Exploring Nurses’ Understanding of Anticipatory Nausea and Vomiting in Patients With Cancer
Purpose: To explore nurses’ self-reported understanding of anticipatory nausea and vomiting (ANV) in patients with cancer.
Participants & Setting: 12 oncology RNs were recruited from University Hospital Limerick in Ireland.
Methodologic Approach: Data were collected via semistructured interviews and analyzed using a qualitative content analysis approach with a focus on the manifest content.
Findings: The following themes were identified: (a) predispositions for and previous experiences with ANV, (b) distinct uncertainties surrounding the prevalence of ANV, (c) individual patient associations with ANV, (d) clear understanding of nausea and vomiting, (e) uncertainty surrounding the management of ANV, and (f) the negative impact of ANV.
Implications for Nursing: Although oncology nurses may understand the importance of assessing and treating patients on an individual basis throughout the course of treatment, formal ANV assessments are warranted to ensure the implementation of best practice. The findings of the current study can guide oncology nurses’ approach to the assessment and management of ANV.
Jump to a section
According to the National Cancer Institute ([NCI], 2018), anticipatory nausea and vomiting (ANV) is a learned response to previous chemotherapy treatment and is identified as an experience of nausea and vomiting that may begin while patients are preparing for their next chemotherapy treatment (Roila et al., 2016). ANV can occur in response to the sights, sounds, and smells that a patient associates with previous treatment (Aapro, 2018; NCI, 2018; Roila et al., 2016). Entering the chemotherapy unit, seeing chemotherapy drugs, or even realizing that the next cycle of treatment is approaching can precipitate ANV (Aapro, 2018; Jordan, Schaffrath, Jahn, Mueller-Tidow, & Jordan, 2014; NCI, 2018). ANV is frequently presented in the literature as chemotherapy-induced nausea and vomiting (CINV) (National Comprehensive Cancer Network [NCCN], 2018; NCI, 2018). As a result, ANV and CINV are often not clearly differentiated.
Background
According to Dranitsaris et al. (2017) and Aapro (2018), as many as 40% of patients with cancer receiving chemotherapy fail to achieve complete nausea and vomiting control, with ANV occurring in 29% of patients with cancer (NCI, 2018). A study by Roscoe, Morrow, Aapro, Molassiotis, and Olver (2011) indicates that as many as 25% of patients will develop ANV by the fourth cycle of chemotherapy treatment. Female patients who are aged 50 years or younger are at a higher risk for developing ANV. Additional risk factors for ANV include experiencing nausea and vomiting following the last chemotherapy session, susceptibility to motion sickness, having a high level of anxiety, the emetogenic potential of the chemotherapy drug administered, and having a history of morning sickness during pregnancy (Aapro, 2018; Clark-Snow, Affronti, & Rittenberg, 2018; NCI, 2018; Roila et al., 2016). Previous studies have indicated that whether the patient experienced nausea and vomiting following previous treatment is the strongest predictor of ANV during additional cycles of chemotherapy (Aapro, 2018; Chan et al., 2015; Molassiotis et al., 2016). In addition, the study by Dranitsaris et al. (2017) suggests that the number of hours of sleep a patient gets the night before treatment with chemotherapy and self-medication with nonprescription treatments are additional risk factors for ANV.
CINV, of which ANV is often subsumed, is described by patients with cancer as one of the most feared side effects of chemotherapy (Aapro, 2018). CINV and its symptoms can lead to withdrawal or delay of chemotherapy treatment, nutrition depletion, and deterioration in physical functioning (Chung et al., 2011; Dranitsaris et al., 2017; NCI, 2018). Severe CINV can also result in prolonged hospitalization, depression, and increased healthcare costs (Aapro, 2018; Clark-Snow et al., 2018; Dranitsaris et al., 2017; NCI, 2018). A study by Clark-Snow et al. (2018) examined nurses’ awareness and perception of CINV, as well as the use of CINV guidelines, and barriers to effective care. Nurses in the Clark-Snow et al. (2018) study reported that they understood the risk factors for developing CINV, but that CINV was often poorly controlled in their patient cohort. Antiemetics were preferred for patient care by physicians; however, nurses recognized the need for more efficient communication among physicians, nurses, and patients, as well as the use of a standardized assessment tool, to increase the awareness and management of CINV (Clark-Snow et al., 2018). Although several CINV assessment tools examine the side effects of chemotherapy, such as the Multinational Association of Supportive Care in Cancer (MASCC) Antiemesis Tool (Molassiotis et al., 2007), the Patient-Reported Outcomes Measurement Information System gastrointestinal symptom scales (Spiegel et al., 2014), and the Rhodes Index of Nausea, Vomiting, and Retching (RINVR) (Moradian et al., 2014), none of these established tools identify and assess ANV alone. The RIVNR tool does, however, assess nausea, vomiting, and retching during the 2 to 24 hours prior to treatment (Moradian et al., 2014), allowing for ANV pretreatment to be identified and assessed. A personalized approach to patient assessment that incorporates individual risk factors is warranted (Clemons, 2018; Dranitsaris et al., 2017; Kamen et al., 2014). The MASCC and European Society for Medical Oncology (ESMO) antiemetic guidelines endorse benzodiazepines as the only drugs that can reduce the occurrence of ANV (MASCC and ESMO, 2016). The American Society for Clinical Oncology and MASCC and ESMO guidelines also indicate that ANV is best managed by initiating the recommended acute and delayed antiemetics for the chemotherapy protocol prescribed (Hesketh et al., 2017; MASCC and ESMO, 2016). In addition, previous studies have suggested that the best approach to preventing ANV is the optimal management of CINV during each chemotherapy treatment (Aapro, 2018; Molassiotis et al., 2016).
The current study was developed to identify and understand the risk factors for and prevalence of ANV in a patient cohort at an acute care hospital in northern Ireland. Patients with cancer at this institution regularly express to nursing staff that they feel nauseated the day before their scheduled chemotherapy treatment; however, these patients are not formally assessed for ANV. Without adequate assessments for and an understanding of the ANV experience, the ability of nurses to deliver holistic patient-centered care is limited. Therefore, the purpose of this study was to explore nurses’ overall understanding of ANV to ensure optimal and tailored treatment for patients with cancer.
Methods
A qualitative descriptive approach was used to capture the participants’ self-reported experiences with ANV. Sandelowski (2000) describes qualitative descriptive research as the preferred method when descriptions of the who, what, and where are required. Using a qualitative descriptive approach allowed the authors to present a comprehensive summary of nurses’ understanding of caring for patients with cancer and ANV using their own words. The study was approved by the ethics committee of University Hospital Limerick in Ireland. Verbal and written consent was obtained from participants. All necessary measures were taken to ensure the anonymity and confidentiality of participants.
Participants and Setting
All participants were general RNs in the cancer services unit at University Hospital Limerick in Ireland, which provides cancer care to patients with varying diagnoses and prognoses. Nurses were eligible for participation if they were registered with the Nursing and Midwifery Board of Ireland, able to communicate in English, and provided direct care to patients with cancer. Posters were created that advertised details of the study. Potential participants responded to information presented on the poster, and a homogeneous sample of staff nurses with similar characteristics and experiences was selected (see Table 1). 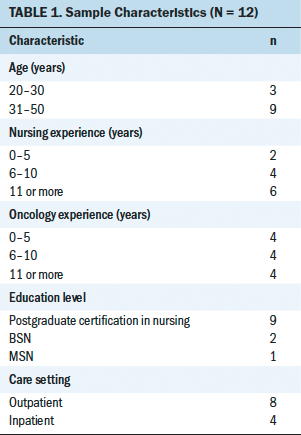
Data Collection
The lead author conducted semistructured interviews with participants from March 29 to May 7, 2016. Interviews were conducted in a private room at the hospital following written participant consent. Interviews varied in length (11–14 minutes). Participants began each interview by completing a demographic questionnaire and were then asked questions that focused on their understanding of ANV (see Figure 1). Participation selection and data analysis continued until reaching data saturation, and interviews ceased once no new themes or subthemes emerged (Streubert & Carpenter, 2011). 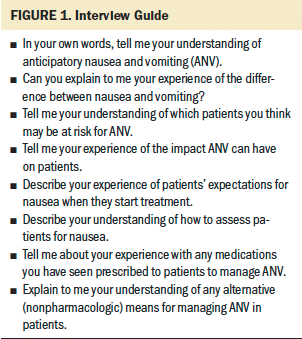
Data Analysis
Data analysis was influenced by the work of Graneheim and Lundman (2004) and focused only on manifest content (also referred to as the visual or obvious component of the data). The authors generated verbatim transcriptions of the audio-recorded interviews and read the transcripts in full to become immersed in the data. The most important points were divided into meaning units (sentences or paragraphs that were extracted according to the participants’ statements), which were then condensed into a description of the text. The condensed meaning units of four selected transcripts were then discussed to resolve any discrepancies. Meaning units were extracted from the remaining transcripts, and codes that reflected the words of the participants in a more abstract way were assigned to the units. Finally, similar codes were grouped into more comprehensive themes and subthemes. All themes and subthemes were discussed by the authors to ensure agreement.
Trustworthiness
Credibility, dependability, transferability, and confirmability were used to ensure trustworthiness (Graneheim & Lundman, 2004). A large volume of verbatim quotations, maximum variance of sampling, researcher debriefing, codes, themes, and subthemes were used to ensure credibility. An ongoing reflexive account by one of the authors describing the experience of a first-time researcher also enhanced credibility. An audit trail, comprised of detailed descriptions of the interview transcripts, codes, and themes, was provided for dependability. Including a second author in the ongoing review of the literature, field notes, transcripts, and analysis increased the dependability of this research. Sufficiently robust descriptions of nurses’ understanding of ANV in patients with cancer, with quotations, ensured transferability. The authors demonstrated confirmability by describing how conclusions and interpretations were established and exemplifying that the findings were derived directly from the participant responses. Providing an ongoing reflexive account detailing methodologic decisions, as well as a reflection of the authors’ own experiences and biases, enhanced the study’s confirmability.
Findings
Twelve female Irish nurses consented to participate in semistructured interviews. Most participants (n = 9) were aged 31–50 years, with the remaining participants (n = 3) ranging in age from 20 to 30 years. On average, participants had 11 years of nursing experience, with a mean of 8 years of experience working with patients with cancer. Nine participants had postgraduate certification in nursing, one had a master of science in nursing degree, and two had baccalaureate degrees in nursing. Eight participants worked in an outpatient hematology-oncology unit and four worked in the inpatient hematology-oncology setting.
The following six themes emerged: (a) predispositions for and previous experiences with ANV, (b) distinct uncertainties surrounding the prevalence of ANV, (c) individual patient associations with ANV, (d) clear understanding of nausea and vomiting, (e) uncertainty surrounding the management of ANV, and (f) the negative impact of ANV. The findings are presented with verbatim quotations that support the generation of each individual theme.
Predispositions and Previous Experiences
Overall, participants recognized that anxiety, fear, or nervousness prior to treatment appeared to influence a patient’s development of ANV. One nurse stated, “We had an anxious lady before she started treatment; she started retching and feeling unwell and queasy before we had even gone near her” (P2). Participants also believed that the frequency of treatment and hospital visits were directly related to the development of ANV. As one participant described, “One patient came in every two weeks, and he would be vomiting at the door of the hospital” (P12). Most participants were aware that the emetogenic potential of the prescribed chemotherapy drug is often unrelated to the development of ANV (Clemons, 2018). In addition, participants believed that patients expected to feel nauseated following treatment and often waited for the nausea to begin. A number of participants believed that depictions of chemotherapy in the media may have influenced their patients’ expectations of chemotherapy side effects: “Every movie you see will have somebody’s head in a bucket when they are [being treated with] chemotherapy; everyone gets sick on chemo according to the media” (P10).
Uncertainties Surrounding Prevalence
The majority of study participants had little to no understanding of the prevalence of ANV. Opinions on prevalence varied among the participants. One participant believed that the incidence of ANV is greater than what is reported to healthcare professionals and nursing staff. Conversely, another participant who worked in the inpatient setting believed that ANV was less prevalent than what is expected.
Individual Patient Associations
According to the participants, patients receiving chemotherapy consider treatment to be a predominantly negative experience:
They think [that] as soon as they come in the door that they are going to start retching and [feeling nauseated], and [they] associate coming in here [with] feeling sick. (P2)
In addition, participants believed that patients’ own senses may have exacerbated the development of ANV symptoms. As one participant described, “They smell a familiar smell, or hear the door opening, or see the chemo . . . [it causes] them to feel nauseated” (P1). Another participant recalled that a particular patient even associated seeing nursing staff with feeling nauseated: “She couldn’t even look into the [outpatient unit]; she associated us with nausea. When she [saw] me, she would associate me with nausea because I had treated her” (P8). Another participant described a patient who associated chemotherapy syringes with feeling nauseated. In an attempt to reduce this nausea, staff placed the chemotherapy in an infusion bag: “When she would see the syringes, she would get sick. For her, . . . to see a bag rather than syringes helped” (P9).
Understanding of Nausea and Vomiting
Each study participant had the ability to distinguish the differences between nausea and vomiting. All participants reiterated that nursing staff are at the forefront of patient assessments for nausea. Throughout the data analysis, participants notably reported that nausea and vomiting were not being assessed separately. One participant said, “You almost associate one with the other; you would assess them together” (P3). Another participant said that nausea and vomiting were definitely assessed together: “The two are related; one leads to the other” (P4). Although participants believed that they are well positioned to administer ANV assessments to patients, no participants had used a standardized nausea and vomiting assessment tool. However, the need for an ANV assessment tool was mentioned: “I don’t use an assessment tool; I suppose we could do with a tool” (P6).
Uncertainty Surrounding Management
Participants reported that pharmacologic management of ANV includes the use of sedatives (benzodiazepines): “I’ve seen lorazepam prescribed for anticipatory nausea to help calm the patient” (P10); “Ativan® [lorazepam] . . . to take the night before or the morning of treatment” (P11). In addition, all participants described limited insight into nonpharmacologic interventions for the management of ANV. One participant said, “I really don’t know much about alternative means apart from talking to the patients” (P10). Participants also reported that nausea, although more difficult to manage than vomiting, was the main concern for patients throughout their chemotherapy treatment: “They find it hard to get rid of that sick feeling” (P7).
Negative Impact of Anticipatory Nausea and Vomiting
Participants demonstrated a strong understanding of the negative impact of ANV:
It affects their quality of life, their diet. . . . [They’re] frightened to eat before coming in. . . . [It] probably [affects] their relationships, too. (P1)
One participant provided insight into the effect that ANV had on one patient’s children:
I had a young girl who I got the social worker to get a caregiver [for] to help take care of [her] kids. Anticipatory nausea can have an awful impact [on patients’ lives]. (P8)
Although ANV can negatively affect patients’ experiences with treatment, participants believed that strong family support also has the potential to either relieve or aggravate these symptoms. One participant said,
Depending on the family members, they might add to the stress and anxiety, or they can be calm and relieve the situation. It can work both ways. (P7)
Conversely, another participant believed that having a strong support system benefited patients. She said, “If the family are supportive and positive, they can help the patient face a day of chemo” (P1).
Discussion
This study provides insight into nurses’ understanding of ANV in patients with cancer in Ireland. According to the findings, participants believed that the emetogenic potential of a chemotherapy drug is not solely related to the development of ANV. Instead, participants described ANV as individualized to the patient. The importance of examining individual patient risk factors when managing CINV in general is supported by the literature (Clemons, 2018; Dranitsaris et al., 2017). Clark-Snow et al. (2018) identified individual risk factors as determinants of patients at risk for CINV; however, the authors also reported that the emetogenicity of the chemotherapy drug, as well as physician preference, can determine the antiemetic protocol used. Participants in the current study indicated that patients’ previous hospital stays and experiences can influence their development of ANV. Sights and sounds associated with chemotherapy administration, as well as patient personalities, can contribute to patients experiencing ANV and CINV. Participants reported that the constant noise of machines in the treatment room or the sight of the nurse who administered treatment during a previous cycle can trigger ANV in patients. Participants described the experiences of patients they have cared for who received low-risk emesis chemotherapy drugs and still experienced ANV. This finding is supported by established NCI (2018) guidelines for CINV and a study by Hesketh et al. (2017), which reports that ANV is often a learned response to previous chemotherapy sessions and not caused by the drug itself. Participants in the current study were confident describing the risk factors commonly associated with the development of ANV. The qualitative nature of this study provided nurses with the opportunity to consider and explore the predispositions for ANV that they encounter in daily practice. Patient anxiety and multiple cycles of treatment were perceived by participants as frequent predictors of ANV.
The study design also allowed participants to describe their understanding of the difference between nausea and vomiting. Because nausea and vomiting are caused by separate neural pathways, these symptoms should be assessed and managed individually (Pirri et al., 2011). Understanding the fundamental difference between nausea and vomiting is described in a study by Krishnasamy et al. (2014), which reported that as many as 77% of nurses agreed that their assessments correctly distinguished between nausea and vomiting. Although 82% of participants of Krishnasamy et al.’s (2014) study identified the importance of nurses in patient assessments, only 20% of participants used an assessment tool to do so. Similarly, Clark-Snow et al. (2018) found that nurses identified the need to use an assessment tool to better understand CINV in patients but did not use such tools in daily practice. Participants in the current study also believed that nurses are well suited for administering patient assessments, but none used a specific ANV assessment tool. Participants in the current study reported assessing patients for nausea and vomiting using questions based on their experience and clinical knowledge rather than using an established assessment tool. Nursing knowledge and experience alone can result in entirely different patient assessments. Varying patient assessments have the potential to impede the correct management of patients’ nausea and vomiting (Dranitsaris et al., 2017; Krishnasamy et al., 2014). Previous research also recommends the implementation of a standardized assessment tool for nausea and vomiting (Clemons, 2018; Dranitsaris et al., 2017; Krishnasamy et al., 2014; Molassiotis et al., 2007, 2016; Moradian et al., 2014; Pirri et al., 2011; Spiegel et al., 2014; Thompson, 2012; Wood, Chapman, & Eilers, 2011). Participants in the current study appear to be fulfilling this responsibility in an ad hoc manner, with little to no use of a standardized framework to guide ANV assessment. The lack of a standardized ANV assessment tool in this setting may account for the uncertainty surrounding ANV prevalence reported by participants. Without stringent, clear, and concise measures to assess and identify ANV, it is unsurprising that participants were unsure and indecisive when asked to discuss the prevalence of ANV in their daily practice. Without formal assessments of patients’ ANV, incidence may not be identified or reported by healthcare professionals (Aapro, 2018; Krishnasamy et al., 2014; Molassiotis et al., 2016; Pirri et al., 2011; Thompson, 2012; Wood et al., 2011).
All participants in this study correctly identified the recommended pharmacologic interventions for ANV, which are outlined by international guidelines for ANV management (MASCC and ESMO, 2016; NCCN, 2018; Roila et al., 2016). However, all participants expressed a lack of sufficient knowledge of or familiarity with nonpharmacologic interventions for ANV management. As a result, participants did not recommend nonpharmacologic treatments to patients. Overall, nonpharmacologic interventions remain poorly defined in the literature and effectiveness in practice is limited (Hesketh et al., 2017; Kamen et al., 2014; Karagozoglu, Tekyasar, & Yilmaz, 2013; MASCC and ESMO, 2016; NCCN, 2018; NCI, 2018). Regarding mindfulness and self-care, the authors believe that it is essentials for healthcare providers not only to provide medical knowledge, but also to evaluate alternative treatments to ensure holistic patient-centered care.
According to participants, ANV negatively affects patients’ quality of life. Participants likened ANV to a “dark and dreary road.” This is supported by the NCI (2018), which reports that uncontrolled ANV can lead to depression. Studies by Aapro (2018) and Vidall (2011) suggest that physicians and oncology nurses often underestimate the impact that ANV has on patients. Although healthcare providers may underestimate the impact of ANV, participants in the current study described changing the administration method used or hiding chemotherapy drugs from the patient’s view as ways to reduce the risk for ANV. These simple measures indicate an understanding of the effects that ANV has on quality of life and encourages implementing strategies to reduce incidence.
Participants described the influence that family caregivers can have on patients’ development and management of ANV. Sasaki et al. (2017) examined patient perceptions of symptoms and concerns during chemotherapy treatment and “affects my family or partner” was ranked the most troublesome nonphysical concern for patients. The emphasis on the nonphysical concerns of chemotherapy highlights the importance of family involvement and engagement during patient care (Sasaki et al., 2017). In the current study, participants’ awareness of the influence that family members can have on the ANV experiences of patients illustrates the importance of encouraging effective communication among patients and family caregivers. However, respecting the patients’ wishes if they refuse to involve family caregivers in their treatment is also fundamental.
Limitations
All participants were selected from a single cancer center, limiting the generalizability of the findings. Although the number of participants was reasonable for data saturation, the small sample size limits the transferability of the findings. Because the sample was comprised of all female participants, the findings may not reflect the experiences of male nurses. Having the first author conduct the interviews and analyze the data may have introduced bias in how the findings were interpreted. The relatively short length of the interviews (11–14 minutes) was also identified as a possible limitation.
Implications for Nursing and Research
Ongoing education for healthcare professionals and patients on the prevalence of and identification of risk factors for ANV is essential to the delivery of quality patient care. Because nurses are central to ongoing patient care, they are best suited to implement ANV assessment tools in practice. Amending existing national nausea and vomiting tools or developing a new assessment tool that focuses on identifying and assessing ANV is essential to best practice. A standardized ANV assessment tool that is clear and concise may facilitate holistic patient care and prompt effective management of ANV. In addition, individual patient risk factors, as well as the emetogenic potential of the drug, should be considered when prescribing antiemetics to prevent the onset of ANV. Research on nurses’ understanding of and ability to recognize patients at risk for ANV is warranted. Qualitative research with a larger sample size that includes male participants, clinical nurse specialists, and clinical nurse managers at various designated cancer centers is needed to ensure adequate care is provided to patients experiencing ANV. Additional research is also needed to examine the use of nonpharmacologic approaches for the management of ANV in clinical practice. 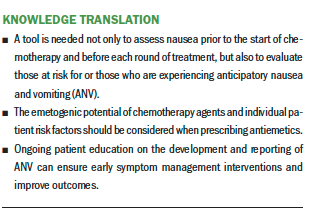
Conclusion
Ensuring that healthcare professionals understand that ANV is an individualized experience and that the type of chemotherapy drug prescribed is unrelated to the development of ANV is essential to best practice in patient care. Assessing and treating patients for ANV at the start of their chemotherapy treatment and at subsequent appointments can mitigate or alleviate symptoms. The lack of a standardized assessment tool for ANV is a gap in clinical practice that needs to be addressed to ensure that oncology nurses can provide holistic patient-centered care. Future research can develop and test a formal tool for the assessment of ANV in patients with cancer.
The authors gratefully acknowledge the oncology nurses in this study who shared their experiences.
About the Author(s)
Anne Ryan, RGN, BSc, MSc, is an oncology nurse manager at University Hospital Limerick, and Brendan Noonan, DN, RGN, BSc, HDip (ENTN), MSc, HDip (TLHE), is the director of undergraduate clinical practice education in the School of Nursing and Midwifery at University College Cork, both in Ireland. No financial relationships to disclose. Mention of specific products and opinions related to those products do not indicate or imply endorsement by the Oncology Nursing Society. Both authors contributed to the conceptualization and design, completed the data collection, provided statistical support and analysis, and contributed to the manuscript preparation. Noonan can be reached at b.noonan@ucc.ie, with copy to ONFEditor@ons.org. (Submitted October 2018. Accepted June 13, 2019.)
References
Aapro, M. (2018). CINV: Still troubling patients after all these years. Supportive Care in Cancer, 26(1, Suppl.), s5–s9. https://doi.org/10.1007/s00520-018-4131-3
Chan, A., Kim, H.K., Hsieh, R.K., Yu, S., de Lima Lopes, G., Jr., Su, W.C., . . . Keefe, D.M. (2015). Incidence and predictors of anticipatory nausea and vomiting in Asia Pacific clinical practice—A longitudinal analysis. Supportive Care in Cancer, 23, 283–291. https://doi.org/10.1007/s00520-014-2375-0
Chung, S.K., Ahn, M.J., Yoo, J.Y., Choi, M., Hyang, N., Woo, S.R., . . . Oh, E.G. (2011). Implementation for best practice for chemotherapy-induced nausea and vomiting in an acute care setting. International Journal of Evidence-Based Healthcare, 9, 32–38. https://doi.org/10.1111/j.1744-1609.2010.00198.x
Clark-Snow, R., Affronti, M.L., & Rittenberg, C.N. (2018). Chemotherapy-induced nausea and vomiting (CINV) and adherence to antiemetic guidelines: Results of a survey of oncology nurses. Supportive Care in Cancer, 26, 557–564. https://doi.org/10.1007/s00520-017-3866-6
Clemons, M. (2018). Guidelines versus individualized care for the management of CINV. Supportive Care in Cancer, 26(1, Suppl.), s11–s17. https://doi.org/10.1007/s00520-018-4115-3
Dranitsaris, G., Molassiotis, A., Clemons, M., Roeland, E., Schwartzberg, L., Dielenseger, P., . . . Aapro, M. (2017). The development of a prediction tool to identify cancer patients at high risk for chemotherapy-induced nausea and vomiting. Annals of Oncology, 28, 1260–1267. https://doi.org/10.1093/annonc/mdx100
Graneheim, U.H., & Lundman, B. (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today, 24, 105–112. https://doi.org/10.1016/j.nedt.2003.10.001
Hesketh, P.J., Kris, M.G., Basch, E., Bohlke, K., Barbour, S.Y., Clark-Snow, R.A., . . . Lyman, G.H. (2017). Antiemetics: American Society of Clinical Oncology clinical practice guideline update. Journal of Clinical Oncology, 35, 3240–3261. https://doi.org/10.1200/JCO.2017.74.4789
Jordan, K., Schaffrath, J., Jahn, F., Mueller-Tidow, C., & Jordan, B. (2014). Neuropharmacology and management of chemotherapy-induced nausea and vomiting in patients with breast cancer. Breast Care, 9, 246–253. https://doi.org/10.1159/000366300
Kamen, C., Tejani, M.A., Chandwani, K., Janelsins, M., Peoples, A.R., Roscoe, J.A., & Morrow, G.R. (2014). Anticipatory nausea and vomiting due to chemotherapy. European Journal of Pharmacology, 722, 172–179. https://doi.org/10.1016/j.ejphar.2013.09.071
Karagozoglu, S., Tekyasar, F., & Yilmaz, F.A. (2013). Effects of music therapy and guided visual imagery on chemotherapy-induced anxiety and nausea-vomiting. Journal of Clinical Nursing, 22(1–2), 39–50. https://doi.org/10.1111/jocn.12030
Krishnasamy, M., Kwok-Wei So, W., Yates, P., de Calvo, L.E., Annab, R., Wisniewski, T., & Aranda, S. (2014). The nurse’s role in managing chemotherapy-induced nausea and vomiting: An international survey. Cancer Nursing, 37(4), E27–E35. https://doi.org/10.1097/NCC.0b013e3182a3534a
Molassiotis, A., Coventry, P.A., Stricker, C.T., Clements, C., Eaby, B., Velders, L., . . . Gralla, R.J. (2007). Validation and psychometric assessment of a short clinical scale to measure chemotherapy-induced nausea and vomiting: The MASCC antiemesis tool. Journal of Pain and Symptom Management, 34, 148–159. https://doi.org/10.1016/j.jpainsymman.2006.10.018
Molassiotis, A., Lee, P.H., Burke, T.A., Dicato, M., Gascon, P., Roila, F., & Aapro, M. (2016). Anticipatory nausea, risk factors and its impact on chemotherapy-related nausea and vomiting: Results from the Pan European Emesis Registry study. Journal of Pain and Symptom Management, 12, 987–993. https://doi.org/10.1016/j.jpainsymman.2015.12.317
Moradian, S., Shahidsales, S., Ghavam Nasiri, M.R., Pilling, M., Molassiotis, A., & Walshe, C. (2014). Translation and psychometric assessment of the Persian version of the Rhodes Index of Nausea, Vomiting and Retching (RINVR) scale for the assessment of chemotherapy-induced nausea and vomiting. European Journal of Cancer Care, 23, 811–818. https://doi.org/10.1111/ecc.12147
Multinational Association of Supportive Care in Cancer and European Society for Medical Oncology. (2016). MASCC/ESMO antiemetic guidelines. Retrieved from https://www.mascc.org/antiemetic-guidelines
National Cancer Institute. (2018). Treatment-related nausea and vomiting (PDQ®)—Heath professional version. Retrieved from https://www.cancer.gov/about-cancer/treatment/side-effects/nausea/nause…
National Comprehensive Cancer Network. (2018). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Anti-emesis [v.3.2018]. Retrieved from https://www.nccn.org/professionals/physician_gls/pdf/antiemesis.pdf
Pirri, C., Katris, P., Trotter, J., Bayliss, E., Bennett, R., & Drummond, P. (2011). Risk factors at pretreatment predicting treatment-induced nausea and vomiting in Australian cancer patients: A prospective, longitudinal, observational study. Supportive Care in Cancer, 19, 1549–1563. https://doi.org/10.1007/s00520-010-0982-y
Roila, F., Molassiotis, A., Herrstedt, J., Aapro, M., Gralla, R.J., Bruera, E., . . . van der Wetering, M. (2016). 2016 MASCC and ESMO guideline update for the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting and of nausea and vomiting in advanced cancer patients. Annals of Oncology, 27(Suppl. 5), v119–v133. https://doi.org/10.1093/annonc/mdw270
Roscoe, J.A., Morrow, G.R., Aapro, M.S., Molassiotis, A., & Olver, I. (2011). Anticipatory nausea and vomiting. Supportive Care in Cancer, 19, 1533–1538. https://doi.org/10.1007/s00520-010-0980-0
Sandelowski, M. (2000). Whatever happened to qualitative description? Research Nurse and Health, 23, 334–340.
Sasaki, H., Tamura, K., Naito, Y., Ogata, K., Mogi, A., Tanaka, T., . . . Takamatsu, Y. (2017). Patient perceptions of symptoms and concerns during cancer chemotherapy: ‘Affects my family’ is the most important. International Journal of Clinical Oncology, 22, 793–800. https://doi.org/10.1007/s10147-017-1117-y
Spiegel, B.M., Hays, R.D., Bolus, R., Melmed, G.Y., Chang, L., Whitman, C., . . . Khanna, D. (2014). Development of the NIH Patient-Reported Outcomes Measurement Information System (PROMIS) gastrointestinal symptom scales. American Journal of Gastroenterology, 109, 1804–1814. https://doi.org/10.1038/ajg.2014.237
Streubert, H.J., & Carpenter, D.R. (2011). Qualitative research in nursing: Advancing the humanistic imperative (5th ed.). Philadelphia, PA: Wolters Kluwer Health.
Thompson, N. (2012). Optimizing treatment outcomes in patients at risk for chemotherapy-induced nausea and vomiting. Clinical Journal of Oncology Nursing, 16, 309–313. https://doi.org/10.1188/12.CJON.309-313
Vidall, C. (2011). Chemotherapy induced nausea and vomiting: A European perspective. British Journal of Nursing, 20(10, Suppl.), S22, S25–S28. https://doi.org/10.12968/bjon.2011.20.Sup5.S22
Wood, J.M., Chapman, K., & Eilers, J. (2011). Tools for assessing nausea, vomiting and retching. Cancer Nursing, 34, E14–E24.




