Support Needs of People With Head and Neck Cancer Regarding the Disease and Its Treatment
Objectives: To provide insight into people’s experiences in dealing with the consequences of head and neck cancer (HNC) in daily life and their needs for self-management support.
Sample & Setting: 13 people with HNC who were successfully treated in the Department of Radiation Oncology at the Erasmus MC Cancer Institute in Rotterdam, the Netherlands.
Methods & Variables: Two focus groups and six individual interviews; data were analyzed with directed content analysis.
Results: Most patients wished to receive professional support for dealing with post-treatment consequences. Apart from physical complaints, patients had difficulties in dealing with the emotional aspects of HNC and its treatment and struggled with building self-confidence to move on with their lives. Patients mentioned the importance of relatives being there for them but complained that their needs were not always met. Support from fellow patients was valued for their empathetic capacity.
Implications for Nursing: Nurses must provide self-management support that meets people’s integral needs inherent in living with the consequences of HNC, particularly in the initial post-treatment period. Practical interventions could be useful.
Jump to a section
Head and neck cancer (HNC) is a relatively frequent type of cancer; it is the sixth most common cancer worldwide (Vigneswaran & Williams, 2014). Each year, about 63,000 people in the United States develop HNC (American Society of Clinical Oncology, 2017). In Europe, about 140,000 people are diagnosed with HNC every year (Ferlay et al., 2013); of these, 3,000 are in the Netherlands (Netherlands Comprehensive Cancer Organization, 2017). Data from the Netherlands Cancer Registry show increasing incidence and survival trends of HNC (Braakhuis, Leemans, & Visser, 2014).
Although the number of HNC survivors has risen steadily because of better treatment, survival does not necessarily imply a life free of physical and psychosocial problems related to the disease and its treatment (Aaronson et al., 2014). Treatment usually involves a combination of radiation therapy, chemotherapy, and surgery, and may have several potential side effects, such as facial disfigurement; dry mouth; difficulties with speaking, chewing, and swallowing; and nutritional deficits (Wells et al., 2015). Apart from these physical discomforts, the psychological impact of HNC is significant. Patients may experience anxiety, depression, uncertainty, and hopelessness (Ledeboer, Velden, Boer, Feenstra, & Pruyn, 2005; Neilson et al., 2013; Shiraz, Rahtz, Bhui, Hutchison, & Korszun, 2014). The initial post-treatment period, when patients receive less support from healthcare providers (HCPs) than they did during treatment, is one of the most vulnerable periods in the HNC trajectory (Moore, Ford, & Farah, 2014; Semple, Dunwoody, George Kernohan, McCaughan, & Sullivan, 2008; Wells, 1998). Wells et al. (2015) demonstrated that in the first five years after the end of treatment, many HNC survivors continued to experience distress, fear of recurrence, and oral and eating problems, among other concerns and unmet needs.
Therefore, although survivors of HNC live longer, they carry a significant physical and psychosocial burden after treatment (Rogers, 2010). The first 6–12 months after treatment are a critical period (Moore et al., 2014); patients are expected to take a more active role themselves, for which adequate self-management support (SMS) from HCPs is needed. A qualitative review by Dwarswaard, Bakker, van Staa, and Boeije (2016) identified generic preferences regarding SMS in various patient groups, including patients with HNC. Adopting a holistic definition of self-management (Barlow, Wright, Sheasby, Turner, & Hainsworth, 2002), the authors concluded that patients need instrumental, psychosocial, and relational support to effectively integrate a disease into daily life. Instrumental support is related to the disease and focuses on its medical management. Psychosocial support focuses on strengthening emotional and psychological resources needed to manage the disease, and relational support refers to helpful interactions with other people, including healthcare providers, family, friends, and fellow patients.
For patients with diseases that have a potential long-term impact on functioning and quality of life, such as HNC, nurses are often in an excellent position to deliver SMS because they play a central role in the care process (Elissen et al., 2013; Singh, 2005). Although they may be willing to provide this support, nurses may not know how to adequately coach patients toward more self-confidence and respond to their psychosocial challenges and concerns (Been-Dahmen, Dwarswaard, Hazes, van Staa, & Ista, 2015; Dutch Society for Ear-Nose-Throat Surgery, 2014; ter Maten-Speksnijder, Dwarswaard, Meurs, & van Staa, 2016). In addition, what exact support that people with HNC need after curative treatment is unknown. Evidence on what promotes health and what empowers individuals living with HNC is still scarce. Therefore, the current study aims to provide insight into the experiences of people with HNC and their needs for SMS in the post-treatment phase, using the conceptual framework of Dwarswaard et al. (2016). This insight could form the basis for an aftercare program that facilitates nurses providing this support.
Methods
Setting
The current study included people with HNC treated in the Department of Radiation Oncology at the Erasmus MC Cancer Institute in Rotterdam, the Netherlands. The role of the nurse practitioner (NP) who works in this outpatient department mainly consists of promoting the continuity and quality of nursing care and medical treatment. Follow-up care after treatment is focused on early detection of local or regional recurrence, morbidity, and secondary tumors.
Design
A qualitative phenomenologic design including focus groups and individual semistructured interviews was used (Polit & Beck, 2010). The study was performed to guide the development of a tailored nurse-led SMS program for outpatients with various conditions that bring with them long-term consequences in daily life.
Participants
Patients were eligible for inclusion if they were aged older than 18 years, had received chemotherapy and radiation therapy for stage II, III, or IV HNC for the first time, had completed their initial phase of treatment (i.e., more than three months after chemotherapy and radiation therapy), and were sufficiently proficient in the Dutch language. Patients who were still in active treatment or in the palliative phase were excluded. Using a full sampling strategy, the authors identified eligible patients and contacted them by telephone to solicit their interest in participating in the study. Those who showed interest were sent an information letter.
Of the 38 patients who were invited, 7 consented to participate in a focus group. The main reason for nonparticipation was not wishing to be reminded of the treatment phase; they wanted to leave this behind them. To ensure maximum variation in terms of age, gender, marital status, employment, and disease stage, six patients were additionally invited by means of purposeful sampling for individual interviews.
Ethical Considerations
The Ethics Review Board of Erasmus MC approved the study protocol (MEC-2013-350). All study participants were informed about the study orally and in writing, and they were ensured complete confidentiality and anonymity. All participants provided written consent for participation. They were rewarded with a €20 gift voucher.
Data Collection
In the focus group sessions, an independent moderator (psychologist) kept the discussions focused and generated a lively and productive conversation. The participants were encouraged to share their expectations and experiences regarding SMS. The six individual semistructured interviews were conducted by trained students and a researcher. Figure 1 provides an overview of the questions asked during the focus group sessions and individual interviews. The development of the interview guide—which also was used in other studies about the same topic (e.g., Been-Dahmen et al., 2017)—was an iterative process in which all questions were critically reviewed by the members of the research team. The questions served to open the conversation and encourage the participants to express their experiences (Polit & Beck, 2010). 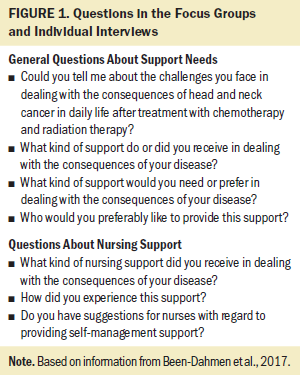
Data Analysis
All data were audio recorded and transcribed verbatim. Data were analyzed with the directed content analysis approach (Hsieh & Shannon, 2005). This method is designed to validate or extend conceptually an existing theoretical framework—in this case, the concept of SMS needs constructed by Dwarswaard et al. (2016), which identifies three types of patient needs for SMS: instrumental, psychosocial, and relational support.
First, each transcript was coded using the predetermined codes from the theoretical framework, containing the types of SMS needed and the sources of support. Any text that could not be categorized with these codes was placed under a subcategory of an existing code or was given a new code. The first author analyzed all data in detail. Then, the second author independently coded and analyzed anonymized data from the focus group sessions and critically read along with the first author’s analysis of the interviews. To increase dependability, results were discussed in the research team. Atlas.ti, version 7.0, was used for data analysis.
Results
Thirteen people successfully treated for HNC (10 men and 3 women with a median age of 60 years [range = 48–73 years]) were included, in line with the distribution in the total population. They had completed treatment as many as two years before. None had participated in a clinical trial. Additional demographic characteristics and information about cancer types and treatments are shown in Table 1. Table 2 presents an overview of the main SMS needs identified. Support needs differed before, during, and after treatment. 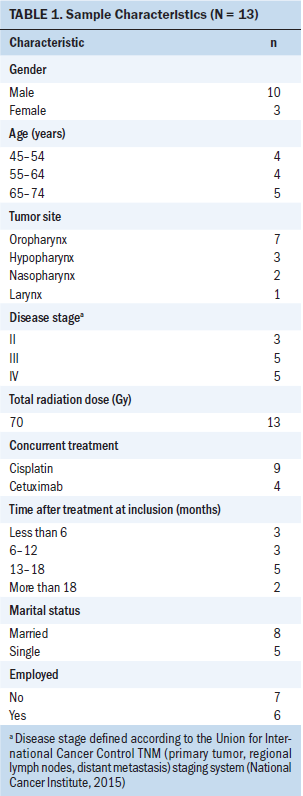
Instrumental Support
Before treatment: Directly after diagnosis, patients had an urgent need for detailed information and instruction about the different treatment options, potential side effects, long-term consequences, and expectations regarding recovery. According to one participant: “The nurse practitioner did explain well what I could expect. . . . Yes, she has done well. I was well prepared for everything, no nervous sweating.” Patients greatly appreciated information from the NP about treatment details, particularly about how to manage the intense chemotherapy and radiation therapy sessions. 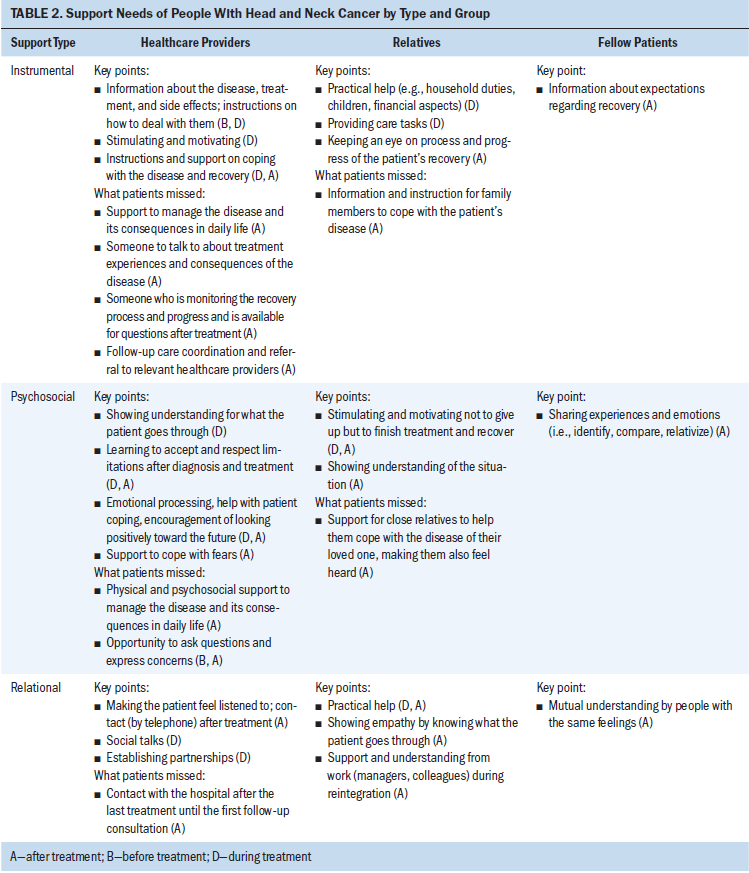
During treatment: During treatment, patients mainly expected instrumental support from HCPs in monitoring their treatment and recovery process. Patients came up with all kind of questions, such as how to deal with weight loss, dehydration, pain, and swallowing difficulties. The availability of HCPs and specific support (e.g., speech therapy, dietary treatment) was important to them. In addition, they wished that HCPs would take an active role in making health- or treatment-related decisions. Most patients felt too sick and exhausted to take the lead in shared decision making. One participant said:
I don’t want to take the lead at all. The ones who are the experts should tell me what the best for me is: “We want to do this, and if that is not okay with you, I will explain why it is necessary.” Well, I think I don’t want to have a voice in that.
Support from relatives was important during the entire treatment trajectory. Hearing the information and instructions provided by HCPs helped patients to remember, internalize, and apply these.
After treatment: After completion of curative treatment, receiving information from HCPs about the consequences of the disease and the medical treatment remained important. Patients felt the NP could play a central role here—for instance, if lifestyle changes had been recommended. They appreciated being told about the importance of adherence to their therapeutic regimen. It also helped when HCPs explored possibilities and were open to discuss disease-related information in the context of patients’ own lives. Patients agreed that more frequent follow-up consultations, with the NP as a coordinator, could help tailor the information to their individual needs. This is supported by one participant, who said the following:
That there is a coordinator who will keep an eye on things . . . that the follow-up from the nurse practitioner is continued, also for information about referral to relevant care professionals. Because you really don’t have an idea [about the possibilities].
Another participant said:
I knew I could contact [the hospital] for support. . . . As the nurse practitioner says: “If something is wrong, just give a call.” But you don’t want to do that too soon. Still a kind of threshold, I think. You first wait for better times, just one more week.
Instrumental support from relatives remained important. Besides monitoring patients’ recovery progress, family and friends could provide practical support in doing household duties, taking care of children, and providing basic care. In addition, family members sometimes encouraged patients to continue eating and drinking. According to one participant:
My wife forced me to eat. She said: “Stop tube feeding. We are going to eat now.” . . . And then she started with small appetizers, a piece of fish, a piece of . . . everything that was smooth. Because I had difficulty swallowing. . . . My wife and children have pulled me through. I did not want it at the time.
Psychosocial Support
Before treatment: Patients valued support from HCPs to accept the diagnosis and therapy treatment plan, which stimulated and motivated not to give up. HCPs encouraged them to ask questions about the diagnosis and treatment. Having a sense of being heard and allowed to express concerns and feelings was important for patients. Some desired more room for this.
During treatment: Being stimulated and motivated not to give up was important for patients during active treatment. They often felt anxious, stressed, and hopeless and needed someone who recognized their emotions and helped them build self-confidence during the treatment process. HCPs and relatives could provide such support. According to one participant:
I said: “I am going home. I am done with it. I don’t want to continue my therapy. This is not a life.” But then, the nurse practitioner came to visit me, on Sunday afternoon. . . . She wanted to talk with me. . . . She said: “There are only seven radiations left. We will keep you here the coming week so that you can finish your treatment.” Finally, she persuaded me to continue.
Another participant said:
The nurse practitioner told me not to give up, while at that moment I actually didn’t want to hear “you have to do this” and “you have to do that.” . . . I often thought: “What are you worrying about?” But now I realize that they did it all for my own good.
Relatives accompanied their loved ones to hospital appointments and visited them during their hospitalizations. Patients needed their help because fatigue from chemotherapy and radiation therapy often worsened as treatment went on. According to one participant: “My husband was always with me. He came with me to my hospital appointments. He said: ‘It isn’t nice for you when you have to do it all on your own.’”
After treatment: Psychosocial support after treatment consisted of helping patients cope with anxiety and stress and showing understanding of what patients have gone through. Some patients feared recurrence of the cancer and were positive about HCPs helping them to cope with these fears or by encouraging them to look positively toward the future. Other patients were not satisfied by the current level of psychosocial support. One participant said: “[I felt] somewhat abandoned. For support after treatment, it would be better to have follow-up continued. . . . This could be part of the tasks of a coordinating nurse.” Relatives also could provide psychosocial support. Humor seemed to be an effective mechanism to cope with cancer-related experiences. According to one participant:
Previously, I was always the first to finish dinner. . . . Nowadays, however, I am the last to finish eating and [at home] they are sometimes joking about that. . . . We all need a little bit of self-mockery; I think it is good to see things positively.
Sharing experiences and emotions with fellow patients also may be supportive in the period after treatment. The focus groups offered such an opportunity and were valued by the participants. One participant said: “That you can share things with each other, about experiences and feelings, and about how to do things. Then you can maybe relativize the severity of your own situation.”
Relational Support
During and after treatment: From the onset of chemotherapy and radiation therapy, patients valued having good partnerships with HCPs and experiencing sympathy through listening and showing interest. This made them feel confident and taken seriously. Patients differed in their views about their own role to play. Some preferred going their own way and relied on their own expertise, and others wanted HCPs to guide them. According to one participant: “I felt that I was getting better, so I stopped my tube feeding and started to eat some food. I just tried it and it went quite well. . . . [I thought]: If it doesn’t work, it doesn’t work.” Another participant said:
Of course, you have to do it on your own. . . . But in these kinds of situations, you do not always want [HCPs] to ask you what you prefer. They should just say, “We are going to do it this way.”
Family and friends provided practical help by performing household duties and taking care of the children. In addition, they contributed to patients’ emotional processing of the disease trajectory and tried to share experiences. However, several patients reported that relatives did not always help them in the “right” way because they did not realize what patients went through. According to one participant: “Honestly, it seemed as if [my family] did not exactly realize what was happening.” Another participant said:
People close to you come to visit you for about one hour, but from the moment they leave, they go straight back to their own lives and do not have any idea of the emotional and physical impact of the disease.
Therefore, some patients found that support from fellow patients could be beneficial because they had similar experiences. According to one participant: “I was not at all prepared for the fact that you can come out of the treatment in such a bad state. [Fellow patients] could have been helpful there.”
Discussion
The current study provided insight into how people with HNC deal with the disease, the treatment, and their consequences in daily life, and explored patients’ needs for SMS. In general, patients were satisfied with the professional support they received during treatment. The period after treatment completion seemed to be most challenging for them. Apart from physical problems, patients experienced difficulties in dealing with the emotional aspects of HNC and its treatment and struggled with building self-confidence to move on with their lives. Most patients would have liked more professional support in the initial post-treatment phase. Patients wanted to be heard by HCPs, invited to express their concerns and ask questions, and guided in health- and treatment-related decisions.
The support needs of people with HNC in the post-treatment phase can be explained by the cancer care continuum. This is a fairly new paradigm in cancer care in which cancer is considered a chronic illness that requires long-term surveillance or treatment (McCorkle et al., 2011). This paradigm shift results from improvements in the early detection, diagnosis, and treatment of cancer, as a result of which survival is longer and care extends beyond the acute phase. The cancer care continuum places demands on patients and their families in arranging their own follow-up care, but also on HCPs (particularly nurses) because it requires establishing ongoing partnerships with patients and providing adequate SMS. This is also true for people with HNC (Moore et al., 2014; Semple et al., 2008; Wells, 1998).
In the current study, the role of family and friends in providing SMS during and after treatment proved important, which is a finding consistent with prior research of Longacre, Ridge, Burtness, Galloway, and Fang (2012). Particularly in the post-treatment phase, which some patients referred to as “a black hole,” participation of family in SMS is desired (Maguire et al., 2017; Nightingale, Curbow, Wingard, Pereira, & Carnaby, 2016). Fellow patients were valued for their empathy, particularly in the period after treatment. Mutual understanding was mentioned as a major benefit of peer support. This is confirmed by previous research that found that support from fellow patients by sharing lived experiences is highly valuable in adapting to the psychosocial outcomes of HNC treatment (Dwarswaard et al., 2016; Egestad, 2013; Pateman, Ford, Batstone, & Farah, 2015). Sharing experiences with peers can help to relativize the severity of one’s own situation and provide comfort and strategies for successful coping. Still, most studies reported about peer support during treatment rather than in the period after treatment completion (Lang, France, Williams, Humphris, & Wells, 2013). In addition, the need for support from fellow patients varies among individuals and is influenced by disease-related and individual factors (i.e., psychological response and changes in patients’ personal situation or network) (Dwarswaard et al., 2016). Some patients in the current study did not wish to share experiences in a focus group but preferred an individual interview; others did not want to tell researchers about their experiences at all.
Although nurses are often focused on providing instrumental support (e.g., monitoring symptoms, giving information), the current study shows that they also have an important role in providing psychosocial and relational support. Providing information and instruction about how to deal with the consequences of HNC in daily life is not enough because patients also need to cope with the emotional and social challenges they face. This finding is supported by other studies about HNC. Lang et al. (2013) and Wells et al. (2015) described the significant psychological impact of HNC, which lasts beyond the end of the treatment period. Their studies emphasized the importance of holistic needs assessment as part of follow-up care for HNC survivors, with subsequent tailoring of support for their individual needs and concerns. In a study by Richardson, Morton, and Broadbent (2015), patients also reported that they would like to receive psychological support to improve understanding, gain perspective, and develop coping strategies. Still, a significant number of the patients said they did not need additional psychological support from HCPs because they felt supported by family and friends. In addition, patients realized that they themselves need to be strong and find emotional healing. Therefore, an open assessment of patients’ support needs should be included in routine nursing after care in patients with head and neck cancer.
Strengths and Limitations
The concept of SMS needs, proposed by Dwarswaard et al. (2016), was helpful for the current study in that the authors could create a deeper understanding of the support needs of people with HNC. However, the deductive analytical method of the direct content analysis approach carries the risk of fitting data to the predetermined coding scheme of types and sources of support. To minimize this, the authors applied inductive coding when data could not be categorized. Distinguishing among three phases (before, during, and after HNC treatment) provided additional insights about when people with HNC need particular types and sources of SMS, which helps to tailor SMS optimally. Secondly, the authors enriched the data by performing face-to-face interviews in addition to focus group interviews. Individual participants elaborated more on their experiences and could be interviewed more thoroughly on specific topics that remained underexposed after the focus group sessions. This helped create a comprehensive understanding of the needs of people with HNC. Still, it should not be ignored that the current study only provides insight into the experiences of individuals willing to share them. Those who were not willing to evaluate their support needs because they did not want to be confronted with the treatment phase probably will react differently to an aftercare program than the people who participated in the study. This implies that nurses must assess peoples’ needs for support at different times in the trajectory of HNC treatment.
A limitation of the current study is the small size of the focus groups, with only seven participants, who were all men. This creates uncertainty about the transferability of the findings. Given that most people with HNC are men (Netherlands Comprehensive Cancer Organization, 2017), women were difficult to recruit. To minimize the risk of selection bias, the authors purposefully searched for women for the additional individual interviews and found some. The authors recommend taking a larger sample size to study the experiences and support needs of people with HNC in future research. In addition, it would be interesting to investigate whether the extent of the disease and its treatment may influence the responses, because the current study cannot make inferences about this.
Another limitation could be that too little attention has been paid to patients’ support needs before the start of treatment, including the need for professional guidance in shared decision making on treatment choices. However, in the interviews, patients expressed some support needs in this period. It seemed as if they only sought some instrumental support, although it may be expected that, particularly in this phase, psychosocial support is needed to overcome the shock and feeling of disbelief of diagnosis. A study by Richardson et al. (2015) found that people with HNC considered empathy from family and friends as the most helpful form of social support at diagnosis. Also, the importance of having close relatives who could help to maintain a sense of normality at diagnosis was emphasized (Richardson et al., 2015).
Implications for Nursing
Nurses working in outpatient care are used to providing patients with information and instruction about how to adjust life to the disease (Been-Dahmen et al., 2015; ter Maten-Speksnijder et al., 2016). Given the burden of treatment for people with cancer, nurses are challenged to provide psychosocial and relational support as well. The current study confirms that people with HNC need SMS from a holistic point of view, and that this support sometimes is lacking. Particularly in the post-treatment period, professional follow-up care that meets patients’ integral needs seems to be missing. HCPs themselves recognized that psychosocial support needs of HNC survivors are not being met. They experienced difficulties in meeting patients’ needs (Breen et al., 2017). Nurses seem to lack sufficient training and practical interventions to provide holistic self-management support (Been-Dahmen et al., 2015).
A useful intervention to support people with HNC is the Self-Management Web (SMW) (Beck et al., 2018). This visual, conversational diagram is combined with solution-focused communication techniques to provide an open, patient-led assessment of 14 life areas. Because multiple areas are represented, SMW ensures a holistic view. It also encourages shared decision making between patients and nurses and intrinsic motivation of patients because they are in charge of selecting an area to work on if support is desired. To promote effectiveness and ensure nurses’ fidelity to the intervention, training before implementation is required. This comprises an explanation on how to carry out the intervention protocol and training in solution-focused brief therapy (Ratner, George, & Iveson, 2012). 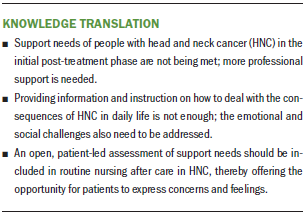
Conclusion
The authors investigated the self-management support needs of people with HNC. Professional SMS seems to be deficient, particularly in the initial post-treatment period. Apart from practical support, patients need psychosocial and relational support to deal with the challenges inherent in living with the effects of HNC. Nurses need practical tools and training to support patients in recovering autonomy and self-confidence.
The authors gratefully acknowledge Erwin Ista, PhD, RN, and Jolanda Dwarswaard, PhD, for their support in the design of the study; Jørgen Mous, MSc, who moderated the focus groups; and all patients who participated in the study.
About the Author(s)
Mariëlle A.C. Peeters, MSc, is a researcher in the Research Centre Innovations in Care at Rotterdam University of Applied Sciences; Cora Braat, MANP, RN, is a nurse specialist in the Department of Radiation Oncology at Erasmus MC Cancer Institute; Janet M.J. Been-Dahmen, MSc, RN, is a PhD student at Rotterdam University of Applied Sciences; Gerda M. Verduijn, MD, is a radiation oncologist in the Department of Radiation Oncology and Wendy H. Oldenmenger, PhD, RN, is a coordinator of oncology nursing research, both at Erasmus MC Cancer Institute; and AnneLoes van Staa, MD, PhD, RN, is a professor at Rotterdam University of Applied Sciences, all in the Netherlands. This study forms part of the research program NURSE-CC (Rotterdam Consortium for NUrsing Research into Self-management and Empowerment in Chronic Care), funded by the Netherlands Organization for Health Research and Development (grant number 520001004). van Staa has previously consulted for Medtronic. Peeters, Braat, and Been-Dahmen completed the data collection. Braat and Oldenmenger provided statistical support. Peeters, Braat, Oldenmenger, and van Staa provided the analysis. All authors contributed to the conceptualization and design and the manuscript preparation. Peeters can be reached at m.a.c.peeters@hr.nl, with copy to ONFEditor@ons.org. (Submitted December 2017. Accepted February 28, 2018).
References
Aaronson, N.K., Mattioli, V., Minton, O., Weis, J., Johansen, C., Dalton, S.O., . . . van de Poll-Franse, L.V. (2014). Beyond treatment—Psychosocial and behavioural issues in cancer survivorship research and practice. EJC Supplements, 12, 54–64. https://doi.org/10.1016/j.ejcsup.2014.03.005
American Society of Clinical Oncology. (2017). Head and neck cancer: Statistics. Retrieved from https://www.cancer.net/cancer-types/head-and-neck-cancer/statistics
Barlow, J., Wright, C., Sheasby, J., Turner, A., & Hainsworth, J. (2002). Self-management approaches for people with chronic conditions: A review. Patient Education and Counseling, 48, 177–187. https://doi.org/10.1016/S0738-3991(02)00032-0
Beck, D.K., Been-Dahmen, J.M.J., Peeters, M.A.C., Grijpma, J.W., Van der Stege, H.S., Tielen, M., . . . van Staa, A.L. (2018). The development of a nurse-led self-management support intervention for kidney transplant recipients using intervention mapping: The ZENN-study. Manuscript submitted for publication.
Been-Dahmen, J.M., Dwarswaard, J., Hazes, J.M., van Staa, A., & Ista, E. (2015). Nurses’ views on patient self-management: A qualitative study. Journal of Advanced Nursing, 71, 2834–2845. https://doi.org/10.1111/jan.12767
Been-Dahmen, J.M., Walter, M.J., Dwarswaard, J., Hazes, J.M., van Staa, A., & Ista, E. (2017). What support is needed to self-manage a rheumatic disorder: A qualitative study. BMC Musculoskeletal Disorders, 18, 84. https://doi.org/10.1186/s12891-017-1440-5
Braakhuis, B.J., Leemans, C.R., & Visser, O. (2014). Incidence and survival trends of head and neck squamous cell carcinoma in the Netherlands between 1989 and 2011. Oral Oncology, 50, 670–675. https://doi.org/10.1016/j.oraloncology.2014.03.008
Breen, L.J., O’Connor, M., Calder, S., Tai, V., Cartwright, J., & Beilby, J.M. (2017). The health professionals’ perspectives of support needs of adult head and neck cancer survivors and their families: A Delphi study. Supportive Care in Cancer, 25, 2413–2420. https://doi.org/10.1007/s00520-017-3647-2
Dutch Society for Ear-Nose-Throat Surgery. (2014). Head and neck cancer guidelines. Retrieved from https://www.nvmka.nl/sites/www.nvmka.nl/files/Richtlijn%20Hoofd-halstum…
Dwarswaard, J., Bakker, E.J., van Staa, A., & Boeije, H.R. (2016). Self-management support from the perspective of patients with a chronic condition: A thematic synthesis of qualitative studies. Health Expectations, 19, 194–208. https://doi.org/10.1111/hex.12346
Egestad, H. (2013). The significance of fellow patients for head and neck cancer patients in the radiation treatment period. European Journal of Oncology Nursing, 17, 618–624. https://doi.org/10.1016/j.ejon.2013.01.001
Elissen, A., Nolte, E., Knai, C., Brunn, M., Chevreul, K., Conklin, A., . . . Vrijhoef, H. (2013). Is Europe putting theory into practice? A qualitative study of the level of self-management support in chronic care management approaches. BMC Health Services Research, 13, 117. https://doi.org/10.1186/1472-6963-13-117
Ferlay, J., Steliarova-Foucher, E., Lortet-Tieulent, J., Rosso, S., Coebergh, J.W., Comber, H., . . . Bray, F. (2013). Cancer incidence and mortality patterns in Europe: Estimates for 40 countries in 2012. European Journal of Cancer, 49, 1374–1403. https://doi.org/10.1016/j.ejca.2012.12.027
Hsieh, H.F., & Shannon, S.E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15, 1277–1288. https://doi.org/10.1177/1049732305276687
Lang, H., France, E., Williams, B., Humphris, G., & Wells, M. (2013). The psychological experience of living with head and neck cancer: A systematic review and meta-synthesis. Psycho-Oncology, 22, 2648–2663. https://doi.org/10.1002/pon.3343
Ledeboer, Q.C., Velden, L.A., Boer, M.F., Feenstra, L., & Pruyn, J.F. (2005). Physical and psychosocial correlates of head and neck cancer: An update of the literature and challenges for the future (1996–2003). Clinical Otolaryngology, 30, 303–319. https://doi.org/10.1111/j.1365-2273.2005.01035.x
Longacre, M.L., Ridge, J.A., Burtness, B.A., Galloway, T.J., & Fang, C.Y. (2012). Psychological functioning of caregivers for head and neck cancer patients. Oral Oncology, 48, 18–25. https://doi.org/10.1016/j.oraloncology.2011.11.012
Maguire, R., Hanly, P., Balfe, M., Timmons, A., Hyland, P., O’Sullivan, E., . . . Sharp, L. (2017). Worry in head and neck cancer caregivers: The role of survivor factors, care-related stressors, and loneliness in predicting fear of recurrence. Nursing Research, 66, 295–303. https://doi.org/10.1097/NNR.0000000000000223
McCorkle, R., Ercolano, E., Lazenby, M., Schulman-Green, D., Schilling, L.S., Lorig, K., & Wagner, E.H. (2011). Self-management: Enabling and empowering patients living with cancer as a chronic illness. CA: A Cancer Journal for Clinicians, 61, 50–62. https://doi.org/10.3322/caac.20093
Moore, K.A., Ford, P.J., & Farah, C.S. (2014). “I have quality of life . . . but . . . ”: Exploring support needs important to quality of life in head and neck cancer. European Journal of Oncology Nursing, 18, 192–200. https://doi.org/10.1016/j.ejon.2013.10.010
National Cancer Institute. (2015). Cancer staging. Retrieved from https://www.cancer.gov/about-cancer/diagnosis-staging/staging
Neilson, K., Pollard, A., Boonzaier, A., Corry, J., Castle, D., Smith, D., . . . Couper, J. (2013). A longitudinal study of distress (depression and anxiety) up to 18 months after radiotherapy for head and neck cancer. Psycho-Oncology, 22, 1843–1848. https://doi.org/10.1002/pon.3228
Netherlands Comprehensive Cancer Organization. (2017). Head and neck cancer [in Dutch]. Retrieved from https://bit.ly/2KdTrVT
Nightingale, C.L., Curbow, B.A., Wingard, J.R., Pereira, D.B., & Carnaby, G.D. (2016). Burden, quality of life, and social support in caregivers of patients undergoing radiotherapy for head and neck cancer: A pilot study. Chronic Illness, 12, 236–245.
Pateman, K.A., Ford, P.J., Batstone, M.D., & Farah, C.S. (2015). Coping with an altered mouth and perceived supportive care needs following head and neck cancer treatment. Supportive Care in Cancer, 23, 2365–2373. https://doi.org/10.1007/s00520-015-2607-y
Polit, D.F., & Beck, C.T. (2010). Essentials of nursing research: Appraising evidence for nursing practice (7th ed.). Philadelphia, PA: Lippincott Williams and Wilkins.
Ratner, H., George, E., & Iveson, C. (2012). Solution focused brief therapy: 100 key ideas and techniques. London, England: Routledge.
Richardson, A.E., Morton, R., & Broadbent, E. (2015). Psychological support needs of patients with head and neck cancer and their caregivers: A qualitative study. Psychology and Health, 30, 1288–1305. https://doi.org/10.1080/08870446.2015.1045512
Rogers, S.N. (2010). Quality of life perspectives in patients with oral cancer. Oral Oncology, 46, 445–447. https://doi.org/10.1016/j.oraloncology.2010.02.021
Semple, C.J., Dunwoody, L., George Kernohan, W., McCaughan, E., & Sullivan, K. (2008). Changes and challenges to patients’ lifestyle patterns following treatment for head and neck cancer. Journal of Advanced Nursing, 63, 85–93. https://doi.org/10.1111/j.1365-2648.2008.04698.x
Shiraz, F., Rahtz, E., Bhui, K., Hutchison, I., & Korszun, A. (2014). Quality of life, psychological wellbeing and treatment needs of trauma and head and neck cancer patients. British Journal of Oral and Maxillofacial Surgery, 52, 513–517. https://doi.org/10.1016/j.bjoms.2014.03.019
Singh, D. (2005). Which staff improve care for people with long-term conditions? A rapid review of the literature. Retrieved from https://www.birmingham.ac.uk/Documents/college-social-sciences/social-p…
ter Maten-Speksnijder, A., Dwarswaard, J., Meurs, P.M., & van Staa, A.L. (2016). Rhetoric or reality? What nurse practitioners do in providing self-management support in outpatient clinics: An ethnographic study. Journal of Clinical Nursing 25, 3219–3228. https://doi.org/10.1111/jocn.13345
Vigneswaran, N., & Williams, M.D. (2014). Epidemiologic trends in head and neck cancer and aids in diagnosis. Oral and Maxillofacial Surgery Clinics of North America, 26, 123–141. https://doi.org/10.1016/j.coms.2014.01.001
Wells, M. (1998). The hidden experience of radiotherapy to the head and neck: A qualitative study of patients after completion of treatment. Journal of Advanced Nursing, 28, 840–848. https://doi.org/10.1111/j.1365-2648.1998x.00714.x
Wells, M., Cunningham, M., Lang, H., Swartzman, S., Philp, J., Taylor, L., & Thomson, J. (2015). Distress, concerns and unmet needs in survivors of head and neck cancer: A cross-sectional survey. European Journal of Cancer Care, 24, 748–760. https://doi.org/10.1111/ecc.12370




