Decay, Transformation, and Growth: Meaning-Making Processes of Patients With Acute Leukemia Within the First Year After Diagnosis or Relapse
Purpose/Objectives: To explore the processes through which patients construct their meanings of acute leukemia (AL).
Research Approach: An exploratory design was employed using serial, in-depth interviews, guided by Smith’s Interpretative Phenomenological Analysis approach.
Setting: Two inpatient hematology clinics in the United Kingdom.
Participants: 10 adult patients with AL.
Methodologic Approach: Two serial interviews were conducted with each participant, two to four weeks apart, within the first year of diagnosis or post-relapse.
Findings: AL creates a state of imbalance, which may initiate a search for new equilibrium. Patients’ journeys toward making sense of their illness may involve three interchangeable processes: decay, transformation, and growth. As patients learned of their diagnosis and their treatment commenced, a sense of decay dominated their lives. Running in parallel, signs of transformation started to become more evident as time elapsed. Within growth, reprioritizing values was prominent.
Conclusions: Findings of this contextually and methodologically novel study highlight the complex nature of sense-making for patients experiencing AL.
Interpretation: Nurses can take valuable lessons on how to manage the invisibility of AL, enhance trust in healthcare professionals, address the impact of isolation, and facilitate the making-sense processes of patients in ways that favor their short- and long-term psychosocial adjustment.
Jump to a section
Finding meaning in life events is embedded in human nature (Frankl, 2011; Richer & Ezer, 2000; Skaggs & Barron, 2006). Particularly when facing negative events that challenge the existing construction of the world, individuals attempt to integrate their experiences (the ones of order and the ones of stress) in a new, meaningful reality through a search for meaning (Bonanno & Kaltman, 1999; Davis, Wortman, Lehman, & Silver, 2000; Janoff-Bulman, 1992; Josef & Linley, 2005; Lepore & Helgeson, 1998; Neimeyer, 2001; Park, 2010; Taylor & Gollwitzer, 1995). Finding meaning in or making sense of adverse events has been shown to increase subjective well-being (Lyubomirsky, King, & Diener, 2005) and subsequently enhance resilience, creativity, and distress tolerance (Fredrickson, Cohn, Coffey, Pek, & Finkel, 2008).
The integrated meaning-making model by Park and Folkman (1997) frequently is used in the context of illness (Lee, Cohen, Edgar, Laizner, & Gagnon, 2004; Park, 2010) because it provides operational definitions for the model’s different components. However, available evidence still is limited in amount and quality. Therefore, whether meaning-making during illness differs according to the stage, type of illness, and treatment trajectory remains unclear. In the context of cancer, individuals may use causal explanations, selective incidence, and placement of responsibility to make sense of their experience (Taylor, 1983; Taylor & Gollwitzer, 1995).
A diagnosis of acute leukemia (AL) is perceived as a watershed moment in patients’ lives, separating life before from life with the illness (Papadopoulou, Johnston, & Themessl-Huber, 2013). Of note, AL may pose particular difficulties because of its acute nature and the invasiveness of treatment it requires (Adelstein, Anderson, & Taylor, 2014; Koehler, Fischer, & Frommer, 2013). The physical and psychosocial impact of AL has been explored in diverse contexts and often drawing on mixed populations (Broers, Kaptein, Le Cessie, Fibbe, & Hengeveld, 2000; Greenberg et al., 1997; Persson, Hallberg, & Ohlsson, 1997; Rodin et al., 2013; Wittmann, Vollmer, Schweiger, & Hiddemann, 2006). Findings from two recent systematic reviews focusing on the symptom experience of patients diagnosed with AL have concluded that, although research interest is increasing for this population, additional research is needed (Albrecht, 2014; Leak Bryant, Lee Walton, Shaw-Kokot, Mayer, & Reeve, 2015). In stark contrast, the making-sense processes involved in the experiences of AL in adult patients remain largely unexplored (Papadopoulou et al., 2013). To move toward the development of tailored and more effective psychobehavioral interventions to support people affected by AL, establishing how they make sense of the illness is necessary. In-depth exploration of the illness experience can serve as a unique means toward greater understanding of the prominent and salient processes that underlie meaning-making in this context. To this end, the current study aimed to explore patients’ main pathways toward making sense of having been diagnosed with AL.
Methods
The current study was conducted from a critical realist perspective and used Interpretative Phenomenological Analysis (IPA) as a methodology, thereby acknowledging the plurality of perspectives and the reflexive voice of the researcher. In adopting a critical realist stance, the contribution of science is recognized, the possibility of objective knowledge is accepted, and an individual’s experiences and meanings can coexist and affect his or her behaviors and wider social structures (Clark, Lissel, & Davis, 2008; Porter, 2002). IPA offers researchers the advantage of learning how specific people deal with specific situations in specific contexts in great detail (Larkin, Watts, & Clifton, 2006; Smith, Flowers, & Larkin, 2009). This detail can reveal links and possibly variations within this same participant of how he or she makes sense of a certain experience.
Setting and Sample
The current study was granted NHS Tayside Research Ethics Committee A and Research and Development approval. Patients were recruited from inpatient and outpatient hematology clinics from two NHS health boards (Tayside and Grampian) in Scotland. Eligible patients were adult (aged older than 18 years) men and women diagnosed with AL (lymphoblastic, myeloid, or promyelocytic), had no previous cancer history, were within the first year post-diagnosis or post-relapse, and were undergoing or had completed anticancer treatment.
During a period of 12 months, a total of 13 consecutive, eligible patients with AL were approached by clinical collaborators at the clinical sites. Ten patients agreed to participate and provided written informed consent. Reasons for refusal included no interest in the study, being overly stressed, and death prior to participation. Characteristics of the study sample are outlined in Table 1.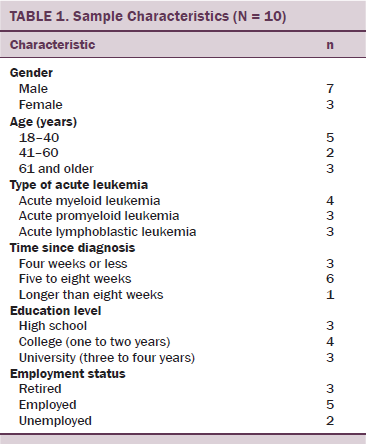
Data Collection Process
Interviews were conducted from October 2010 to March 2012. They were done by the first author in a private room in each site after patients had consented. The interviews were designed to capture the range and depth of the patients’ experiences following diagnosis or relapse (broad topic areas of interest included physical, emotional, mental, and social aspects and coping styles) but also to allow for sufficient flexibility for the interviewer to respond to individual participant circumstances. Interviews started with an open-ended question: “What does AL mean to you?” Cues from patients’ responses then were followed with a series of prompts, such as “Can you tell me a bit more about this?,” “How did this make you feel?,” “What does this mean to you?,” and “What does this mean about you?” All patients were interviewed twice. The interval between the two interview points ranged from two to four weeks, ensuring richness and depth of the collected data and also being in line with the iterative nature of the chosen methodology (Flowers, 2008). During the second interview, specific issues identified in the first interview were further explored. A debriefing procedure followed each interview, and patients were thanked for their participation. All data were treated confidentially, and all transcripts were anonymized and stored securely.
Quality
After the end of each interview, a reflexive sheet was completed, which detailed initial thoughts to identify any prejudices regarding the discussions raised during the interviews. In addition, a debriefing session (Clancy, 2013) was held within the research team to share thoughts and emotions after the interviews. Reflexivity during the data analysis process involved the maintenance of a personal reflexive diary, which started off with a statement of positionality (Clancy, 2013) and continued with the range of different emotions and considerations at the time of analysis. Previous professional expertise and experience were noted and revisited throughout the analysis process to ensure transparency and rigor. In engaging with the patients’ accounts, particular emphasis was placed when analyzing the text to maintain a balance between the theory of empathy and the theory of suspicion (Larkin et al., 2006).
Data Analysis
Interviews were transcribed verbatim. The two interviews were combined and analyzed together, forming a case (Flowers, 2008). Analyses followed the steps described by Smith et al. (2009), starting with a detailed examination of each case separately and examining similarities and differences across the cases. Combining the themes (emergent themes at first, then subordinate themes later) in different ways aided the final development and organization of the superordinate themes. These variations were followed by close checks of the transcripts to ensure that each subordinate theme was represented by a sufficient amount of examples within the transcripts. For a subordinate theme to be included in the organization of the superordinate themes, it had to be present in at least 50% of patients’ accounts. This process enhanced rigor of analysis and facilitated identification of exemplar quotes that were included in the final written account.
The integrated meaning-making model (Park, 2010) was influential during the preliminary stages of analysis when several elements in the accounts were identified as forming situational meaning or aspects of global meaning. During the development of superordinate themes (i.e., the meaning-making processes), the focus was placed specifically on patients’ accounts and experiences and the researcher’s interpretations of them.
Findings
Patients made sense of AL by engaging in three processes (superordinate themes): decay, transformation, and growth. Because AL created a state of imbalance for the individual, these processes were initiated as a mechanism to restore the previous balance or find a new state of equilibrium. To best capture the complexity of how meaning-making processes occur, a tree metaphor was selected for visual representation purposes. Maintaining equilibrium between decay, transformation, and growth can be seen as resembling the life of a tree: some leaves may wither, some start to grow, and some are in full bloom. Therefore, the three processes have no specific boundaries but may occur in parallel and manifest in different subordinate themes. As such, subordinate themes may appear in and shape more than one process. Fluidity of the three processes is demonstrated through examples of selected subordinate themes related to one, two, or three processes, and supported by patients’ quotes (see Figure 1).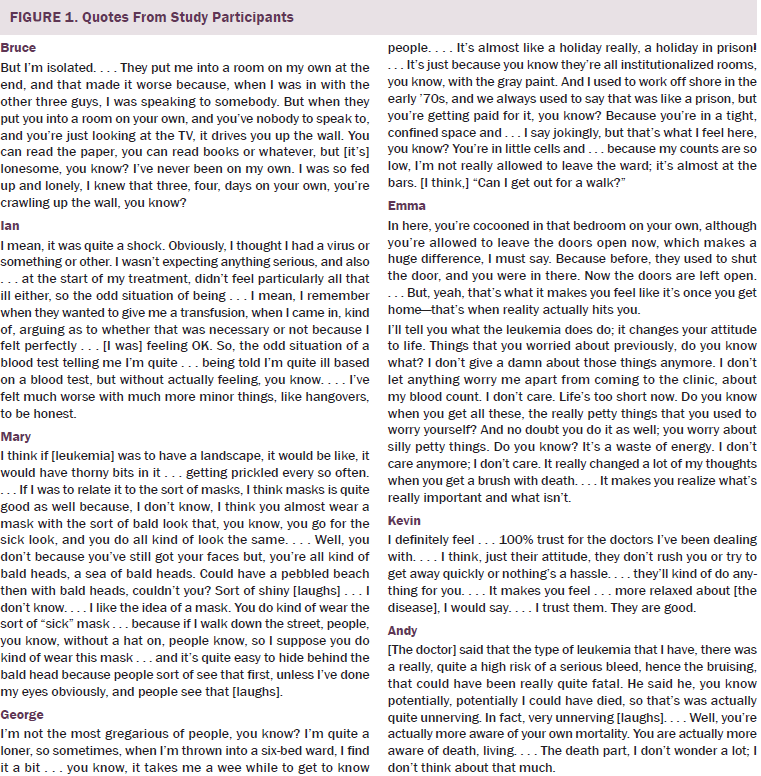
Decay: World of Emotions
Patients expressed an array of emotions during the interviews. In the initial phase of the cancer journey, the shock of diagnosis and fear dominated their minds; this was followed by uncertainty and a sense of living in an unreal world. Perhaps because of AL’s “invisibility,” these feelings and reactions were experienced to a greater extent, hindering patients’ efforts to understand their illness and possibly slowing down the initiation of coping mechanisms. Feelings of isolation and loneliness also were suggestive of decay at an emotional level that can prohibit patients’ sense-making process.
One participant, Bruce, used a strong metaphor to describe the emotional impact of his hospitalization: imprisonment. He said it made him want to “crawl up the wall.” His agony was prevalent as he said he felt like a trapped insect trying to find its way out by crawling up the walls of confinement to freedom. Leukemia places physical restrictions on patients that can have a profound emotional impact.
Decay and Transformation: Leukemia in Disguise
Aside from the emotional manifestations, the process of decay involved mental projections as well. One of the most prominent signs of a patient’s physical decay was AL’s disguise as an infection. The illness remained invisible for almost all of the patients (n = 9). Consequently, the diagnosis was conceived as a body blow, a sense that escalated as medical interventions were put on a fast-track mode: hospitalization, intensive chemotherapy, and supportive treatment.
One participant, Ian, described how he got his diagnosis of acute lymphoblastic leukemia. His AL was camouflaged by a viral infection. Ian struggled to finish his sentences, a sign of an internal tension or an indication of an underlying cognitive process to make sense of something that, in his mind, makes no sense. A single blood test, something considered to be a routine practice, carried the news of a serious, life-threatening illness. He said that this was an odd situation for him, particularly because he did not feel ill. His difficulty in understanding what was happening to him was even more striking as he questioned the need for treatment. A quite common assumption is that serious illnesses are accompanied by serious signs and symptoms. AL hardly falls under this category because symptoms resemble common flu, making patients comprehending its seriousness harder. The process of decay is indicative of how an illness that is invisible to the person yet serious can interfere with his or her process of making sense.
Within the process of transformation, leukemia’s form begins to evolve. By forming mental images, patients start to perceive their leukemia as an individual illness. Nevertheless, the difficulty in making sense of leukemia remains.
One participant, Mary, was in her final year of her studies in arts when she was diagnosed. She offered a vivid description of how she pictured leukemia: a thorn field piercing her body. She could be referring to the tests she underwent as a patient—the needles that went through her body during IV catheterization and bone marrow aspiration. For patients with AL, giving blood samples on a daily basis is a routine practice, and bone marrow aspiration is performed periodically to check the bone marrow activity to evaluate the effectiveness of chemotherapy. Mary also could have been referring to the physical distress the illness causes—a constant reminder of leukemia being there. Alternatively, because she was experiencing relapse, the thorns could represent the instances of leukemia. She wanted to move on with her life, but leukemia came back, “prickling” her again.
Mary’s transformation is that she is still processing leukemia. She uses two strong metaphors: the mask and a sea of bald heads. In her description is a double masking: the bald mask that covers the true self and a second masking that she employs by wearing a hat and coloring her eyes to conceal her baldness.
In Mary’s final picture, she mentioned the sea of bald heads, perhaps referring to all patients with leukemia. During the interviews, she mentioned how surprised she was when she first was admitted to the hospital to find out that leukemia was not as uncommon as she thought. This was her way of expressing how people, adults, and children affected by leukemia all eventually have the same bald head. She stressed how they all look the same—all passengers on the same train, on the same cancer journey. They all became patients, and the bald head stripped them of their previous identity and defined their new identity.
Seen as a thorn field, mask, or sea of baldness, AL is not faceless anymore; its disguise starts to crumble. This transformation from an illness in disguise to an illness with a more specific shape indicates how patients begin to shape meanings of their leukemia.
Decay, Transformation, and Growth: From a “Holiday in Prison” to “Being in a Coccoon”
Following a diagnosis of AL, treatment initiation is imperative. Not only do patients have to deal with treatment-related side effects, but they also have to deal with prolonged hospitalization, often experienced as a state of imprisonment and affected by dynamics within the patient–doctor relationship.
In another account, George described how he was “thrown” in a six-bedded ward, like a person with no will or power of his own, like a prisoner thrown into a cell with a number of strangers, who were ultimately his cell mates. During his first interview, he used the phrase “a holiday in prison” to describe his sense of institutionalization. Although he chose to compare his stay to a holiday, this description serves only as a euphemism to the hard reality of how he felt: a prisoner “at the bars.” In his comparison between staying in the hospital and the time he worked offshore, basic elements of imprisonment are present: the confinement, the gray color of the building, remaining inside, the everyday routine, and the lost track of time.
From a spatial perspective, patients with AL may feel like prisoners because remaining in the hospital is necessary to prevent infections. In reality, they are prisoners of their own body. Because of low blood counts, staying in the room is critical to help prevent acquiring infections that could cause delays in treatment or be fatal. This loss of freedom can cause a sense of agony, suggesting another sign of decay.
In time, this imprisonment is understood as temporary and is rationalized. The unknown starts to transform into a sense of familiarity. New routines emerge that are aspects of a new life in the hospital (e.g., receiving treatment, socializing with other patients and hospital staff).
Another participant, Emma, started to see her hospitalization in a different light. The metaphor she chose, the cocoon, is one of the most typical examples of transformation in nature. The cocoon in this case is the hospital room. Despite its confining and restricting nature, it also offers a shield of protection. Within it, all physiological things transform. She is receiving the treatment that transforms her marrow, leukemic cells are killed, and new cells are generated. The hospital cocoon also may provide protection from her emotional response. However, this transformation is not stable. It swings back to decay once she gets back home and the reality of the illness hits her on an emotional and physical level. This serves as an example of the degree to which transformation of the sense of captivity is a changeable, yet paramount, process in one’s efforts to make sense of AL.
The notion of imprisonment and confinement did eventually transform to a sense of security, indicating that the process of growth took over. Growth was evident when patients described their trust in healthcare professionals, which appears to be a result of two factors: the time spent together and the quality of information exchanged. This therapeutic collaboration signified the dynamic relationship between patients and clinicians. Feeling important and equal to the healthcare professionals partly relieved patients’ burden and potentially played a significant role in patients’ making-sense process. A sense of ease and security stemming from the staff members’ attitude is what one participant, Kevin, said made his trust blind, gave him permission to completely surrender to their hands, and, in a way, made his imprisonment tolerable.
Transformation and Growth: Assimilating Leukemia
The assimilation of leukemia starts within the transformation process and develops toward growth via the realization of mortality and the reprioritization of personal values. Patients in the current study spoke of the awareness of their own mortality. Leukemia, like any life-threatening illness, shakes two common assumptions: those of immortality and invincibility. Youth usually is paired with strength and health, which are thought to be ensured until old age. One participant, Andy, already had been diagnosed with another serious illness prior to his leukemia, so one would assume that he already would have realized his mortality. However, the transformation of his preexisting beliefs was not easily accomplished. He pointed out that he did not overthink the fact that he was mortal; therefore, signs existed of him assimilating the new illness but not to a full extent. When describing how he felt, he repeated twice how “unnerving” his experience was and he said he chose not to think about death as he chuckled, a sign of minimizing tension. A sense existed of not feeling at ease when he mentioned the word death; he immediately added the word “living.”
The transformation of assimilating leukemia refers to the point at which a person becomes aware of his or her mortal nature, which can be an important element in creating one’s understanding of leukemia. This transformation then leads to growth when the person has shaped an understanding of the illness and can identify its impact on his or her life. In this sense, the inclusion of leukemia in a person’s life story is the final result and the goal of the making-sense process.
A quote from Emma is a testament of the growth process in action. Through a reprioritizing process, she made decisions on what was important in her life and what did not matter anymore. She used a vivid metaphor to highlight the impact leukemia had in her life; she said she was “brushed with death.” This shaped her understanding of the illness and important things in life. She emphasized that she did not care about anything else other than staying alive and being with her loved ones. Focusing on trivial matters is an inherent part of human nature, but a life-threatening situation changes this for a person. It shifts attention to what genuinely is important.
Discussion
This qualitative study revealed that as patients learn of their diagnosis and their treatment commences, they undergo three different processes to make sense of their illness. This in-depth exploration and interpretation of these processes offered the opportunity to gain a better understanding of the highly complex pathways of making sense of an illness, such as AL. For patients in the current study, because they were close to the time of their diagnosis, the experience described as decay seemed to be more prevalent than the processes of transformation and growth, with the latter being the least evident. Even so, patients did show elements of all three processes, supporting the idea that even at the initial stages of the cancer journey, transformation and growth, not only decay, are experienced.
The coexistence of decay, transformation, and growth is indicative of the inextricable way in which meaning-making occurs. The meaning-making process has been postulated to be linear, consisting of overlapping phases (Skaggs & Barron, 2006). In their meaning-making model, Park and Folkman (1997) identified a number of distinct categories of making-sense processes, such as automatic and deliberate or assimilating and accommodating. The three processes identified in the current study are consistent with all of these distinctions (Park, 2010; Park & Folkman, 1997). For instance, within the processes of transformation and growth, signs of assimilation were seen, and, in certain occasions, signs of accommodation were seen in which patients’ illness affected their global meanings. Similarly, patients were not always aware of the meaning-making processes taking place, supporting the existence of automatic processes. However, patients also made more conscious, deliberate efforts to cope with AL.
Previous research on the processes patients use to construct meaning in the context of a life-threatening illness (Lee, 2008; Lee et al., 2004; Park, 2010), as well as in end-of-life care (Breitbart et al., 2010; Lethborg, Aranda, Bloch, & Kissane, 2006), share commonalities with the current study’s findings. Based on three domains (assumptive world, sense of coherence, and meaning-based coping), Lethborg et al. (2006) shared the idea that patients go through a dynamic process in order to make sense of their advanced cancer. This process involves positive reappraisal and revision of beliefs and goals. Lethborg et al. (2006) argued that their proposed model is linear and fluid and stressed the idea that as illness progresses, new issues may derange the balance. The processes of decay, transformation, and growth share this idea of linearity and fluidity. Although aspects of decay, transformation, and growth often co-occur in patients’ experiences, for an experience to move from decay to growth, it must go through a period of transformation and vice versa from growth back to decay, implying a linear process. Similarly, two sense-making processes have been identified in patients with colorectal cancer: disorientation and reconstruction (Tang et al., 2007). The phase of disorientation resembles the process of decay of patients with AL, and the process of reconstruction has elements of transformation and growth. Researchers identified internal and relational factors that can affect whether patients will move toward transformation and growth, proposing that the pathways are different for different people (Tang et al., 2007). This conceptualization of meaning-making is in accordance with the current study’s findings of maintaining a state of equilibrium within the three identified experiential processes.
Findings from the current study highlight the specific characteristics of AL that make patients’ understanding difficult. One of the most prominent signs of decay was AL’s disguise as infection. Leukemia’s trait of invisibility has been reported previously (Evans, Ziebland, & Pettitt, 2012; Koehler et al., 2011; Koenigsmann, Koehler, Franke, & Frommer, 2006; Koenigsmann, Koehler, Regner, Franke, & Frommer, 2006) and further supported by the experience of early flu-like symptoms, as well as the requirement for several referrals before a definite diagnosis can be made (Haberman, 1995; Meenaghan & Dowling, 2010). This partly explains why the diagnosis came as a body blow for patients. The invisibility of AL has been identified as a factor that hinders patients’ coping processes six weeks after their diagnosis (Koehler et al., 2011). In a Canadian study that concluded with similar findings, Nissim et al. (2013) described the initial phase of learning the diagnosis like “being abducted by the illness.” This feeling of rapid overnight transition from health to illness also was reported by patients with breast cancer after receiving results from routine testing (Boehmke & Dickerson, 2006). Within the process of transformation, patients started to perceive their AL more as an individual illness and formed mental images of what their cancer looked like.
Within the process of transformation, because of its ever-changing nature, elements can trigger decay as well as growth. This tendency has been documented elsewhere. The process, as well as outcome, of meaning-making can be distressing (Kernan & Lepore, 2009). The idea of post-traumatic growth during the initial phase of patients’ illness also has been documented (Nissim et al., 2013). For patients with AL, this contextual nature of meaning has been supported because the meanings emerging (as an end product) are always dependent on the person’s values and experiences at a given point (Steeves, 1992; Xuereb & Dunlop, 2003). Patients’ sense-making also can transform and grow, indicating life-affirming aspects of this experience. Similar results have been reported for patients with breast cancer, whose meaning-making was described as part of reframing the illness experience (Ching, Martinson, & Wong, 2012). This reframing process can lead to reprioritizing of values and eventually assigning new meanings to illness and purpose in life, resulting in a renewed self (Papadopoulou et al., 2013).
Strengths and Limitations
To the researchers’ knowledge, this is the first study to focus on the making-sense processes of patients with AL during the phase of intensive chemotherapy treatment using a novel approach to data analysis. Some limitations warrant comment. The sample consisted primarily of men (n = 7). Including more women in additional studies is necessary to tackle their making-sense processes. The current study was conducted in Scotland, and all patients were Caucasian and British. Including people with different cultural backgrounds could have produced different narratives and, therefore, different findings. Although the serial interviews ensured richness of data, they may have played a role in patients’ actual meaning-making by enabling the initiation or promotion of a making-sense process, which may not have occurred outside of the study. One way to reach meaning is through narrating a story (Holloway & Freshwater, 2007). According to Smith et al. (2009), a double hermeneutic—the interviewer trying to make sense of the interviewee trying to make sense of an experience —is normally part of an IPA study. Finally, these findings are from a specific group of people affected by AL under very different circumstances; therefore, the making-sense processes described are more suggestive than conclusive. The current study only was able to provide a snapshot of AL and the meaning-making processes people use to accommodate the illness in their lives. However, the philosophic underpinnings of the current study helped to compensate for this by supporting the notion of multiple aspects of reality. As time passes and the context and circumstances change, the patients’ meaning-making processes are expected to develop. Further research is warranted to examine how meaning-making processes change over time and to investigate these findings in larger populations.
Implications for Practice
For patients with AL, surrendering control to the clinical team has been reported as an adaptation strategy to manage the initial shock of a life-threatening illness (Nissim et al., 2013). Research suggests that patients with hematologic malignancies may prefer a more passive role in decision making (Friis, Elverdam, & Schmidt, 2003; Haberman, 1995; Tamayo, Broxson, Munsell, & Cohen, 2010; Yogaparan et al., 2009). In this sense, the clinical teams are perceived as “powerful others” to whom patients give permission to take control of the situation (Nissim et al., 2013). Whether this surrendering is beneficial for the patient is debatable. Patients in the current study had a strong sense of imprisonment because of their hospitalization that involved feelings of powerlessness rather than adaptation. Preserving patients’ autonomy and including them in the decision-making process is important even in the face of trivial tasks because it makes a difference to their perception of control during their hospital life (Papadopoulou et al., 2013; Tariman, Berry, Cochrane, Doorenbos, & Schepp, 2010, 2012). Interventions are needed that aim to enhance patients’ capability of managing the various cognitive and emotional challenges of the illness and increase their resilience by rebuilding strengths through adversities. For example, giving patients the opportunity to talk through their thoughts and emotions and receive tailored emotional support can be an effective way to facilitate meaning-making.
Conclusion
What the findings of this novel study underscore is the dynamic nature of the overall making-sense journey for patients experiencing AL. Additional longitudinal research will be required to not only inform and develop existing evidence, but also to shed light on the various ways in which meaning is initially constructed, negotiated, revisited, and reformed as patients and family carers go through the different phases of living with the illness. Meanwhile, a strong requirement exists for clinicians to provide adequate and ongoing support to help patients visualize the invisible AL and make sense of their illness-related situation that favors their short- and long-term psychosocial adjustment.
References
Adelstein, K.E., Anderson, J.G., & Taylor, A.G. (2014). Importance of meaning-making for patients undergoing hematopoietic stem cell transplantation [Online exclusive]. Oncology Nursing Forum, 41, E172–E184. doi:10.1188/14.ONF.E172-E184
Albrecht, T.A. (2014). Physiologic and psychological symptoms experienced by adults with acute leukemia: An integrative literature review. Oncology Nursing Forum, 41, 286–295. doi:10.1188/14.ONF.286-295
Boehmke, M.M., & Dickerson, S.S. (2006). The diagnosis of breast cancer: Transition from health to illness. Oncology Nursing Forum, 33, 1121–1127. doi:10.1188/06.onf.1121-1127
Bonanno, G.A., & Kaltman, S. (1999). Toward an integrative perspective on bereavement. Psychological Bulletin, 125, 760–776.
Breitbart, W., Rosenfeld, B., Gibson, C., Pessin, H., Poppito, S., Nelson, C., . . . Olden, M. (2010). Meaning-centered group psychotherapy for patients with advanced cancer: A pilot randomized controlled trial. Psycho-Oncology, 19, 21–28. doi:10.1002/pon.1556
Broers, S., Kaptein, A.A., Le Cessie, S., Fibbe, W., & Hengeveld, M.W. (2000). Psychological functioning and quality of life following bone marrow transplantation: A 3-year follow-up study. Journal of Psychosomatic Research, 48, 11–21.
Ching, S.S., Martinson, I.M., & Wong, T.K. (2012). Meaning making: Psychological adjustment to breast cancer by Chinese women. Qualitative Health Research, 22, 250–262. doi:10.1177/1049732311421679
Clancy, M. (2013). Is reflexivity the key to minimising problems of interpretation in phenomenological research? Nurse Researcher, 20, 12–16. doi:10.7748/nr2013.07.20.6.12.e1209
Clark, A.M., Lissel, S.L., & Davis, C. (2008). Complex critical realism: Tenets and application in nursing research. Advances in Nursing Science, 31, E67–E79. doi:10.1097/01.ANS.0000341421.34457.2a
Davis, C.G., Wortman, C.B., Lehman, D.R., & Silver, R. (2000). Searching for meaning in loss: Are clinical assumptions correct? Death Studies, 24, 497–540. doi:0.1080/07481180050121471
Evans, J., Ziebland, S., & Pettitt, A.R. (2012). Incurable, invisible and inconclusive: Watchful waiting for chronic lymphocytic leukaemia and implications for doctor-patient communication. European Journal of Cancer Care, 21, 67–77. doi:10.1111/j.1365-2354.2011.01278.x
Flowers, P. (2008). Temporal tales: The use of multiple interviews with the same participant. Qualitative Methods in Psychology, 5, 24–27.
Frankl, V.E. (2011). Man’s search for meaning: The classic tribute to hope from the Holocaust. London, England: Rider.
Fredrickson, B.L., Cohn, M.A., Coffey, K.A., Pek, J., & Finkel, S.M. (2008). Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology, 95, 1045–1062. doi:10.1037/a0013262
Friis, L.S., Elverdam, B., & Schmidt, K.G. (2003). The patient’s perspective: A qualitative study of acute myeloid leukaemia patients’ need for information and their information-seeking behaviour. Supportive Care in Cancer, 11, 162–170.
Greenberg, D.B., Kornblith, A.B., Herndon, J.E., Zuckerman, E., Schiffer, C.A., Weiss, R.B., . . . Holland, J.C. (1997). Quality of life for adult leukemia survivors treated on clinical trials of cancer and leukemia group B during the period 1971–1988: Predictors for later psychologic distress. Cancer, 80, 1936–1944.
Haberman, M. (1995). The meaning of cancer therapy: Bone marrow transplantation as an exemplar of therapy. Seminars in Oncology Nursing, 11, 23–31. doi:10.1016/S0749-2081(95)80039-5
Holloway, I., & Freshwater, D. (2007). Narrative research in nursing. Oxford, England: Wiley-Blackwell.
Janoff-Bulman, R. (1992). Shattered assumptions: Towards a new psychology of trauma. New York, NY: Free Press.
Josef, S., & Linley, P.A. (2005). Positive adjustment to threatening events: An organismic valuing theory of growth through adversity. Review of General Psychology, 9, 262–280.
Kernan, W.D., & Lepore, S.J. (2009). Searching for and making meaning after breast cancer: Prevalence, patterns, and negative affect. Social Science and Medicine, 68, 1176–1182. doi:10.1016/j.socscimed.2008.12.038
Koehler, M., Fischer, T., & Frommer, J. (2013). Caught by an acute leukaemia: Facing patients’ own experiences. Leukemia Research, 37, 481–482. doi:10.1016/j.leukres.2013.02.011
Koehler, M., Koehler, K., Koenigsmann, M., Kreutzmann, N., Fischer, T., & Frommer, J. (2011). Beyond diagnosis: Subjective theories of illness in adult patients with acute myeloid leukemia. Hematology, 16, 5–13. doi:10.1179/102453311x12902908411599
Koenigsmann, M., Koehler, K., Regner, A., Franke, A., & Frommer, J. (2006). Facing mortality: A qualitative in-depth interview study on illness perception, lay theories and coping strategies of adult patients with acute leukemia 1 week after diagnosis. Leukemia Research, 30, 1127–1134. doi:10.1016/j.leukres.2005.12.016
Koenigsmann, M., Koehler, M., Franke, A., & Frommer, J. (2006). Acute leukaemia in adults: Researching the patient’s perspective. Leukemia, 20, 206–207. doi:10.1038/sj.leu.2404005
Larkin, M., Watts, S., & Clifton, E. (2006). Giving voice and making sense in interpretative phenomenological analysis. Qualitative Research in Psychology, 3, 102–120. doi:10.1191/1478088706qp062oa
Leak Bryant, A., Lee Walton, A., Shaw-Kokot, J., Mayer, D.K., & Reeve, B.B. (2015). Patient-reported symptoms and quality of life in adults with acute leukemia: A systematic review [Online exclusive]. Oncology Nursing Forum, 42, E91–E101. doi:10.1188/15.onf.e91-e101
Lee, V. (2008). The existential plight of cancer: Meaning making as a concrete approach to the intangible search for meaning. Supportive Care in Cancer, 16, 779–785. doi:10.1007/s00520-007-0396-7
Lee, V., Cohen, S.R., Edgar, L., Laizner, A.M., & Gagnon, A.J. (2004). Clarifying “meaning” in the context of cancer research: A systematic literature review. Palliative and Supportive Care, 2, 291–303. doi:10.1017/S1478951504040386
Lepore, S.J., & Helgeson, V.S. (1998). Social constraints, intrusive thoughts, and mental health after prostate cancer. Journal of Social and Clinical Psychology, 17, 89–106. doi:10.1521/jscp.1998.17.1.89
Lethborg, C., Aranda, S., Bloch, S., & Kissane, D. (2006). The role of meaning in advanced cancer—Integrating the constructs of assumptive world, sense of coherence and meaning-based coping. Journal of Psychosocial Oncology, 24, 27–42. doi:10.1300/J077v24n01_03
Lyubomirsky, S., King, L., & Diener, E. (2005). The benefits of frequent positive affect: Does happiness lead to success? Psychological Bulletin, 131, 803–855. doi:10.1037/0033-2909.131.6.803
Meenaghan, T., & Dowling, M. (2010). Treatment for acute leukaemia: Elderly patients’ lived experiences. British Journal of Nursing, 19, 52–57. doi:10.12968/bjon.2010.19.1.45912
Neimeyer, R.A. (2001). The language of loss: Grief therapy as a process of meaning reconstruction. In R.A. Neimeyer (Ed.), Meaning reconstruction and the experience of loss (pp. 261–292). Washington, DC: American Psychological Association.
Nissim, R., Zimmermann, C., Minden, M., Rydall, A., Yuen, D., Mischitelle, A., . . . Rodin, G. (2013). Abducted by the illness: A qualitative study of traumatic stress in individuals with acute leukemia. Leukemia Research, 37, 496–502. doi:10.1016/j.leukres.2012.12.007
Papadopoulou, C., Johnston, B., & Themessl-Huber, M. (2013). The experience of acute leukaemia in adult patients: A qualitative thematic synthesis. European Journal of Oncology Nursing, 17, 640–648. doi:10.1016/j.ejon.2013.06.009
Park, C.L. (2010). Making sense of the meaning literature: An integrative review of meaning making and its effects on adjustment to stressful life events. Psychological Bulletin, 136, 257–301. doi:10.1037/a0018301
Park, C.L., & Folkman, S. (1997). Meaning in the context of stress and coping. Review of General Psychology, 1, 115–144.
Persson, L., Hallberg, I.R., & Ohlsson, O. (1997). Survivors of acute leukaemia and highly malignant lymphoma—Retrospective views of daily life problems during treatment and when in remission. Journal of Advanced Nursing, 25, 68–78. doi:10.1046/j.1365-2648.1997.1997025068.x
Porter, S. (2002). Critical realist ethnography. In T. May (Ed.), Qualitative research in action (pp. 53–72). London, England: Sage.
Richer, M.C., & Ezer, H. (2000). Understanding beliefs and meanings in the experience of cancer: A concept analysis. Journal of Advanced Nursing, 32, 1108–1115. doi:10.1046/j.1365-2648.2000.01581.x
Rodin, G., Yuen, D., Mischitelle, A., Minden, M.D., Brandwein, J., Schimmer, A., . . . Zimmermann, C. (2013). Traumatic stress in acute leukemia. Psycho-Oncology, 22, 299–307. doi:10.1002/pon.2092
Skaggs, B.G., & Barron, C.R. (2006). Searching for meaning in negative events: Concept analysis. Journal of Advanced Nursing, 53, 559–570. doi:10.1111/j.1365-2648.2006.03761.x
Smith, J.A., Flowers, P., & Larkin, M. (2009). Interpretative phenomenological analysis. London, England: Sage.
Steeves, R.H. (1992). Patients who have undergone bone marrow transplantation: Their quest for meaning. Oncology Nursing Forum, 19, 899–905.
Tamayo, G.J., Broxson, A., Munsell, M., & Cohen, M.Z. (2010). Caring for the caregiver [Online exclusive]. Oncology Nursing Forum, 37, E50–E57. doi:10.1188/10.ONF.E50-E57
Tang, V.Y., Lee, A.M., Chan, C.L., Leung, P.P., Sham, J.S., Ho, J.W., & Cheng, J. (2007). Disorientation and reconstruction: The meaning searching pathways of patients with colorectal cancer. Journal of Psychosocial Oncology, 25, 77–102. doi:10.1300/J077v25n02_05
Tariman, J.D., Berry, D.L., Cochrane, B., Doorenbos, A., & Schepp, K. (2010). Preferred and actual participation roles during health care decision making in persons with cancer: A systematic review. Annals of Oncology, 21, 1145–1151.
Tariman, J.D., Berry, D.L., Cochrane, B., Doorenbos, A., & Schepp, K.G. (2012). Physician, patient, and contextual factors affecting treatment decisions in older adults with cancer and models of decision making: A literature review [Online exclusive]. Oncology Nursing Forum, 39, E70–E83. doi:10.1188/12.ONF.E70-E83
Taylor, S.E. (1983). Adjustment to threatening events: A theory of cognitive adaptation. American Psychologist, 38, 1161–1173.
Taylor, S.E., & Gollwitzer, P.M. (1995). Effects of mindset on positive illusions. Journal of Personality and Social Psychology, 69, 213–226. doi:10.1037/0022-3514.69.2.213
Wittmann, M., Vollmer, T., Schweiger, C., & Hiddemann, W. (2006). The relation between the experience of time and psychological distress in patients with hematological malignancies. Palliative and Supportive Care, 4, 357–363. doi:10.1017/S1478951506060469
Xuereb, M.C., & Dunlop, R. (2003). The experience of leukaemia and bone marrow transplant: Searching for meaning and agency. Psycho-Oncology, 12, 397–409. doi:10.1002/pon.648
Yogaparan, T., Panju, A., Minden, M., Brandwein, J., Mohamedali, H.Z., & Alibhai, S.M.H. (2009). Information needs of adult patients 50 or older with newly diagnosed acute myeloid leukemia. Leukemia Research, 33, 1288–1290. doi:10.1016/j.leukres.2008.12.008
About the Author(s)
Papadopoulou is a lecturer in cancer care at the University of the West of Scotland in Paisley; Johnston is a professor in the School of Health Sciences at the University of Nottingham in Nottinghamshire, England; and Themessl-Huber is a clinical psychologist at NHS Tayside in Brechin, Scotland. No financial relationships to disclose. Papadopoulou contributed to the conceptualization and design, data collection, analysis, and manuscript preparation. Johnston and Themessl-Huber contributed to the manuscript preparation. Papadopoulou can be reached at constantina.papadopoulou@uws.ac.uk, with copy to editor at ONFEditor@ons.org. Submitted May 2015. Accepted for publication July 11, 2015.

