Testicular Cancer Awareness and Screening Practices: A Systematic Review
Purpose/Objectives: To critically appraise empirical evidence gathered from studies that (a) explored men’s knowledge, awareness, and attitudes toward testicular cancer (TC) and its screening; (b) addressed their testicular self-examination (TSE) practice; and/or (c) highlighted barriers and facilitators to this practice.
Data Sources: MEDLINE®, CINAHL®, and EMBASE®.
Data Synthesis: 25 articles met the inclusion criteria. Knowledge deficits regarding TC and its screening were seen. Participants who did not perform TSE often were uninformed about this practice. The majority of men perceived TC education as a positive step toward raising awareness about this malignancy.
Conclusions: Very few men were informed about TC and TSE. Future studies should include valid and reliable tools to assess TC knowledge and screening, address the means through which TC knowledge is delivered, explore the individual’s experience with TC screening, and focus on TC awareness and screening among minority groups.
Implications for Nursing: Although regular screening for TC is a controversial issue, nurses should encourage young men to seek medical attention in the event of discovering scrotal abnormalities.
Jump to a section
Testicular cancer (TC) is a rare malignancy that constitutes 0.5% of all new cancer cases and 0.1% of all cancer deaths in the United States. About 1 in every 263 men will develop TC in their lifetime and 8,430 men will be diagnosed with TC in 2015 (National Cancer Institute, 2014a). Men aged 20–34 years are at the highest risk for TC, with a median age of 33 years at diagnosis. However, in the United States, TC has one of the highest cure rates, with a five-year survival rate of 95% (National Cancer Institute, 2014a).
TC screening in asymptomatic males continues to be a controversial issue because of a lack of empirical evidence that supports or discourages the practice (Law, 2004; National Cancer Institute, 2014b). The U.S. Preventive Services Task Force ([USPSTF], 2011) issued a statement against TC screening among asymptomatic males. This statement was based on a Cochrane review conducted by Ilic and Misso (2011) in which no evidence was found regarding the beneficial effect of TC screening on mortality. In addition, it was suggested that TC screening may cause unnecessary anxiety and increase the likelihood of having false-positive findings that would consequently expose men to invasive diagnostic tests. However, key cancer organizations, such as the American Cancer Society ([ACS], 2014c), recommend TC screening as a component of routine cancer-related physical examinations. In the United Kingdom, men are encouraged to be aware of the normal anatomy of their testes (Cancer Research UK, 2014) despite having no evidence to support weekly or monthly testicular self-examination (TSE). Similarly, the Irish Cancer Society (2014) offers infographic material to encourage young men to perform TSE. In addition, a number of foundations have been established to raise awareness about TC and its screening. One of those organizations, the Testicular Cancer Awareness Foundation (2014), uses 89% of its funds to educate young men about the importance of periodically practicing TSE.
Studies that have assessed TC knowledge and TC screening practices among healthy men have been conducted; however, no systematic reviews have been conducted to pool findings from these studies to inform practice. The aim of this review was to critically appraise evidence gathered from studies that explored men’s knowledge, awareness, and attitudes toward TC and its screening; addressed their TSE practice; and/or highlighted barriers and facilitators to this practice.
Methods
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) checklist was used in this review (Moher, Liberati, Tetzlaff, & Altman, 2009). Studies included in this systematic review are quantitative or qualitative; published in or translated to English; published from 2004–2014; included findings from men only; assessed knowledge, awareness, and attitudes toward TC; assessed knowledge, awareness, attitudes, and practice of TC screening, including TSE; and examined barriers and facilitators to TC knowledge and screening. The term TC screening was considered to comprise TC examination by a clinician and TSE.
Three electronic databases (MEDLINE®, CINAHL®, and EMBASE®) were searched. Boolean terms “OR” and “AND,” Medical Subject Headings (MeSH), and truncation “*” were used. Keywords and their synonyms were combined and yielded the following search history: (cancer* OR tumor* OR tumour* OR malignan* OR neoplas*) AND (testicul* OR testes OR testis OR testicle*) AND (self-exam* OR ‘self exam*’ OR screening OR ‘early detection’ OR awareness OR knowledge OR attitudes OR practice OR ‘health promotion’ OR symptoms).
Studies were exported to EndNode® X7 and duplicates were deleted. Records were screened on title and abstract and irrelevant articles were excluded. Data from the included studies were extracted by the primary reviewer (MS) using a standardized research matrix (Gooseens et al., 2014) and later cross-checked by another reviewer (JH). Data collected included name of the author(s), year of publication, and country and setting where the studies were conducted. Demographic data of the study population (sample size, mean age, and age range) were extracted along with the study design and instruments. The search results were independently reviewed by two authors (MS and ML), and a kappa coefficient was calculated.
A total of 3,076 records were identified through database search. Following the deletion of duplicates, 1,731 articles were independently screened on title and abstract by two reviewers (MS and ML) and irrelevant articles were excluded. A Cohen’s kappa coefficient of 0.715 was obtained and was perceived as satisfactory (Higgins & Green, 2011). The authors assessed 126 full-text articles for eligibility. Following the exclusion of 101 articles, 21 quantitative cross-sectional surveys, 3 qualitative descriptive studies, and 1 integrative review were deemed eligible for review. Figure 1 summarizes the study selection process.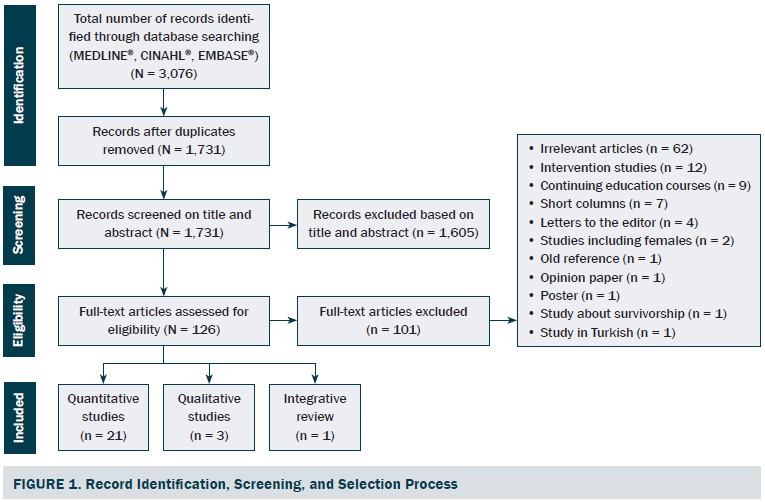
Results
Study Characteristics
The majority of the reviewed studies were conducted in the United States (n = 7). Because TC is most common among young adults, the majority of data was collected in universities (n = 13). The smallest sample size in quantitative studies was 177 (Beydag, 2012) and the largest sample size was 8,680 (Evans, Steptoe, & Wardle, 2006). As for qualitative studies, the minimum sample size was 20 (Dubé, Fuller, Rosen, Fagan, & O’Donnell, 2005) and the maximum was 37 (Evans, Simon, & Wardle, 2010). Non-probability purposive sampling was used in all of the reviewed qualitative studies as well as the majority of the quantitative studies (n = 19). Random sampling was used in only two quantitative studies (Muliira, Nalwanga, Muliira, & Nankinga, 2013; Powe, Ross, Wilkerson, Brooks, & Cooper, 2007). Ages of participants ranged from 14–78 years. With the exception of one integrative review (de Souza, dos Reis, Gomes, & de Carvalho, 2011), all included records used a descriptive approach.
Quality Appraisal of Included Studies
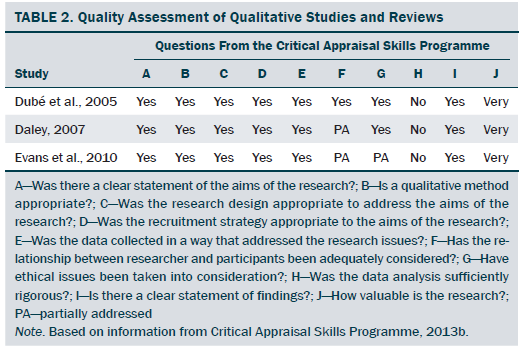
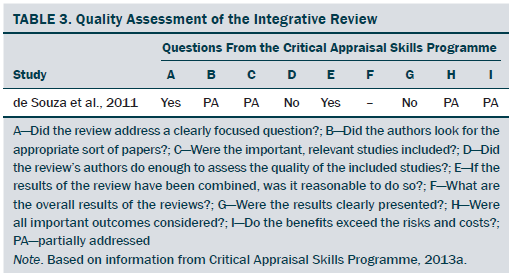
Three tools were used to assess the quality of the included studies. A quality-appraisal tool was used to assess the quality of the quantitative studies (Davids & Roman, 2014; Louw, Morris, & Grimmer-Somers, 2007; Roman & Frantz, 2013; Wong, Cheung, & Hart, 2008). Studies that scored from 0%–33.9% were considered weak (n = 3), 34%–66.9% were considered moderate (n = 9), and 67%–100% were interpreted as strong (n = 9). The quality of the qualitative studies and the integrative review was assessed using two tools developed by the Critical Appraisal Skills Programme (2013a, 2013b). Quality appraisal of the included literature is presented in Tables 1–3.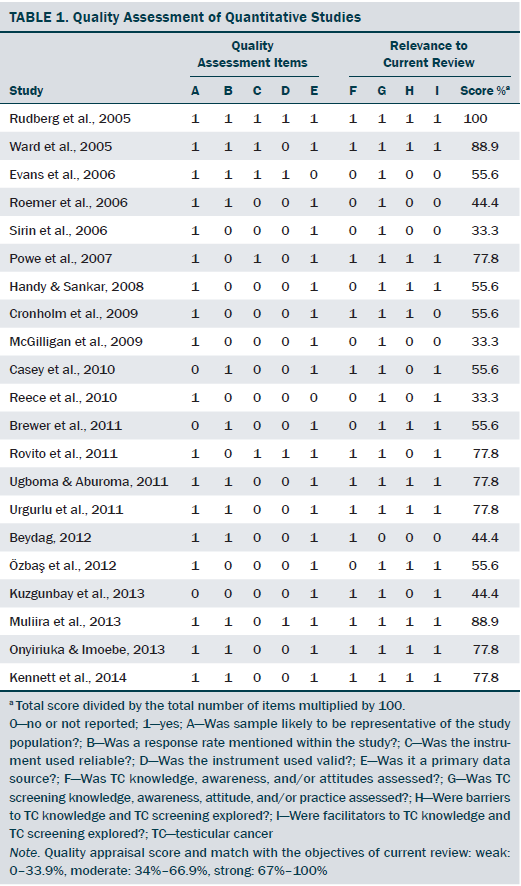
Discussion
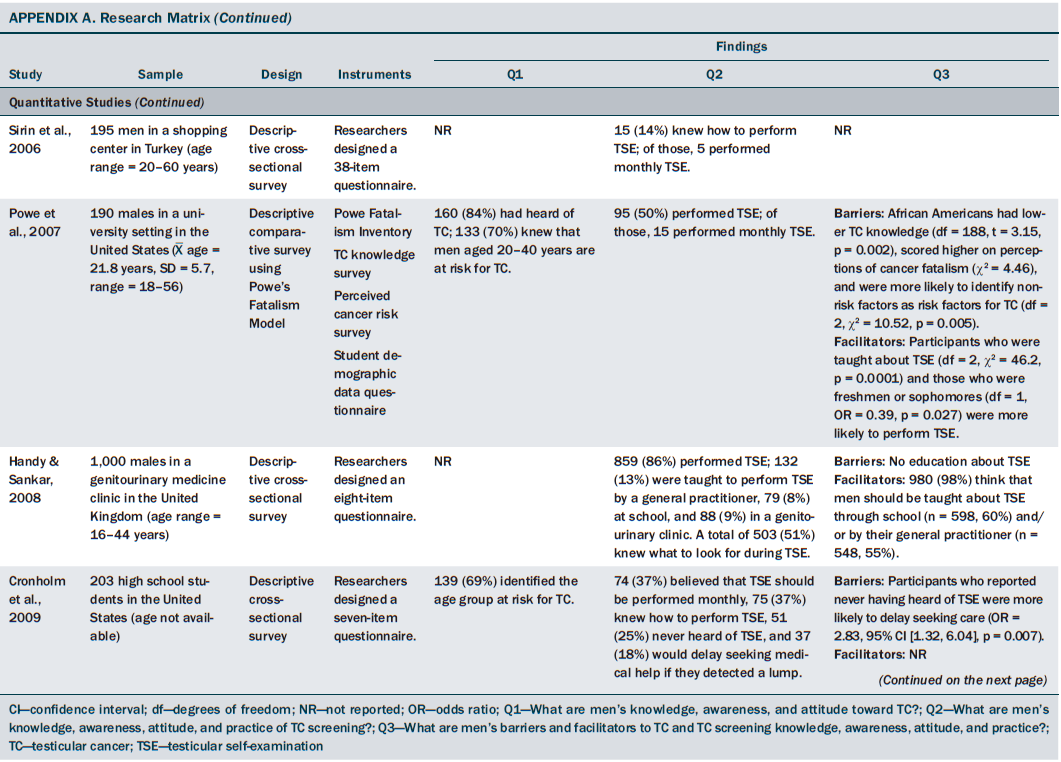
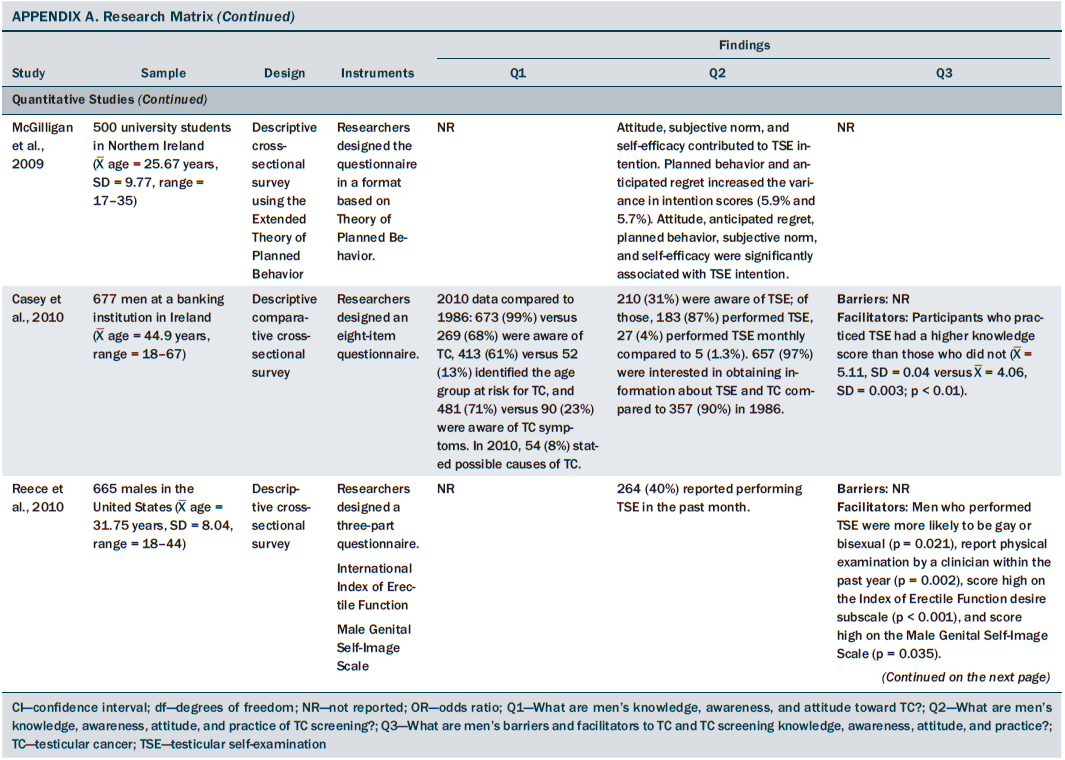
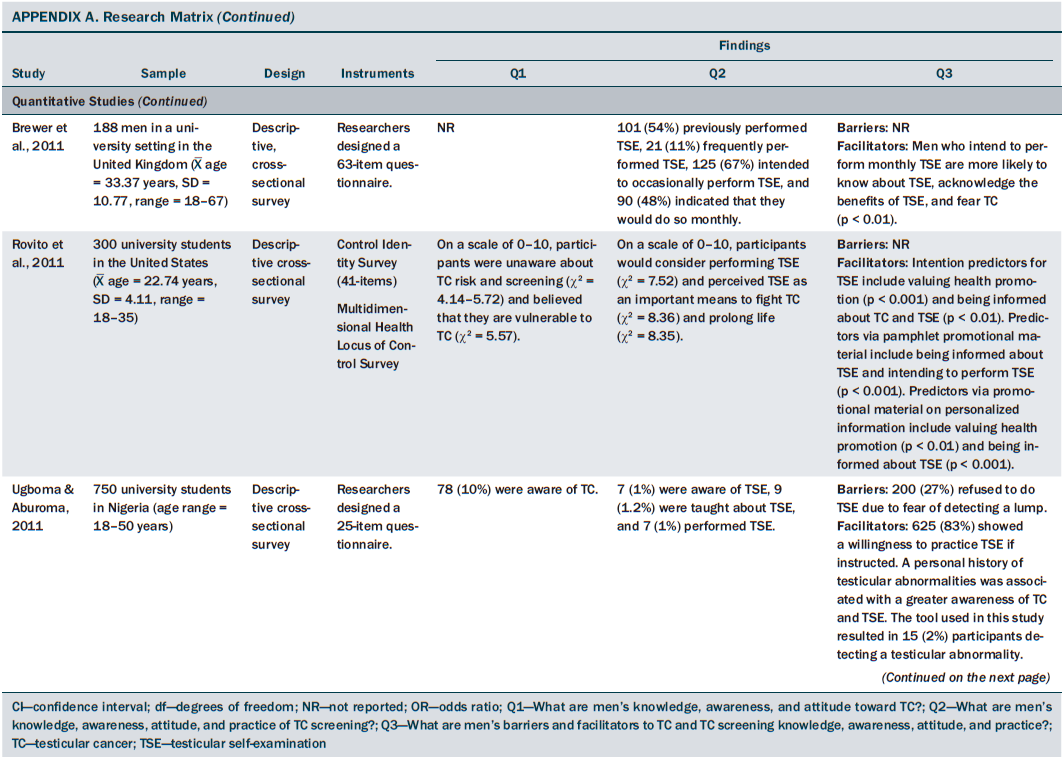
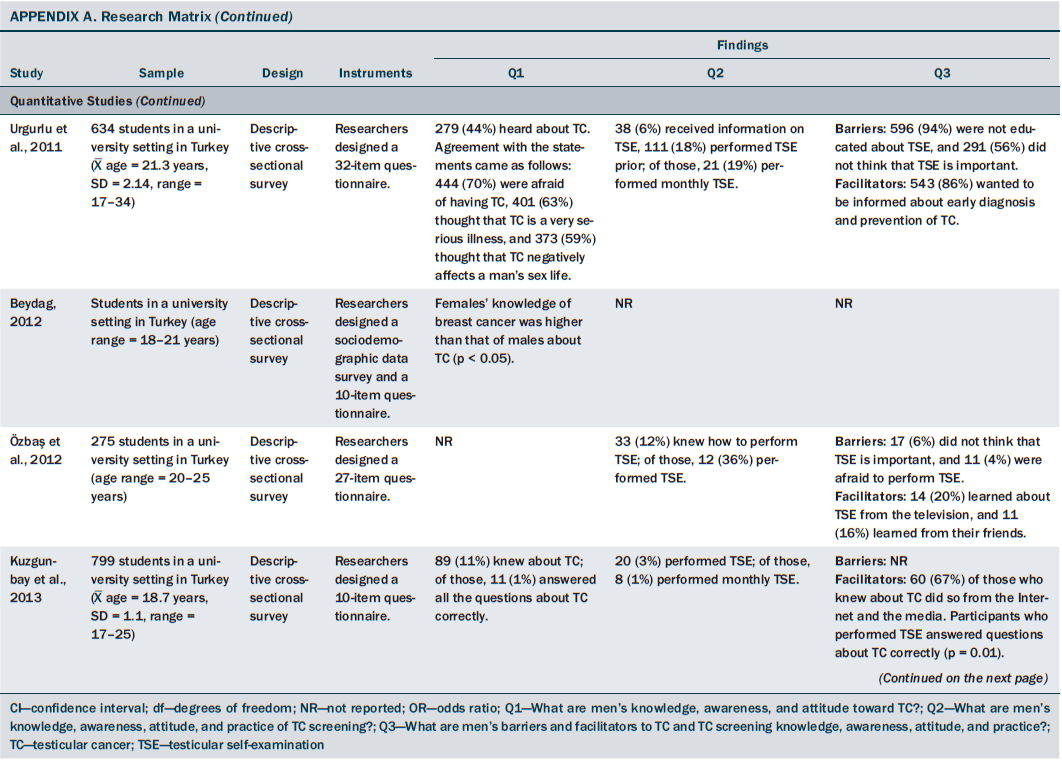
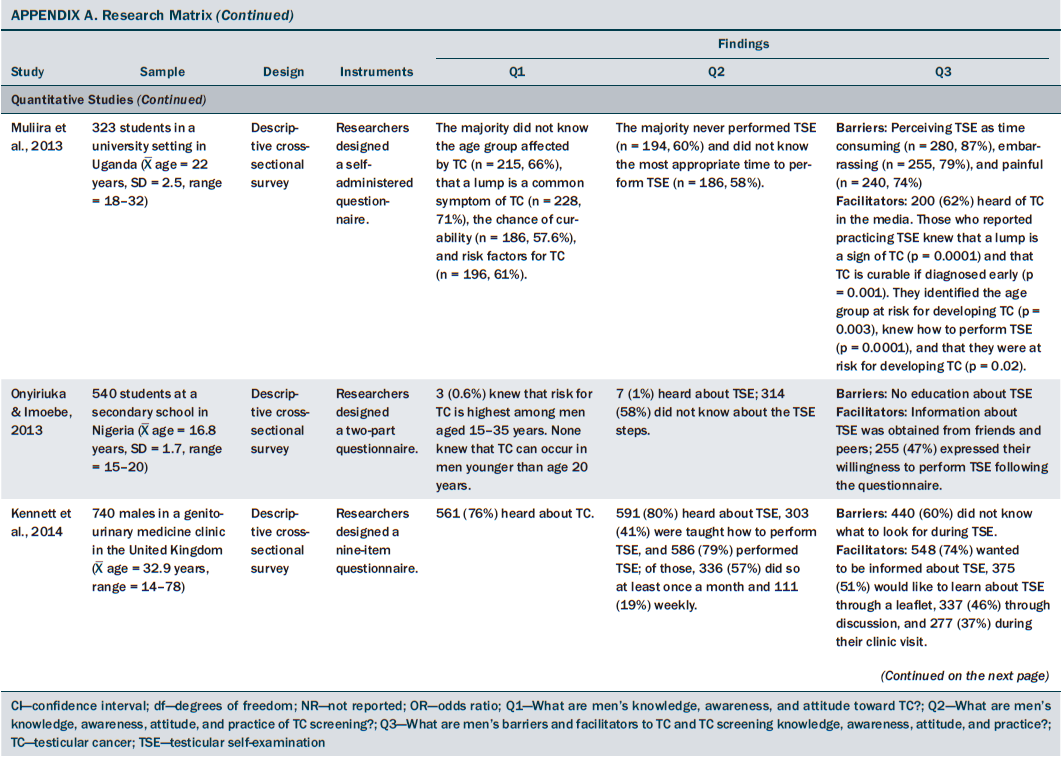
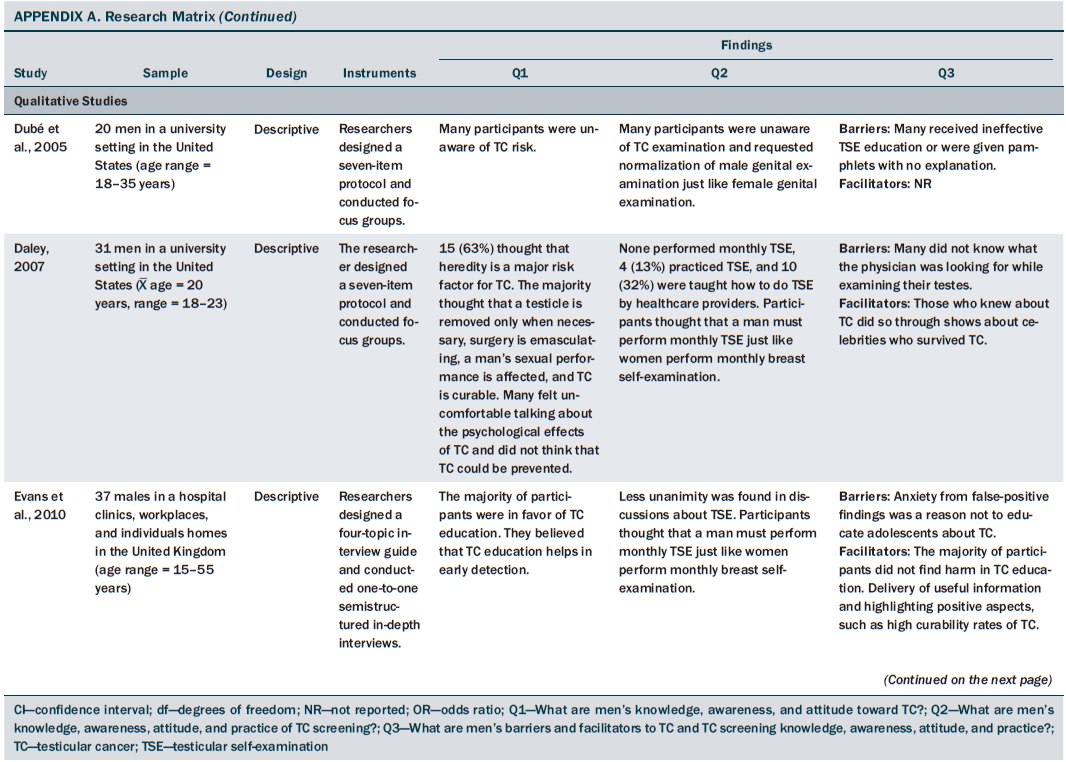
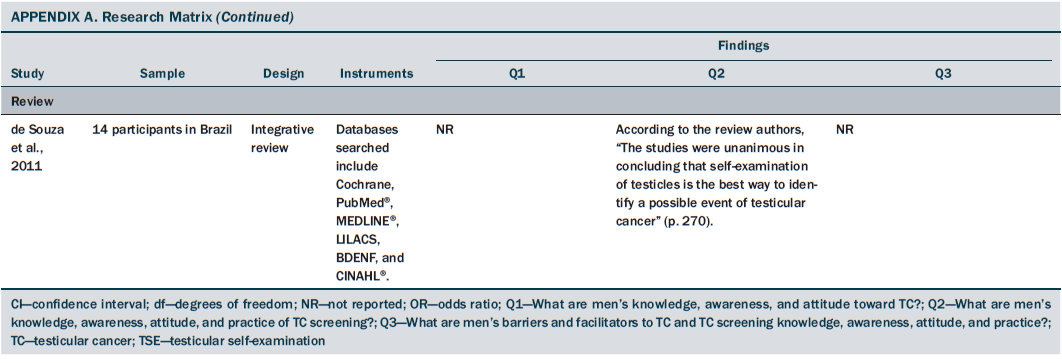
Researchers used a multitude of questionnaires to collect data, with the majority being researcher designed surveys (n = 18). Therefore, given the heterogeneous nature of the data collected, it was not feasible to combine the data for a meta-analysis. Findings from individual studies are presented in Appendix A.
Knowledge, Awareness, and Attitudes Toward Testicular Cancer
Having heard of TC did not equate to knowledge about the various aspects of this malignancy, such as its risk factors, signs and symptoms, and treatment modalities. Evidence shows that men’s knowledge of TC increased over time. This increase in knowledge, however, was not found in studies conducted in developing countries. This trend may be attributable to the lack of public awareness and education about TC and its symptoms in the developing world (Kuzgunbay et al., 2013; Muliira et al., 2013; Ugboma & Aburoma, 2011).
While exploring the different attitudes toward TC, fear was found to be the most commonly reported feeling. Participants perceived TC as a serious illness, believed that they were at risk for TC, and were afraid of developing it. These participants were more likely to be unaware that TC is curable and believed that TC is not preventable. These perceptions may stem from the general views of cancer. Cancer diagnosis in general and TC in particular has long been associated with fear (Saab, Noureddine, Huijer, & DeJong, 2014; Skaali et al., 2009).
Of the risk factors for TC, age was addressed the most. A difference exists between the knowledge of TC risk factors among men living in developed countries (Casey, Grainger, Butler, McDermott, & Thornhill, 2010; Cronholm, Mao, Nguyen, & Paris, 2009; Daley, 2007; Powe et al., 2007) and that of men living in developing countries (Muliira et al., 2013; Onyiriuka & Imoebe, 2013). Again, this can be attributed to the lack of public awareness and education about TC in the developing world.
Knowledge, Awareness, Attitudes, and Practice of Testicular Self-Examination
A certain degree of knowledge deficit regarding TC screening was noted. Like TC awareness, having heard of TC screening did not equate to practicing TSE or undergoing TC screening by a clinician. Of those who claimed to have heard of TSE, very few knew what to look for while checking their testes. Like TC knowledge, the lowest TSE knowledge scores were noted among men living in developing countries, which was attributed to the lack of public awareness about health surveillance, insufficient health education in schools and universities, and the lack of endorsement of TC practices by policymakers.
Almost all men in the reviewed studies showed a positive attitude toward TC screening. As for help-seeking behaviors, very few stated that they would delay seeking medical attention in the event of a painless testicular lump. Delay in seeking medical care was strongly associated with not knowing about and/or not practicing TSE, as well as fear from contracting TC. Attitudes toward TC screening were thought to be shaped by cultural norms, health education, and the media. In addition, of the small amount of men who reported performing TSE, few did so regularly.
Barriers to Awareness and Screening
Evidence suggests that participants who did not perform TSE often were uninformed about this practice. Ambiguity of messages delivered by healthcare providers and men’s negative attitudes toward TC and TSE served as barriers to TC screening. The evidence suggests that fear of detecting a lump and anxiety from false-positive results played a key role in the participants’ refusal to perform TSE. In addition, those who perceived TSE as unimportant, time consuming, embarrassing, and/or painful were more likely to refrain from performing it. Of note, misconceptions about TC screening were predominant in developing countries and stemmed from the preexisting knowledge deficit about TC and its screening.
The lowest TC knowledge scores and TC screening practices were noted in studies conducted in developing countries. Conceivably, education could have affected their scores. However, the majority of participants in these studies were university students, including medical students (Kuzgunbay et al., 2013). Of note, the risk of developing TC is highest in the United States and Europe and lowest in Africa and Asia (ACS, 2014b). This could be another reason why efforts were not made to increase TC awareness and TC screening practices in developing countries.
Participants’ ethnic backgrounds also were found to influence TC knowledge and TC screening practices. In the United States, African American men scored the lowest on questions about TC and TSE. Despite the fact that the incidence of TC is higher among Caucasians, African Americans are more likely to have advanced TC at time of diagnosis (ACS, 2014c). To date, no clear explanation exists for this trend; however, a number of factors could have contributed to these findings. For instance, African Americans often learn about TC and TSE through healthcare providers and schools. African Americans are, as a group, less likely than Caucasians to visit physicians on a regular basis (Powe et al., 2007). African Americans also generally have a lower socioeconomic status, which often is associated with lower screening rates, advanced stage of disease at diagnosis, and decreased survival rates (ACS, 2014a).
Facilitators to Awareness and Screening
The evidence suggests that men who were educated about TC and TSE were more likely to undergo TC screening. In the majority of the reviewed studies, mass media served as the means through which knowledge about TC and TC screening was conveyed. Despite its numerous detrimental effects, such as exposure to violent content and harmful lifestyle habits, the evidence suggests that mass media can play a key role in providing information about safe health practices (Strasburger, Jordan, & Donnerstein, 2012).
The majority of participants believed that TC education is a positive step toward raising awareness about TC and increasing TC screening practices. They displayed interest in obtaining information about TSE, showed willingness to practice TSE, and thought that men should be taught about TC. Participants also believed that no harm could come from TC education and suggested that delivering useful information and highlighting the TC high curability rate can help overcome cancer-related anxiety (Evans et al., 2010). They also believed that men should be encouraged to perform TSE the same way women are encouraged to perform breast self-examination and assumed that the normalization of TSE would lead to increased TC screening practices (Dubé et al., 2005; Evans et al., 2010).
Limitations
During the review process, a number of methodologic limitations were noted. Using the American Association of Critical Care Nurses’ hierarchy of evidence, all the reviewed papers fall under the level of evidence C (Armola et al., 2009). Focus groups rather than individual interviews were conducted in all three qualitative studies; therefore, some participants may not have been forthcoming in their answers, which could have led to omission of important details. In addition, no meta-analyses or meta-syntheses were identified during the literature search. Of note, a multitude of researcher-designed questionnaires were used in the majority of the reviewed survey studies, which has led to heterogeneous results that could not be combined for a meta-analysis. In addition, the majority of these studies did not report on reliability and validity. Almost all the reviewed studies used non-probability purposive sampling, which is known to increase the risk of selection bias and yield a sample that is less likely to be representative of the target population (Cochrane Bias Methods Group, 2013). Finally, the majority of participants were Caucasian university students. Data from ethnic, sexuality, and gender, as well as religious minorities and people with disabilities was not sought, which hinders the generalizability and transferability of the findings.
The search was limited to three databases and did not include data from the grey literature. In addition, the search was limited to studies conducted from 2004 to 2014 and studies that were published in or translated to English, which leaves room for study selection bias. Reporting bias may have taken place since only findings pertinent to the review aims are presented (Cochrane Bias Methods Group, 2013). Finally, some descriptive statistics were calculated using data from the publications, which leaves room for error. Minimizing the risk for this error was attempted by having a second reviewer (JH) cross-check the extracted data.
Implications for Future Research
Future research on TC and TC screening is needed to close the gap in the literature and address the identified limitations. The use of standardized, valid, and reliable tools should be encouraged to allow the replication of studies in different contexts. In addition, the use of random sampling should be encouraged to minimize the risk of selection bias and yield a representative sample.
Despite assessing men’s knowledge of TC and TSE, very few studies addressed the means through which this knowledge is delivered. For this reason, future research should focus on assessing men’s information needs and exploring the preferred means through which they wish to acquire new knowledge. From a qualitative perspective, a need exists to explore the individual man’s experience with TC screening and to offer an in-depth interpretation of the psychosocial constituents of this experience.
Research on cancer prevention in minority groups is among the top priorities of key oncology organizations, such as the Oncology Nursing Society (Wood et al., 2014). For this reason, future studies should be targeted toward assessing TC knowledge and screening practices as well as exploring the experiences minority groups.
Finally, given that the majority of existing data was collected from universities, future studies that focus on TC knowledge and screening in men with low educational and/or socioeconomic background should be considered.
Implications for Nursing
The controversy and lack of consensus regarding TC screening might instill a sense of ambiguity amongst healthcare providers and educators. A middle ground could be reached by informing nurses who are involved in health promotion to encourage young men to seek medical attention in the event of scrotal abnormalities, such as pain or the presence of a testicular lump or swelling.
[[{"type":"media","view_mode":"media_original","fid":"20686","attributes":{"alt":"","class":"media-image","height":"239","typeof":"foaf:Image","width":"369"}}]]
Conclusions
A certain degree of knowledge deficit regarding TC and its screening exists. Generally, men perceived TC as a serious illness, were unaware that it is curable, and often were uninformed about TSE. In addition, not all who claimed having heard of TC screening knew what to look for during TSE. The majority of men perceived TC education as a positive step toward raising awareness about TC and TSE. Men who were educated about TC and TSE were more likely to undergo TC screening. Mass media served as the key means through which participants learned about TC and its screening.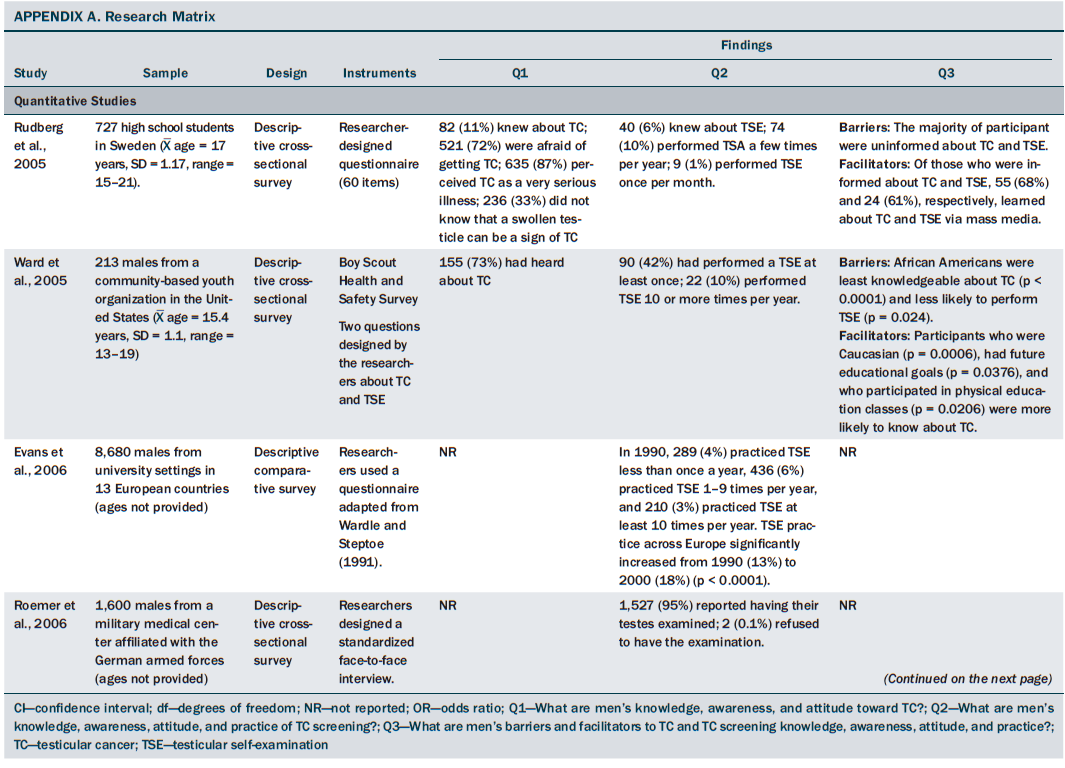
References
American Cancer Society. (2014a). Cancer facts and figures for African Americans. Retrieved from http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/docum…
American Cancer Society. (2014b). How is testicular cancer found? Retrieved from http://www.cancer.org/cancer/testicularcancer/overviewguide/testicular-…
American Cancer Society. (2014c). What are the risk factors for testicular cancer? Retrieved from http://www.cancer.org/cancer/testicularcancer/detailedguide/testicular-…
Armola, R.R., Bourgault, A.M., Halm, M.A., Board, R.M., Bucher, L., Harrington, L., . . . Medina, J. (2009). AACN levels of evidence: What’s new? Critical Care Nurse, 29(4), 70–73.
Beydag, K.D. (2012). Factors affecting the knowledge levels of a group of university students about the protection ways against breast and testicular cancer. HealthMED, 6, 3073–3079.
Brewer, G., Roy, M., & Watters, J. (2011). Testicular self-examination in an adult community sample. American Journal of Men’s Health, 5, 57–64.
Cancer Research UK. (2014). Finding testicular cancer early. Retrieved from http://www.cancerresearchuk.org/about-cancer/type/testicular-cancer/abo…
Casey, R.G., Grainger, R., Butler, M.R., McDermott, T.E., & Thornhill, J.A. (2010). Public awareness of testis cancer and the prevalence of testicular self-examination—Changing patterns over 20 years. Urology, 76, 915–918.
Cochrane Bias Methods Group. (2013). Assessing risk of bias in included studies. Retrieved from https://bmg.cochrane.org/assessing-risk-bias-included-studies
Critical Appraisal Skills Programme. (2013a). 10 questions to help you make sense of a review. Retrieved from http://media.wix.com/ugd/dded87_37491d0241aa448a8f3d4ae17c869472.pdf
Critical Appraisal Skills Programme. (2013b). 10 questions to help you make sense of qualitative research. Retrieved from http://media.wix.com/ugd/dded87_951541699e9edc71ce66c9bac4734c69.pdf
Cronholm, P.F., Mao, J.J., Nguyen, G.T., & Paris, R.T. (2009). A dilemma in male engagement in preventive services: Adolescent males’ knowledge and attitudes toward testicular cancer and testicular self-exam. American Journal of Men’s Health, 3, 134–140.
Daley, C.M. (2007). College men’s knowledge, attitudes, and beliefs about testicular cancer. American Journal of Men’s Health, 1, 173–182.
Davids, E.L., & Roman, N.V. (2014). A systematic review of the relationship between parenting styles and children’s physical activity. African Journal for Physical, Health Education, Recreation and Dance, 2, 228–246.
de Souza, K.W., dos Reis, P.E.D., Gomes, I.P., & de Carvalho, E.C. (2011). Prevention strategies for testicular cancer and penile cancer: An integrative review. Revista da Escola Enfermagem da USP, 45, 270–275.
Dubé, C.E., Fuller, B.K., Rosen, R.K., Fagan, M., & O’Donnell, J. (2005). Men’s experiences of physical exams and cancer screening tests: A qualitative study. Preventive Medicine, 40, 628–635.
Evans, R.E.C., Simon, A.E., & Wardle, J. (2010). Public perceptions of the harms and benefits of testicular cancer education: A qualitative study. Cancer Epidemiology, 34, 212–219.
Evans, R.E.C., Steptoe, A., & Wardle, J. (2006). Testicular self-examination: change in rates of practice in European university students, from 13 countries, over a 10-year period. Journal of Men’s Health and Gender, 3, 368–372.
Gooseens, J., Delbaere, I., Van Lancker, A., Beeckman, D., Verhaeghe, S., & Van Hecke, A. (2014). Cancer patients’ and professional caregivers’ needs, preferences and factors associated with receiving and providing fertility-related information: A mixed-methods systematic review. International Journal of Nursing Studies, 51, 300–319.
Handy, P., & Sankar, K.N. (2008). Testicular self-examination—Knowledge of men attending a large genito urinary medicine clinic. Health Education Journal, 67, 9–15.
Higgins, J.P.T., & Green, S. (2011). Cochrane handbook for systematic reviews of interventions. Retrieved from http://community.cochrane.org/handbook
Ilic, D., & Misso, M.L. (2011). Screening for testicular cancer [Review]. Cochrane Collaboration. New York, NY: John Wiley and Sons.
Irish Cancer Society. (2014). How to check your testicles. Retrieved from http://www.cancer.ie/cancer-information/testicular-cancer/how-to-check-…
Kennett, A., Shaw, J.W., & Woolley, P.D. (2014). Testicular self-examination amongst genitourinary medicine clinic attendees. International Journal of STD and AIDS, 25, 844–850.
Kuzgunbay, B., Yaycioglu, O., Soyunpak, B., Kayis, A.A., Ayan, S., Yavascaoglu, C., & Beduk, Y. (2013). Public awareness of testicular cancer and self-examination in Turkey: A multicenter study of Turkish urology society. Urologic Oncology: Seminars and Original Investigations, 31, 386–391.
Law, M. (2004). Screening without evidence of efficiency. BMJ, 328, 301–302.
Louw, Q.A., Morris, L.D., & Grimmer-Somers, K. (2007). The prevalence of low back pain in Africa: A systematic review. BMC Musculoskeletal Disorders, 8, 105.
McGilligan, C., McClenahan, C., & Adamson, G. (2009). Attitudes and intentions to performing testicular self-examination: Utilizing an extended theory of planned behavior. Journal of Adolescent Health, 44, 404–406.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D.G. (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. Annals of Internal Medicine, 151, 264–269.
Muliira, J.K., Nalwanga, P.B., Muliira, R.S., & Nankinga, Z. (2013). Knowledge, perceived risk and barriers to testicular self-examination among male university students in Uganda. Journal of Men’s Health, 9, 36–44.
National Cancer Institute. (2014a). Surveillance epidemiology and end results: SEER stat fact sheets: Testis. Retrieved from http://seer.cancer.gov/statfacts/html/testis.html
National Cancer Institute. (2014b). Testicular cancer screening. Retrieved from http://www.cancer.gov/cancertopics/pdq/screening/testicular/HealthProfe…
Onyiriuka, A.N., & Imoebe, F.E. (2013). Testicular self-examination among Nigerian adolescent secondary school boys: Knowledge, attitudes and practices. Journal of Preventive Medicine and Hygiene, 54, 163–166.
Özbas, A., Çavdar, I., Findik, Ü.Y., & Akyüz N. (2012). Inadequate knowledge levels of Turkish male university students about testicular self-examination. Asian Pacific Journal of Cancer Prevention, 12, 919–922.
Powe, B.D., Ross, L., Wilkerson, D., Brooks, P., & Cooper, D. (2007). Testicular cancer among African American college men: Knowledge, perceived risk, and perceptions of cancer fatalism. American Journal of Men’s Health, 1, 73–80.
Reece, M., Herbenick, D., Sanders, S.A., Dodge, B., Ghassemi, A., & Fortenberry, J.D. (2010). Prevalence and predictors of testicular self-exam among a nationally representative sample of men in the United States. International Journal of Sexual Health, 22, 1–4.
Roemer, H.C., von Kathen, M., Schöps, W., & Golka, K. (2006). Palpation of the testes in draftees: Acceptance of the occasion of muster and implication for health promotion. International Journal of Occupational Medicine and Environmental Health, 19, 254-259.
Roman, N.V., & Frantz, J.M. (2013). The prevalence of intimate partner violence in the family: A systematic review of the implications for adolescents in Africa. Family Practice, 30, 256–266.
Rovito, M.J., Gordon, T.F., Bauerle, B., & DuCette, J. (2011). Perceptions of testicular cancer and testicular self-examination among college men: A report on intention, vulnerability, and promotional material preferences. American Journal of Men’s Health, 5, 500–507.
Rudberg, L., Nilsson, S., Wikblad, K., & Carlsson, M. (2005). Testicular cancer and testicular self-examination: Knowledge and attitudes of adolescent Swedish men. Cancer Nursing, 28, 256–262.
Saab, M., Noureddine, S., Huijer, H.A.S., & DeJong, J. (2014). Surviving testicular cancer: The Lebanese lived experience. Nursing Research, 63, 203–209.
Sirin, A., Atan, S.U., & Tasci, E. (2006). Protection from cancer and early diagnosis applications in Izmir, Turkey. A pilot study. Cancer Nursing, 29, 207–213.
Skaali, T., Fosså, S.D., Bremnes, R., Dahl, O., Haaland, C.F., Hauge, E.R., . . . Dahl, A.A. (2009). Fear of recurrence in long-term testicular cancer survivors. Psycho-Oncology, 18, 580–588.
Strasburger, V.C., Jordan, A.B., & Donnerstein, E. (2012). Children, adolescents, and the media: Health effects. Pediatric Clinics of North America, 59, 533–587.
Testicular Cancer Awareness Foundation. (2014). Where does the money go? Retrieved from www.testicularcancerawarenessfoundation.org
Ugboma, H.A.A., & Aburoma, H.L.S. (2011). Public awareness of testicular cancer and testicular self-examination in academic environments: A lost opportunity. Clinics, 66, 1125–1128.
Urgurlu, Z., Akkuzu, G., Karahan, A., Beder, A., Dogan, N., Okdem, S., & Kav, S. (2011). Testicular cancer awareness and testicular self-examination among university students. Asian Pacific Journal of Cancer Prevention, 12, 695–698.
U.S. Preventive Services Task Force. (2011). Screening for testicular cancer: U.S. Preventive Services Task Force reaffirmation recommendation statement. Annals of Internal Medicine, 154, 483–486.
Ward, K.D., Vander Weg, M.W., Read, M.C., Sell, M.A., & Beech, B.M. (2005). Testicular cancer awareness and self-examination among adolescent males in a community-based youth organization. Preventive Medicine, 41, 386–398.
Wardle, J., & Steptoe, A. (1991). The European Health and Behaviour Survey: Rationale, methods and initial results from the United Kingdom. Social Science and Medicine, 33, 925–936.
Wong, W.C., Cheung, C.S., & Hart, G.J. (2008). Development of a quality assessment tool for systematic reviews of observational studies (QATSO) of HIV prevalence in men having sex with men and associated risk behaviours. Emerging Themes in Epidemiology, 5, 23–27.
Wood, G.L.B., Brown, C.G., Knobf, M.T., Lyon, D., Mallory, G., Mitchell, S.A., & Von Ah, D. (2014). Priorities for oncology nursing research: The 2013 national survey. Oncology Nursing Forum, 41, 67–76.
About the Author(s)
Saab is a PhD candidate, Landers is a lecturer, and Hegarty is a professor, all in the Catherine McAuley School of Nursing and Midwifery at the University College of Cork in Ireland. No financial relationships to disclose. Saab, Landers, and Hegarty contributed to the conceptualization and design and manuscript preparation. Saab and Landers completed the data collection. Saab and Hegarty provided statistical support. Saab contributed to the analysis. Saab can be reached at msaab@ucc.ie, with copy to editor at ONFEditor@ons.org. Submitted March 2015. Accepted for publication June 7, 2015.

