Decision-Making Styles and Levels of Involvement Concerning Breast Reconstructive Surgery: An Israeli Study
Purpose/Objectives: To address decision-making styles among breast cancer survivors considering breast reconstruction.
Design: A primary analysis of a cross-sectional sample among survivors who chose to have breast reconstruction to examine correlations among patient age, decision-making style, and the level of involvement of decision making.
Setting: Hadassah Medical Center in Jerusalem, Israel.
Sample: 70 women who had undergone breast reconstruction surgery in the past five years.
Methods: Participants completed decision-making style and demographic questionnaires and an assessment of their level of involvement in the decision-making process.
Main Research Variables: Level of involvement in decision making, decision-making model between provider and patient, and decision-making styles were examined.
Findings: No correlation was found between four main decision-making styles and patient age or the extent of patient decision-making involvement and age. A statistically significant correlation was found between the level of involvement in decision making and the decision-making style of the patient.
Conclusions: Nurses should assess patient decision-making styles to ensure maximum patient involvement in the decision-making process based on personal desires regardless of age.
Implications for Nursing: Nurses working in breast cancer care must address the decision-making process of patients diagnosed with breast cancer, including the choice to undergo breast reconstruction after mastectomy. Nurses should understand the complex factors that influence a woman’s decision-making style to best help with the decision.
Jump to a section
Breast cancer is the most common malignant tumor found among women in the Western world. In Israel, one in eight women will be diagnosed with breast cancer at some point during her life (Ministry of Health Israel, 2015). Of the 4,000 women diagnosed with breast cancer each year in Israel, about one-fifth will undergo a mastectomy, and 30% of them (about 240 women per year) will have breast reconstructive surgery (Barnea, 2014). Many factors influence whether a woman will choose breast reconstruction after mastectomy. This decision making is a complex process influenced by a myriad of factors. The treating clinician and auxiliary support healthcare personnel play a crucial role in a woman’s decision to choose postmastectomy reconstruction, a choice with considerable psychological and social ramifications. Although many studies have examined why women choose breast reconstruction and whether they are satisfied with their choice, little is known about what factors influence Israeli women in particular regarding their decision-making processes. This population is interesting because of its broad spectrum of nationalities and ethnicities that, in some cases, emigrated from healthcare systems dominated by the paternalistic model (Davidovitch, Filc, Novack, & Balicer, 2013). In addition, the Israeli female population is comprised of about 693,000 Arab Muslim women, 63,000 Christian Arab women, 65,000 Druze women, and 3,059,000 Jewish women (Israel Central Bureau of Statistics, 2014). Although no exact statistics exist, it is estimated that, of the Jewish female population, 12% consider themselves to be Orthodox, and 14% define themselves as Ultra-Orthodox in their religious practices (Malhi & Abromovsky, 2014)
Given that such a high percentage of women in Israel will undergo mastectomy, understanding what influences these women’s choices concerning the extent of their subsequent breast reconstruction is important. Age and the degree of involvement are factors influencing the decision-making process (Budden, Pierce, Hayes, & Buettner, 2003; Pierce, 1995). Therefore, the authors decided to investigate how those factors affect the decision-making process of patients in Israel.
Postmastectomy Reconstructive Surgery
Breast reconstruction after mastectomy has undergone significant progress since the 1980s. The evolution from prosthetic implants to reconstruction using autologous tissue has led to a wider variety of postmastectomy reconstructive options (Hinkle & Cheever, 2013; Reddy et al., 2011). In addition to deciding whether to opt for breast reconstruction at all, a woman must also decide the particular method for reconstruction (i.e., alloplastic reconstruction using a silicone or saline implant or autologous reconstruction using her own body tissue). Postmastectomy reconstruction is strongly influenced by the size and shape of the original breast, body habitus, age, previous medical conditions, smoking history, and current adjuvant therapies (Cordeiro, 2008). Cancer stage or chest wall involvement may also influence the timing of the reconstruction (Hinkle & Cheever, 2013; Reddy et al., 2011). Many women will be asked not only to decide whether to have their breast reconstructed, but also to have a role in deciding which type of reconstructive breast surgery to be performed. The decisions of whether to undergo reconstruction and which type of reconstruction are usually made with the plastic surgeon. The patient and doctor must consider medical aspects regarding the treatment of the cancer and the personal preferences of the woman.
Decision Making
Patient decision making has been studied widely to better understand how a patient arrives at a final conclusion and to recognize what factors influence this decision-making process. Seminal research by Janis and Mann (1977) defined the seven processes necessary to make an informed decision: (a) identifying the problem, (b) weighing the pros and cons of each alternative, (c) seeking out relevant information to clarify those pros and cons, (d) testing and taking into account any new information, (e) reviewing the possible results and consequences of the decision, (f) making the decision, and (g) preparing a plan for implementation. Further research during subsequent decades has shown a multitude of factors that influence this process at any one of these steps, such as personal characteristics, values, beliefs, expectations, level of personal involvement, attitudes toward health-related and non–health-related issues, and the relationship between patient and treating physician (El-Wakeel, Taylor, & Tate, 2006; Janis & Mann, 1977; Lee, Hultman, & Sepucha, 2010; Popejoy, 2005).
Role of the Physician in Patient Decision Making
The decision about medical treatment in general and postmastectomy breast reconstruction in particular is made by the patient, physician, or both. Some physicians assume that patients naturally prefer that the provider make any final decision regarding treatment (Beaver et al., 2007). However, at times, the physician minimizes the patient’s desire to be involved in the decision-making process (Butow, Harrison, & Choy, 2007; Kleeberg, Feyer, Günther, & Behrens, 2008). In addition, studies have shown that the reconstructive decision is sometimes made without considering the patient’s thoughts about her specific desires and needs (Lee, Chen, et al., 2010). In general, the various combinations of patient and physician roles in the decision-making process can be categorized into one of four models: (a) paternalistic, (b) informed, (c) professional as agent, and (d) shared decision making (SDM). The paternalistic model places the medical provider as the sole decision maker, taking the patient’s best interests and needs into account. The informed model assumes that, by providing information to the patient, the physician is empowering the patient to make the decision totally independently. In the professional-as-agent model, the provider queries the patient regarding goals, interests, and desires but makes the final treatment decision based on her answers to those inquires. In SDM, the patient and physician are involved in sharing information and equally participate in the eventual decision (Charles, Gafni, & Whelan, 1999).
In the past, the paternalistic model, in which the patient is passive and the provider is the dominant figure, was the most accepted decision-making modality. Since 1978, most of the Western world has abandoned that model for one that empowers the patient to become more involved in the process. Studies have shown that most patients prefer to be informed about all of their options before any decision is made, but, in the end, many patients do not want to make the final decision (Elwyn, Hutchings, & Edwards, 2005; Levinson, Kao, Kuby, Thisted, 2005; Visser & Winslow, 2003).
Decision-Making Styles
Although SDM has become a goal to increase quality of care, particularly in patients with cancer, not all women want to make medical decisions alone. Studies have focused on the various levels of patient and physician involvement within the decision-making process, and an overall split of preference exists between the three possible options (patient alone, physician alone, and shared) (Hawley, Lantz, & Janz, 2007; Vogel, Helmes, & Hasenburg, 2008). Specific personality traits influence a woman’s desire for more or less physician involvement when making a decision. By identifying specific styles prior to assessment, the healthcare professional may better meet the individual needs of the woman. One such instrument, designed by Pierce (1995), is an easy-to-complete questionnaire that identifies specific decision-making style types prior to the physician–patient interaction.
A lack of information exists regarding the extent of shared physician–patient decision making in general and in the area of postmastectomy breast reconstruction in particular in this population in Israel. The goal of this study, therefore, was to apply Pierce’s (1995) model to an Israeli female population undergoing postmastectomy breast reconstruction to shed light on the decision-making process and show possible associations with patient age.
Methods
This cross-sectional study used purposive sampling within the Hadassah Medical Center in Jerusalem, Israel. Ethical approval was received from the sponsoring medical center.
The sample included Israeli women who were literate in Hebrew, aged older than 18 years when diagnosed with breast cancer, and had undergone breast reconstruction within the past five years. Women were identified from medical records and invited to participate.
From January to April 2011, possible participants were recruited. A list was compiled of all the women who had undergone breast reconstructive surgery at the sponsoring tertiary medical center within the past five years. Questionnaires, an informed consent form, and a stamped envelope were sent to all the women on the list with the request to complete the questionnaires and send them back to the researcher. One month after posting, the researcher called the women to confirm that they had received the questionnaires and encouraged them to complete the forms if they had not already done so. The questionnaire was also distributed to women who were attending the plastic surgery clinic in the medical center and to women in the plastic surgery ward after undergoing reconstructive surgery. A minimum sampling of 80 women was needed for an 80% power analysis and an alpha of 0.05, assuming an attrition rate of 15%.
Measures
A questionnaire was created for this study that included age, place of birth, marital status, education, income, religious affiliation, time of surgery, type of surgery and status (delayed versus immediate), bilateral or unilateral mastectomy, type of reconstruction (implants, own tissue, or both), source of information about reconstruction (surgeon, plastic surgeon, breast care nurse specialist, social worker, or friend), level of involvement in decision making, and decision-making style (physician, shared decision, professional as agent, or independent). Two questions were used to test the level of involvement in decision making. Patients were asked, “What was the extent of your involvement in the decision-making process?” Possible responses included “not involved,” “slightly involved,” and “highly involved.” Patients were then asked, “How were decisions made about your breast reconstruction?” Possible responses included, “the physician decided,” “the physician and I decided together,” “the physician decided after hearing my opinion,” and “I decided after hearing the physician’s opinion.”
The Michigan Assessment of Decision Style Questionnaire (MADS) (Pierce, 1995) helps determine the style women use when making breast cancer–related decisions. The 16-item questionnaire contains four factors: avoiding (when the patient avoids making the decision and taking responsibility), deferring (when the patient agrees to the advice of the physician), information seeking (when the patient has a systematic means of reaching a decision), and deliberation (when the patient prefers to gather information to make a shared decision with the expert physician). Responses range from 1 (strongly disagree) to 5 (strongly agree). The initial instrument had high reliability scores that were validated in other English-speaking countries (Budden et al., 2003), as well as translated and validated in Hebrew (Kadmon, Pierce & Antonakos, 2012).
Statistical Analysis
In this study, a total of 30 variables were analyzed. To calculate and compare the MADS styles, the four questions were averaged to provide a final score. The research hypotheses were analyzed using linear regression. Logistic regression and the differential were used depending on the question (alpha = 0.05). Age was analyzed using linear regression and correlated to decision-making styles. Age was also analyzed using logistic regression and correlated to level of involvement. The differentials were all used depending on the question with an alpha of 0.05. The correlation between decision-making styles and level of involvement was analyzed using analysis of variance.
Results
A total of 70 women participated in the final study. The mean age of the participants was 52.7 years (SD = 10.2), with a median age of 52 years. The sociodemographic characteristics of the sample are summarized in Table 1.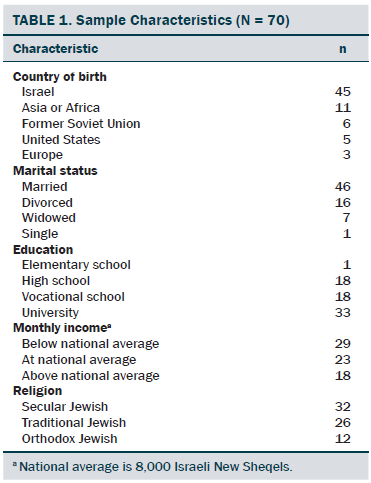
Thirty-eight women had chosen a mastectomy and immediate reconstruction, and the rest had reconstructive surgery later. In 70% of cases, the mastectomy was unilateral; in the rest, it was bilateral. Sixty-two women had chosen the surgery because of the presence of cancer; four women had chosen prophylactic mastectomies. Fifty-five women had chosen the surgery because of the presence of cancer; four had chosen prophylactic mastectomies. With 55 of the participants, implants were used; 6 had autologous reconstruction, and 9 received a combination of autologous tissue and implants.
The variance within the variable time from surgery until the study was analyzed to determine whether distance from time of surgery until the study influenced patient response. The authors found that this did not influence patient’s perception of involvement in the decision-making process.
When asked about involvement in decision making, 59 of the women felt that they had been very involved, 9 felt they had been only slightly involved, and 2 felt they were not involved at all. For final breast reconstruction decision, 4 stated that the surgeon alone had made the decision, 6 said the surgeon had decided after hearing from them, 26 said that it was a shared decision, and 34 said they had made the decision on their own after discussing all of their concerns with the physician.
No statistically significant association was found between the type of decision-making style and age (avoidance: p = 0.53, deferring responsibility: p = 0.72, information seeking: p = 0.22, and deliberation: p = 0.17). In addition, no statistically significant correlation was found between age and level of involvement in the decision-making process (p = 0.18). No other sociodemographic variables were associated with decision-making style.
A statistically significant correlation was found between the level of involvement in decision making and the decision-making style of the patient. Women who stated that the physician made the decision alone without or after having heard their opinions voiced had a significantly higher avoidance score than those in the other groups (p = 0.0001). This strength of correlation was also seen in those that deferred responsibility. Women possessing these two decision-making styles (avoidance and deferred responsibility) were significantly more likely to have the physician make the decision alone, with or without having their concerns heard (p = 0.02). However, a trend was seen between the increasing age of the patient and the likelihood of her engaging in the deliberation style of decision making, but it was not statistically significant.
Discussion
To better understand the quality of information provided to Israeli women who undergo unilateral or bilateral mastectomy who make a decision about breast reconstruction, this study sought to examine the relationship among patient age, type of decision-making style, and level of involvement in decision making.
The effect of age on decision-making styles among Israeli women has been examined in the literature among female patients with breast cancer, but the literature is limited (Miron-Shatz, Golan, Brezis, Siegal, & Doniger, 2012). Previous studies have shown that, among women from any nationality who had undergone mastectomy alone (unilateral or bilateral), age was found not to have a statistically significant correlation with level of involvement in final decision making. However, the choice of mastectomy or breast-conserving surgery did correlate with certain age groups, such as older women preferring mastectomy and younger women preferring breast-conserving surgery (Bleicher, Abrahamse, Hawley, Katz, & Morrow, 2008; Romanek, McCaul, & Sandgren, 2005). In another study, age was also found not to have a statistically significant correlation with the final decision making with regard to postmastectomy breast reconstruction (Fallbiork, Karlsson, Salander, & Rasmussen, 2010).
The results in this study reveal that, for postmastectomy breast reconstruction among Israeli women, patient age did not exhibit a correlation with type of decision-making style or with the declared level of involvement with the decision-making process. These results corroborate a previous and similar study on older women and breast cancer decision making conducted in Israel (Kadmon et al., 2012). In that study, however, all of the participants were aged older than 65 years, and the common decision-making style among that group was avoidance. This difference could be explained by the fact that, in Kadmon et al.’s (2012) study, the questions were hypothetical because all of the women who were questioned were awaiting a routine mammography examination. The women in the present study were already diagnosed with breast cancer. To further emphasize the lack of consistency among different nationalities, previous studies on this topic reveal significant differences in decision-making trends. A study conducted on older aged women in Australia and the United States regarding theoretical scenarios of a breast cancer diagnosis demonstrated a clear correlation between age and decision-making style (Budden et al., 2003; Pierce, 1993). In addition, other research has also shown statistically significant negative correlation between a patient’s increasing age and a decreasing level of likelihood to be involved in the decision-making process (Cox, Jenkins, Catt, Langride, & Fallowfield, 2006; Cyran, Crane, & Palmer, 2001; Gilligan, Kneusel, Hoffman, Greer, & Nattinger, 2002; Levinson et al., 2005; Mandelblatt, Kreling, Figeuriedo, & Feng, 2006). However, other research found that younger women expressed less involvement in the decision-making process than older women (Hawley et al., 2007).
The incidence of breast cancer increases with women’s age and, in Israel, the majority of breast cancer diagnoses are reported in women aged older than 50 years (Ministry of Health Israel, 2015). These women must cope with difficult medical decisions, including whether to undergo postmastectomy breast reconstruction. Healthcare providers must keep in mind that, of the women in Israel diagnosed with breast cancer, a considerable number, particularly those age older than 50 years, emigrated from countries with strong paternalistic health systems (e.g., northern Africa, former Soviet Union), and their openness and comfort with voicing their individual opinion may not have been as forthcoming as in younger women (Davidovitch et al., 2013). The current study shows that an overwhelming majority of participants who underwent postmastectomy breast reconstruction stated they had been included, on some level, in the decision-making process, and 49% felt they had made the final decision with the physician. A more in-depth analysis of the women’s decision-making process with a survey of the provider’s assessment of how the decision is made would be necessary to truly investigate whether women are actively engaging in SDM.
From a study by Kadmon, Pierce, and Antonakos (2012) conducted in Israel on women with breast cancer and their decision-making behavior, it can be concluded that a correlation exists between the decision-making styles of the patients and their level of involvement in decision making. Decision-making styles and level of involvement in decision making have been studied in the past. Rather than thinking of them as two separate entities, they may simply constitute two tightly connected traits on a similar spectrum of character trait. The finding of a correlation between the two was measured and showed that women who exhibited detached decision-making styles preferred that the physician take the lead in the decision-making process. The authors also found that all women have some degree of desire for SDM. This is of crucial importance because it could be wrongly assumed that older adult women prefer to be less involved in the decision-making process.
Limitations
This study was conducted on a sample of patients in one large medical center and may not represent the broader Israeli society. The questionnaires were in Hebrew only, which is a limitation of its applicability to fluent Hebrew-speaking groups only and not those who have recently immigrated to the country with inadequate proficiency in the language. The study also asked for participation of women who had undergone surgery within the past five years, with women being an average of 2.2 years postsurgery. This could create a recall bias because the evaluation of the decision-making process was removed from the decision itself. This study only focused on the patient evaluation of the process and would have benefited from involving the opinions of the attending surgeon and breast care nurse specialist.
Implications for Nursing
This study contributes to the understanding of the decision-making process regarding breast reconstruction and serves to increase the body of knowledge on the subject, which assists oncology and surgery nurses. To ensure and facilitate the active participation of women in decision making (Romanek et al., 2005), the nurse must provide patients with information according to preferred decision-making style, possibly with less emphasis on other factors, such as age, marital status, economic status, and education. Nurse educators may teach nurses to identify the decision-making needs of the patient and to create an intervention plan aimed toward improving the quality of the relationship between the patient, the physician, and the nurse while encouraging patient involvement in decision making.
A collaborative decision-making process is favored by patients during treatment, particularly when different treatment options are present or uncertainty about the results exist. The positive relationship between collaborative decision-making process and the quality of life and psychosocial status continues to be strengthened in research (Levinson et al., 2005; Mandelblatt et al., 2006).
The desired goal is that the nurse or physician will offer the patient the opportunity to participate and actively encourage the patient during the process. However, to achieve this goal, the healthcare professional must request information about the patient’s preferences and avoid assumptions about desire for involvement based solely on sociodemographic variables.
Although attitudes that support collaborative decision making have demonstrated a range of health and wellness benefits (Légaré et al., 2014), many barriers exist with this approach. Barriers to implementation include time pressure, unwillingness to share power, difficulty in expressing uncertainty, and difficulty in dealing with contradictory information sources (Edwards et al., 2004). Healthcare providers need to establish evidence-based guidelines in this area and create protocols for assessing patient preferences for treatment decision making and implementing SDM where appropriate.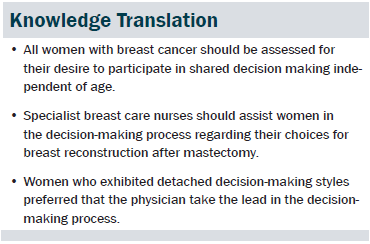
Conclusion
Regardless of age, it appears that, when faced with the decision of breast reconstruction after unilateral or bilateral mastectomy, Israeli women exhibit a desire for SDM with their physicians. In addition, the research findings show that patient age does not affect the pattern of behavior and the degree of involvement in the decision-making process regarding breast reconstruction. Some of the patterns of behavior are influenced by the behavior of the physician, indicating that physicians had a great impact on patient behavior.
The information from this study may help health-care providers gain insight into the lack of influence of age influencing decision making in women considering breast reconstruction and will hopefully serve as a solid foundation for additional studies focused on SDM in the field of reconstructive oncology.
References
Barnea, Y. (2014). [Plastic surgery in breast cancer.] Bama: The Journal for Health Professionals on Cancer and Its Consequences, 20, 74–76.
Beaver, K., Craven, O., Witham, G., Tomlinson, M., Susnerwala, S., Jones, D., & Luker, K.A. (2007). Patient participation in decision making: Views of health professionals caring for people with colorectal cancer. Journal of Clinical Nursing, 16, 725–733.
Bleicher, R.J., Abrahamse, P., Hawley, S.T., Katz, S.J., & Morrow, M. (2008). The influence of age on the breast surgery decision-making process. Annals of Surgical Oncology, 15, 854–862.
Budden, L.M., Pierce, P.F., Hayes, B.A., & Buettner, P.G. (2003). Australian women’s prediagnostic decision-making styles, relating to treatment choice for early breast cancer treatment. Research and Theory for Nursing Practice, 17, 117–136.
Butow, P., Harrison, J.D., & Choy, E.T. (2007). Health professional and consumer views on involving breast cancer patients in the multidisciplinary discussion of their disease and treatment plan. Cancer, 110, 1937–1944.
Charles, C., Gafni, A., & Whelan, T. (1999). Decision making in the physician patient encounter: Revisiting the shared treatment decision making model. Social Science and Medicine, 49, 651–661.
Cordeiro, P. (2008). Breast reconstruction after surgery for breast cancer. New England Journal of Medicine, 359, 1590–1601.
Cox, A., Jenkins, V., Catt, S., Langride, C., & Fallowfield, L. (2006). Information needs and experiences: An audit of UK cancer patients. European Journal of Oncology Nursing, 10, 263–272.
Cyran, E.M., Crane, L.A., & Palmer L. (2001). Physician sex and other factors associated with type of breast cancer surgery in older women. Archives of Surgery, 136, 185–191.
Davidovitch, N., Filc, D., Novack, L., & Balicer, R.D. (2013). Immigrating to a universal health care system: Utilization of hospital services by immigrants in Israel. Health and Place, 20, 13–28. doi:10.1016/j.healthplace.2012.11.005
Edwards, A., Elwyn, G., Hood, K., Atwell, C., Robling, M., Houston, H., . . . Russell, I. (2004). Patient-based outcome results from a cluster randomized trial of shared decision making skill development and use of risk communication aids in general practice. Family Practice, 21, 347–354. doi:10.1093/fampra/cmh402
El-Wakeel, H., Taylor, G.J., & Tate, J.J. (2006). What do patients really want to know in an informed consent procedure? A questionnaire-based survey of patients in the Bath area, UK. Journal of Medical Ethics, 32, 612–616.
Elwyn, G., Hutchings, H., & Edwards, A. (2005). The OPTION scale: Measuring the extent that clinicians involve patient in decision making tasks. Health Expectations, 8, 34–42.
Fallbiork, U., Karlsson, S., Salander, P., & Rasmussen, B.H. (2010). Differences between women who have and have not undergone breast reconstruction after mastectomy due to breast cancer. Acta Oncolologica, 49, 174–179.
Gilligan, M.A., Kneusel, R.T., Hoffman, R.G., Greer, A.L., & Nattinger, A.B. (2002). Persistent differences in socio demographic determinants of breast conservation treatment despite overall increased adoption. Medical Care, 40, 181–189.
Hawley, S.T., Lantz, P.M., & Janz, N.K. (2007). Factors associated with patient involvement in surgical treatment decision making for breast cancer. Patient Education and Counseling, 65, 387–395.
Hinkle, J.L., & Cheever, K.H. (2013). Brunner and Suddarth’s textbook of medical-surgical nursing (13th ed.). Riverwoods, IL: Lippincott, Williams and Williams. 1691–1710.
Israel Central Bureau of Statistics. (2014). Annual census. Retrieved from http://www.cbs.gov.il/reader/cw_usr_view_SHTML?ID=802
Janis, I.L., & Mann, L. (1977). Decision making: A psychological analysis of conflict, choice, and commitment. New York, NY: Free Press.
Kadmon, I., Pierce, P., & Antonakos, C. (2012). Elder women’s decision-making in breast cancer care. European Journal of Oncology Nursing, 16, 233–237.
Kleeberg, U.R., Feyer, P., Günther, W., & Behrens, M. (2008). Patient satisfaction in outpatient cancer care: A prospective survey using the PASQOC® questionnaire. Supportive Care in Cancer, 16, 947–954.
Lee, B.T., Chen, C., Yueh, J., Nguyen, M.D., Lin, S., & Tobias, A.M. (2010). Computer-based learning module increases shared decision making in breast reconstruction. Annals of Surgical Oncology, 17, 738–743.
Lee, C.N., Hultman, C.S., & Sepucha, K. (2010). Do patient and providers agree about the most important facts and goals for breast reconstruction decision? Annals of Plastic Surgery, 64, 563–566.
Légaré F., Stacey, D., Turcotte, S., Cossi, M.J., Kryworuchko, J., Graham, I.D., . . . Donner-Banzhoff, N. (2014). Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database of Systematic Reviews, 9, CD006732.
Levinson, W., Kao, A., Kuby, A., & Thisted, R.A. (2005). Not all patients want to participate in decision making: A national study of public preferences. Journal of General Internal Medicine, 20, 531–535.
Malhi, A., & Abromovsky, M. (2014). Combining the home, family and work among Haredi Women. Jerusalem, Israel: Ministry of the Economy.
Mandelblatt, J., Kreling, B., Figeuriedo, M., & Feng, S. (2006). What is the impact of shared decision making on treatment and outcomes for older women with breast cancer? Journal of Clinical Ostyncology, 24, 4908–4913.
Ministry of Health Israel. (2015). Cancer registry. Retrieved from http://www.health.gov.il/UnitsOffice/HD/ICDC/ICR/Pages/default.aspx
Miron-Shatz, T., Golan, O., Brezis, M., Siegal, G., & Doniger, G.M. (2012). Shared decision making in Israel: Status, barriers, and recommendations. Israel Journal of Health Policy Research, 1, 1–8.
Pierce, P. (1995). Michigan Assessment of Decision Style (MADS). Ann Arbor, MI: University of Michigan.
Pierce, P.F. (1993). Deciding on breast cancer treatment: A description of decision behavior. Nursing Research, 42, 22–28.
Popejoy, L. (2005). Health related decision making by older adult and their families: How clinicians help. Journal of Gerontological Nursing, 31(9), 12–18.
Reddy, S., Colakoglu, S., Curtis, M.S., Yueh, J.H., Ogunleye, A., Tobias, A.M., & Lee, B.T. (2011). Breast cancer recurrence following post mastectomy reconstruction compared to mastectomy with no reconstruction. Annals of Plastic Surgery, 66, 466–471.
Romanek, K.M., McCaul, K.D., & Sandgren, A.K. (2005). Age differences in treatment decision making for breast cancer in a sample of healthy women: The effect of body image and risk framing. Oncology Nursing Forum, 32, 799–806.
Visser, A., & Winslow, L. (2003). From patient education to communication health care. Editorial Patient Education and Counseling, 5, 227–228.
Vogel, B.A., Helmes, A.W., & Hasenburg, A. (2008). Concordance between patients’ desired and actual decision making roles in breast cancer care. Psycho-Oncology, 17, 182–189.
About the Author(s)
Kadmon is a senior lecturer and a nurse specialist in breast cancer care in the Hadassah School of Nursing at Hebrew University; and Noy is a registered nurse in the Plastic Surgery Department, Billig is a resident, and Tzur is an attending plastic surgeon, all at the Hadassah Medical Center, all in Jerusalem, Israel. No financial relationships to disclose. Kadmon and Noy contributed to the conceptualization and design and analysis. Noy completed the data collection. Tzur and Billig contributed to the manuscript preparation. Kadmon can be reached at ikadmon@hadassah.org.il, with copy to editor at ONFEditor@ons.org. Submitted May 2015. Accepted for publication June 7, 2015.

