Hematopoietic Stem Cell Transplantation Recipient and Caregiver Factors Affecting Length of Stay and Readmission
Purpose/Objectives: To evaluate the contributions of patient and caregiver factors to length of stay (LOS) and 30-day readmission status for recipients of allogeneic hematopoietic stem cell transplantation (HSCT).
Design: Secondary data analysis from a phase 2 clinical trial.
Setting: National Institutes of Health Clinical Center in Bethesda, Maryland.
Sample: 68 dyads (N = 136) comprised of patients receiving HSCT and their caregivers.
Methods: Multiple linear regression and logistic regression analyses were used to investigate associations between caregiver and patient factors and outcomes.
Main Research Variables: Patients’ initial LOS, 30-day readmission, and demographic and disease characteristics; caregiver demographic factors, health problems, psychological distress, burden, and self-efficacy.
Findings: Twenty-five patients were readmitted within 30 days after hospital discharge following their initial hospitalization for HSCT. LOS was 34% longer for patients with infection than patients without infection. Patients with grade 2 or greater acute graft-versus-host disease (GVHD) stayed longer compared to patients with no or mild acute GVHD. Patients who had nonspousal caregivers stayed longer than patients with spousal caregivers. Infection was significantly related to readmission.
Conclusions: Knowledge regarding factors associated with increased LOS and 30-day readmission can help nurses and transplantation team members anticipate the healthcare needs of patients receiving HSCT, improve outcomes, and decrease the use of expensive health services.
Implications for Nursing: Educating patients and caregivers on infection prevention is critically important to reduce LOS and 30-day readmission after HSCT.
Jump to a section
The annual number of allogeneic hematopoietic stem cell transplantation (HSCT) recipients in the United States is steadily increasing. Multiple myeloma and lymphoma are associated with 56% of all HSCTs, whereas acute leukemia and myelodysplastic syndrome are the most common indications for allogeneic HSCT (D’Souza & Zhu, 2016). HSCT has the ability to cure a variety of diseases, but the procedure is associated with complications related to the donor type (autologous, related or unrelated allogeneic), pretransplantation conditioning regimen (full- or reduced-intensity myeloablation), and the source of stem cells (bone marrow, peripheral blood cells, or cord blood cells) (Rimkus, 2009). In the first 100 days after transplantation, the patient can experience symptoms such as fatigue and diarrhea, as well as life-threatening complications such as infection, graft-versus-host disease (GVHD), and organ failure (Arnaout et al., 2014; Bevans, Mitchell, & Marden, 2008). The number of complications, increased mortality risk, and altered immune function contribute to the complexity of the procedure and care plan.
The success of HSCT depends on multiple factors, including the quality of care that a patient receives and the timely management of complications. Therefore, transplantation centers often require a caregiver to become involved with the HSCT recipient’s care (Cooke, Grant, & Gemmill, 2012). Although “required,” the caregiver’s involvement and role changes across the HSCT trajectory. When the patient is an inpatient, the caregiver’s participation may vary. The caregiver’s role during the hospital stay includes psychological support, advocacy, and building skills related to medication administration, symptom management, and problem identification (Beattie & Lebel, 2011). In addition, the caregiver often has home-care duties to attend to—including those at a secondary/temporary residence close to the transplantation center—along with providing care for other family members (Bevans et al., 2008; Sabo, McLeod, & Couban, 2013). After discharge, the caregiver assumes responsibility 24 hours a day for symptom management in addition to monitoring for problems and coordination of care.
The burden of caregiving for a family member receiving an allogeneic HSCT has been shown to take a significant toll on the caregiver’s health (Beattie & Lebel, 2011; Sabo et al., 2013). Physical issues include fatigue, sleep disturbances, and sexual dysfunction, and psychological issues including emotional distress, fear, and relationship difficulties (Aslan, Sanisolu, Akyol, & Yetkin, 2009; Bevans & Sternberg, 2012; Fife, Monahan, Abonour, Wood, & Stump, 2009; Poloméni, Lapusan, Bompoint, Rubio, & Mohty, 2016; Wilson, Eilers, Heermann, & Million, 2009). A study by Poloméni et al. (2016) that explored the impact of allogeneic HSCT on patients’ and close relatives’ quality of life (QOL) revealed caregiver concerns regarding changes in marital and family dynamics and disruptions in daily routine tasks. In the study, caregivers showed worse overall results in their evaluation of QOL than the patients (Poloméni et al., 2016). The complexity and uncertainty associated with the transplantation process increases the level of distress for the patient and the caregiver (Wilson et al., 2009). In a critical review, Beattie and Lebel (2011) found female gender, elevated subjective burden, and higher patient symptom burden to be predictors of distress among caregivers. Caregivers often displayed distress levels that were comparable to or even higher than patients’ reported distress levels (Beattie & Lebel, 2011). A study by Bevans et al. (2016) indicated a higher level of perceived stress, anxiety, and depression scores among the caregivers of patients receiving HSCT compared with controls matched for age, gender, race, and ethnicity, illustrating the impact of HSCT on a caregiver’s psychological health. Another phenomenologic study (Sabo et al., 2013) suggested that spouses of patients receiving HSCT are at risk for adverse psychological effects, including distress and secondary traumatic stress one year before and after transplantation. Despite understanding the impact of allogeneic HSCT on the caregiver, little research has been done regarding the impact of the caregiver’s experience on the patient.
Length of stay (LOS) and hospital readmission rates are important proxies of patient acuity that lead to increased hospitalization costs and patient and family suffering (Bennett et al., 1995; Lee, Klar, Weeks, & Antin, 2000). LOS and readmission risk are influenced by patient factors, such as infection, unrelated donor status, total body irradiation-based conditioning, and GVHD status (Bejanyan et al., 2012; Faucher et al., 2012; Prieto et al., 2002; Spring et al., 2015).
Caregiver factors may also play a role in prolonging LOS and predisposing patients to unscheduled readmissions. Existing research has focused on caregivers of patients with cancer and the LOS of older adult patients. For patients with cancer, marital status or cohabitation with the caregiver, as well as continuity of caregivers, may improve outcomes (Pruthi, Lentz, Sand, Kouba, & Wallen, 2009). In the older adult patient population, high caregiver burden and perception of low self-competency prolong LOS (Wolff & Kasper, 2004). Caregiver age, number of caregivers, and geographic proximity of caregivers also contribute to prolonged LOS and hospital admission (Skinner, Tennstedt, & Crawford, 1994). Few studies have examined the influence of caregiver factors on the risk for readmission among patients receiving HSCT, with conflicting findings. According to Spring et al. (2015), having a child or nonrelative as a primary caregiver, versus a spouse or significant other, increased the risk of 30-day readmission. In contrast, Rauenzahn et al. (2014) found no significant association between social variables (e.g., caregiver relationship to the patient, number of caregivers) and the readmission risk for patients receiving HSCT.
Given the inadequacy of research investigating the relationship between caregiver factors and LOS and readmission, the current study was conducted to examine the impact of caregiver factors on these outcomes. The Model of Health Care Utilization, proposed by Andersen (1995), guided this study. According to the model, three components contribute to the use of health care: (a) predisposing factors (biologic and demographic factors), (b) enabling factors (community and caregiver support), and (c) need factors (functional status of the patient). The adapted model is presented in Figure 1. The objectives of the current study were to evaluate the contributions of caregiver factors to the LOS of patients receiving allogeneic HSCT while controlling for patient factors, and evaluate the contributions of caregiver factors to readmission status of patients receiving allogeneic HSCT within the first 30 days of discharge, controlling for patient factors. 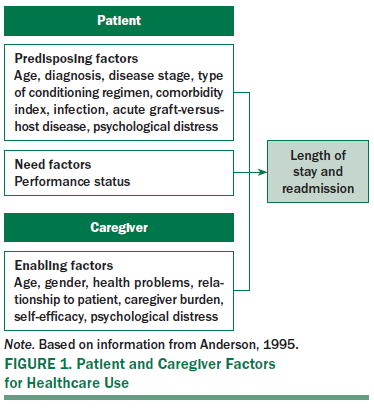
Methods
Data from a phase 2 clinical trial were used to examine the predictors of LOS and 30-day readmission following allogeneic HSCT (Bevans et al., 2014). The study used a prospective repeated design to test the efficacy of a problem-solving education intervention in caregivers of allogeneic HSCT recipients. The study was approved by the Institutional Review Board of the National Heart, Lung and Blood Institute. Data on HSCT recipients and caregivers were collected at three time points: pretransplantation, at the time of initial discharge from the inpatient setting (post-transplantation), and six weeks after initial discharge from the inpatient setting (Bevans et al., 2014). In the current analysis, pre-HSCT data were used to predict the LOS, and data collected at the time of initial discharge were used to predict the 30-day readmission status.
Participants
A sample of 68 dyads (N = 136) from a total of 151 patients and caregivers were included in this analysis (see Figure 2). Demographic information was described previously (Bevans et al., 2014). The primary caregiver for each patient was identified and self-reported at least six hours of support activities per day for the HSCT recipient. During the outpatient phase, HSCT recipients and their caregivers were required to find housing located within a one-hour commute of the transplantation center to facilitate attending clinic appointments an average of two times per week. Additional inclusion criteria for patients were (a) being a first-time allogeneic HSCT recipient, (b) being aged 18 years or older, (c) being able to provide informed consent, (d) being able to read and speak English, and (e) having an adult caregiver who was willing to participate in the study. All patients and caregivers gave informed written consent to participate in the study.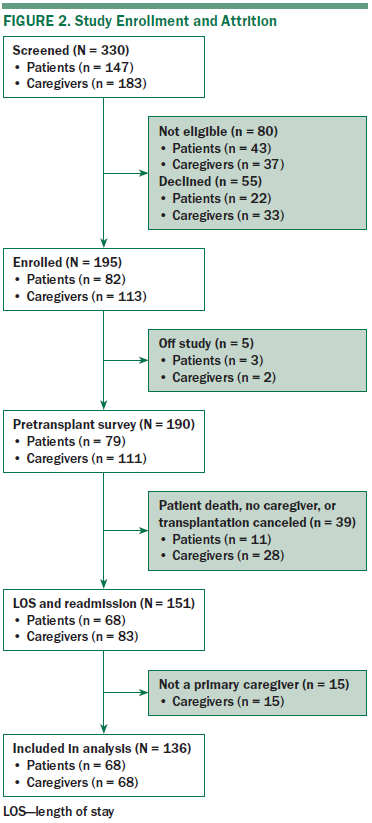
Measures
Initial LOS and 30-day readmission were collected from the electronic health record (EHR). LOS was defined as the number of overnight stays from the day of transplantation (day 0) until discharge from the hospital. Readmission was defined as admission to the hospital within 30 days of the patient being discharged from initial hospitalization.
Patient demographic and disease characteristics were conceptualized as predisposing factors and were collected from the EHR. These factors included age, diagnosis, disease stage, type of conditioning (reduced intensity or myeloablative), comorbidity index, acute GVHD grade, and infection status. Performance status of the patient at the time of transplantation was considered a “need” factor in the analyses. Caregiver characteristics were conceptualized as “enabling” factors and included demographics (age, gender, relationship to patient), health problems, psychological distress, caregiver burden, and self-efficacy. The caregiver factors and the self-report measures (patient and caregiver) were collected during the study visit using hard copy questionnaires.
The Brief Symptom Inventory (BSI-18), an 18-item self-report measure of psychological functioning, was used (Derogatis, 1993). Respondents rated each item on a five-point Likert-type scale, ranging from 0 (never) to 4 (extremely) based on the degree to which they were bothered during the previous seven days. Higher scores indicate a higher level of distress (range = 0–90). The scale had strong internal consistency, with a Cronbach alpha of 0.89 (Zabora, BrintzenhofeSzoc, Curbow, Hooker, & Piantadosi, 2001). In the current sample, the internal consistency for the total score was 0.88 for caregivers.
In addition, the Caregiver Reaction Assessment (CRA) scale was used to assess caregiver burden (Given et al., 1992). The CRA is a well-established scale with 24 items scored on a five-point Likert-type scale. Domains are caregiver self-esteem, family support, finances, schedule, and health. Scores range from 1 (strongly disagree) to 5 (strongly agree), with higher total CRA scores representing more burden. Construct validity has been supported through correlations with the Center for Epidemiologic Studies Depression Scale and the Activities of Daily Living Dependency Scale. The internal consistency in this study sample was 0.67.
The Cancer Self-Efficacy Scale–Transplant (CASE-T), a 17-item self-report measure, was used to assess self-efficacy (Lewis et al., 2008). The CASE-T determines a person’s confidence in managing the impact of the stem cell transplantation. The family caregiver-specific scale used statements such as, “I am confident that I can call on my inner strengths to pull myself through my family member’s transplant,” to measure caregiver self-efficacy. Responses range from 0 (not at all confident) to 10 (very confident). Higher scores (range = 0–170) represent a higher level of self-efficacy. The internal consistency reliability for the total CASE scale was 0.97 (Lewis et al., 2008), and the internal consistency of this sample for caregivers was 0.96.
Data Analysis
Exploratory data analyses were conducted to screen the data for outliers and missing values. Tests of assumptions for univariate and multivariate normality were conducted. Descriptive statistics were used for demographic characteristics (patients and caregivers), clinical characteristics, and LOS and 30-day readmission. Multiple linear regression analysis was used to examine the association between caregiver factors and LOS, and multiple logistic regression analysis was applied to investigate the association between caregiver factors and 30-day readmission. Because the distribution of LOS was skewed, it was log transformed to meet the assumptions of linear regression. Initial bivariate linear regression analyses were conducted to evaluate the contributions of individual predictors of LOS, and parallel logistic regression analyses were conducted to evaluate the contributions of the individual predictors to 30-day readmission. Pre-HSCT recipient and caregiver factors with p < 0.2 were entered, and variables that did not predict the outcome with this criterion were not retained for subsequent models. The most parsimonious models based on this hierarchical procedure are outlined in the results section. Data were analyzed with SPSS®, version 23.0.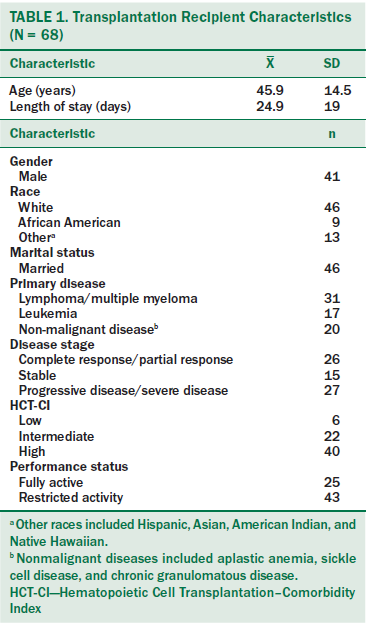
Results
A total of 68 patient–caregiver dyads were included in the final analysis. Demographic and clinical data for HSCT recipients are presented in Table 1. Table 2 shows the demographic characteristics of primary caregivers. 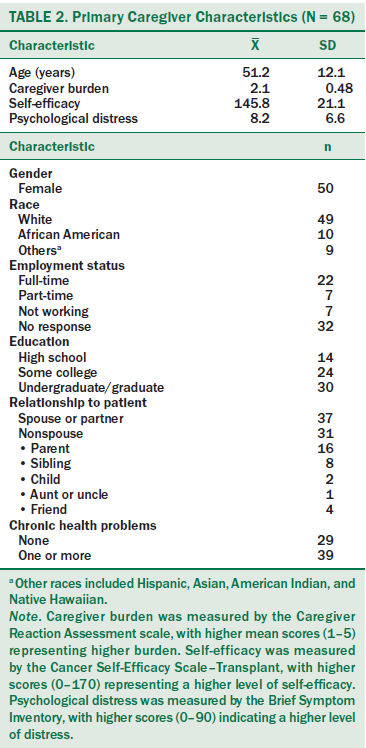
Initial Hospitalization Length of Stay
When controlling for patient’s age and caregiver relationship, infection status and acute GVHD status were significantly associated with LOS (see Table 3). LOS was 34% longer for patients with infection than patients without infection (p = 0.004). Compared to patients with no or mild acute GVHD, patients with grade 2 or greater acute GVHD stayed 58% longer (p < 0.001). When controlling for patient factors and adding caregiver psychological distress, the only caregiver factor that predicted the LOS was caregiver relationship to the patient. Patients who had nonspousal caregivers stayed 23% longer than patients with a spousal caregiver (p = 0.04).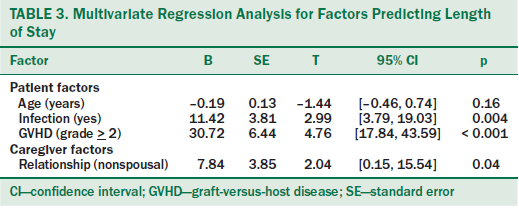
30-Day Readmission
Twenty-five (37%) of the patients were readmitted within 30 days of hospital discharge. Pre-HSCT factors were used to predict the readmission status, except for caregiver burden; discharge CRA scores for burden were included. No significant difference was noted in the BSI-18 (patient and caregiver) or CASE-T scores from pre-HSCT to discharge (Bevans et al., 2014). However, a significant difference was noted between caregiver burden scores from before transplantation to after discharge.
Logistic regression analysis was performed to assess the impact of patient and caregiver factors on the likelihood of an HSCT recipient’s readmission to the hospital (see Table 4). Caregiver factors did not affect readmission status. In multivariate analysis, documented infection status predicted 30-day readmission after controlling for patient and caregiver factors. Patients with infection were 16.8 times more likely to be readmitted to the hospital than those without infection (p < 0.001).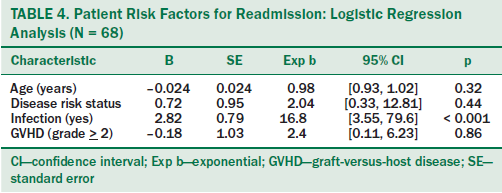
Infection Status
Because infection was found to be a significant predictor for both outcomes, additional descriptive analyses were performed (see Table 5). Infection status was measured by Common Toxicity Criteria for Adverse Events, as evidenced by the presence of one or more infections or the presence of febrile neutropenia (FN) during initial hospitalization, following discharge, and through readmission within 30 days. During the initial LOS, 29% of patients had FN, 15% had central venous catheter-related bacterial infection, and 32% had non–catheter-related bacterial infection. Among the patients who were readmitted within 30 days of initial hospital stay, FN was present in 16% of patients. Fifteen percent of patients had non–catheter-related bacterial infections, whereas 9% had central venous catheter-related bacterial infections. The primary sites of non–catheter-related infections were the stool, sinuses, and lung.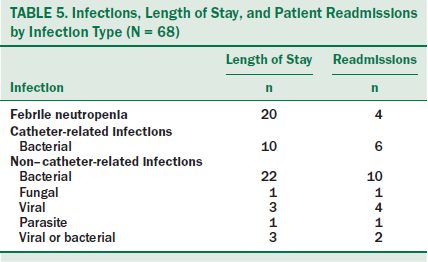
Discussion
This study is one of the first to examine the influence of informal caregiver characteristics on hospitalization for HSCT recipients. First, the findings of this study suggested an association between caregiver relationship and HSCT recipient’s LOS, indicating a shorter LOS for patients with spousal caregivers. This finding corroborates previous research that examined the impact of marital status on patient outcomes (Kelly, Sharp, Dwane, Kelleher, & Comber, 2012; Pruthi et al., 2009). Kelly et al. (2012) examined the factors associated with LOS in patients undergoing colorectal resection and found a shorter LOS among married patients. The investigators pointed out how a lack of social support among unmarried patients may be a contributing factor. Although, in a sample of patients with acute leukemia, social problems accounted for only 2% of avoidable hospital readmissions (El-Jawahri et al., 2016), the impact during initial hospitalization is unknown. Factors associated with a partnered relationship, including the postdischarge environment and a shared sense of life’s meaning and purpose, should be explored.
None of the caregiver factors in the current study were significantly associated with 30-day readmission. This finding is consistent with Rauenzahn et al. (2014), where the number of caregivers and the type of caregiver (e.g., spouse) were not significantly related to readmission in a multivariate model. Although the caregiver is instrumental in the patient’s discharge planning and outpatient care, the post-HSCT complications are often numerous and a strong predictor of hospital readmission.
The authors’ finding of prolonged LOS among patients with acute GVHD support results from two previous studies (Liu et al., 2011; Prieto et al., 2002). Those studies showed a significant association between acute GVHD (grades 1–4) and increased LOS among HSCT recipients. In addition, the findings from the current study revealed a longer LOS for those with infection that is consistent with findings from previous research among allogeneic HSCT recipients (Liu et al., 2011; Menzin et al., 2011; Poutsiaka et al., 2007). A significantly increased LOS was noted in Liu et al. (2011) for HSCT recipients with bloodstream infections (BSI). Poutsiaka et al. (2007) evaluated the relationship between BSI and LOS and mortality. The median LOS for HSCT recipients who did not develop BSI was 19 days, compared to 25 days for patients who did develop BSI. Menzin et al. (2011) compared the impact of invasive fungal infections in high-risk patients across many conditions and concluded that fungal infections have a major impact on a transplantation recipient’s LOS and mortality. Despite the advancements in the management of HSCT recipients, infection remains as a major complication. Using new immunosuppressive therapies and prophylactic antibiotic/antifungal treatments may reduce the risk of infection (Kim, Baek, & Min, 2012). However, adherence to the treatment plan and management of side effects are an essential aspect of the caregiver’s role. Using strategies and guidelines as ways to prevent infection, such as early identification and effective management of infectious complications, can help caregivers improve patient outcomes and reduce morbidity and mortality.
In the current study, presence of infection was significantly related to 30-day readmission, which supports previous reports. Bejanyan et al. (2012) listed infection as a major risk factor for 30-day readmission after controlling for a patient’s demographic, disease, and transplantation characteristics. A study conducted by Spring et al. (2015) also documented that infection during hospitalization was a significant predictor of readmission at 30 days and 100 days. Rauenzahn et al. (2014) examined the predictors and impact of 30-day readmission on patient outcomes and healthcare costs. In that study, documented infection during index hospitalization affected the 30-day risk of readmission. Thirty-day readmission was, in turn, significantly associated with 100-day readmission and increased healthcare costs.
Several factors could be involved in these findings. Allogeneic HSCT recipients are at higher risk for complications, such as infection, organ failure, and GVHD, than those undergoing autologous transplantation (Grant, Cooke, Bhatia, & Forman, 2005). Many caregivers report being ill-prepared for the complex and extended role of a transplantation caregiver (Metoyer, 2013).
Limitations
This study had several limitations. The study had a relatively small sample size and the primary study enrolled only allogeneic HSCT recipients and their caregivers. In addition, the primary study included an intervention, which might have influenced outcome variables; therefore, only baseline data from patients and caregivers (preintervention) were used.
Implications for Nursing Practice and Research
Understanding the contribution of the patients’ clinical factors as well as the caregivers’ factors to major outcomes, such as LOS and readmission, is critical. Family caregivers are assuming greater responsibility to ensure quality care is delivered and maintained. The findings from this study suggest that, when a nonspousal caregiver is identified for a patient preparing to undergo HSCT, a more in-depth assessment may be needed to understand the relationship and its potential impact on the discharge environment. In addition, how nurses provide education and evaluate the knowledge and skill of an HSCT recipient and caregiver is critical (Cooke et al., 2012). Establishing a standardized approach to the education of HSCT recipients and their caregivers from a dyadic perspective may create a shared understanding of the expectations associated with quality outcomes.
Future research can attempt to replicate the findings from this study in other HSCT recipients and caregivers. Although prospective data collection is optimal, databases from other sources with more heterogeneity in the HSCT populations could be explored. Future studies should include socioeconomic factors (e.g., education, insurance, caregiver employment, social support) that may influence readmission status. Specific attention to the differences between partnered and nonpartnered (e.g., parent, friend) relationships and how those differences affect patient outcomes would be valuable.
For HSCT recipients, 100 days post-transplantation is an important marker. During this period, both caregivers and patients are expected to assume the responsibility of managing the physical and psychological consequences of transplantation. The 30-day readmission variable was used in the current study because of its relevance as a quality-of-care indicator after discharge from an index hospitalization. Exploring the influence of caregiver factors on 100-day readmission rates could reveal a possible association between caregiver factors and the readmission risk.
Conclusion
This study contributes to the knowledge of the factors that may be associated with increased LOS and 30-day readmission rates. With this knowledge, nurses and transplantation team members can better anticipate the needs of HSCT recipients, which may lead to an improvement in healthcare outcomes and decrease the use of expensive health services.
The authors gratefully acknowledge Stephen Klagholz, BS, Li Yang, MS, Deborah Kolakowski, DNP, RN, and Sue Johnson, BSN, for their invaluable support of this work and analysis.
About the Author(s)
Sundaramurthi is a senior clinical research nurse and Wehrlen is a senior nurse consultant, both in the Nursing Department at the National Institutes of Health Clinical Center in Bethesda, MD; Friedman is an associate dean of research and professor and Thomas is a professor emeritus, both in the School of Nursing at the University of Maryland in Baltimore; and Bevans is a nurse researcher in the Nursing Department at the National Institutes of Health Clinical Center. This research was funded by the Intramural Research Program of the National Institutes of Health, Clinical Center (Clinical Trials Identifier: NCT00766883—Problem-Solving Education for Caregivers and Patients During Stem Cell Transplant). Sundaramurthi, Wehrlen, Friedman, and Bevans provided statistical support and the analysis. Sundaramurthi, Wehrlen, and Bevans completed the data collection. All authors contributed to the conceptualization and design and manuscript preparation. Sundaramurthi can be reached at sundaramurthit@gmail.com, with copy to editor at ONFEditor@ons.org. Submitted December 2016. Accepted for publication February 27, 2017.
References
Andersen, R.M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36, 1–10.
Arnaout, K., Patel, N., Jain, M., El-Amm, J., Amro, F., & Tabbara, I.A. (2014). Complications of allogeneic hematopoietic stem cell transplantation. Cancer Investigation, 32, 349–362. doi:10.3109/07357907.2014.919301
Aslan, O., Sanisolu, Y., Akyol, M., & Yetkin, S. (2009). Quality of sleep in Turkish family caregivers of cancer patients. Cancer Nursing, 32, 370–377. doi:10.1097/NCC.0b013e3181a87fb9
Beattie, S., & Lebel, S. (2011). The experience of caregivers of hematological cancer patients undergoing a hematopoietic stem cell transplant: A comprehensive literature review. Psycho-Oncology, 20, 1137–1150. doi:10.1002/pon.1962
Bejanyan, N., Bolwell, B.J., Lazaryan, A., Rybicki, L., Tench, S., Duong, H., . . . Copelan, E.A. (2012). Risk factors for 30-day hospital readmission following myeloablative allogeneic hematopoietic cell transplantation (allo-HCT). Biology of Blood and Marrow Transplantation, 18, 874–880. doi:10.1016/j.bbmt.2011.10.032
Bennett, C.L., Armitage, J.L., Armitage, G.O., Vose, J.M., Bierman, P.J., Armitage, J.O., & Anderson, J.R. (1995). Costs of care and outcomes for high-dose therapy and autologous transplantation for lymphoid malignancies: Results from the University of Nebraska 1987 through 1991. Journal of Clinical Oncology, 13, 969–973. doi:10.1200/JCO.1995.13.4.969
Bevans, M., & Sternberg, E.M. (2012). Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. JAMA, 307, 398–403. doi:10.1001/jama.2012.29
Bevans, M., Wehrlen, L., Castro, K., Prince, P., Shelburne, N., Soeken, K., . . . Wallen, G.R. (2014). A problem-solving education intervention in caregivers and patients during allogeneic hematopoietic stem cell transplantation. Journal of Health Psychology, 19, 602–617. doi:10.1177/1359105313475902
Bevans, M.F., Mitchell, S.A., & Marden, S. (2008). The symptom experience in the first 100 days following allogeneic hematopoietic stem cell transplantation (HSCT). Supportive Care in Cancer, 16, 1243–1254. doi:10.1007/s00520-008-0420-6
Bevans, M.F., Ross, A., Wehrlen, L., Klagholz, S.D., Yang, L., Childs, R., . . . Pacak, K. (2016). Documenting stress in caregivers of transplantation patients: Initial evidence of HPA dysregulation. Stress, 19, 175–184. doi:10.3109/10253890.2016.1146670
Cooke, L., Grant, M., & Gemmill, R. (2012). Discharge needs of allogeneic transplantation recipients [Online exclusive]. Clinical Journal of Oncology Nursing, 16, E142–E149. doi:10.1188/12.CJON.E142-E149
Derogatis, L.R. (1993). Brief Symptom Inventory (BSI): Administration, scoring, and procedures manual (3rd ed.). Minneapolis, MN: National Computer Systems.
D’Souza, A., & Zhu, X. (2016). Current uses and outcomes of hematopoietic cell transplantation (HCT): 2016 summary slides. Retrieved from http://bit.ly/2uY5QcC
El-Jawahri, A., Keenan, T., Abel, G.A., Steensma, D.P., LeBlanc, T.W., Chen, Y.B., . . . Temel, J.S. (2016). Potentially avoidable hospital admissions in older patients with acute myeloid leukaemia in the USA: A retrospective analysis. Lancet Haematology, 3, E276–E283. doi:10.1016/s2352-3026(16)30024-2
Faucher, C., Le Corroller Soriano, A.G., Esterni, B., Vey, N., Stoppa, A.M., Chabannon, C., . . . Blaise, D. (2012). Randomized study of early hospital discharge following autologous blood SCT: Medical outcomes and hospital costs. Bone Marrow Transplantation, 47, 549–555. doi:10.1038/bmt.2011.126
Fife, B.L., Monahan, P.O., Abonour, R., Wood, L.L., & Stump, T.E. (2009). Adaptation of family caregivers during the acute phase of adult BMT. Bone Marrow Transplant, 43, 959–966. doi:10.1038/bmt.2008.405
Given, C.W., Given, B., Stommel, M., Collins, C., King, S., & Franklin, S. (1992). The Caregiver Reaction Assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Research Nursing and Health, 15, 271–283.
Grant, M., Cooke, L., Bhatia, S., & Forman, S.J. (2005). Discharge and unscheduled readmissions of adult patients undergoing hematopoietic stem cell transplantation: Implications for developing nursing interventions [Online exclusive]. Oncology Nursing Forum, 32, E1–E8. doi:10.1188/04.ONF.E1-E8
Kelly, M., Sharp, L., Dwane, F., Kelleher, T., & Comber, H. (2012). Factors predicting hospital length-of-stay and readmission after colorectal resection: A population-based study of elective and emergency admissions. BMC Health Services Research, 12, 77. doi:10.1186/1472-6963-12-77
Kim, S., Baek, J., & Min, H. (2012). Effects of prophylactic hematopoietic colony stimulating factors on stem cell transplantations: Meta-analysis. Archives of Pharmacal Research, 35, 2013–2020. doi:10.1007/s12272-012-1119-2
Lee, S.J., Klar, N., Weeks, J.C., & Antin, J.H. (2000). Predicting costs of stem-cell transplantation. Journal of Clinical Oncology, 18, 64–71. doi:10.1200/JCO.2000.18.1.64
Lewis, F.M., Cochrane, B.B., Fletcher, K.A., Zahlis, E.H., Shands, M.E., Gralow, J.R., . . . Schmitz, K. (2008). Helping her heal: A pilot study of an educational counseling intervention for spouses of women with breast cancer. Psycho-Oncology, 17, 131–137. doi:10.1002/pon.1203
Liu, H., Rich, E.S., Godley, L., Odenike, O., Joseph, L., Marino, S., . . . van Besien, K. (2011). Reduced-intensity conditioning with combined haploidentical and cord blood transplantation results in rapid engraftment, low GVHD, and durable remissions. Blood, 118, 6438–6445. doi:10.1182/blood-2011-08-372508
Menzin, J., Meyers, J.L., Friedman, M., Korn, J.R., Perfect, J.R., Langston, A.A., . . . Papadopoulos, G. (2011). The economic costs to United States hospitals of invasive fungal infections in transplant patients. American Journal of Infection Control, 39(4), E15–E20. doi:10.1016/j.ajic.2010.06.009
Metoyer, L.J. (2013). Education of hematopoietic stem cell transplant caregivers in preparation for their role. Journal of the Advanced Practitioner in Oncology, 4, 432–437.
Nijboer, C., Triemstra, M., Tempelaar, R., Sanderman, R., & van den Bos, G.A. (1999). Measuring both negative and positive reactions to giving care to cancer patients: Psychometric qualities of the Caregiver Reaction Assessment (CRA). Social Science and Medicine, 48, 1259–1269.
Poloméni, A., Lapusan, S., Bompoint, C., Rubio, M.T., & Mohty, M. (2016). The impact of allogeneic-hematopoietic stem cell transplantation on patients’ and close relatives’ quality of life and relationships. European Journal of Oncology Nursing, 21, 248–256. doi:10.1016/j.ejon.2015.10.011
Poutsiaka, D.D., Price, L.L., Ucuzian, A., Chan, G.W., Miller, K.B., & Snydman, D.R. (2007). Blood stream infection after hematopoietic stem cell transplantation is associated with increased mortality. Bone Marrow Transplantation, 40, 63–70.
Prieto, J.M., Blanch, J., Atala, J., Carreras, E., Rovira, M., Cirera, E., & Gastó, C. (2002). Psychiatric morbidity and impact on hospital length of stay among hematologic cancer patients receiving stem-cell transplantation. Journal of Clinical Oncology, 20, 1907–1917. doi:10.1200/JCO.2002.07.101
Pruthi, R.S., Lentz, A.C., Sand, M., Kouba, E., & Wallen, E.M. (2009). Impact of marital status in patients undergoing radical cystectomy for bladder cancer. World Journal of Urology, 27, 573–576. doi:10.1007/s00345-009-0380-6
Rauenzahn, S., Truong, Q., Cumpston, A., Goff, L., Leadmon, S., Evans, K., . . . Kanate, A.S. (2014). Predictors and impact of thirty-day readmission on patient outcomes and health care costs after reduced-toxicity conditioning allogeneic hematopoietic cell transplantation. Biology of Blood and Marrow Transplantation, 20, 415–420. doi:10.1016/j.bbmt.2013.12.559
Rimkus, C. (2009). Acute complications of stem cell transplant. Seminars in Oncology Nursing, 25, 129–138.
Sabo, B., McLeod, D., & Couban, S. (2013). The experience of caring for a spouse undergoing hematopoietic stem cell transplantation: Opening Pandora’s box. Cancer Nursing, 36, 29–40. doi:10.1097/NCC.0b013e31824fe223
Skinner, K.M., Tennstedt, S.L., & Crawford, S.L. (1994). Do characteristics of informal caregivers affect the length of hospital stay for frail elders? Journal of Aging and Health, 6, 255–269.
Spring, L., Li, S., Soiffer, R.J., Antin, J.H., Alyea, E.P., 3rd, & Glotzbecker, B. (2015). Risk factors for readmission after allogeneic hematopoietic stem cell transplantation and impact on overall survival. Biology of Blood and Marrow Transplantation, 21, 509–516.
Wilson, M.E., Eilers, J., Heermann, J.A., & Million, R. (2009). The experience of spouses as informal caregivers for recipients of hematopoietic stem cell transplants. Cancer Nursing, 32(3), E15–E23. doi:10.1097/NCC.0b013e31819962e0
Wolff, J.L., & Kasper, J.D. (2004). Informal caregiver characteristics and subsequent hospitalization outcomes among recipients of care. Aging Clinical and Experimental Research, 16, 307–313.
Zabora, J., BrintzenhofeSzoc, K., Curbow, B., Hooker, C., & Piantadosi, S. (2001). The prevalence of psychological distress by cancer site. Psycho-Oncology, 10, 19–28.

