Decisional Conflict: Relationships Between and Among Family Context Variables in Cancer Survivors
Purpose/Objectives: To investigate the relationships among life stress, family functioning, family coping, reliance on formal and informal resources, and decisional conflict in cancer survivors.
Design: Cross-sectional.
Setting: Participants were recruited from the California Cancer Surveillance Program, hospital registries, and community agencies in southern California and Cleveland, Ohio.
Sample: 243 European American, African American, Chinese American, and Korean American cancer survivors diagnosed with breast, colorectal, or prostate cancer.
Methods: The merged data from an ethnically diverse cohort of cancer survivors participating in the two survey studies were used. Standardized measures were used to identify family context variables and decisional conflict.
Main Research Variables: Life stress, family functioning, family coping, reliance on formal and informal resources, and decisional conflict.
Findings: Structural equation modeling demonstrated that life stress was significantly associated with decisional conflict. Family functioning significantly mediated the impact of life stress on decisional conflict through family coping. Reliance on formal and informal resources moderated the relationships among the study variables.
Conclusions: The role of the family context, which includes family functioning and coping, on decisional conflict is important in the adjustment process to make high-quality decisions in cancer survivorship care.
Implications for Nursing: Findings present nursing practice and research implications that highlight the need for efforts to encourage and support family involvement in the decision-making process and to enhance cancer survivors’ adjustment process.
Jump to a section
The importance of shared decision making in treatment for patients with cancer has increased in recent years. However, a lack of understanding about decision making in follow-up care after cancer treatment is still prevalent (Hudson et al., 2012). Cancer survivors may be involved in decision making about their survivorship care plans with the healthcare team, including their primary care provider and family members. Survivorship care plans are used to monitor the long-term and late physical and psychological effects of cancer and its treatment, screen for the development of secondary cancers, and manage comorbid medical conditions (Haq et al., 2013). The benefits, harms, and inconveniences in the options for cancer survivorship care can influence a patient’s prognosis and quality of life (Andersen, Bowen, Morea, Stein, & Baker, 2009; O’Connor, Légaré, & Stacey, 2003); cancer survivors may experience decisional conflict about the best options for survivorship care (e.g., when or where to get follow-up care after cancer treatment) and may require emotional and tangible support in the decision-making process (Abrahamson, Durham, & Fox, 2010).
Decisional conflict refers to uncertainty about the types of actions individuals should take when a choice among multiple options involves risk, loss, or challenge to personal life values (LeBlanc, Kenny, O’Connor, & Légaré, 2009). The manifestation of decisional conflict may vary by individual, familial, and situational contexts. For example, personal anxiety, unrealistic expectations, or a lack of support and resources in choice situations (e.g., surgery versus nonsurgery, telling the truth versus not telling the truth) may make decisions difficult and complex (Blank, Graves, Sepucha, & Llewellyn-Thomas, 2006). For cancer, decisional conflicts can occur in the transition from active treatment to post-treatment care as the patient’s role changes to focus on self-management of lifestyle behaviors or late effects of treatment.
During the adjustment to the survivorship phase, the family context (e.g., life stress, functioning, coping, resources) may have a primary role in affecting decisional conflict about survivorship care (Lim & Paek, 2013; Powazki, 2011). The life stress (e.g., dealing with money, raising children) that family members experience can influence decision-making processes. Under stressful circumstances, people with severe illness often fail to make rational choices based on their weighing of the utilities and probabilities associated with all available courses of action (Powazki, 2011). In terms of family functioning (i.e., cohesion, flexibility, and communication), family members in highly cohesive families tend to unite for resolving decisional conflict and mutual support in times of decision making (Olson, 2000). The family’s ability to change role relationships and rules to respond to situational needs (i.e., flexibility) is helpful in addressing decisional conflicts (Deimling, Smerglia, & Schaefer, 2001). Several studies in the literature have indicated that good communication between cancer survivors and families can reduce decisional conflict in cancer care (Siminoff, Zyzanski, Rose, & Zhang, 2008). In addition, coping, a set of cognitive and behavioral strategies, plays a key role in the resolution of decisional conflict in stressful situations (Folkman & Moskowitz, 2004). For example, people tend to search for relevant information using external resources to resolve decisional conflict (David, Montgomery, & Bovbjerg, 2006). In addition, families are often involved in the decision-making process about cancer care options (Andersen et al., 2009; Jansen, Otten, & Stiggelbout, 2006; Michael, O’Callaghan, Baird, Hiscock, & Clayton, 2014). Whether cancer survivors rely on formal (e.g., health professionals) or informal resources (e.g., family members) in healthcare decisions may influence how they cope with stress and manage decisional conflict (Davison, Goldenberg, Gleave, & Degner, 2003; Lingler, Sherwood, Crighton, Song, & Happ, 2008; O’Rourke, 2001; Shin et al., 2013). However, no research exists regarding the way reliance on formal and informal resources influences decisional conflict within the family context for those moving into the survivorship phase after active treatment is over.
Conceptual Framework
The current study was guided by the adjustment phase of the Typology Model of Family Adjustment and Adaptation (hereafter referred to as the Typology Model) (McCubbin & McCubbin, 1988) and the Conflict-Theory Model of Decision Making (CTM) (Janis & Mann, 1977). According to the Typology Model, the level of family adjustment in a crisis situation is determined by stressor events interacting with family functioning, the family’s resources, and the family’s problem-solving and coping skills. More specifically, family resources buffer the impact of a stressor or change on family life and promote adjustment (Curran, 1983; Stinnett & DeFrain, 1985). However, the Typology Model does not specify crisis situations in cancer survivorship care. To link the relationship between the family context under the Typology Model and decisional conflict as a crisis situation, the current study combines the CTM with the Typology Model. The CTM (Janis & Mann, 1977) assumes that the stressful nature of choosing, influenced by risk, ambiguity, and loss, is strongly related to the level of stress that an individual experiences during the process of decision making. Based on the Typology Model and the CTM, life stress, family functioning, and family coping factors were included to investigate how the family context influences cancer survivors’ maladjustment—that is, decisional conflict. Reliance on informal and formal resources as one of the family resources was also considered as a moderator of the stress process on decisional conflict.
The current study aimed to investigate the relationships among life stress, family functioning, family coping, reliance on formal and informal resources, and decisional conflict in cancer survivors under the Typology Model and the CTM. The authors hypothesized that (a) life stress is significantly associated with decisional conflict (H1); (b) family functioning significantly mediates the impact of life stress on decisional conflict through family coping (H2); and (c) reliance on formal and informal resources in survivorship care moderates the effects of life stress, family functioning, and family coping on decisional conflict (H3).
Methods
Data Sources and Study Population
The current authors merged two sets of secondary survey data that investigated family coping and communication for cancer survivors in two regions (Los Angeles, California, and Cleveland, Ohio) from October 2009 to February 2012. The recruitment period and procedures, survey administration, and measures were almost identical, making these two studies comparable. A total of 243 cancer survivors (153 in Los Angeles and 90 in Cleveland) were included in the final analysis.
The study sample, population, recruitment, and data collection procedures are detailed elsewhere (Lim & Ashing-Giwa, 2013; Lim, Shon, Paek, & Daly, 2014). Eligible participants included adults within one to five years of a diagnosis with breast, colorectal, or prostate cancer in stages I–III and who had completed active treatment, including surgery, chemotherapy, and radiation. The study participants consisted of European Americans (n = 74), African Americans (n = 16), Chinese Americans (n = 83), and Korean Americans (n = 70). Participants were able to speak Mandarin/Cantonese, Korean, and/or English. Survivors who were diagnosed with stage IV cancer and those with other major medical (e.g., heart disease) and psychiatric (e.g., schizophrenia) conditions were excluded because their disease progression and prognosis were significantly different from their study counterparts.
Recruitment strategies to identify the study samples included the following: (a) sending invitation letters to potential participants whose contact information was obtained from the cancer registries in the California Cancer Surveillance Program and University Hospitals (Cleveland, Ohio) and (b) distributing study flyers in the community. Survivors provided informed consent to participate in the study. Experienced bilingual interviewers recruited and interviewed patients. The studies were approved by the institutional review boards at each study site.
Instruments
Survey instruments were translated and back-translated into Chinese and Korean using a rigorous “forward-backward” translation procedure. The panel of translators compared the two English versions, and corrections were made until equivalence was achieved (Lim & Ashing-Giwa, 2013).
Life stress: Life stresses were measured from the 14 items of the Life Stress Scale, which was designed to examine the level of burden regarding various aspects of life (Ashing-Giwa, Padilla, Tejero, & Kim, 2004). The current authors’ preliminary confirmatory factor analysis demonstrated that this scale comprised four components: (a) socioeconomic stress (four items), (b) family stress (three items), (c) racist crime and violence (three items), and (d) neighborhood stress (three items). Items were rated from 1–5, with higher scores indicating higher levels of stress. Scores were obtained by averaging the items in each component. In the current study, the internal consistency of the scales ranged from 0.71–0.84.
Family functioning: Two family functioning scales were used to comprehensively create the latent factor of family functioning, including family cohesion, flexibility, and communication. First, family cohesion (i.e., the emotional bonding that exists between family members) and family flexibility (i.e., the family’s ability to change its power structure, role relationships, and rules) were adapted from the Family Adaptability and Cohesion Evaluation Scales III (FACES III) (Olson, 1986). Responses to this 20-item standardized family functioning instrument were provided on a five-point Likert scale. The family cohesion (seven items) and flexibility (three items) scores were obtained by averaging the items of each component. Higher scores indicate positive functioning in family cohesion and flexibility. The FACES IV-Family Communication Scale, which was designed to investigate the functionality of communication within the family, was used to assess family communication (Olson, Gorall, & Tiesel, 2004). This 10-item self-reported questionnaire was measured on a five-point Likert scale, and scores were calculated by averaging all items. Higher scores reflect better family communication. The internal consistency of the scales was 0.86, 0.7, and 0.96 for family cohesion, flexibility, and communication, respectively.
Family coping: The Family Crisis Oriented Personal Evaluation Scales (F-COPES), which was designed to identify families’ problem-solving strategies when faced with crises, was used to assess family coping (McCubbin, Larsen, & Olson, 1987). Although the F-COPES is a 29-item, five-subscale inventory, the current study included three active coping subscales (Lim & Townsend, 2012): (a) relative or friend support, (b) neighbor support, and (c) mobilization of the family to obtain and accept help. Respondents were asked to rate items on a scale of 1 (almost never) to 5 (almost always). Subscale scores were obtained by averaging the responses to all items. High scores indicate more frequent use of active coping strategies. In this study, the internal consistency of the subscales ranged from 0.71–0.8.
Reliance on formal and informal resources: Reliance on formal and informal resources was measured using the question, “How important are each of these groups/people to making healthcare decisions?” The measure is composed of eight support sources, including four informal social ties (i.e., family, children, partner or spouse, and friends) and four formal social ties (i.e., religious or faith community, support group, medical team, and counselors or therapists). Respondents rated each of the eight support sources on a five-point Likert scale. To divide reliance on formal and informal resources by two groups (hereafter referred to as formal reliance and informal reliance groups), the individual mean scores of the degree of importance of formal or informal social ties were standardized based on the total mean and standard deviation. Then, individual standardized mean scores were directly compared to choose either formal or informal reliance. Higher numbers of formal standardized scores than informal standardized scores suggest that individuals rely more heavily on formal ties than informal ties when making healthcare decisions.
Decisional conflict: Decisional conflict was adapted from the Decisional Conflict Scale (O’Connor, 1995). The 11-item scale was designed to evaluate personal perceptions of (a) feeling uncertainty in choosing options (two items), (b) feeling uninformed (two items), (c) being unclear about personal values (two items), (d) being unsupported in decision making (three items), and (e) conducting effective decision making (two items). In this measure, 11 items were rated on a five-point Likert scale. To score decisional conflict, items were averaged to obtain a mean score of each subscale, with higher scores indicating higher decisional conflict in healthcare. In the current study, the reliability coefficients ranged from 0.7–0.89.
Data Analyses
Descriptive statistics were determined to describe the study samples. Independent sample t tests and chi-square tests were conducted to investigate whether demographic and medical variables varied between formal and informal reliance groups. The univariate general linear model was used to compare differences in predictors and outcomes between the two groups, and demographic and medical variables that showed significant differences were included as covariates. The data were analyzed using SPSS®, version 20.0. All hypotheses were tested using the p < 0.05 criterion for significance.
A preliminary analysis based on a multistep procedure (Horn & McArdle, 1992; Meredith, 1993) was conducted to determine whether the scales possessed measurement invariance across research sites because the scales for the Los Angeles study had been translated into Chinese or Korean. The findings demonstrated that life stress, family functioning, and family coping showed measurement variance based on the chi-square difference tests. Consequently, these three measures were modified to have equivalent meaning across the studies, removing items that had different meanings (i.e., differences in factor loadings). The modified factor models demonstrated measurement invariance across the studies (life stress: chi-square[9] = 16.4, p = 0.06; family functioning: chi-square[16] = 26, p = 0.05; family coping: chi-square[9] = 14.6, p = 0.1; decisional conflict: chi-square[6] = 7.3, p = 0.29).
Structural equation modeling (SEM) was used to test the mediation model (H1 and H2) using AMOS®, version 20.0. In the authors’ dataset, the number of missing values was less than 1%; therefore, missing data were addressed with full information maximum likelihood estimation. Prior to testing the structural model, the measurement model at the item level was tested to assess the adequacy of the latent factors and to confirm the dimensionality of the latent variables. The findings for the measurement models demonstrated that the factor loadings on each latent factor were statistically significant at a p < 0.001 level. As a result, composite scores were used for each construct to reduce the number of parameter estimations. The structural model was then tested to examine the hypothesized relationships between the study variables based on the theoretical model. The hypothesized model was evaluated using goodness-of-fit indices that included the chi-square statistic or discrepancy function, the ratio of the discrepancy function to the number of degrees of freedom, the root mean square error of approximation ([RMSEA], acceptable fit ≤ 0.08) (Steiger, 1990), and the comparative fit index ([CFI], acceptable model fit ≥ 0.9) (Bentler, 1990).
The moderating effects of reliance on formal and informal resources in the overall model (H3) were tested using a multigroup SEM analysis (Bollen, 1989; Kline, 1998). The multi-group analysis is conducted by comparing three models: (a) unconstrained, (b) measurement-model constrained, and (c) structural-model constrained. If model comparisons using chi-square difference tests do not reach statistical significance, this indicates the invariance of factor loadings and path coefficients between formal and informal reliance groups. Critical ratios (CRs) for differences tests were conducted to examine differences between the two groups on all direct effect parameters.
Results
The mean age of the cancer survivors was 58 years (SD = 11), and the mean number of comorbidities was 3.4 (SD = 3.3). The mean number of years since diagnosis was 3.6 (SD = 1.7). The majority of the respondents were female (n = 186, 77%), had completed either high school or college (n = 220, 91%), and had spouses or partners (n = 211, 87%). Most were diagnosed with breast cancer (n = 181, 75%), and almost half were diagnosed with stage II cancer (n = 131, 54%).
The formal (n = 134) and informal (n = 109) reliance groups showed significant differences in the degree of importance of formal (t = 3.9, p < 0.001) and informal social ties (t = –6.39, p < 0.001). The formal and informal reliance groups did not differ significantly in most demographic characteristics except marital status; the informal reliance group was more likely than the formal group to have spouses or partners. For medical characteristics, comorbidities showed a significant difference, indicating that the formal reliance group was more likely than the informal group to have higher comorbidities (see Table 1). Consequently, marital status and current comorbidities were adjusted in the following analysis.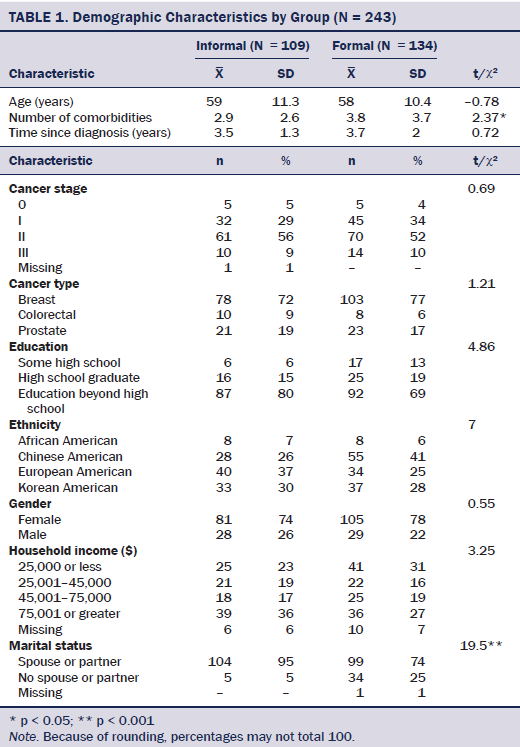
Life stress, family coping, and decisional conflict scores did not reveal significant differences between the formal and informal reliance groups after adjusting covariates. However, in the family functioning constructs, cohesion and family communication showed significant differences. The informal reliance group was more likely than the formal group to have better cohesion and family communication scores (see Table 2).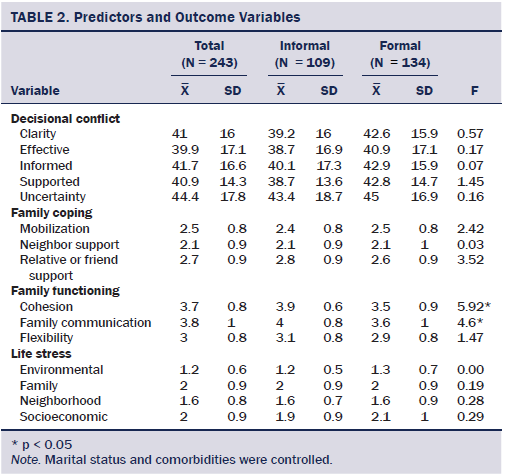
Testing the Mediation Model
The proposed mediation model was created with an outcome (decisional conflict), one predictor (life stress), two mediators (family functioning and coping), and four covariates (cancer stage, current comorbidities, income, and marital status). The hypothesized model produced an acceptable fit: chi-square(141) = 303.57, CFI = 0.91, RMSEA = 0.07. The model accounted for 23% of the variance in decisional conflict.
Factor loadings on the construct of decisional conflict ranged from 0.68–0.92. In addition, factor loadings on life stress, family functioning, and family coping ranged from 0.51–0.79, from 0.6–0.98, and from 0.63–0.88, respectively. All latent constructs were relatively well defined. The SEM findings demonstrated that life stress is significantly associated with family functioning (b = –0.31, p < 0.001). Family functioning was significantly related to family coping (b = 0.53, p < 0.001), and family coping was significantly associated with decisional conflict (b = –0.16, p < 0.05). The total effect of life stress on decisional conflict, which includes mediating and direct effects, was significant (b = 0.42, p < 0.001). Survivors who experienced life stresses showed worse family functioning, did not use active coping, and, in turn, were more likely to have decisional conflicts.
Moderating Effect of Reliance on Formal and Informal Resources
Multigroup SEM was used to determine the moderating effect of reliance on formal and informal resources (see Table 3). The first step of the analysis tested the baseline model for the two groups (formal versus informal reliance groups). Findings showed acceptable fit indices: chi-square(282) = 475.64, CFI = 0.9, RMSEA = 0.05. The chi-square difference tests did not find significant differences between the baseline model and the factor loading constrained model (chi-square[11] = 12.68, p = 0.31). Differences between the baseline model and the constrained structural path model were found at a p < 0.01 level (chi-square[36] = 64.98), which suggests that life stress affects decisional conflict through family functioning and family coping differently, according to reliance on formal and informal resources. Specifically, the two groups showed different pathways from family coping to decisional conflict (CR = 2.01, p < 0.05). The family coping of survivors who relied on informal resources in healthcare decisions was directly associated with decisional conflict, whereas the family coping of survivors who relied on formal resources was not associated with decisional conflict.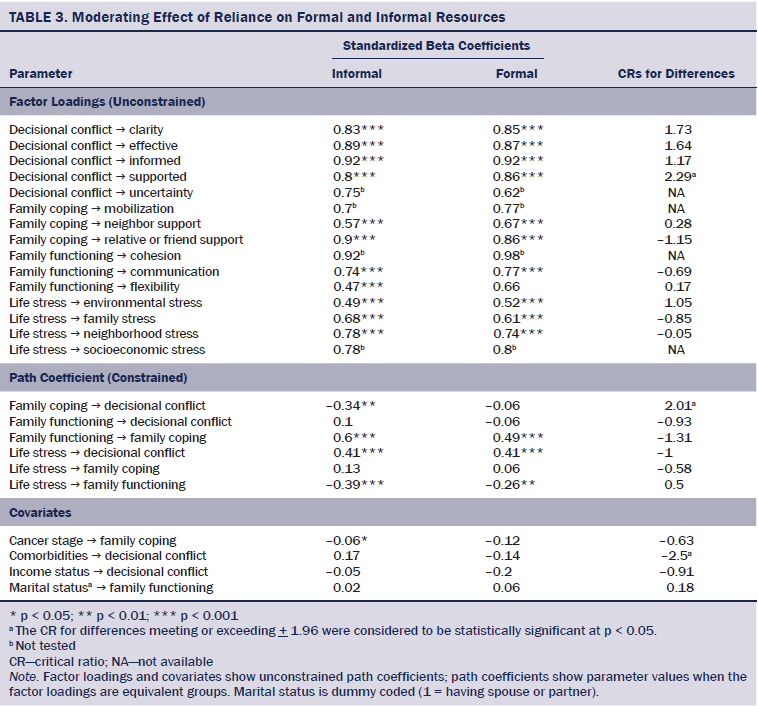
Discussion
The current study intended to investigate the relationships among life stress, family functioning, family coping, reliance on formal and informal resources, and decisional conflict in cancer survivors under the Typology Model and the CTM. The study demonstrated that life stress was significantly associated with decisional conflict (H1). Family functioning significantly mediated the impact of life stress on decisional conflict through family coping (H2). Reliance on formal and informal resources moderated the relationships among the study variables, suggesting a difference in the pathway from family coping to decisional conflict between formal and informal reliance groups (H3). As such, this study supported its hypotheses.
Most research on cancer survivorship to date has focused on individuals coping with cancer. The current study has shown that considering the family context in healthcare decisions has implications for the family that can shape how cancer survivors make decisions related to survivorship care during the transition from active treatment to post-treatment care. One of the significant findings was that family functioning and family coping mediate the pathway linking life stress and decisional conflict. It suggests that decisional conflict may be influenced by how close and flexible the family members are, how family members communicate with one another, and how family members cope with their problems in stressful situations. According to the Typology Model, families engage in processes to balance life stress with family functioning, resources, and coping and, in turn, influence their adjustment and maladjustment. In addition, the CTM emphasized the relationship between family coping and decisional conflict. Based on findings, the current study conceptually supports the Typology Model and the CTM for cancer survivors.
Study findings demonstrated that life stress and family coping were directly associated with decisional conflict for cancer survivors, which is consistent with other studies (Gillis, 1993; Michael et al., 2014). Survivors who have higher life stresses are more likely to have decisional conflicts, whereas those who have active coping strategies are less likely to have decisional conflicts. Individuals who experience life stress tend to be vulnerable to the dynamics of the environment and decision-making activities because stress narrows the focus of attention (Kerstholt, 1994). Nevertheless, some studies show that individuals adopt simpler modes of information processing that may help in focusing on critical issues, suggesting that decisions can only be made based on the information available (Kowalski-Trakofler, Vaught, & Scharf, 2003). As a result, coping with stressful situations may influence decision-making activities, and active coping strategies may be particularly helpful to reduce decisional conflict. The current study provides a better understanding of how individuals make the choices they do under stress.
Based on findings from this study, family functioning may be an important precondition for effective strategies for coping with life stress, and the use of effective coping can ultimately reduce decisional conflict in survivorship care. How close and flexible the family members are and how family members communicate with one another in stressful situations may be associated with how they cope with their problems, producing either decisional conflicts or satisfaction in survivorship care. As suggested in the Typology Model, family functioning may be an important component of family contexts, which is required to maintain the balance between demands and capabilities. The current study suggests that families that are flexible in modifying their daily tasks with strong family bonds and that communicate with one another more effectively may enhance survivors’ ability to alleviate the impacts of life stress.
The moderating effect of reliance on formal and informal resources in the adjustment process was observed for cancer survivors. In fact, cancer survivors may use diverse resources to solve their problems and to ultimately improve their quality of life. Although the use of specific resources may be dependent on survivors’ needs or problems, cancer survivors may have preferences, such as inclinations toward informal or formal social ties. The current study found that almost half of the respondents preferred either informal or formal social ties when making healthcare decisions. In addition, this study’s findings demonstrated that the adjustment process of survivors varied according to their resources. For example, the informal reliance group showed that family coping was negatively associated with decisional conflict, whereas their relationships were not found in the formal group. Survivors who rely on informal resources may seek active coping mechanisms to reduce decisional conflict in survivorship care. However, for the formal group, family coping was not a key factor that influenced decisional conflict. A possible explanation is that survivors who rely on formal resources may have a lower level of intimacy in family relationships or may not communicate effectively with family members.
Limitations
This study has several limitations. For example, the findings may not be generalizable to all cancer survivors. The number of African Americans in this study was too small to report, and other ethnic groups (i.e., Latina, other Asian ethnic subgroups) were not included. In addition, the current study is based on a cross-sectional design, and causality cannot be assumed. The data were collected by participants’ self-reports, and questions during the treatment period may have been influenced by recall biases. Although this study focused on the family context, it featured only cancer survivors. Future studies should include family members to enhance understanding of family functioning and coping in making healthcare decisions.
Implications for Nursing
The current study increases knowledge of the relationships among family contexts and decisional conflict for cancer survivors under the Typology Model and the CTM. The study findings draw attention to the importance of nurses and other medical practitioners to attend to the family context in cancer survivorship care. From a clinical perspective, this study suggests that the role of the family context, which includes family functioning and coping, on decisional conflict may be important in the adjustment process to make high-quality decisions in cancer survivorship care. The current study also highlights the role of informal social ties when making decisions, which can positively influence the adjustment process. Family intervention or therapy may be effective to achieve a balance between family flexibility and coherence and to effectively communicate with family members to reduce decisional conflict. In addition, efforts to encourage and support family involvement in the decision-making process are necessary to enhance cancer survivors’ adjustment process. For example, family members who maintain good relationships with healthcare professionals may encourage cancer survivors to get routine cancer screening tests or visit a doctor for certain health-risk conditions at an appropriate time.
In terms of future research, the findings support the need to examine the impact of the family context on decisional conflict among a large multiethnic, population-based cohort of cancer survivors. The findings also highlight the need for more research on changes in the decision-making process from the active treatment phase through long-term survivorship. Such research would be helpful for healthcare professionals to encourage, inspire, and guide patients and family members to make the best decisions throughout the cancer journey.
Conclusion
The role of the family context on decisional conflict is important in the adjustment process to make good decisions in cancer survivorship care. Findings present nursing practice and research implications that highlight the need for efforts to encourage and support family involvement in the decision-making process and to enhance cancer survivors’ adjustment.
References
Abrahamson, K., Durham, M., & Fox, R. (2010). Managing the unmet psychosocial and information needs of patients with cancer. Patient Intelligence, 2, 45–52. doi:10.2147/pi.s9442
Andersen, M.R., Bowen, D.J., Morea, J., Stein, K.D., & Baker, F. (2009). Involvement in decision-making and breast cancer survivor quality of life. Health Psychology, 28, 29–37. doi:10.1037/0278-6133.28.1.29
Ashing-Giwa, K.T., Padilla, G.V., Tejero, J.S., & Kim, J. (2004). Breast cancer survivorship in a multiethnic sample: Challenges in recruitment and measurement. Cancer, 101, 450–465. doi:10.1002/cncr.20370
Bentler, P.M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. doi:10.1037/0033-2909.107.2.238
Blank, T., Graves, K., Sepucha, K., & Llewellyn-Thomas, H. (2006). Understanding treatment decision making: Contexts, commonalities, complexities, and challenges. Annals of Behavioral Medicine, 32, 211–217. doi:10.1207/s15324796abm3203_6
Bollen, K.A. (1989). Structural equations with latent variables. New York, NY: John Wiley and Sons, Inc.
Curran, D. (1983). Traits of a healthy family. Minneapolis, MN: Winston Press.
David, D., Montgomery, G.H., & Bovbjerg, D.H. (2006). Relations between coping responses and optimism-pessimism in predicting anticipatory psychological distress in surgical breast cancer patients. Personality and Individual Differences, 40, 203–213. doi:10.1016/j.paid.2005.05.018
Davison, B.J., Goldenberg, S.L., Gleave, M.E., & Degner, L.F. (2003). Provision of individualized information to men and their partners to facilitate treatment decision making in prostate cancer. Oncology Nursing Forum, 30, 107–114. doi:10.1188/03.ONF.107-114
Deimling, G.T., Smerglia, V.L., & Schaefer, M.L. (2001). The impact of family environment and decision-making satisfaction on caregiver depression: A path analytic model. Journal of Aging and Health, 13, 47–71. doi:10.1177/089826430101300103
Folkman, S., & Moskowitz, J.T. (2004). Coping: Pitfalls and promise. Annual Review of Psychology, 55, 745–774. doi:10.1146/annurev.psych.55.090902.141456
Gillis, J.S. (1993). Effects of life stress and dysphoria on complex judgments. Psychological Reports, 72, 1355–1363. doi:10.2466/pr0.1993.72.3c.1355
Haq, R., Heus, L., Baker, N.A., Dastur, D., Leung, F.H., Leung, E.,. . . Parsons, J.A. (2013). Designing a multifaceted survivorship care plan to meet the information and communication needs of breast cancer patients and their family physicians: Results of a qualitative pilot study. BMC Medical Informatics and Decision Making, 13, 76. doi:10.1186/1472-6947-13-76
Horn, J.L., & McArdle, J.J. (1992). A practical and theoretical guide to measurement invariance in aging research. Experimental Aging Research, 18, 117–144. doi:10.1080/03610739208253916
Hudson, S.V., Miller, S.M., Hemler, J., Ferrante, J.M., Lyle, J., Oeffinger, K.C., & Dipaola, R.S. (2012). Adult cancer survivors discuss follow-up in primary care: ‘Not what I want, but maybe what I need.’ Annals of Family Medicine, 10, 418–427. doi:10.1370/afm.1379
Janis, I.L., & Mann, L. (1977). Decision making: A psychological analysis of conflict, choice, and commitment. New York, NY: Free Press.
Jansen, S.J., Otten, W., & Stiggelbout, A.M. (2006). Factors affecting patients’ perceptions of choice regarding adjuvant chemotherapy for breast cancer. Breast Cancer Research and Treatment, 99, 35–45. doi:10.1007/s10549-006-9178-z
Kerstholt, J.H. (1994). The effect of time pressure on decision making behavior in a dynamic task environment. Acta Psychologica, 84, 89–104. doi:10.1016/0001-6918(94)90013-2
Kline, R.B. (1998). Principles and practice of structural equation modeling. New York, NY: Guilford Press.
Kowalski-Trakofler, K.M., Vaught, C., & Scharf, T. (2003). Judgment and decision making under stress: an overview for emergency managers. International Journal of Emergency Management, 1, 278–289. doi:10.1504/IJEM.2003.003297
LeBlanc, A., Kenny, D.A., O’Connor, A.M., & Légaré, F. (2009). Decisional conflict in patients and their physicians: A dyadic approach to shared decision making. Medical Decision Making, 29, 61–68. doi:10.1177/0272989X08327067
Lim, J.W., & Ashing-Giwa, K.T. (2013). Is family functioning and communication associated with health-related quality of life for Chinese- and Korean-American breast cancer survivors? Quality of Life Research, 22, 1319–1329. doi:10.1007/s11136-012-0247-y
Lim, J.W., & Paek, M.S. (2013). The relationship between communication and health-related quality of life in survivorship care for Chinese-American and Korean-American breast cancer survivors. Supportive Care in Cancer, 21, 1157–1166. doi:10.1007/s00520-012-1641-2
Lim, J.W., Shon, E.J., Paek, M., & Daly, B. (2014). The dyadic effects of coping and resilience on psychological distress for cancer survivor couples. Supportive Care in Cancer, 22, 3209–3217. doi:10.1007/s00520-014-2334-9
Lim, J.W., & Townsend, A. (2012). Cross-ethnicity measurement equivalence of family coping for breast cancer survivors. Research on Social Work Practice, 22, 689–703. doi:10.1177/1049731512448933
Lingler, J.H., Sherwood, P.R., Crighton, M.H., Song, M.K., & Happ, M.B. (2008). Conceptual challenges in the study of caregiver-care recipient relationships. Nursing Research, 57, 367–372. doi:10.1097/01.NNR.0000313499.99851.0c
McCubbin, H.I., Larsen, A., & Olson, D. (1987). Family crisis orientated personal evaluation scales (F COPES). In H.I. McCubbin & A.I. Thompson (Eds.), Family assessment inventories for research and practice (pp. 193–207). Madison, WI: University of Wisconsin-Madison.
McCubbin, H.I., & McCubbin, M.A. (1988). Typologies of resilient families: Emerging roles of social class and ethnicity. Family Relations, 37, 247–254. doi:10.2307/584557
Meredith, W. (1993). Measurement invariance, factor analysis and factorial invariance. Psychometrika, 58, 525–543.
Michael, N., O’Callaghan, C., Baird, A., Hiscock, N., & Clayton, J. (2014). Cancer caregivers advocate a patient- and family centered approach to advance care planning. Journal of Pain and Symptom Management, 47, 1064–1077. doi:10.1016/j.jpainsymman.2013.07.009
O’Connor, A.M. (1995). Validation of a decisional conflict scale. Medical Decision Making, 15, 25–30. doi:10.1177/0272989x9501500105
O’Connor, A.M., Légaré, F., & Stacey, D. (2003). Risk communication in practice: The contribution of decision aids. BMJ, 327, 736–740. doi:10.1136/bmj.327.7417.736
Olson, D.H. (1986). Circumplex Model VII: Validation studies and FACES III. Family Process, 25, 337–351. doi:10.1111/j.1545-5300.1986.00337.x
Olson, D.H. (2000). Circumplex Model of Martial and Family Sytems. Journal of Family Therapy, 22, 144–167. doi:10.1111/1467-6427.00144
Olson, D.H., Gorall, D.M., & Tiesel, J.W. (2004). FACES IV package. Minneapolis, MN: Life Innovations.
O’Rourke, M.E. (2001). Decision making and prostate cancer treatment selection: A review. Seminars in Oncology Nursing, 17, 108–117. doi:10.1053/sonu.2001.23076
Powazki, R.D. (2011). The family conference in oncology: Benefits for the patient, family, and physician. Seminars in Oncology, 38, 407–412. doi:10.1053/j.seminoncol.2011.03.011
Shin, D.W., Cho, J., Roter, D.L., Kim, S.Y., Sohn, S.K., Yoon, M.S., . . . Park, J.H. (2013). Preferences for and experiences of family involvement in cancer treatment decision-making: Patient-caregiver dyads study. Psycho-Oncology, 22, 2624–2631. doi:10.1002/pon.3339
Siminoff, L.A., Zyzanski, S.J., Rose, J.H., & Zhang, A.Y. (2008). The Cancer Communication Assessment Tool for Patients and Families (CCAT-PF): A new measure. Psycho-Oncology, 17, 1216–1224. doi:10.1002/pon.1350
Steiger, J.H. (1990). Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research, 25, 173–180.
Stinnett, H., & DeFrain, J. (1985). Secrets of strong families. Boston, MA: Little, Brown and Co.
About the Author(s)
Lim is an associate professor in the College of Social Welfare at Kangnam University in Yongin, South Korea, and Shon is a PhD candidate in the Jack, Joseph and Morton Mandel School of Applied Social Sciences at Case Western Reserve University in Cleveland, Ohio. No financial relationships to disclose. Lim contributed to the conceptualization and design and completed the data collection. Shon contributed to the analysis. Both authors provided statistical support and contributed to the manuscript preparation. Lim can be reached at jungwonlim@kangnam.ac.kr, with copy to editor at ONFEditor@ons.org. Submitted July 2015. Accepted for publication August 19, 2015.

