Caregivers’ Need for Support in an Outpatient Cancer Setting
Purpose: To investigate the needs of caregivers for individuals with cancer and to gain insight into how to provide support for caregivers.
Participants & Setting: 47 caregivers for patients with cancer in an outpatient setting in Denmark.
Methodologic Approach: This qualitative study used focus group interviews. Data were analyzed using a hermeneutics framework and Malterud’s systematic text condensation.
Findings: Results of the nine focus groups showed the experiences of caregiving. Theme 1 was interdependence, which consisted of the subthemes responsibility, a moral obligation and loneliness and talking. The results also revealed a second theme, different needs for support, which contained three subthemes: support through personal time, support through peers, and support through talking to healthcare professionals.
Implications for Nursing: Caregivers for individuals with cancer do not distinguish their own needs and perspectives of support from those of the patients. Caregivers’ need for support includes having support from peers, talking to healthcare professionals, and having personal time. Support of caregivers should allow for focusing on the family as a unit instead of solely addressing the patient.
Jump to a section
Cancer incidence and prevalence have increased globally (Jemal & Torre, 2018; Sundhedsdatastyrelsen, 2017). The implications for Danish society are imminent in terms of expenses associated with aggressive and enhanced treatments (Danske Regioner, KL, Økonomi- Og Indenrigsministeriet, Finansministeriet, & Ministeriet for Sundhed og Forebyggelse, 2013). Therefore, there is political focus on efficient use of resources (Sundhedsstyrelsen, 2016). The focus on efficient healthcare services has led to fast-tracked treatments and an increasing number of patients in outpatient clinics for care and treatment (Sundhedsdatastyrelsen, 2016). The change of setting related to treatment and care from the hospital to an outpatient setting engages relatives as caregivers, which is also reflected in other countries (Australian Government, Department of Social Services, 2018; Levit, Balogh, Nass, & Ganz, 2013). However, research exploring the needs and experiences of caregivers for individuals with cancer is limited in the context of Danish healthcare services and often focuses on specific illnesses and related symptoms instead of the general challenges and experiences related to caring for an individual with cancer.
Caregiving for an individual with cancer has proven to have a severe impact on the physical, emotional, and psychological health of the caregiver (Deeken, Taylor, Mangan, Yabroff, & Ingham, 2003; Molassiotis, Zheng, Denton-Cardew, Swindell, & Brunton, 2010; Papastavrou, Charalambous, & Tsangari, 2009; Yildiz, Karakaş, Güngörmüs, & Cengiz, 2017). Girgis et al. (2013) conducted a longitudinal survey, including 547, 519, and 443 caregivers at 6, 12, and 24 months after the care recipient’s diagnosis, respectively. The study found that unmet needs increased over time in relation to caregivers’ anxiety and depression. Jepsen (2015) found that caregivers experienced additional burden when care was provided in an outpatient treatment facility. Dieperink, Coyne, Creedy, and Østergaard (2018) found that, compared to patients, caregivers reported receiving less emotional support from nurses.
Caregivers face potential caregiver burden because of disrupted schedules and financial problems (Hartnett, Thom, & Kline, 2016). A review by Ge and Mordiffi (2017) found that the burden is specific to caregivers for older adults with cancer, caregivers who are of younger age, those caring for individuals with solid tumors, and caregivers providing assistance with patients’ activities of daily living. Adelman, Tmanova, Delgado, Dion, and Lachs (2014) also examined the risk factors for caregiver burden and concluded that female gender, low educational attainment, cohabiting, high number of hours spent caregiving, depression, social isolation, financial stress, and lack of choice in being a caregiver are important factors for experiencing caregiver burden. Being a caregiver for an individual with cancer presents challenges for all caregivers involved, not only for those cohabiting with the patient. Lund, Ross, Petersen, and Groenvold (2014) suggested that challenges are not directly related to the nature of relation between caregiver and patient.
Berry, Dalwadi, and Jacobson (2016) described caregivers’ sense of control and self-efficacy as important relative to perceived support, and they proposed empowering caregivers by assisting proactively in caregiver duties.
Supportive interventions targeting caregivers were identified in a review by Frambes, Given, Lehto, Sikorskii, and Wyatt (2018) as the following:
• Psychoeducation relative to the patient’s disease
• Skill development for coping, communication, and problem solving
• Counseling for reactions to caring for an individual with cancer
Frambes et al. (2018) noted the importance of research focusing on new categories of supportive interventions for caregivers as standards of care evolve and nursing interventions continue to emerge for symptom management. Research underpins the need for further studies on advancing the development of interventions designed to improve outcomes for caregivers (Kent et al., 2016).
The overall aim of the current study was to investigate the needs of caregivers for individuals with cancer in Danish outpatient settings and to explore how to support caregivers.
Methodologic Approach
This study is a qualitative study using focus group interviews. Data were analyzed in a hermeneutics framework. When applying a hermeneutic approach, subjective experiences are essential for the interpretation of the dataset, and understanding is considered to be a dialogic, practical, situated activity, which is essential to the process of the “fusion of horizons” (Gadamer, 2004, p. 256). The purpose of this study was to investigate caregivers’ perspectives on their need for support, which aligns well with choosing qualitative methodology using focus groups, allowing for exploration of the caregivers’ experiences. To organize the process of the analysis, the steps from systematic text condensation were followed (Malterud, 2012b).
Participants and Setting
The participants were purposively recruited from three outpatient clinics at the Department of Oncology and Haematology, Odense University Hospital, located in the municipality of Southern Denmark. Participants were included in focus group interviews conducted from December 2017 to January 2018. Descriptive data (age, gender, education level, relationship to patient, and patient’s diagnosis) were collected from all participants upon attending the sessions. In the current study, caregivers were defined according to the following definition of family by Wright, Watson, and Bell (1996): “A group of individuals who are bound by strong emotional ties, a sense of belonging, and a passion for being involved in one another’s lives” (p. 46). Applying this definition made it possible to recruit caregivers related by blood and caregivers who were emotionally committed without the necessity of being family.
Participation was not related to a specific cancer diagnosis, stage of cancer, or treatment. Caregivers for patients who did not give informed consent to contact their caregivers, and caregivers who did not speak Danish were excluded. The authors sought to vary the composition of participants in the focus groups with regard to gender, age, and relationship to patient. The selection of participants was expected to ensure group heterogeneity to allow discussions concerning experiences and perspectives on support.
Focus Groups
Focus groups allow access to caregivers’ experiences from interactions between caregivers in similar situations (Malterud, 2012a). A semistructured interview guide steered the focus group interviews and included wide and open questions that allowed participants to share sensitive information and experiences. The focus of the questions was keeping the discussions on the caregivers and not the patients. The guide included caregivers’ experiences and needs, and their opinions on support. The participants were encouraged to actively participate and share their points of view, even if they were in contrast to those of other participants. The first focus group was conducted as a pilot test of the interview guide and the prompts and probes (Alexandra Instituttet, 2012; Nielsen, 2011). The probes and interview guide were modified based on the pilot test to ensure the validity of the study. The pilot test provided relevant data on the topic, despite the need for adjusting questions and exercises; therefore, the data from the pilot test were fully incorporated into the analysis. Either the first or second author facilitated the sessions, which took place in a conference room at the hospital. An observer was present to capture group interactions, write field notes, and validate the content of the discussions. The observer was the third or last author. The senior researchers have extensive experience conducting qualitative research, including focus group sessions. The authors also have extensive experience working as clinical nurses with patients with cancer and their caregivers. However, no authors were directly involved in the care and treatment of the patients related to the caregivers included in the study.
Systematic Text Condensation
For analysis of transcripts of the focus groups, Malterud’s (2011, 2012b) systematic text condensation was followed. The focus group sessions were recorded, transcribed verbatim, coded, and analyzed by the first and second authors. Systematic text condensation presents a systematic approach for thematic analysis of qualitative data and entails a process of intersubjectivity, reflexivity, and feasibility (Malterud, 2012b). Systematic text condensation consists of the following four steps:
• Total impression: from chaos to themes
• Identifying meaningful units: from themes to codes
• Condensation: from code to meaning
• Synthesizing: from condensation to descriptions and concepts
Initially, the transcripts were read in their entirety, separately by the authors, and then discussed to identify themes and codes in the data. Table 1 provides an example of the process of analysis. Coding and analysis of the data were done in NVivo, version 11. 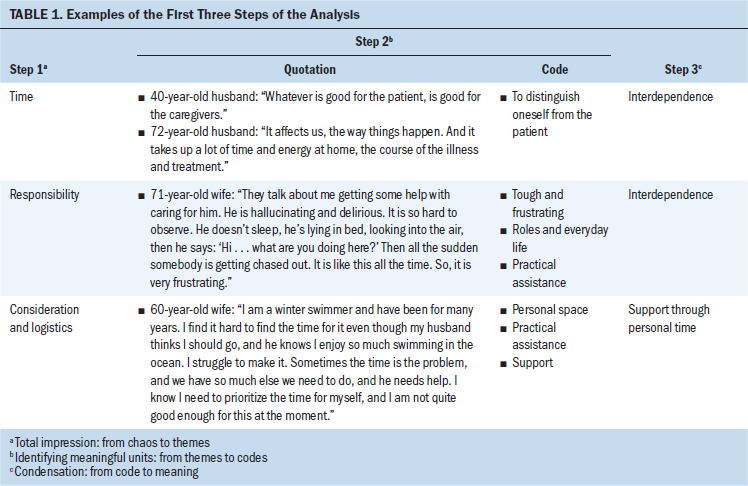
Ethical Considerations
Informed consent was obtained from all participants included in the study. Information about the study was given verbally and in writing. Consent to contact the caregiver was initially obtained from the patient and subsequently from the caregivers themselves. Sensitive information gathered in this study has been anonymized, and all data are managed confidentially. The participants were free to withdraw from the study at any time. All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments (World Medical Association, 2008). The study is registered with the Danish Data Protection Agency (no. 17/30425), and the data are stored securely in Microsoft SharePoint®.
Findings
Participants
The authors obtained informed consent from 109 individuals with cancer to contact their caregivers. Caregivers were contacted by telephone or email or approached in person. Ninety-three caregivers responded to the inquiry, and 74 consented to participate in focus group interviews; 19 declined participation because they did not want to make the extra trip to the hospital, they could not leave the patient unattended, they had an illness, or they had no perceived needs. Twenty-seven of the 74 caregivers canceled or did not attend the sessions for previously mentioned reasons, leaving 47 caregivers for interviews. Nine focus groups were conducted, with three focus groups from each outpatient clinic: the oncology outpatient clinic, the hematology outpatient clinic, and the radiation treatment facility. Data did not suggest differences in demographic characteristics among the participants who took part and those who declined or did not attend. The comparison between participants’ and nonparticipants’ demographic characteristics was based on impression rather than statistical analysis. Each focus group consisted of 3–10 caregivers and lasted 1.5–2 hours. The population of participants consisted mostly of women (n = 32) and wives (n = 22), and a total of 31 participants were aged 60 years or older. Time since the primary diagnosis ranged from zero months to more than two years. See Table 2 for additional sociodemographic characteristics of participants. [[{"fid":"53771","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
Themes and Subthemes
Two main themes emerged during the analysis, and additional subthemes were revealed during interpretation. The theme of interdependence contained the following subthemes: responsibility, a moral obligation and loneliness and talking. The second theme, different needs for support, contained the following three subthemes: support through personal time, support through peers, and support through talking to healthcare professionals.
Interdependence
Throughout the focus groups, it became clear that caregivers did not distinguish their own needs and perspectives on support from the needs and support of the patient. This was illustrated by the fact that they often said “we” instead of “I” when they talked about their needs. There is a mutual dependency between the caregiver and the patient with cancer; caregivers describe patients needing practical and emotional assistance, and caregivers are dependent because of the emotional ties between the caregiver and the patient.
In addition, caregivers described having needs of their own that were not being fulfilled. Often, the unmet needs stemmed from disabilities and difficulties concerning the patient but ended up being an important area of concern for the caregivers themselves.
Responsibility, a moral obligation: Some caregivers found being a resource for the patient without being cared for themselves to be particularly challenging and stressful. They described that responsibility related to treatment, home chores, and handling medicine was left to the caregivers, deliberately or unconsciously, and this was experienced by husbands, daughters, friends, and wives and was not connected to a specific relationship between caregiver and patient. A 55-year-old wife talked about taking on the responsibilities as a moral obligation: “It’s like, from the day he fell ill, we turned on a switch. I discovered that, now, everything is my responsibility.”
The caregivers described taking on responsibility because of the patient’s illness and accepting this without hesitation and without question. The caregivers described a change in their everyday lives because the patients suddenly became weak from the illness or treatment. This resulted in caregivers not leaving the patient because they found their physical presence to be important for the patient. A 75-year-old husband referred to his wife’s dependency on his assistance:
I have to keep an eye on her, because when her head drops, I have to see if she’s breathing. We have been picked up by the ambulance a few times, because she needed oxygen, so I couldn’t take her to hospital myself.
Taking on responsibility also refers to caregivers monitoring results of blood tests and scans, and keeping updated on complementary treatment. The focus group discussions showed that caregivers withdrew from social arrangements and limited visits at home to avoid the patient being exposed to infections. Although caregivers took precautions, they also referred to the importance of maintaining everyday life as it was before the patient became ill.
Loneliness and talking: Some caregivers struggled to make room for sharing and talking about their situation and experiences. A 66-year-old husband described the following: “My wife is not particularly interested in talking to someone about it. She withdraws into herself. It doesn’t make it easy either, because I’m more outgoing.”
The caregivers reported that some patients were silent and rejected talking about their illness. A 43-year-old daughter talked about needing to verbalize the situation to make sense and counteract hopelessness:
I am the kind of person who needs to talk about everything, about the practicalities, about going to the hospital, and things like this. But I was cut off, and . . . she did not want to talk about it, she did not want to hear about it, and she could not handle hearing about it. . . . Then, there was silence. And I had to respect her wish, and yet I hope she will be ready to talk about it.
The caregivers needed to talk to someone and address their experiences and the patient’s illness. However, they found it stressful if they constantly had to talk about the illness with the patient, relatives, friends, and healthcare professionals, and constantly were confronted with challenges and the uncertainty associated with the illness.
Different Needs for Support
Support through personal time: Some caregivers found it hard to find personal time despite support from the patient. Caregivers described regulating their personal time depending on the well-being of the patient. A 66-year-old husband described having to fight for personal time; as the illness progressed, it became harder for him to prioritize himself: “It is something I’ve had to fight for. Even though I’m not away much, my wife thinks I am gone too much. And, it has become more distinct with time.”
Caregivers described activities, such as making chocolate, cycling exercises, or bird watching, that allow them to spend time away from the patient and prioritize their own interests, depending on the well-being of the patient. The need for personal time was described by caregivers of newly diagnosed patients and caregivers for patients who had been ill for years.
Support through peers: Caregivers stressed the significance of having peer support. However, the establishment of contact between peers was somewhat random and depended on their own efforts. A 62-year-old husband talked about his experience with support from a peer: “I still work a little, and at my job there’s a female colleague, almost my age, who had experienced something similar, . . . and I felt that we supported each other and talked openly.”
In all group sessions, the participants discussed the importance of peer support. Peers were considered to be contributing to support on a different level than support provided by healthcare professionals. Caregivers were unable to point out a specific need but agreed on having unmet needs. A 29-year-old daughter referred to peers and not being able to specify her needs: “Your family has their own life. It is hard to find a confidant to turn to and admit you need help. This is hard for me. Also, I don’t always know what I need help for.”
The discussions revealed that caregivers find it problematic that they themselves are responsible for seeking out the needed peer support. Despite most caregivers being aware of existing peer group facilities, most caregivers did not make use of the available counseling. A 52-year-old wife talked about the discrepancy between knowing and going: “I have been wanting to go, but I have not managed to do it on my own.”
It became evident that caregivers found it hard to find and contact peers themselves. Some participants considered participating in the focus groups a relief and a place to be met with understanding regarding the frustration and challenges they experience providing care. Two caregivers exchanged telephone numbers before parting because they mirrored and related to each other.
Support through talking to healthcare professionals: It became apparent when discussing support and healthcare professionals that caregivers were responsible for seeking out support themselves. The participants’ experiences with support indicated that support for caregivers is not systematic and is defined by the person they encounter.
Some of the caregivers did not want more information than what the patient asked for, whereas other caregivers considered talking to healthcare professionals without the patient being present as potential support. A 35-year-old daughter shared the following:
I could have benefited from talking to a doctor or a nurse without my mom being present. She and I have had a rough time, so I’ve constantly been considerate of my mom. I didn’t want to make her sad, because she’s the one who’s ill.
The need for talking to healthcare professionals without the patient being present was not related to a specific time; rather, it was considered supportive in the context of individuals with multimorbidity and life-threatening illness. In addition, the caregivers said that caregivers could be supported by seemingly ordinary actions, such as healthcare professionals greeting the caregivers or offering them a cup of coffee.
Discussion
This study explored the needs of caregivers for individuals with cancer in an outpatient setting and how caregivers can be supported. The overall findings of this study showed that caregivers’ need for support is influenced by the interdependency between the caregiver and the individual with cancer. Caregivers have unmet needs, and they described the need for conversations with healthcare professionals without the patient being present, as well as support through peers. Caregivers also explained that having personal time is crucial for their well-being because of the extensive responsibilities they take on by providing care.
Interdependency and Interventions
One main finding in this study was the caregivers’ experience that their needs are inseparable from the needs of the patients. The connection between the needs and experiences of caregivers and patients is consistent with a review by Northouse, Williams, Given, and McCorkle (2012), which described that interventions targeting caregivers alone or targeting caregivers and patients jointly have a positive effect on caregiver and patient outcomes. Ferrell and Wittenberg (2017) explored interventions targeting caregivers in 50 randomized controlled trials (RCTs) from 2010 to 2016 and found an increasing number of RCTs and interventions focusing primarily on caregivers, despite the study also demonstrating couple-based interventions to be most effective in improving communication, distress, and relationship functioning.
Nursing based on a family nursing method of care derived from systemic theory addresses patients and their caregivers and the interdependency in the relationship between the two (Wright & Bell, 2009; Wright & Leahey, 2012). This is in line with the findings of the current study, demonstrating that caregivers want to be addressed by healthcare professionals and need to be recognized not only as a caregiver for the patient, but also as an individual with needs of his or her own. Therefore, optimizing support for caregivers, in terms of design and targeting of support interventions, should include the caregiver and patient together.
Support When Needed
Caregivers in the current study described being supported randomly depending on the healthcare professional they encounter, rather than by systematized support interventions. Caregivers are not sure what they need help for but are in need of emotional and practical support from peers, regardless of the patient’s cancer diagnosis, stage, and prognosis. This is in line with Walshe et al. (2017), who described caregivers themselves being responsible for seeking out support from healthcare professionals. Peer support, as described by Solomon (2004), is seen as an embodiment of a strong message of hope and experience that reaches beyond the scope of traditional treatment and can be used in many different contexts (Repper et al., 2013). The finding that peer support is not dependent on the specifics of the illness is in keeping with Timm, Glasdam, and Vittrup (2007), who argued that the wider the effect of the illness and symptoms, the greater the burden on the caregivers. Therefore, caregiver burden makes it harder to create balance in life as a caregiver, because of a change in social, economic, physical, and emotional conditions (Timm et al., 2007). Benzein, Olin, and Persson (2015) described the effect of family interventions in relation to chronic illness and caregivers’ challenges regarding obtaining the support they need. Therefore, caregivers could benefit from peers with whom they can relate to in terms of burden and challenges and whom they could use as a role model, leading the way when they feel insecure.
Coping Interventions
Family nursing is a nursing theory that integrates assessing techniques based on systemic theory and identifies caregivers as part of intertwined and complex systems (Wright & Bell, 2009; Wright & Leahey, 2012). Family nursing provides healthcare professionals with an approach to accommodating caregivers’ individual needs for support so they can grow as a family, considering the interdependency between the caregiver and the patient.
Likewise, family nursing could be a way for healthcare professionals to accommodate caregivers’ need for personal time, with insight through the unique knowledge of which functions support or strain a family, allowing for healthcare professionals to provide support for the family as a unit as required (Wright & Leahey, 2012). In the study by Walshe et al. (2017), caregivers described the impact of self-management on their coping. This is consistent with the current study, in terms of the caregivers describing activities like making chocolate, cycling exercises, or bird watching as activities that allowed them to spend time away from the patient and prioritize their own interests.
The participants had different relationships with the patients; some cohabited, and others did not share living arrangements. The sense of responsibility and burden was related to caregivers’ possibility of having time away from the patient, leaving caregivers who lived with the patient to struggle more to create personal time. In addition, the experiences and feelings of burden among the participants differed, depending on the role they filled, such as mother or daughter. Spouses, by definition, took on the caring role, whereas others, such as daughters, also took care of the patient but often had trouble balancing caregiving with the other parts of their lives, like studying, working, or parenting.
Addressing the Interdependency
Caregivers in the current study described experiencing support by talking to healthcare professionals without the patient being present; this interaction provides caregivers with an overview and allows healthcare professionals to convey information to the caregivers. Also, for some caregivers, the possibility of asking questions provides possible relief and resolution because, with the patient present, caregivers hold back their own needs and questions for the sake of not hurting the patient. Conversations could be with healthcare professionals associated with the outpatient clinic or healthcare professionals with no association with the patient’s treatment. The topic of a team working around the patient was discussed by Foxwell and Scott (2011), who described the cooperation related to the patient as important for gaining trust between caregivers and healthcare professionals. In the study by Walshe et al. (2017), communication with healthcare professionals was also highlighted as important to caregivers’ perception of support but was not described without the patient being present. The population of the study by Walshe et al. (2017) investigated caregivers and patients together rather than caregivers on their own, as in the current study. The differences in design and sample could allow for different perspectives on caregivers’ experience of and perspectives on support. This may explain Walshe et al. (2017) not describing the need for talking with healthcare professionals without the patient being present. There may be legal problems if the patient does not allow the caregivers to talk with healthcare professionals on their own. The need for talking to healthcare professionals with or without the patient being present could be identified through family nursing by making ecomaps and outlining the responsibilities and considerations internally in the family. This contributes to healthcare professionals gaining insight into families being dysfunctional and patients needing assistance from family during the illness. This is important with regard to assessment of the need for support interventions for the family (Carlstedt, 2016).
Strengths and Limitations
Overall, the large sample of participants represents variation in diagnosis, time since diagnosis, patient–caregiver relation, gender, and age, providing a comprehensive picture of the caregiving experience. Caregivers who agreed to participate in the study may represent caregivers who are resourceful and have the prerequisites to cope in a way that reduces their stress and burden. However, the study showed that participants in the focus group interviews described and discussed the challenges and experiences consistent with previous research in the field (Girgis et al., 2013; Harding, List, Epiphaniou, & Jones, 2012; Leonidou & Giannousi, 2018).
Participants representing different cancer diagnoses and stages in their family could be a possible limitation, supposing experiences and challenges related to the specific diagnosis and stage of the illness trajectory had the consequence that participants would not be able to address their need for support and relate to each other. However, this was not an issue; in fact, the similarities regarding experiences, challenges, and perspectives on support were across diagnosis, stage, gender, age, and patient–caregiver relation, making diversity a strength of this study.
It is unclear the exact number of patients who initially were approached, which complicates the overall assessment of representation. Some caregivers declined participation because they did not perceive any needs in their caring role, which could present a limitation in this study. Mainly including caregivers who did experience caregiving as burdensome may influence the generalizability of the findings.
The sample size and heterogeneity of participants is a strength, allowing for capturing of challenges and opinions related to a wide range of patient–caregiver relations. The results cannot claim statistical generalizability, but analytical generalization emerges based on the interactions between theory and practice (Tanggaard & Brinkmann, 2010).
The heterogeneity of participants included caregivers at multiple points of the cancer trajectory, presenting experiences and views on support specifically related to a variety of challenges, making it possible to explore the needs of caregivers and to explore how caregivers can be supported. In addition, the study is strengthened by following the steps of systematic text condensation, which contributes to maintaining academic rigor through a process of reflexivity, ensuring the relevance and validity of the study (Malterud, 2011, 2012b).
Implications for Nursing
To improve care for caregivers currently and in the future, it is important to assess, recognize, and respond to caregivers’ need for support through having personal time, peer support, and opportunities to talk to healthcare professionals. This may help caregivers cope with their caregiving tasks and roles and involves taking accessible resources into account. The incorporation of a family nursing approach of care within the outpatient oncology settings may assist nurses and facilitate care with regard for the interdependency between the caregiver and the patient. Family nursing involves the whole family (Wright & Bell, 2009). Family nursing could possibly encompass the challenges and needs experienced by the patient and caregivers, allowing for healthcare professionals to take individual needs and conditions into account. 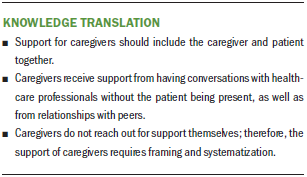
Conclusion
The current study showed that supporting caregivers in the outpatient setting should focus on the interdependency within the family, instead of solely addressing the patient or supporting caregivers by educating about patients’ needs. Support of caregivers should include support from peers, the possibility to talk to healthcare professionals, and personal time for self-care. Future studies could take into account the inclusion of caregivers who are less resourceful to ensure the heterogeneity of the participants. It would be of interest to expand the study to explore the lived experiences of caregivers with no perceived needs to determine the resources they have in caring for an individual with cancer.
About the Author(s)
Nina Ingerslev Andersen, RN, MScN, is a clinical nurse specialist and Carina Ingemann Nielsen, RN, MScN, is a research assistant, both in the Department of Oncology at Odense University Hospital; Dorthe Boe Danbjørg, RN, PhD, is an associate professor in the Department of Clinical Research at the University of Southern Denmark and the Department of Haematology and Centre for Innovative Medical Technology at Odense University Hospital; Pia Krause Møller, RN, MPH, is a doctoral student in the Department of Oncology at Odense University Hospital; and Karin Dieperink Brochstedt, RN, PhD, is an associate professor in the Academy of Geriatric Cancer Research in the Department of Oncology at Odense University Hospital and the Family Focused Healthcare Research Center in the Department of Clinical Research at the University of Southern Denmark, all in Denmark. This study was funded, in part, by grants from AgeCare, the Academy of Geriatric Cancer Research Group, and the Novo Nordisk Foundation (NNF17Oc0028688). All authors contributed to the conceptualization and design and the manuscript preparation. Andersen, Nielsen, Møller, and Brochstedt completed the data collection. Brochstedt provided statistical support. Andersen, Nielsen, Danbjørg, and Brochstedt provided the analysis. Andersen can be reached at nina.ingerslev.andersen@rsyd.dk, with copy to ONFEditor@ons.org. (Submitted September 2018. Accepted March 20, 2019.)
References
Adelman, R.D., Tmanova, L.L., Delgado, D., Dion, S., & Lachs, M.S. (2014). Caregiver burden: A clinical review. JAMA, 311, 1052–1060. https://doi.org/10.1001/jama.2014.304
Alexandra Instituttet. (2012). Brugerdreven innovation: Metodekort. Retrieved from https://alexandra.dk/sites/default/files/downloads/Metodekatalog.pdf
Australian Government, Department of Social Services. (2018). New services for carers. Retrieved from https://www.dss.gov.au/sites/default/files/documents/04_2018/fact_sheet…
Benzein, E., Olin, C., & Persson, C. (2015). ‘You put it all together’—Families’ evaluation of participating in Family Health Conversations. Scandinavian Journal of Caring Sciences, 29, 136–144. https://doi.org/10.1111/scs.12141
Berry, L.L., Dalwadi, S.M., & Jacobson, J.O. (2016). Supporting the supporters: What family caregivers need to care for a loved one with cancer. Journal of Oncology Practice, 13, 35–41. https://doi.org/10.1200/JOP.2016.017913
Carlstedt, E. (2016). Familien i sundhedsvæsenet. In B. Østergaard & H. Konradsen (Eds.), Familiesygepleje (pp. 13–25). København, Denmark: Munksgaard.
Danske Regioner, KL, Økonomi- Og Indenrigsministeriet, Finansministeriet, & Ministeriet for Sundhed og Forebyggelse. (2013). Bedre incitamenter i sundhedsvæsenet. Retrieved from https://bit.ly/2lolo6U
Deeken, J.F., Taylor, K.L., Mangan, P., Yabroff, K.R., & Ingham, J.M. (2003). Care for the caregivers: A review of self-report instruments developed to measure the burden, needs, and quality of life of informal caregivers. Journal of Pain and Symptom Management, 26, 922–953.
Dieperink, K.B., Coyne, E., Creedy, D.K., & Østergaard, B. (2018). Family functioning and percieved support from nurses during cancer treatment among Danish and Australian patients and their families. Journal of Clinical Nursing, 27, e154–e161. https://doi.org/10.1111/jocn.13894
Ferrell, B., & Wittenberg, E. (2017). A review of family caregiving intervention trials in oncology. CA: A Cancer Journal for Clinicians, 67, 318–325. https://doi.org/10.3322/caac.21396
Foxwell, K.R., & Scott, S.E. (2011). Coping together and apart: Exploring how patients and their caregivers manage terminal head and neck cancer. Journal of Psychosocial Oncology, 29, 308–326. https://doi.org/10.1080/07347332.2011.563343
Frambes, D., Given, B., Lehto, R., Sikorskii, A., & Wyatt, G. (2018). Informal caregivers of cancer patients: Review of interventions, care activities, and outcomes. Western Journal of Nursing Research, 40, 1069–1097. https://doi.org/10.1177/0193945917699364
Gadamer, HG. (2004). Sandhed og metode: Grundtræk af en filosofisk hermeneutik (pp. 101–125, 253–292). Århus, Denmark: Systime Academic.
Ge, L., & Mordiffi, S.Z. (2017). Factors associated with higher caregiver burden among family caregivers of elderly cancer patients: A systematic review. Cancer Nursing, 40, 471–478. https://doi.org/10.1097/NCC.0000000000000445
Girgis, A., Lambert, S.D., McElduff, P., Bonevski, B., Lecathelinais, C., Boyes, A., & Stacey, F. (2013). Some things change, some things stay the same: A longitudinal analysis of cancer caregivers’ unmet supportive care needs. Psycho-Oncology, 22, 1557–1564. https://doi.org/10.1002/pon.3166
Harding, R., List, S., Epiphaniou, E., & Jones, H. (2012). How can informal caregivers in cancer and palliative care be supported? An updated systematic literature review of interventions and their effectiveness. Palliative Medicine, 26, 7–22. https://doi.org/10.1177/0269216311409613
Hartnett, J., Thom, B., & Kline, N. (2016). Caregiver burden in end-stage ovarian cancer. Clinical Journal of Oncology Nursing, 20, 169–173. https://doi.org/10.1188/16.CJON.169-173
Jemal, A., & Torre, L.A. (2018). The global burden of cancer. In The American Cancer Society’s principles of oncology: Prevention to survivorship (pp. 33–44). Atlanta, GA: Wiley.
Jepsen, L.Ø. (2015). Outpatient management of acute leukemia patients: The experience of patients and their relatives. (Doctoral thesis, University of Southern Denmark, Odense, Denmark). Retrieved from https://findresearcher.sdu.dk:8443/ws/portalfiles/portal/121499104/Outp…
Kent, E.E., Rowland, J.H., Northouse, L., Litzelman, K., Chou, W.Y., Shelburne, N., . . . Huss, K. (2016). Caring for caregivers and patients: Research and clinical priorities for informal cancer caregiving. Cancer, 122, 1987–1995.
Leonidou, C., & Giannousi, Z. (2018). Experiences of caregivers of patients with metastatic cancer: What can we learn from them to better support them? European Journal of Oncology Nursing, 32, 25–32. https://doi.org/10.1016/j.ejon.2017.11.002
Levit, L.A., Balogh, E.P., Nass, S.J., & Ganz, P.A. (2013). Delivering high-quality cancer care: Charting a new course for a system in crisis. Washington, DC: National Academies Press.
Lund, L., Ross, L., Petersen, M.A., & Groenvold, M. (2014). Cancer caregiving tasks and consequences and their associations with caregiver status and the caregiver’s relationship to the patient: A survey. BMC Cancer, 14, 541. https://doi.org/10.1186/1471-2407-14-541
Malterud, K. (2011). Kvalitative metoder i medisinsk forskning: En innføring (3rd ed.). Oslo, Norway: Universitetsforlaget.
Malterud, K. (2012a). Fokusgrupper som forskningsmetode for medisin og helsefag. Oslo, Norway: Universitetsforlaget.
Malterud, K. (2012b). Systematic text condensation: A strategy for qualitative analysis. Scandinavian Journal of Public Health, 40, 795–805. https://doi.org/10.1177/1403494812465030
Molassiotis, A., Zheng, Y., Denton-Cardew, L., Swindell, R., & Brunton, L. (2010). Symptoms experienced by cancer patients during the first year from diagnosis: Patient and informal caregiver ratings and agreement. Palliative and Supportive Care, 8, 313–324. https://doi.org/10.1017/S1478951510000118
Nielsen, L. (2011). Persona. Aarhus, Denmark: Universitetsforlag.
Northouse, L., Williams, A.L., Given, B., & McCorkle, R. (2012). Psychosocial care for family caregivers of patients with cancer. Journal of Clinical Oncology, 30, 1227–1234. https://doi.org/10.1200/JCO.2011.39.5798
Papastavrou, E., Charalambous, A., & Tsangari, H. (2009). Exploring the other side of cancer care: The informal caregiver. European Journal of Oncology Nursing, 13, 128–136. https://doi.org/10.1016/j.ejon.2009.02.003
Repper, J., Aldridge, B., Gilfoyle, S., Gillard, S., Perkins, R., & Rennison, J. (2013). Peer support workers: Theory and practice. Retrieved from https://www.centreformentalhealth.org.uk/sites/default/files/2018-09/Im…
Solomon, P. (2004). Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatric Rehabilitation Journal, 27, 392–401. https://doi.org/10.2975/27.2004.392.401
Sundhedsdatastyrelsen. (2016). FAKTAANALYSE—Kræftområdet 2007–2014. Retrieved from https://sundhedsdatastyrelsen.dk/-/media/sds/filer/find-tal-og-analyser…
Sundhedsdatastyrelsen. (2017). Nye kræfttilfælde i Danmark. Retrieved from https://sundhedsdatastyrelsen.dk/-/media/sds/filer/find-tal-og-analyser…
Sundhedsstyrelsen. (2016). Styrket indsats på kræftområdet: Fagligt oplæg til Kræftplan IV. København, Denmark: Sundhedsstyrelsen. Retrieved from http://www.sum.dk/Aktuelt/Nyheder/Kraeft/2016/Juli/~/media/FINAL%20Fagl…
Tanggaard, L., & Brinkmann, S. (2010). Interviewet: Samtalen som forskningsmetode. In L. Tanggaard & S. Brinkmann (Eds.), Kvalitative metoder: En grundbog (pp. 29–53). København, Denmark: Hans Reitzels Forlag.
Timm, H., Glasdam, S., & Vittrup, R. (2007). Sundhedsfaglige interventioner rettet mod pårørende til mennesker med kronisk sygdom – en systematisk litteraturgennemgang. København, Denmark: Sundhedsstyrelsen.
Walshe, C., Roberts, D., Appleton, L., Calman, L., Large, P., Lloyd-Williams, M., & Grande, G. (2017). Coping well with advanced cancer: A serial qualitative interview study with patients and family carers. PLOS ONE, 12, e0169071. https://doi.org/10.1371/journal.pone.0169071
World Medical Association. (2008). Declaration of Helsinki 2008. Retrieved from https://www.wma.net/wp-content/uploads/2016/11/DoH-Oct2008.pdf
Wright, L.M., & Bell, J.M. (2009). Beliefs and illness: A model for healing. Calgary, Alberta, Canada: 4th Floor Press.
Wright, L.M., & Leahey, M. (2012). Nurses and families: A guide to family assessment and intervention. Philadelphia, PA: F.A. Davis.
Wright, L.M., Watson, W.L., & Bell, J.M. (1996). Beliefs: The heart of healing in families and illness. New York, NY: Basic Books.
Yildiz, E., Karakaş, S.A., Güngörmüs, Z., & Cengiz, M. (2017). Levels of care burden and self-efficacy for informal caregiver of patients with cancer. Holistic Nursing Practice, 31, 7–15. https://doi.org/10.1097/HNP.0000000000000185




