Whole Exome Sequencing: The Next Phase of Genetics Care
Exome sequencing is a technique for sequencing all of the genes that code for functioning proteins in the genome. It is now being used to identify mutations in families with suspected hereditary cancer syndromes where single-gene testing or testing for a panel of genes has not been able to detect a mutation. Oncology nurses need to anticipate that more patients and families will be undergoing this testing and be prepared to explain basic concepts about this new technology.
Jump to a section
Exome sequencing is a technique for sequencing all of the genes that code for functioning proteins in the genome. It is now being used to identify mutations in families with suspected hereditary cancer syndromes where single-gene testing or testing for a panel of genes has not been able to detect a mutation. Oncology nurses need to anticipate that more patients and families will be undergoing this testing and be prepared to explain basic concepts about this new technology. Challenges exist with this testing. For example, testing must often be done on several family members to yield useful results, many variants of unknown clinical significance may be detected, and unexpected gene variants associated with known diseases unrelated to the primary purpose of the test may be incidentally discovered. Families need support and information throughout the genetic testing process for whole exome sequencing.
The identification of mutations associated with an increased risk for developing cancer have implications for better long-term follow-up of cancer survivors, the prevention or detection of second malignancies, and the ability to identify which other close family members might be at risk, so they can make good decisions about cancer prevention and early detection. Oncology nurses routinely identify families with suspected hereditary risk because of family history and clinical characteristics (e.g., early onset cancers) and refer these families for genetic counseling and, when appropriate, genetic testing services.
Next-generation sequencing (NGS) allows for rapid analysis of multiple genes at a considerably lower cost compared to traditional genetic sequencing techniques. Patients with cancer undergoing genetic testing for hereditary cancer syndromes typically undergo a panel of 10–40 genes using NGS rather than single-gene testing with Sanger sequencing. The standard only a few years ago, Sanger sequencing uses short pieces of DNA to sequence a gene by separating fragments of DNA by size and then sequencing them with capillary electrophoresis to detect the order of base pairs on each fragment. NGS technology has paved the way to bring the next phase of genetic care, whole exome sequencing (WES), to the clinical setting (Levenson, 2015).
Data from the Human Genome Project suggest that the human genome consists of 3 billion nucleotides of DNA. However, only 1%–1.5% of those nucleotides are actually translated into proteins that have functional significance. This part of the genome is known as the exome. WES has the potential to sequence 20,000 genes simultaneously (Biesecker & Green, 2014). Research suggests that WES may be able to routinely identify genetic mutations in 25%–31% of individuals with suspected hereditary syndromes and possibly in as many as 50% of cases where more traditional single-site Sanger sequencing or NGS panels have not been able to identify a mutation, despite a clinical picture and family history being extremely suggestive of hereditary risk (Atwal et al., 2014; Levenson, 2015). In many cases, clinicians turn to WES in patients and families for whom more traditional NGS has been unable to identify a mutation; this is the appropriate indication (Arora, Haverfield, Richard, Haga, & Mills, 2015; Biesecker & Green, 2014).
Process of Whole Exome Sequencing
The technology used for WES breaks up DNA into small fragments, and then isolates and sequences the DNA fragments that came from exons (Prows, Tran, & Blosser, 2014). This is usually done with a blood specimen. Typical test turnaround time is 11–16 weeks (Atwal et al., 2014).
The American College of Medical Genetics and Genomics (ACMG) emphasizes that WES should be carried out only by credentialed genetics providers because of the complexities of counseling patients and families and the multitude of possible findings (ACMG Board of Directors, 2013). Families can be psychologically overwhelmed by the volume of data in the reports. As a result, genetics professionals can spend a great deal of time providing psychological support, and, in some cases, this may be more important than ensuring that patients understand the very technical details of how testing is conducted in the laboratory (Wynn, 2015). WES is often offered to families in the context of a research study, and families need to understand how the findings will be used (ACMG Board of Directors, 2013).
A number of steps occur with WES. A detailed family history is prepared that includes a minimum of three generations on the paternal and maternal sides. A detailed physical examination is undertaken, and, in the case of oncology, tumor characteristics and presentation are documented to better represent the phenotype. This process is followed by a careful review of the medical literature and databases to better characterize the phenotype and ascertain if it is suggestive of a rare syndrome. Other family members are evaluated for similar phenotypic characteristics. Once this information is gathered, the next step is to identify which family member or members should undergo WES to most likely receive useful test results. When three or more family members undergo WES simultaneously, the chance that a mutation will be detected is much greater (Retterer et al., 2015). This testing often includes a combination of individuals with the phenotypic characteristics and at least one other individual who appears to be healthy. In some cases, sequencing two more distant relatives with the phenotype than two close relatives with the phenotype is better because fewer variants will be shared solely by chance in close relatives (Biesecker & Green, 2014). WES compares each individual’s sequences to the standard and then considers the variants. The variants are compared among family members—a process that often points to the genetic change that may be contributing to the hereditary cancer syndrome. These variants are also evaluated using databases, literature review, and genetic models that predict whether the variant will affect protein function (Biesecker & Green, 2014). Findings are summarized in a report that details the outcomes of the testing. Organizing and coordinating testing and ensuring informed consent from multiple relatives can be challenging in terms of time and logistics, particularly if families are geographically distant.
Informed Consent
Families must be counseled that WES produces enormous amounts of genetic data, making interpretation of results much more complicated than with traditional NGS. Discussing the limitations of testing, including challenges in interpreting the clinical significance of variants and the meaning of negative results, is critical (Amendola et al., 2015; Bernhardt et al., 2015). Components that should be addressed prior to an individual’s undergoing WES are presented in Figure 1. 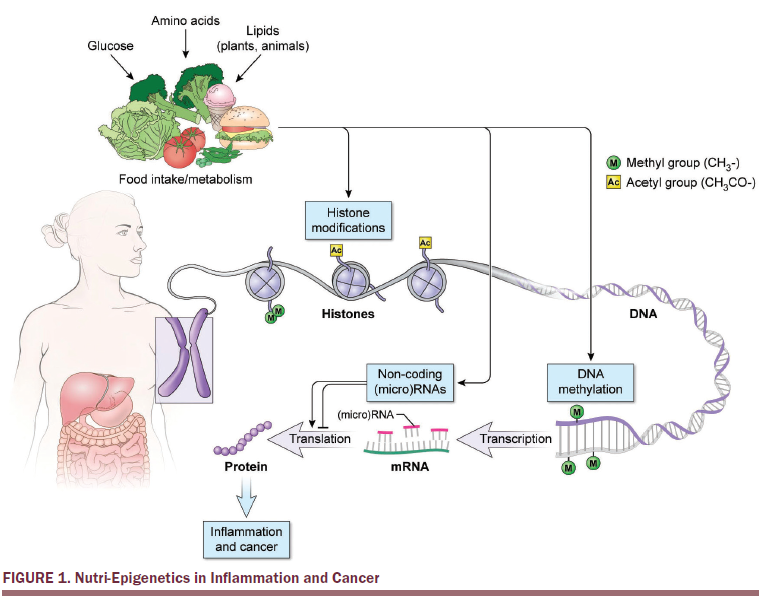
Outcomes of WES can be varied. Because multiple outcomes result from WES, results are typically reported separately (Prows et al., 2014). The primary result provides information about the disorder, syndrome, or clinical indication for the testing. It may be positive (a mutation was detected), negative (no known mutation was detected), or uncertain (variants were detected, but the clinical significance is not clear).
One of the biggest challenges of WES is the identification of variants and findings that may have clinical significance but were unexpected and unrelated to the original indication of the testing. These are referred to as incidental findings (IFs). IFs, or secondary findings, are reported similarly to primary results. Depending on what patients choose for disclosure, they may or may not learn about all of these results.
IFs can lead to unexpected distress. The possibility of IFs needs to be thoroughly explored in precounseling sessions. Patients and families must have a clear explanation of this possibility and need to decide how much information they wish to receive from such testing (Amendola et al., 2015). This can be particularly difficult if a healthy family member receives information about a potentially devastating diagnosis that was not expected. For this reason, counselors can consider giving results in two steps: the results regarding the indication for the testing first and the IFs second. Patients must decide if they want to know about all IFs or only those that are likely at this time to have clinically actionable steps (Roche & Berg, 2015).
WES will undoubtedly generate findings that will be better understood with additional research. Families need to understand how they will learn about this updated information or if such information will be provided (ACMG Board of Directors, 2013). One question that arises when considering this matter is whether the family assumes the responsibility of regularly contacting the genetics professional to determine if more information is available or if the genetics professional should contact the family. If an affected family member dies, a plan needs to be in place for how information about the genetic testing results will be shared with the next of kin.
Limitations
Costs of WES remain very high and may not be covered by traditional insurance plans. Exact costs are not readily published but are estimated to range from $4,500–$15,000; when a patient decides to pursue such testing, the laboratory doing the testing is contacted for a quote, and billing is arranged (Atwal et al., 2014; Biesecker & Green, 2014).
A negative test can be difficult to interpret. Some exons, such as those located in the repeats out toward the chromosome ends, may not be detectable with current technology (Prows et al., 2014). A small number of genes with potential mutations reside in mitochondria, rather than in the nucleus, and will often go undetected. Translocations and inversions that move or flip DNA, but do not alter the base sequence, may not be detected with all sequencing methods. Another limitation is that, if a mutation is identified in a family, having other family members undergo testing for this mutation may be challenging, particularly if such testing is not readily available in the clinical setting (Amendola et al., 2015).
Implications for Nurses
Because WES has been provided only on a limited basis and often in the context of a research study, understanding how patients manage and use this information to develop plans to prevent or reduce the risk of developing malignancy, as well as create personalized plans for early detection, is important. Such understanding, including whether negative psychological effects exist, will help nurses to provide better informed consent to future patients.
Equipping patients with the tools to make informed decisions is challenging (Roche & Berg, 2015). A limit exists to how much a patient can understand in one setting. Patients learn in many different ways. For example, some patients may prefer detailed printed literature, whereas others may want audiovisual presentations. Many patients travel great distances to access genetics providers, and using in-person time well is critical. Because counseling for WES should be provided by credentialed genetics professionals, and because many regions of the country lack resources, a need exists to find ways to efficiently provide this information, including means to provide introductory teaching prior to the appointment. This clearly is an area that requires more research.
Conclusion
WES holds much excitement and possibility for the future. Technological developments will continue to emerge in the field of genomics. Families who previously have not been able to have a mutation identified may now have that opportunity. Oncology nurses need to understand not only the technology and biology underlying these newer genetic testing techniques, but also the significance of the clinical applications of new technologies, implications for patients and their families, and the potential for developing tailored prevention and early detection guidelines and recommendations. Oncology nurses will continue to be challenged to correctly identify patients who may benefit from genetic counseling and possibly genetic testing, as well as refer those individuals to a genetics professional who can coordinate care for patients and their families.
References
Amendola, L.M., Lautenbach, D., Scollon, S., Bernhardt, B., Biswas, S., East, K., . . . Jarvik, G.P. (2015). Illustrative case studies in the return of exome and genome sequencing results. Personalized Medicine, 12, 283–295. doi:10.2217/pme.14.89
American College of Medical Genetics and Genomics Board of Directors. (2013). Points to consider for informed consent for genome/exome sequencing. Genetics in Medicine, 15, 748–749. doi:10.1038/gim.2013.94
Arora, S., Haverfield, E., Richard, G., Haga, S.B., & Mills, R. (2015). Clinical and counseling experiences of early adopters of whole exome sequencing. Journal of Genetic Counseling. Advance online publication. doi:10.1007/s10897-015-9876-y
Atwal, P.S., Brennan, M.-L., Cox, R., Niaki, M., Platt, J., Homeyer, M., . . . Hudgins, L. (2014). Clinical whole-exome sequencing: Are we there yet? Genetics in Medicine, 16, 717–719. doi:10.1038/gim.2014.10
Bernhardt, B.A., Roche, M.I., Perry, D.L., Scollon, S.R., Tomlinson, A.N., & Skinner, D. (2015). Experiences with obtaining informed consent for genomic sequencing. American Journal of Medical Genetics, 167, 2635–2646. doi:10.1002/ajmg.a.37256
Biesecker, L.G., & Green, R.C. (2014). Diagnostic clinical genome and exome sequencing. New England Journal of Medicine, 370, 2418–2425. doi:10.1056/NEJMra1312543
Levenson, D. (2015). Whole-exome sequencing effective at diagnosing elusive genetic disorders: Tests diagnose about 25% of patients, find a variety of mutation types. American Journal of Medical Genetics, 167A, vii–viii. doi:10.1002/ajmg.a.36965
Prows, C.A., Tran, G., & Blosser, B. (2014). Whole exome or genome sequencing: Nurses need to prepare families for the possibilities. Journal of Advanced Nursing, 70, 2736–2745. doi:10.1111/jan.12516
Retterer, K., Juusola, J., Cho, M.T., Vitazka, P., Millan, F., Gibellini, F., . . . Bale, S. (2015). Clinical application of whole-exome sequencing across clinical indications. Genetics in Medicine. Advance online publication. doi:10.1038/gim.2015.148
Roche, M.I., & Berg, J.S. (2015). Incidental findings with genomic testing: Implications for genetic counseling practice. Current Genetic Medicine Reports, 3, 166–176. doi:10.1007/s40142-015-0075-9
Wynn, J. (2015). Genomic testing: A genetic counselor’s personal reflection on three years of consenting and testing. Journal of Genetic Counseling. Advance online publication. doi:10.1007/s10897-015-9868-y
About the Author(s)
Mahon is a professor in the Department of Internal Medicine, Division of Hematology/Oncology, and a professor of adult nursing in the School of Nursing at Saint Louis University in Missouri. No financial relationships to disclose. Mahon can be reached at mahonsm@slu.edu, with copy to editor at ONFEditor@ons.org.

