Oncology Nurses’ Knowledge, Confidence, and Practice in Addressing Caregiver Strain and Burden
Objectives: To describe nurses’ practices, confidence, and knowledge of evidence-based interventions for cancer caregiver strain and burden and to identify factors that contribute to these aspects.
Sample & Setting: 2,055 Oncology Nursing Society members completed an emailed survey.
Methods & Variables: Pooled analysis of survey results. Variables included the baseline nursing assessment, intervention, confidence, knowledge, strategies used, and barriers encountered.
Results: Nurses tend to overestimate the strength of evidence for interventions not shown to be effective and have moderate confidence in assessing and intervening with caregivers. Having been an informal caregiver and having received care from an informal caregiver were associated with higher reported practice and confidence. Major strategies used were referral to social workers and others. Barriers reported were financial, caregiver emotional responses, and distance.
Implications for Nursing: An opportunity exists to increase nurses’ knowledge and confidence in assessment and intervention with caregivers. Greater use of technology may help nurses overcome some barriers to working with caregivers. Findings can be used to plan continuing education, develop clinical processes, and identify resources nurses need to address strain and burden among informal caregivers.
Jump to a section
Family caregivers are long-term care providers for people with cancer and an important extension of the cancer care workforce. Caregivers communicate with healthcare providers about patients’ health, monitor the severity of their condition, provide hands-on care, and advocate on behalf of patients. Research has indicated that caregiving is an intense experience that can be physically and emotionally demanding, and the proportion of cancer caregivers who report high levels of stress is higher than that of non-cancer caregivers (National Alliance for Caregiving, 2016). Although family caregivers play a central role in helping patients, demands on caregivers that exceed their resources can lead to strain and burden (Honea et al., 2008). Caregiver strain and burden is a construct that “encompasses difficulties assuming and functioning in the caregiver role as well as associated alterations in the caregiver’s emotional and physical health that can occur when care demands exceed resources” (Oncology Nursing Society [ONS], 2017, para. 1). According to a national survey by the National Alliance for Caregiving (2016), 62% of caregivers of patients with cancer reported high burden situations, averaging 33 hours of care per week, and 43% of caregivers provided complex medical or nursing tasks for which they had no preparation (National Alliance for Caregiving, 2016). High caregiver burden needs to be addressed because it can have detrimental effects on caregivers’ health (National Alliance for Caregiving, 2016; Stenberg, Ruland, & Miaskowski, 2010), hinder caregivers’ ability to help patients (Havyer, van Ryn, Wilson, & Griffin, 2017), and negatively affect patients’ mental and physical health (Boele et al., 2017; Kershaw et al., 2015).
The caregiver’s need for help is often overlooked. According to the National Alliance for Caregiving (2016), 40% of the caregivers wanted more help managing their own emotional and physical stress, but only 29% of the caregivers reported discussing these needs with a healthcare professional. Unmet caregiver needs for help contribute to overall strain and burden. A meta-analysis of caregiver studies indicated that caregivers of patients with cancer reported less caregiver burden, distress, and anxiety, as well as higher self-efficacy, coping, and quality of life, after receiving interventions that provided information and support (Northouse, Katapodi, Song, Zhang, & Mood, 2010). The National Alliance for Caregiving (2016) also reported that greater dissemination and implementation of evidence-based support interventions are needed to help those who experience high caregiver burden.
Because of their proximity to patients and caregivers in practice settings, nurses are in a unique position to assess caregiver burden and to provide evidence-based interventions (Honea et al., 2008). Nurses and caregivers also have overlapping goals to provide optimal physical and emotional care to patients with cancer. However, little is known about the extent to which nurses assess and intervene to address caregiver needs. In addition, not much is known about the barriers that nurses face when providing assistance to caregivers. The purpose of the current study was to describe nurses’ practices, confidence, and knowledge of evidence-based interventions for cancer caregiver burden and strain and to identify factors that contribute to these aspects of nursing care.
Methods
From 2013–2016, investigators at ONS implemented a two-phase project to test a targeted email dissemination of evidence to ONS members regarding caregiver strain and burden. The study was approved by the University of Pittsburgh Institutional Review Board and was given exempt status. The project employed a pre-/post-test design to examine the effects of a targeted email dissemination of evidence. As part of this project, society members were surveyed regarding knowledge, practices, and confidence in dealing with caregiver strain and burden. Participation was voluntary, and informed consent was implied by participants’ completion of the survey. This article specifically addresses findings about nurses’ practice in assessment, frequency of intervention, confidence, and knowledge of evidence regarding interventions for caregiver strain and burden from a pooled analysis of surveys that were completed prior to the email intervention. Pre-/post-test findings and details of the email intervention will be reported elsewhere.
Sample
The study sample was obtained by identifying members in the ONS database who met the following inclusion criteria: RNs or advanced practice RNs who were employed full- or part-time in a functional area identified as patient care and who had a valid email address. Members were excluded if they were international members or if their primary setting was pediatrics, to reduce variability that could result from such differences in setting and culture.
Measurement
The survey was constructed with input from members of an advisory council composed of nurse scientists with expertise and published research in caregiver strain and burden and evidence dissemination, and expertise in survey design and analysis, based on a review of the caregiving cancer research literature. The survey consisted of 32 items designed to identify nurses’ practice and confidence in conducting caregiver assessment and intervention and nurses’ knowledge of evidence-based interventions to address caregiver strain and burden. The survey invitation included a definition of caregiver strain and burden. Nurses indicated the frequency that they assessed and intervened with caregivers on 100-point numeric scale, representing the percentage of cases (0%–100%) in which they carried out those practices. Nurses rated their confidence in assessing and intervening with caregivers on a scale from 0 (not at all confident) to 100 (completely confident).
The current authors evaluated nurses’ knowledge by asking them to identify which interventions were supported by strong evidence according to the ONS Putting Evidence Into Practice (PEP) resources on the ONS website (ONS, 2017). Participants were provided with a set of interventions, some that were supported by evidence (e.g., psychoeducation) and some that were not supported by evidence (e.g., journaling), and were asked to identify those that were likely to be effective or recommended for practice according to the ONS PEP resources. Responses were scored as 1 (correct) or 0 (incorrect). Total scores were calculated, and the total percent age of correct knowledge scores was used in analysis.
Respondents also were asked if they had ever been an informal caregiver and if they had ever received care from an informal caregiver (yes or no response) in the pretest version of the survey. Demographic data from the ONS database were imbedded in the survey to enable descriptive analysis of participants.
The survey was piloted with 2,410 individuals. In phases 1 and 2, the survey was sent to an additional 11,890 ONS members. The advisory group made revisions in the survey for phase 2 of the overall project, based on phase 1 findings, to reduce the survey length and obtain new information regarding strategies used and barriers encountered when managing caregiver strain and burden. The survey was revised to include two open-ended items that assessed strategies nurses used and barriers encountered when managing caregiver strain and burden: “Tell us how you deal with the issue of caregiver strain and burden” and “Do you encounter barriers to working with informal caregivers in your practice? If so, tell us about the barriers you encounter.”
The survey was created and distributed via an email invitation and survey link in Zarca. A reminder email was sent to individuals who had not completed the survey one week prior to closing the survey. Nurses who participated were entered into a drawing for a computer tablet.
Analysis
Only participants who received the email survey invitation were included, as shown in the Zarca distribution report. The presence of any survey data, regardless of how many items were completed, was used to identify individuals who were considered responders to the survey. Only the first survey response was counted per person without differentiating at what point in the study the response took place. Chi-square analysis was used to compare demographic characteristics between responders and nonresponders.
Descriptive statistics were used to describe nurses’ practice and confidence in assessment and intervention, as well as the frequency of having been or having received care from an informal caregiver. Verbatim comments to open-ended questions were analyzed by the first author using IBM SPSS Text Analytics for Surveys, version 4.0.1, to identify and group derived concepts for summative content analysis. A 15% random sample of responses to both questions was provided to two external reviewers who were not involved in the study for validation of concepts derived. Differences in assignment and labeling of concepts were resolved by consensus.
To examine factors that may have contributed to practice and confidence in assessment and intervention with informal caregivers, a mixed-modeling approach was employed in two stages. In stage one, a series of models were run with an increasing number of subgroups according to the recommendations by Marsh, Lüdtke, Trautwein, and Morin (2009) and Masyn (2013) to identify subgroups according to patterns of practice and confidence. At each model, aspects of fit, Akaike information criterion, Bayesian information criterion (BIC), and sample size–adjusted BIC were examined, and the Lo-Mendel-Rubin likelihood ratio test (Lo, Mendell, & Rubin, 2001) was used to test if a given model was superior to a model with one less group (K versus K-1). In addition, models with less than 10% of the sample were discarded to avoid focus on models in which a small minority of the sample would drive the solution. In this approach, patterns across four indicators of caregiver practice were examined: level of confidence in assessment and ability to intervene, as well as percent age of patients who were assessed or had interventions.
In stage two, predictors of subgroup members were examined using multinomial logistic regression analyses within the Vermunt 3-step approach (Vermunt, 2010) as implemented in Mplus (Asparouhov & Muthén, 2014). Demographic variables, including role, practice setting, years in nursing, years in oncology, prior experience as an informal caregiver, and experience having received informal caregiving, were examined. Two-tailed tests of significance were used. Analyses were completed using IBM SPSS Statistics, version 24.0, and Mplus, version 7.4.
Results
Pilot survey responses were received from 262 nurses, for a 10.7% response rate. Pilot results showed near normal distributions, suggesting no significant floor or ceiling effects and that the survey was ready for full implementation.
The survey email invitation was sent to 14,300 ONS members who met inclusion criteria, and was successfully delivered to 12,926 (90%). A total of 2,055 individuals responded to the survey in the pilot, phase 1, and phase 2, for an overall response rate of 15.9%. This volume of responses from ONS members meeting inclusion criteria resulted in a less than 3% sampling error (Dillman, 2007).
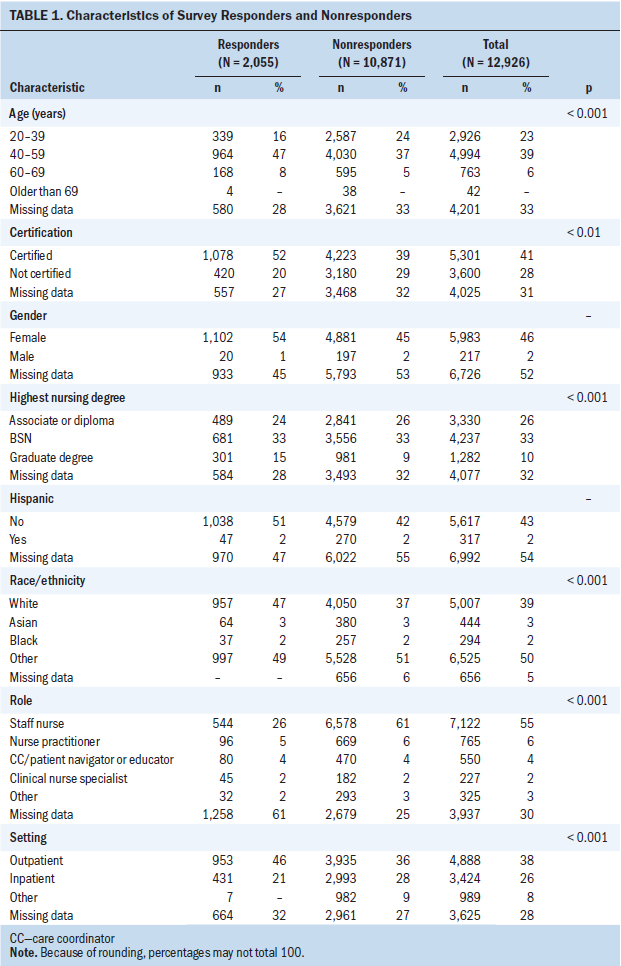
Sample Characteristics
Characteristics of survey responders and nonresponders are shown in Table 1. Responders were mostly White, had oncology nursing certification, had higher levels of nursing education, worked in an outpatient setting, were in advanced practice or care coordination roles, were older, and had more years of experience in nursing, in oncology and as members of ONS. Survey responders had an average of 23.4 years’ experience (SD = 11.9) in nursing, 13.87 years (SD = 9.9) in oncology practice, and 7.18 years in ONS (SD = 8.23), compared to 16.59 years (SD = 12.02) in nursing, 10.7 years (SD = 9.02) in oncology and 4.4 (SD = 6.32) years in ONS among nonresponders (p < 0.001). Of those who completed the pretest survey, 1,260 said they had been an informal caregiver and 535 said they had previously been ill and received care from an informal caregiver.
Nursing Practice, Confidence, and Knowledge
Nurses reported that they assessed caregivers of patients with cancer for strain and burden in an average of 50% of cases, and nurses reported that they provided interventions to caregivers in an average of 47% of cases. Nurses’ mean confidence level for assessing caregivers was 51, and nurses’ mean confidence level for intervening with caregivers was 45.6, both rated on 100-point scales. Nurses’ average knowledge of evidence-based interventions for caregiver strain and burden was 59.1% out of a possible 100%. Knowledge calculations showed that nurses tended to correctly identify interventions that were likely to be effective or be recommended for practice in PEP resources, but overestimated the strength of evidence for interventions for which effectiveness was not established.
[[{"type":"media","view_mode":"media_original","fid":"39991","attributes":{"alt":"","class":"media-image","height":"432","typeof":"foaf:Image","width":"366"}}]]
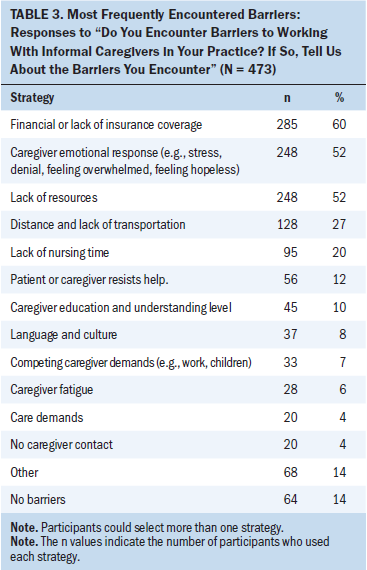
Responses to phase 2 open-ended questions (one or both questions) were provided by 681 nurses. Responses to questions regarding strategies used and barriers encountered in dealing with caregiver strain and burden are shown in Tables 2 and 3. As shown, the most frequent strategies used were referral to a social worker or others. Counseling was reported by 120 participants, and use of supportive interventions was reported by 75 participants. The most frequent barriers that nurses reported were financial (e.g., “availability of insurance to cover for help,” “money and time away from work”), difficulty dealing with intense emotional responses by caregivers (e.g., “too shocked or stressed to hear what the nurse is saying,” “resistance and defensiveness”), lack of resources (e.g., “mental health,” “crisis intervention services,” “local support services”), and distance and lack of transportation.
Factors Contributing to Practice and Confidence
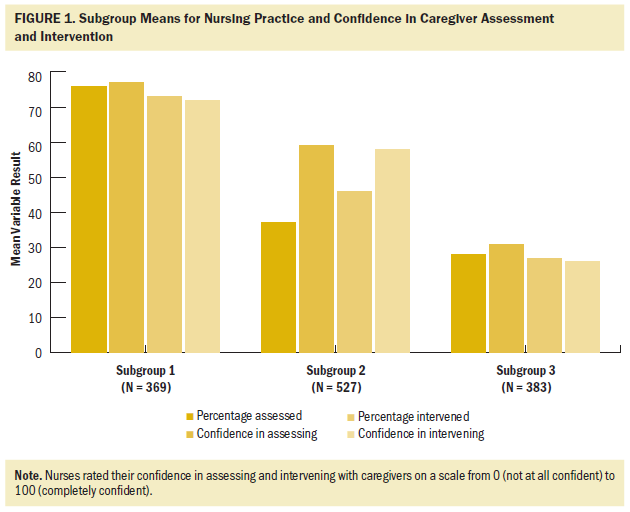
Because of confluence of fit indices and interpretability, the authors decided that a three-group model of nursing practice and confidence results was the best fit and greatest use of interpretation. As shown in Figure 1, nurses in group 1 were characterized by assessing and intervening with a high percentage of caregivers and by having high levels of confidence in carrying out these activities. Nurses in group 2 were characterized by assessing and intervening with few caregivers but with having higher levels of confidence. Nurses in group 3 were characterized by lower levels of assessment and intervention and also by lower levels of confidence. Groups 1 and 3 showed strong correlations between assessment and intervention practice and related confidence (0.47 and 0.55, respectively). No correlation between these existed in group 2, with a coefficient of 0.06.
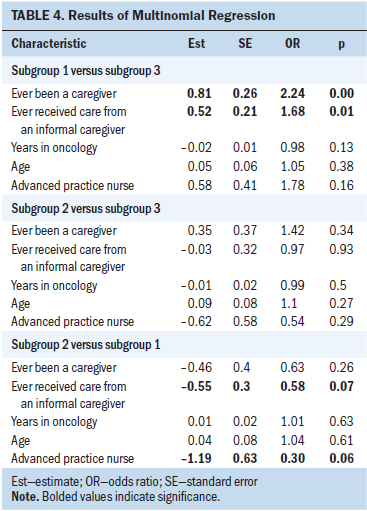
Results of multinomial logistic regression analysis using the Vermunt 3-step process are shown in Table 4. This analysis yielded a consistent finding that having been the recipient of informal caregiving (odds ratio [OR] = 1.68, p = 0.01) or having provided informal caregiving (OR = 2.24, p = 0.000) was significantly predictive of membership in group 1 versus group 3. Nurses who had received care from an informal caregiver (OR = 0.58, p = 0.07) or who were advanced practice nurses (OR = 0.3, p = 0.06) was predictive of being in group 1 versus group 2. No significant predictors of membership were observed in subgroup 2 versus subgroup 3.
Discussion
This study provides information about oncology nurses’ self-reported practices in terms of their frequency of assessing and intervening with informal caregivers of patients with cancer, their confidence in those practices, the strategies they used and barriers encountered in dealing with caregivers, and their knowledge of evidence-based interventions. Results show that, overall, nurses assessed and provided interventions to caregivers in about half their cases. The National Alliance for Caregiving (2016) reported that 54% of caregivers discussed care needs for the patient, but only 29% discussed their own needs. It is unclear if needs assessment and interventions reported in the current study reflect mostly caregiver skill training and care needs for patients or interventions aimed at other types of caregiver needs.
Although these data provide information about the self-reported level of confidence of nurses in dealing with caregiver assessment and intervention, the current authors cannot explain reasons for low confidence. Analysis of nurses’ verbatim responses about barriers suggested that the nurses had difficulty knowing how to deal with some of the strong emotional responses reported by caregivers (e.g., hopelessness, feeling overwhelmed), which may have affected nurses’ confidence. In addition, distance and transportation were identified as a barrier, suggesting that some caregivers may not have been present in the clinical settings, perhaps limiting nurses’ opportunity to work with caregivers and to gain confidence assessing and intervening with them. Additional research is needed to explore nurses’ confidence in working with caregivers and ways to enhance it.
Total knowledge scores of effective evidence-based interventions neared 60% on a 100-point scale. In general, lower knowledge scores were because many nurses reported that caregiver interventions without evidence of effectiveness, such as the use of music, massage, journaling, and art therapy, had a greater than actual strength of evidence than has been reported in the literature. Although these interventions are low risk and may provide some benefit, little evidence suggests that these interventions improve outcomes for informal caregivers of patients with cancer.
Subgroup analysis allowed the current authors to look at practice and confidence in assessment and interventions at the person level, rather than the variable level, to show patterns of practice. The most consistent finding from this analysis was that having been an informal caregiver or having received care from an informal caregiver was predictive of more frequent assessment, intervention, and confidence in these practices. Having the direct experience of caregiving or having received informal caregiving might increase nurses’ empathy, attention to, and understanding of the issues involved and needs of caregivers. These findings lead to the question of how nurses’ experience can be leveraged to educate and support others in practice.
The profile of practice variables across groups showed some interesting qualitative differences that were supported by correlation results. Groups 1 and 3 were consistent, such that practices and confidence were similar. In group 2, results were inconsistent, such that confidence was in assessment and intervention was much higher than frequency of performance of these practices. It is unclear if nurses in group 2 lacked direct access to caregivers or if they focused primarily on patient-related care and less on caregiver-related care, although they expressed confidence working with caregivers.
Problems like distance and transportation were identified as barriers to dealing with caregivers that may make it difficult to directly connect with caregivers. A growing body of evidence has examined the effectiveness of telephone-, video-, or computer-based psychoeducational, cognitive behavioral, and supportive interventions that can potentially eliminate the barrier of distance in working with informal caregivers (Badger et al., 2011; Demiris et al., 2012; DuBenske et al., 2014; Lapid et al., 2016; Lee, Yiin, & Chao, 2016; Leow, Chan, & Chan, 2015; Mosher et al., 2016; Northouse et al., 2014; Sherwood et al., 2012; Shum, Lui, Law, & Fong, 2014; Slev et al., 2016; Zheng, Head, & Schapmire, 2016). Ongoing research in this area is warranted.
The frequency of referral to social workers and others as a major nursing strategy for caregiver strain and burden indicates the importance of an interprofessional team approach to care and availability of social work and other professional resources in cancer care. The identification of caregiver emotional responses as a barrier to care suggests a need to further educate nurses on how to manage emotional aspects of providing care.
The barriers most often identified by participants were financial aspects and lack of insurance coverage. Current attention to financial toxicity in cancer care has focused on the costs of cancer treatment. Cost can also be a barrier to using services that might otherwise be available through referrals or recommendations from nurses to meet specific caregiver needs. The current findings suggest that assessment of financial burden needs to include its effect on families and caregivers. Caregivers may need to cut back on work or spend additional money on employing other caregivers. According to the AARP Public Policy Institute (2015), 6 of 10 caregivers have had to make workplace accommodation, such as cutting back on work, because of caregiving and have difficulty finding affordable caregiver services. Informal caregiving in the United States costs an estimated $522 billion annually (Chari, Engberg, Ray, & Mehrotra, 2015), and about 7%–8% of informal caregiving is related to cancer (Romito, Goldzweig, Cormio, Hagedoorn, & Andersen, 2013). If this cost were assumed by general healthcare services, it would overwhelm the healthcare system. Obtaining financial and instrumental resources is difficult compared to obtaining emotional support and advice (Romito et al., 2013). Policy, advocacy groups, and insurance approaches to provide some level of financial and instrumental support for informal caregiving should be considered.
Limitations
The results are limited because they are based on nurses’ self-report of practices and confidence. As shown in the analysis of survey responders and nonresponders, participants tended to be older, more educated, and have more experience in nursing and oncology practice. These results may not reflect the practice, confidence, or knowledge of younger and less experienced nurses. Results of analysis of verbatim survey responses regarding strategies used and barriers encountered are limited because, as with summative content analysis, the assignment and labeling of concepts derived may differ according to the analyst. This limitation was mitigated to some extent by the inclusion of external reviewers in the analysis to address reliability.
The surveys were constructed for this study and lack reliability data. Advisory group involvement in survey construction and review of the surveys prior to implementation provide some content validity, but validity was not directly measured.
Implications for Nursing
These findings add to the body of knowledge about family caregiving and specifically about the health professionals’ limited role with caregivers of patients with cancer. Nurses’ reported practices in assessing and intervening with caregivers, along with their relatively low confidence and limited knowledge of evidence-based interventions, point to the need for the ongoing education of nurses. Identification of caregiver emotional responses as a barrier presents an opportunity to improve nursing skills to effectively deal with these responses. Other identified barriers reveal the need for appropriate resources and strategies that can be used when distance and transportation become difficult. Lack of nursing time was identified as a barrier but was not the most prevalent barrier. Because nurses are in a unique position to identify and address caregiver needs and concerns, they should develop confidence in assessing caregiver strain and burden, as well as implement appropriate evidence-based interventions. Additional dissemination of evidence-based interventions to address caregiver strain and burden is needed.
Having been a caregiver and having received care from an informal caregiver were predictive of patterns of practice that reflected greater attention to caregivers and greater confidence in practice, which raises the question of how the experience of caregiving can be better incorporated into the practice environment and how more experiential learning techniques might be used in relevant nursing education. The information regarding the most frequent strategies used for caregiver strain and burden and most frequently encountered barriers suggests additional areas for education and resource needs in clinical practice settings. The identification of distance as a frequent barrier reveals the need for ongoing research in the use of technologic approaches to intervene with caregivers.
[[{"type":"media","view_mode":"media_original","fid":"39996","attributes":{"alt":"","class":"media-image","height":"164","typeof":"foaf:Image","width":"316"}}]]
Conclusion
Caregivers of individuals with cancer often face high caregiver strain and burden. Nurses are in a key role to assess and intervene with caregivers, but some may have little contact with caregivers or lack confidence in dealing with caregivers’ high emotional distress. More attention needs to be directed toward facilitating nurses’ contact with caregivers, increasing nurses’ understanding of effective caregiver interventions, and helping nurses gain additional skills as needed to address the emotionally demanding situations that caregivers face. Findings point to the importance of interprofessional care and availability of social workers and others for referrals as needed.
About the Author(s)
Margaret M. Irwin, PhD, RN, MN, is an adjunct faculty member in the Rangos School of Health Sciences at Duquesne University in Pittsburgh, PA; William Dudley, PhD, is a professor in the School of Health and Human Sciences at the University of North Carolina in Greensboro; Laurel Northouse, PhD, RN, is a professor emerita in the School of Nursing at the University of Michigan in Ann Arbor; Donna L. Berry, PhD, RN, AOCN®, FAAN, is the director of the Phyllis F. Cantor Center for Research in Nursing and Patient Care Services at Dana-Farber Cancer Institute in Boston, MA; and Gail A. Mallory, PhD, RN, NEA-BC, FAAN, is a retired director of research in Pittsburgh, PA. This research was funded by a grant (R18HS021957) from the Agency for Healthcare Research and Quality (principal investigator: Mallory). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. Dudley has previously consulted for the Oncology Nursing Society. Irwin and Dudley completed the data collection and analysis. All authors contributed to the conceptualization and design and the manuscript preparation. Irwin can be reached at m.irwin940@comcast.net, with copy to ONFEditor@ons.org. (Submitted July 2017. Accepted September 19, 2017.)
References
AARP Public Policy Institute. (2015). Caregiving in the United States, 2015. Retrieved from https://www.aarp.org/ppi/info-2015/caregiving-in-the-united-states-2015…
Asparouhov, T., & Muthén, B. (2014). Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling, 21, 329–341. https://doi.org/10.1080/10705511.2014.915181
Badger, T.A., Segrin, C., Figueredo, A.J., Harrington, J., Sheppard, K., Passalacqua, S., . . . Bishop, M. (2011). Psychosocial interventions to improve quality of life in prostate cancer survivors and their intimate or family partners. Quality of Life Research, 20, 833–844. https://doi.org/10.1007/s11136-010-9822-2
Boele, F.W., Given, C.W., Given, B.A., Donovan, H.S., Schulz, R., Weimer, J.M., . . . Sherwood, P.R. (2017). Family caregivers’ level of mastery predicts survival of patients with glioblastoma: A preliminary report. Cancer, 123, 832–840. https://doi.org/10.1002/cncr.30428
Chari, A.V., Engberg, J., Ray, K.N., & Mehrotra, A. (2015). The opportunity costs of informal elder-care in the United States: New estimates from the American Time Use Survey. Health Services Research, 50, 871–882. https://doi.org/10.1111/1475-6773.12238
Demiris, G., Parker Oliver, D., Wittenberg-Lyles, E., Washington, K., Doorenbos, A., Rue, T., & Berry, D. (2012). A noninferiority trial of a problem-solving intervention for hospice caregivers: In person versus videophone. Journal of Palliative Medicine, 15, 653–660. https://doi.org/10.1089/jpm.2011.0488
Dillman, D.A. (2007). Mail and internet surveys: The tailored design method (2nd ed.). Hoboken, NJ: John Wiley & Sons.
DuBenske, L.L., Gustafson, D.H., Namkoong, K., Hawkins, R.P., Atwood, A.K., Brown, R.L., . . . Cleary, J.F. (2014). CHESS improves cancer caregivers’ burden and mood: Results of an eHealth RCT. Health Psychology, 33, 1261–1272. https://doi.org/10.1037/a0034216
Havyer, R.D., van Ryn, M., Wilson, P.M., & Griffin, J.M. (2017). The effect of routine training on the self-efficacy of informal caregivers of colorectal cancer patients. Supportive Care in Cancer, 25, 1071–1077. https://doi.org/10.1007/s00520-016-3494-6
Honea, N.J., Brintnall, R., Given, B., Sherwood, P., Colao, D.B., Somers, S.C., & Northouse, L.L. (2008). Putting Evidence Into Practice: Nursing assessment and interventions to reduce family caregiver strain and burden. Clinical Journal of Oncology Nursing, 12, 507–516. https://doi.org/10.1188/08.CJON.507-516
Kershaw, T., Ellis, K.R., Yoon, H., Schafenacker, A., Katapodi, M., & Northouse, L. (2015). The interdependence of advanced cancer patients’ and their family caregivers’ mental health, physical health, and self-efficacy over time. Annals of Behavioral Medicine, 49. 901–911. https://doi.org/10.1007/s12160-015-9743-y
Lapid, M.I., Atherton, P.J., Kung, S., Sloan, J.A., Shahi, V., Clark, M.M., & Rummans, T.A. (2016). Cancer caregiver quality of life: Need for targeted intervention. Psycho-Oncology, 25, 1400–1407. https://doi.org/10.1002/pon.3960
Lee, K.-C., Yiin, J.-J., & Chao, Y.-F. (2016). Effect of integrated caregiver support on caregiver burden for people taking care of people with cancer at the end of life: A cohort and quasi-experimental clinical trial. International Journal of Nursing Studies, 56, 17–26. https://doi.org/10.1016/j.ijnurstu.2016.01.002
Leow, M., Chan, S., & Chan, M.F. (2015). A pilot randomized, controlled trial of the effectiveness of a psychoeducational intervention on family caregivers of patients with advanced cancer [Online exclusive]. Oncology Nursing Forum, 42, E63–E72. https://doi.org/10.1188/15.ONF.E63-E72
Lo, Y., Mendell, N.R., & Rubin, D.B. (2001). Testing the number of components in a normal mixture. Biometrika, 88, 767–778. https://doi.org/10.1093/biomet/88.3.767
Marsh, H.W., Lüdtke, O., Trautwein, U., & Morin, A.J.S. (2009). Classical latent profile analysis of academic self-concept dimensions: Synergy of person- and variable-centered approaches to theoretical models of self-concept. Structural Equation Modeling, 16, 191–225. https://doi.org/10.1080/10705510902751010
Masyn, K.E. (2013). Latent class analysis and finite mixture modeling. In T.D. Little (Ed.), The Oxford handbook of quantitative methods in psychology: Statistical analysis (vol. 2, pp. 1–44). New York, New York: Oxford University Press.
Mosher, C.E., Winger, J.G., Hanna, N., Jalal, S.I., Einhorn, L.H., Birdas, T.J., . . . Champion, V.L. (2016). Randomized pilot trial of a telephone symptom management intervention for symptomatic lung cancer patients and their family caregivers. Journal of Pain and Symptom Management, 52, 469–482. https://doi.org/10.1016/j.jpainsymman.2016.04.006
National Alliance for Caregiving. (2016). Cancer caregiving in the U.S.: An intense, episodic, and challenging care experience. Retrieved from https://healthcaredelivery.cancer.gov/caregiving
Northouse, L., Schafenacker, A., Barr, K.L., Katapodi, M., Yoon, H., Brittain, K., . . . An, L. (2014). A tailored Web-based psychoeducational intervention for cancer patients and their family caregivers. Cancer Nursing, 37, 321–330. https://doi.org/10.1097/NCC.0000000000000159
Northouse, L.L., Katapodi, M.C., Song, L., Zhang, L., & Mood, D.W. (2010). Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. CA: A Cancer Journal for Clinicians, 60, 317–339. https://doi.org/10.3322/caac.20081
Oncology Nursing Society. (2017). Caregiver strain and burden. Retrieved from https://www.ons.org/practice-resources/pep/caregiver-strain-and-burden
Romito, F., Goldzweig, G., Cormio, C., Hagedoorn, M., & Andersen, B.L. (2013). Informal caregiving for cancer patients. Cancer, 119(Suppl. 11), 2160–2169. https://doi.org/10.1002/cncr.28057
Sherwood, P.R., Given, B.A., Given, C.W., Sikorskii, A., You, M., & Prince, J. (2012). The impact of a problem-solving intervention on increasing caregiver assistance and improving caregiver health. Supportive Care in Cancer, 20, 1937–1947. https://doi.org/10.1007/s00520-011-1295-5
Shum, N.F., Lui, Y.L., Law, W.L., & Fong, Y.T.D. (2014). A nurse-led psycho-education programme for Chinese carers of patients with colorectal cancer. Cancer Nursing Practice, 13, 31–39. https://doi.org/10.7748/cnp.13.5.31.e1074
Slev, V.N., Mistiaen, P., Pasman, H.R., Verdonck-de Leeuw, I.M., van Uden-Kraan, C.F., & Francke, A.L. (2016). Effects of eHealth for patients and informal caregivers confronted with cancer: A meta-review. International Journal of Medical Informatics, 87, 54–67. https://doi.org/10.1016/j.ijmedinf.2015.12.013
Stenberg, U., Ruland, C.M., & Miaskowski, C. (2010). Review of the literature on the effects of caring for a patient with cancer. Psycho-Oncology, 19, 1013–1025. https://doi.org/10.1002/pon.1670
Vermunt, J.K. (2010). Latent class modeling with covariates: Two improved three-step approaches. Political Analysis, 18. 450–469. http://doi.org/10.1093/pan/mpq025
Zheng, Y., Head, B.A., & Schapmire, T.J. (2016). A systematic review of telehealth in palliative care: Caregiver outcomes. Telemedicine and E-Health, 22, 288–294. https://doi.org/10.1089/tmj.2015.0090


