbergh, M.E., & van der Geest, S. (2012). Understanding and improving communication and decision-making in palliative care for Turkish and Moroccan immigrants: A multiperspective study. Ethnicity and Health, 17, 363–384. doi:10.1080/13557858.2011.645152
Delvaux, N., Razavi, D., Marchal, S., Brédart, A., Farvacques, C., & Slachmuylder, J.L. (2004). Effects of a 105 hours psychological training program on attitudes, communication skills and occupational stress in oncology: A randomised study. British Journal of Cancer, 90, 106–114. doi:10.1038/sj.bjc.6601459
Fallowfield, L., Jenkins, V., Farewell, V., Saul, J., Duffy, A., & Eves, R. (2002). Efficacy of a Cancer Research UK communication skills training model for oncologists: A randomised controlled trial. Lancet, 359(9307), 650–656. doi:10.1016/S0140-6736(02)07810-8
Faysman, K. (2002). Cultural dimensions of anxiety and truth telling. Oncology Nursing Forum, 29, 757–759. doi:10.1188/02.ONF.757-759
Federal Statistical Office. (2015). Migration and integration. http://www.bfs.admin.ch/bfs/portal/en/index/themen/01/07.html
Gibson, F. (2008). The cultural context of communicating complex information to parents of children with cancer—Not just a linguistic obstacle. European Journal of Oncology Nursing, 12(1), 2–3. doi:10.1016/j.ejon.2008.01.004
Hudelson, P., Dominice Dao, M., Perneger, T., & Durieux-Paillard, S. (2014). A “migrant friendly hospital” initiative in Geneva, Switzerland: Evaluation of the effects on staff knowledge and practices. PLOS ONE. Retrieved from http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0106758
International Organization for Migration. (2015). World migration report 2015. http://publications.iom.int/system/files/wmr2015_en.pdf
Kai, J., Beavan, J., & Faull, C. (2011). Challenges of mediated communication, disclosure and patient autonomy in cross-cultural cancer care. British Journal of Cancer, 105, 918–924. doi:10.1038/bjc.2011.318
Libert, Y., Merckaert, I., Reynaert, C., Delvaux, N., Marchal, S., Etienne, A.M., . . . Razavi, D. (2007). Physicians are different when they learn communication skills: Influence of the locus of control. Psycho-Oncology, 16, 553–562. doi:10.1002/pon.1098
Maccioni, J., Etienne, A., & Efira, A. (2012). Le patient étranger face au cancer: Projet d’accompagnement multiculturel. Santé Conjuguée, 59, 13–17.
Mitchison, D., Butow, P., Sze, M., Aldridge, L., Hui, R., Vardy, J., . . . Goldstein, D. (2012). Prognostic communication preferences of migrant patients and their relatives. Psycho-Oncology, 21, 496–504. doi:10.1002/pon.1923
Nederhof, A.J. (1985). Methods of coping with social desirability bias: A review. European Journal of Social Psychology, 15, 263–280. doi:10.1002/ejsp.2420150303
Park, E.R., Chun, M.B., Betancourt, J.R., Green, A.R., & Weissman, J.S. (2009). Measuring residents’ perceived preparedness and skillfulness to deliver cross-cultural care. Journal of General Internal Medicine, 24, 1053–1056. doi:10.1007/s11606-009-1046-1
Pergert, P., Ekblad, S., Enskär, K., & Björk, O. (2007). Obstacles to transcultural caring relationships: Experiences of health care staff in pediatric oncology [published erratum appears in Journal of Pediatric Oncology Nursing, 25, 56]. Journal of Pediatric Oncology Nursing, 24, 314–328. doi:10.1177/1043454207308066
Pergert, P., Ekblad, S., Enskär, K., & Björk, O. (2008). Bridging obstacles to transcultural caring relationships—Tools discovered through interviews with staff in pediatric oncology care. European Journal of Oncology Nursing, 12, 35–43. doi:10.1016/j.ejon.2007.07.006
Powell Sears, K. (2012). Improving cultural competence education: The utility of an intersectional framework. Medical Education, 46, 545–551. doi:10.1111/j.1365-2923.2011.04199.x
Quinn, G.P., Jimenez, J., Meade, C.D., Muñoz-Antonia, T., Gwede, C.K., Castro, E., . . . Brandon, T.H. (2011). Enhancing oncology health care provider’s sensitivity to cultural communication to reduce cancer disparities: A pilot study. Journal of Cancer Education, 26, 322–325. doi:10.1007/s13187-011-0223-1
Razavi, D., Delvaux, N., Marchal, S., De Cock, M., Farvacques, C., & Slachmuylder, J.L. (2000). Testing health care professionals’ communication skills: The usefulness of highly emotional standardized role-playing sessions with simulators. Psycho-Oncology, 9, 293–302.
Richardson, A., Thomas, V.N., & Richardson, A. (2006). “Reduced to nods and smiles”: Experiences of professionals caring for people with cancer from black and ethnic minority groups. European Journal of Oncology Nursing, 10, 93–101. doi:10.1016/j.ejon.2005.05.002
Roter, D.L., & Hall, J.A. (2004). Physician gender and patient-centered communication: A critical review of empirical research. Annual Review of Public Health, 25, 497–519.
Schell, J.O., Green, J.A., Tulsky, J.A., & Arnold, R.M. (2013). Communication skills training for dialysis decision-making and end-of-life care in nephrology. Clinical Journal of the American Society of Nephrology, 8, 675–680. doi:10.2215/CJN.05220512
Seeleman, C., Suurmond, J., & Stronks, K. (2009). Cultural competence: A conceptual framework for teaching and learning. Medical Education, 43, 229–237. doi:10.1111/j.1365-2923.2008.03269.x
Shields, H.M., Leffler, D.A., White, A.A., III, Hafler, J.P., Pelletier, S.R., O’Farrell R.P., . . . Peters, A.S. (2009). Integration of racial, cultural, ethnic, and socioeconomic factors into a gastrointestinal pathophysiology course. Clinical Gastroenterology and Hepatology, 7, 279–284. doi:10.1016/j.cgh.2008.10.012
Singy, P. (2005). Langue, médecine et genre. In H. Geissner (Ed.), Kommunikationskulturen. Intra- und interkulturell (pp. 87–93). St. Ingbert: Roehrig-Universitätsverlag.
Stiefel, F. (2006). Communication in cancer care. Berlin: Springer.
Stiefel, F., Barth, J., Bensing, J., Fallowfield, L., Jost, L., Razavi, D., & Kiss, A. (2010). Communication skills training in oncology: A position paper based on a consensus meeting among European experts in 2009. Annals of Oncology, 21, 204–207. doi:10.1093/annonc/mdp564
Surbone, A. (2006). Telling the truth to patients with cancer: What is the truth? Lancet Oncology, 7, 944–950.
Surbone, A. (2008). Cultural aspects of communication in cancer care. Supportive Care in Cancer, 16, 235–240. doi:10.1007/s00520-007-0366-0
Surbone, A. (2010). Cultural competence in oncology: Where do we stand? Annals of Oncology, 21, 3–5.
Swinglehurst, D., Roberts, C., Li, S., Weber, O., & Singy, P. (2014). Beyond the ‘dyad’: A qualitative re-evaluation of the changing clinical consultation. BMJ Open. Retrieved from http://bmjopen.bmj.com/content/4/9/e006017.full
Yeo, T.P., Phillips, J., Delengowski, A., Griffiths, M., & Purnell, L. (2011). Oncology nursing: Educating advanced practice nurses to provide culturally competent care. Journal of Professional Nursing, 27, 245–254. doi:10.1016/j.profnurs.2011.03.004
About the Author(s)
Weber is a research manager, Sulstarova is a researcher, and Singy is a professor, all in the Department of Psychiatry at the University Hospital of Lausanne in Switzerland. This research was funded by a grant from the Forum for Bilingualism, Biel/Bienne in Switzerland. Weber, Sulstarova, and Singy contributed to the conceptualization and design, collection of data, analysis, and manuscript preparation. Sulstarova and Singy provided statistical support. Weber can be reached at orest.weber@chuv.ch, with copy to editor at ONFEditor@ons.org. Submitted March 2015. Accepted for publication June 7, 2015.

