Effects of a Mindfulness Intervention on Hospitalized Patients With Hematologic Malignancies and Their Caregivers
Objectives: To examine the effects of a mind–body intervention on the psychological distress of hospitalized patients with hematologic malignancies and their caregivers.
Sample & Setting: 29 patients with hematologic malignancies and 5 caregivers were recruited from the bone marrow transplantation unit at Barnes-Jewish Hospital in St. Louis, Missouri.
Methods & Variables: After completing the Rotterdam Symptom Checklist (RSCL) to rate their levels of psychological and physiologic distress and quality of life, participants were taught a mindfulness activity. Two weeks postintervention, participants completed the RSCL again, reported how often they practiced the activity, and answered qualitative questions regarding their experience.
Results: Participants reported increased relaxation and improved sleep and showed interest in practicing mindfulness as a part of their treatment plan.
Implications for Nursing: Nurses can help to alleviate symptoms of distress in patients with hematologic malignancies by integrating education on how to perform short and simple mindfulness activities into the care plan.
Jump to a section
Cancer is a disease with physiologic, emotional, and psychological effects, and treatment often requires long hospitalizations, which may increase the risk for experiencing additional stress and anxiety (Papadopoulou, Johnston, & Themessl-Huber, 2013; Zimmermann et al., 2013). Patients with hematologic malignancies, such as leukemia, lymphoma, and multiple myeloma, may require immediate and intensive treatment with extended hospitalization. For some patients, first-line treatment may include chemotherapy or a hematopoietic stem cell transplantation (Rautenberg, Germing, Haas, Kobbe, & Schroeder, 2019). Hematopoietic stem cell or bone marrow transplantations can often lead to unpleasant or lengthy side effects and comorbidities (Negrin, 2018). Psychosocial issues and challenges can also occur at the time of initial treatment decisions and continue through to survivorship (Korol et al., 2017; McQuellon & Duckworth, 2016).
Background
The psychological impact of cancer on patients can be profound and long-lasting (El-Jawahri et al., 2017). Psychological distress is commonly assessed using measures that evaluate levels of stress, anxiety, and depression (Rouleau, Garland, & Carlson, 2015). Prolonged psychological distress has been shown to decrease immune function, indicating a need to develop coping skills and stress management strategies in patients with cancer (Rosenkranz et al., 2016). Identifying and addressing psychological distress can help to prevent decreased quality of life and disease-related morbidity and mortality (Andersen et al., 2014).
Increased levels of depression and anxiety can be experienced by patients with cancer or their caregivers (Kent et al., 2016). Caregivers typically provide care that is uncompensated and involves significant physical, emotional, social, and financial demands (Kent et al., 2016). According to Kim, Carver, Shaffer, Gansler, and Cannady (2015), caregiver distress can have lasting effects on patients and the caregivers themselves. In a study by Rha, Park, Song, Lee, and Lee (2015), patients’ partners, particularly those providing care to hospitalized family members, experienced a decline in quality of life, which demonstrates the importance of considering caregivers’ overall well-being during patients’ cancer trajectories.
Mindfulness, which is defined as a practice that involves “paying attention in a particular way: on purpose, in the present moment, and non-judgmentally” (Kabat-Zinn, 2013, p. xxvii), has been shown to be effective in reducing psychological distress in patients with cancer (Zhang et al., 2015). Research on mindfulness has increased significantly (Gu, Strauss, Bond, & Cavanagh, 2016). Some examples of mindfulness interventions that have been shown to have psychological benefits for patients with cancer include an eight-week intensive mindfulness-based stress reduction program (Kabat-Zinn, 2013), yoga (Agarwal & Maroko-Afek, 2018), and guided imagery (Chen, Wang, Yang, Chung, 2015).
Studies have shown that mindfulness-based interventions can alleviate the symptoms of anxiety and depression that often accompany the cancer experience (Carlson, 2017). A study by Stonnington et al. (2016) that examined the effects of a mind–body intervention on patients undergoing solid organ and stem cell transplantation and their caregivers found that the intervention improved perceived stress and anxiety outcomes and increased quality of life. A pilot study by Bauer-Wu et al. (2008) evaluated the effects of mindfulness meditation on hospitalized patients undergoing autologous stem cell transplantation. The bedside intervention encouraged patient awareness of breath, thoughts, and physical sensations, and patients were given an audio recording of the guided meditation so that they could practice independently. The results of Bauer-Wu et al.’s (2008) study suggest that mindfulness interventions can be effective in reducing physical and psychological distress for hospitalized patients undergoing transplantation.
The body scan, a mindfulness activity that involves scanning the body from the toes to the top of the head in a systematic way, encourages individuals to be aware of their breathing, sensations, or feelings, and to observe these sensations without judgment (Kabat-Zinn, 2018). Although it is most commonly practiced while lying down, it can also be practiced while seated or standing. Mindfulness interventions, such as the body scan, have been shown to significantly improve psychological well-being across healthy populations (Sauer-Zavala, Walsh, Eisenlohr-Moul, & Lykins, 2013) and cancer populations (Tang, Tang, & Gross, 2019). Therefore, patients and their caregivers may experience some degree of improvement in psychological distress following participation in a mindfulness activity.
The purpose of this pilot study was to examine whether implementing a mind–body intervention during inpatient hospitalization improved self-reports of physical and psychological symptoms two weeks postintervention among patients with hematologic malignancies and their caregivers. By educating patients and their caregivers on mindfulness and providing them with the necessary tools to practice the mindfulness activity independently, this study aimed to decrease feelings of stress and anxiety and to empower patients and caregivers to better cope with such feelings in the future.
Methods
Sample and Setting
A convenience sample of 34 participants (29 patients and 5 caregivers) was recruited from a leukemia, lymphoma, and bone marrow transplantation unit at the Barnes-Jewish Hospital in St. Louis, Missouri. Participants were eligible if they were aged 18 years or older, alert and oriented, and able to understand and sign their own informed consent form. Patient participation was not dependent on caregiver participation; patients were eligible to participate without their caregiver. Patients and caregivers were excluded from the study if they required a language translator or interpreter. The Washington University Institutional Review Board and the Protocol Review and Monitoring Committee of the Alvin J. Siteman Cancer Center approved the study.
Procedures
Nurses on the study unit informed the principal investigator (PI) of any patients who showed interest in participating. The PI then approached patients to discuss the study and their interest. Because of the risk for infection, all patients on the unit had private rooms, ensuring confidentiality. Patients who were approached for participation were given an informational flyer that outlined the study aims and mindfulness-based body scan activity, and the PI followed up with the patient at an agreed-on time. Eligible patients and caregivers reviewed and signed the consent form, and the PI was available to answer any questions pertaining to study involvement. Most patients did not request that their caregiver participate in the study.
Once consent was obtained, participants completed a pretest comprised of the Rotterdam Symptom Checklist (RSCL) and questions that captured demographic information such as age and diagnosis. The RSCL is a 39-item Likert-type scale that assesses physical and psychological symptoms (30 questions), daily function (8 questions), and overall valuation of life (1 question) (de Haes et al., 1996). For the 30 symptom-related questions, participants rated how bothered they were by specific symptoms during the past week on a scale ranging from 1 (not at all) to 4 (very much), with higher scores indicating higher levels of distress. Participants rated their overall valuation of life on a scale ranging from 1 (excellent) to 7 (extremely poor). For this study, the authors of the scale granted permission to remove the eight questions on daily function because they were not applicable to the inpatient patient population (e.g., light housework, household jobs). The physical and psychological symptom questions on the RSCL were specifically tested and shown to be reliable and valid in patients with a cancer diagnosis (de Haes, van Knippenberg, & Neijt, 1990). The psychological dimension has been shown to be highly reliable across several cancer populations, with a Cronbach alpha ranging from 0.88–0.94. The physical distress scale has been presented through several dimensions (e.g., pain, fatigue) in a homogeneous population and undimensionally in a heterogeneous population, with a Cronbach alpha ranging from 0.71–0.88 (de Haes et al., 1990). In addition to completing the RSCL, patients were given a practice log to record when, where, and for how long they practiced the mindfulness activity, as well as whether they practiced independently or with their caregiver. Additional space was provided on the practice log for any comments.
At two weeks postintervention, participants completed a post-test consisting of the RSCL and five open-ended questions that addressed how the mindfulness intervention affected their distress level (see Figure 1). If the participant was still available on the unit, the post-test was administered in person; otherwise, post-test data were collected via a follow-up telephone call. As part of a debriefing session on the overall experience, participants were able to ask questions, express concerns, and provide feedback. 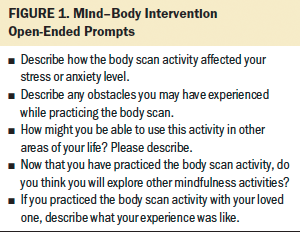
The pre- and post-tests were given a unique code by the PI. This coding sheet was secured in a locked filing cabinet in a room that could only be accessed by individuals with an employee badge. Upon completion of the study, the master coding sheet was destroyed once all data were collected and recorded.
Mind–Body Intervention
To establish the treatment fidelity of the body scan mindfulness activity as an effective mind–body intervention, the intervention was delivered and completed by the PI alone. The PI is a practicing oncology nurse and a 500-hour registered yoga teacher (RYT® 500), with training that encompassed rigorous study of biomechanics and subtle anatomy (Circle Yoga Shala, n.d.). In addition, the PI has extensive experience in Vipassana meditation, which informs the techniques used in the body scan mindfulness activity. Prior to the implementation of the mind–body intervention, healthcare professionals on the unit were notified of the study in progress.
Measures were taken to ensure that participants would not be interrupted during the intervention and that the intervention did not interfere with clinical care. Potential conflicts (e.g., scheduled procedure or laboratory draw, expected visit from a healthcare professional) were addressed with the patients’ nurses prior to implementation. During the intervention, a sign was hung outside of the patient’s room that asked visitors to return at a later designated time. Additional efforts were made to minimize any other potential disruptions. Patients were given antiemetic medications (if requested), asked to empty their bladder prior to the intervention, and instructed to turn off telephones and televisions. If the intervention was interrupted, the PI used it as an opportunity to provide further mindfulness education, asking participants to be aware of how they felt during the interruption and to acknowledge their feelings with objective observation. The intervention took 20 minutes to complete, and all participants completed the intervention with the PI present. The five caregivers who participated in the study completed the intervention with the patient; the remaining 24 participants performed the activity alone with the PI.
At the start of the mindfulness activity, the participants were instructed to find a comfortable seated or lying position and to close their eyes. Participants were then asked to objectively observe their breathing and instructed on how to perform deep belly breathing. Patients with respiratory issues, such as asthma or pneumonia, were told to take “easy breaths.” Once participants were aware of their breathing, they were guided through the body scan activity. Beginning with awareness of sensations in the left toe, participants were asked to observe any sensations without judgment and to notice and allow them. Awareness of sensations were continued up through the remainder of the body, ending with the very top of the head. All efforts were made to normalize the participants’ experiences (e.g., the desire to open their eyes, thinking about other things, wanting to move around). Participants were encouraged to become interested in and curious about any perceptions in their body and to allow these natural tendencies to occur. After completing the guided body scan, participants were told to again become aware of their breathing and were given several minutes of quiet reflection.
After opening their eyes, participants were given the opportunity to discuss their experience with the PI and ask questions. To ensure understanding and determine how the intervention was received, participants were asked to summarize the process. Participants and the PI discussed a plan for implementing the techniques from the mindfulness activity (e.g., belly breathing, body scan) during hospitalization and following discharge, if applicable. For reference, participants were given a handout that outlined the mindfulness activity and additional practice logs. At the end of the activity, the PI reminded participants that they would receive a visit or a follow-up telephone call two weeks after the intervention.
Results
Data were analyzed using IBM SPSS Statistics, version 22.0. Descriptive statistics were used to analyze the demographic characteristics of patient participants. Depending on mutual availability, the timing of the two-week follow-up ranged from 13 to 31 days postintervention. Most participants were women (n = 17) and identified as White (n = 22). The majority of patients were aged 60–69 years. Twelve participants had earned a high school diploma or equivalent, and 10 had earned a bachelor’s degree. The primary diagnosis in this sample was multiple myeloma (n = 9), followed by acute myeloid leukemia (n = 8). The remaining patients had various diagnoses. Thirteen patients in this sample had previously heard of mindfulness.
At two weeks postintervention, a Wilcoxon signed-rank test indicated that patients’ physiologic (z = 4.12, p < 0.05, r = 0.54) and psychological distress (z = 2.16, p < 0.05, r = 0.28) was significantly reduced. The Wilcoxon signed-rank test also revealed no statistically significant improvement in quality-of-life scores among patients. Because of the small sample size (n = 5), data from caregivers were not included in the analysis.
During the follow-up appointment, participants answered open-ended questions regarding their experience with the mind–body intervention. Although quality-of-life scores were not significantly improved following the intervention, reflections in the participants’ self-reports indicate that there were clinically significant improvements in participants’ perceptions of their quality of life. In addition, participants were able to further describe their experience with the mindfulness activity through open discussion (see Figure 2). Self-reports from patients suggest that the mindfulness activity provided many benefits, such as help focusing “when [your] mind goes all over the place,” an “immediate decrease in feelings of tension and stress,” and “help becoming aware of tensions.” In describing the mindfulness activity’s effect on his neuropathy, one patient said the following:
If I can ride [the wave], whether it was cresting or falling, maybe I can manage it on my own without medication. It’s a great method for quickly finding tensions and releasing them . . . anytime and anywhere necessary.
Patients also reported that they used the mindfulness techniques that they learned during the intervention while being transferred to the intensive care unit and receiving a stem cell transplantation or other procedure. One patient, who cited a history of anxiety and claustrophobia, reported that she performed the body scan mindfulness activity during an magnetic resonance imaging scan and was so relaxed that she had to be “poked” when it was completed. Overall, patients reported feeling more relaxed following the mind–body intervention. However, some challenges were experienced by participants. For example, most participants reported difficulty in finding 20 minutes of anticipated, uninterrupted time during their hospital stay. Some participants reported that they overcame this challenge by setting a timer for several minutes to focus on one area of the mindfulness activity (e.g., belly breathing) or on sensations that they were feeling. 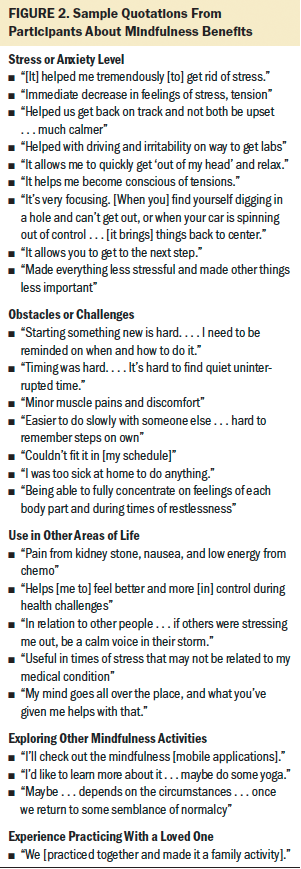
Four caregivers who participated in the study reported that they encouraged their loved ones to practice mindfulness whenever they were feeling stressed. Therefore, it is believed that implementing a mind–body intervention can provide patients and caregivers with beneficial stress-relief techniques. One caregiver stated that participating in the intervention was “the most relaxed I felt in a month, and this was the most stressful month of my life.” Three other caregivers reported practicing the mindfulness activity with their loved ones after the intervention and making it a family activity. Two caregivers suggested that the hospital could provide group classes on mindfulness, and one requested an audio recording of the activity for independent use.
Information from the practice logs was collected at the two-week follow-up. Similar to Bauer-Wu et al.’s (2008) study, few participants completed the log. In this study, only five patients and three caregivers completed the practice log. Reasons for not completing the practice log included not recording every time the mindfulness activity was practiced or losing the log. Several participants reported praying or watching television while practicing the mindfulness activity independently; however, they did not log this practice time because they felt that they had to be solely focused on the mindfulness activity for it to be logged as practice time.
Discussion
The current study focused on the effects of a mind–body intervention on the physical and psychological distress of hospitalized patients with hematologic malignancies and their caregivers. Similar to previous studies, this intervention was shown to reduce psychological distress in patients (Rouleau et al., 2015; Zhang et al., 2015). In this study, the mindfulness activity was implemented beyond the original aim of the study; patients applied the body scan and belly breathing techniques to other experiences in their lives. One patient reported using mindfulness techniques before going to his art studio to work, saying that it “opens my mind and lets me think and do what is natural for me.” Another participant reported that mindfulness is helpful in “trying to concentrate on [the] physical body and realizing I don’t have pain or physical symptoms of disease. . . . [It] helps me realize it’s getting better.” At the study institution, mindfulness activities are not currently included as part of patients’ treatment plans; however, one participant suggested that “it should be written into the plan. . . . It encourages patient participation and ownership and responsibility . . . more patient involvement.” Patient involvement has become an increasingly important element in providing patient-centered care (Castro, Van Regenmortel, Vanhaecht, Sermeus, & Van Hecke, 2016). At the bedside, nurses can include the integration of a mindfulness activity as a patient goal for that particular day.
Only five caregivers agreed to participate in this study. Of the caregivers who were approached for the study, most stated that they would rather allow the patient to have time to participate in the intervention alone while giving themselves respite. The five caregivers who did participate provided insightful feedback when answering the open-ended questions at follow-up. When discussing patients’ levels of stress or anxiety, caregiver participants reported encouraging their loved ones to practice the mindfulness activity and belly breathing. Participation in the mind–body intervention empowered the caregivers to help patients through difficult periods of stress and anxiety. In addition, caregivers generally found that the belly breathing technique helped them to acknowledge tension that they were not aware of and allowed them to relax. Several caregivers suggested holding daily mindfulness classes with open participation for patients and family caregivers. Although it can be challenging to hold daily classes on hospital units, offering prerecorded videos or audio recordings of mindfulness classes might be a strategy to meet this need. One caregiver claimed that providing a class on mindfulness might give family caregivers a sense of formal permission to take time for themselves. Because caregivers often report feeling guilty for leaving their loved ones’ bedsides (Feast, Orrell, Russell, Charlesworth, & Moniz-Cook, 2017), providing mindfulness classes may help to alleviate the burden felt by caregivers. These classes could be suggested as daily goals of care during discussions with patients and their caregivers. Caregivers also suggested offering a designated time and space to learn and practice mindfulness activities. Unfortunately, available space is at a premium in most settings. Caregiver distress is often overlooked, but it has the potential to influence patient distress (Kent et al., 2016). Because of the importance of acknowledging caregivers’ need for self-care, providing an opportunity for privacy and quiet in even a minimal space can help to reduce caregiver burden.
Limitations
Patients in this sample were staying on the bone marrow transplantation unit for various reasons (e.g., a variety of chemotherapy regimens, transplantation, complications from transplantation). Therefore, the intervention did not take place at the same time in the treatment or transplantation process for all patient participants. Because of this, patients had varying degrees of control over their environment (i.e., spending most of the two-week intervention period at home versus on the intensive care unit) and experienced varying intensities of chemotherapy side effects, which may have influenced the frequency and duration of practice. This may also have negatively affected patients’ motivation to practice. Future studies might implement the intervention and follow-up during a more uniformed study period to determine the most beneficial time in the cancer trajectory to introduce mindfulness practice to patients. In this study, the PI was the only individual conducting the intervention and follow-up, which may not be feasible in future studies. Because of familiarity with the concept of mindfulness, self-selection bias may have also occurred. In addition, because the PI was a staff nurse on the unit, patients may have been willing to participate based on their familiarity with the PI, increasing the risk for social desirability bias. Participants in this study reported varying frequencies and duration of practice, which may be improved in future studies by providing audio- or visual-recorded mindfulness activities of a set length and with a required minimum frequency of practice. Nurses who are responsible for the care of multiple patients may not be available to conduct the 20-minute mindfulness activity with patients while also providing standard clinical care. Therefore, the intervention as outlined in this article may not be practical in all settings.
Implications for Nursing
To ensure the effectiveness of educating patients on mindfulness, it is recommended that nurses have some level of understanding of mindfulness techniques and practices, as well as feel comfortable instructing patients or caregivers in how to perform these activities. Although it is not necessary to specifically train nurses on how to guide others during a body scan activity, experience in similar mindfulness techniques, such as yoga, tai chi, or meditation, can better prepare nurses who are introducing patients to the foundational principles of mindfulness.
This pilot study suggests that a mind–body intervention may be an effective strategy to potentially reduce physical and psychological distress among hospitalized patients with hematologic malignancies. However, several challenges were experienced while implementing the mindfulness activity, such as time and availability. When implementing a similar intervention at other institutions, considerations must be taken to ensure that enough time is allotted to perform the mindfulness activity and that nurses who are responsible for the care of multiple patients are not overwhelmed with the additional demands of assisting patients with the activity. Nurses can also overcome the challenge of finding time to conduct the mindfulness activity with patients by instead providing visual or auditory guidance to patients. A recording of the body scan activity or a similar mind–body intervention can help patients to practice mindfulness independently form their nurse. If patients are feeling anxious about an upcoming procedure or require immediate pain control between medication doses, nurses can then direct patients to the mindfulness recording while they attend to the task of providing clinical patient care. This may be a more realistic method of implementing the intervention for nurses under time constraints.
Patients in this study reported that they had difficulty practicing the mindfulness activity independently because of a lack of planned, uninterrupted time during hospitalization. During the intervention, a sign was placed on the door that requested that any visitors return after 25 minutes, which allowed for the intervention to take place with minimal interruptions. Placing a sign on the doors to patients’ rooms for 20 minutes may be a viable way to incorporate time for practicing mindfulness into patients’ daily care plans. Although time may not be allotted to formally practice mindfulness without any interruptions, some situations may be able to provide informal opportunities to do so. For example, if patients are feeling nauseated, the wait for antiemetic medication can cause additional stress and anxiety. During this period, the staff nurse might encourage patients to focus on the sensations that they are feeling. This allows time for patients to refocus their attention on sensations while the nurse retrieves the required medication. Another obstacle that several patients reported was lack of motivation to practice the mindfulness activity because they were feeling too sick or tired. One patient reported that the minor muscle pains and discomfort she was experiencing were distressing enough to prevent her from practicing mindfulness. This is an opportunity for nurses to remind patients that this is what mindfulness practices can be used for: purposefully paying attention to present sensations without judgment and acknowledging those sensations. 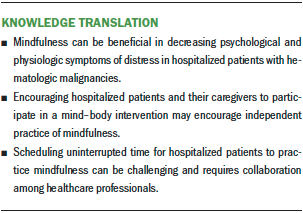
Conclusion
By implementing a mind–body intervention, such as the mindfulness-based body scan activity, patient–provider communication can be improved, and nurses can better understand what physiologic symptoms hospitalized patients are experiencing. Having a more comprehensive understanding of the patient experience can ensure that nurses are able to provide the best care to patients to mitigate the symptoms and side effects of cancer treatment. Encouraging patients to acknowledge and be aware of any sensations or symptoms that they are experiencing can lead to early interventions and better inform the clinical team’s decisions and treatment plan. The current study suggests that introducing mindfulness techniques and activities can be beneficial to cancer populations that are experiencing high levels of stress.
The authors gratefully acknowledge Kathleen Rensing, MSN, ANP-BC, CRNI, for her support throughout the research process, Rita Wunderlich, PhD, RN, CNE, for reviewing the manuscript, and the staff and patients on the bone marrow transplantation unit for making this study possible.
About the Author(s)
Maggie C. Compernolle, RN, BSN, RYT® 500, is a nurse and Jennifer A. Sledge, PhD, MSW, is a research scientist, both at Barnes-Jewish Hospital in Saint Louis, MO. This research was funded by the Barnes-Jewish Hospital Foundation through support from the Department of Research sabbatical program at Barnes-Jewish Hospital. Both authors contributed to the conceptualization and design, provided statistical support and analysis, and contributed to the manuscript preparation. Compernolle completed the data collection. Compernolle can be reached at margaret.compernolle@bjc.org, with copy to ONFEditor@ons.org. (Submitted May 2019. Accepted July 31, 2019.)
References
Agarwal, R.P., & Maroko-Afek, A. (2018). Yoga into cancer care: A review of the evidence-based research. International Journal of Yoga, 11, 3–29. https://doi.org/10.4103/ijoy.IJOY_42_17
Andersen, B.L., DeRubeis, R.J., Berman, B.S., Gruman, J., Champion, V.L., Massie, M.J., . . . Rowland, J.H. (2014). Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: An American Society of Clinical Oncology guideline adaptation. Journal of Clinical Oncology, 32, 1605–1619. https://doi.org/10.1200/JCO.2013.52.4611
Bauer-Wu, S., Sullivan, A.M., Rosenbaum, E., Ott, M.J., Powell, M., McLoughlin, M., & Healey, M.W. (2008). Facing the challenges of hematopoietic stem cell transplantation with mindfulness meditation: A pilot study. Integrative Cancer Therapies, 7, 62–69. https://doi.org/10.1177/1534735408319068
Carlson, L.E. (2017). Distress management through mind-body therapies in oncology. Journal of the National Cancer Institute. Monographs, 2017(52), lgx009. https://doi.org/10.1093/jncimonographs/lgx009
Castro, E.M., Van Regenmortel, T., Vanhaecht, K., Sermeus, W., & Van Hecke, A. (2016). Patient empowerment, patient participation and patient-centeredness in hospital care: A concept analysis based on a literature review. Patient Education and Counseling, 99, 1923–1939. https://doi.org/10.1016/j.pec.2016.07.026
Chen, S.F., Wang, H.H., Yang, H.Y., & Chung, U.L. (2015). Effect of relaxation with guided imagery on the physical and psychological symptoms of breast cancer patients undergoing chemotherapy. Iranian Red Crescent Medical Journal, 17(11), e31277. https://doi.org/10.5812/ircmj.31277
Circle Yoga Shala. (n.d.). Advanced yoga teacher training. Retrieved from http://www.circleyogashala.com/300-hour-yoga-teacher-training-program
de Haes, J.C.J.M., Olschewski, M., Fayers, P., Visser, M.R.M., Cull, A., Hopwood, P., & Sanderman, R. (1996). Measuring the quality of life of cancer patients with the Rotterdam Symptom Checklist (RSCL): A manual. Groningen, the Netherlands: Northern Center for Healthcare Research.
de Haes, J.C., van Knippenberg, F.C., & Neijt, J.P. (1990). Measuring psychological and physical distress in cancer patients: Structure and application of the Rotterdam Symptom Checklist. British Journal of Cancer, 62, 1034–1038. https://doi.org/10.1038/bjc.1990.434
El-Jawahri, A., Traeger, L., Greer, J.A., VanDusen, H., Fishman, S.R., LeBlanc, T.W., . . . Temel, J.S. (2017). Effect of inpatient palliative care during hematopoietic stem-cell transplant on psychological distress 6 months after transplant: Results of a randomized clinical trial. Journal of Clinical Oncology, 35, 3714–3721. https://doi.org/10.1200/JCO.2017.73.2800
Feast, A., Orrell, M., Russell, I., Charlesworth, G., & Moniz-Cook, E. (2017). The contribution of caregiver psychosocial factors to distress associated with behavioural and psychological symptoms in dementia. International Journal of Geriatric Psychiatry, 32, 76–85. https://doi.org/10.1002/gps.4447
Gu, J., Strauss, C., Bond, R., & Cavanagh, K. (2016). Corrigendum to “How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies” [Clinical Psychology Review, 37(2015), 1–12]. Clinical Psychology Review, 49, 119. https://doi.org/10.1016/j.cpr.2016.09.011
Kabat-Zinn, J. (2013). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Bantam.
Kabat-Zinn, J. (2018). An inquiring practice to notice the body. Retrieved from https://www.mindful.org/an-inquiring-practice-to-notice-the-body
Kent, E.E., Rowland, J.H., Northouse, L., Litzelman, K., Chou, W.Y., Shelburne, N., . . . Huss, K. (2016). Caring for caregivers and patients: Research and clinical priorities for informal cancer caregiving. Cancer, 122, 1987–1995. https://doi.org/10.1002/cncr.29939
Kim, Y., Carver, C.S., Shaffer, K.M., Gansler, T., & Cannady, R.S. (2015). Cancer caregiving predicts physical impairments: Roles of earlier caregiving stress and being a spousal caregiver. Cancer, 121, 302–310. https://doi.org/10.1002/cncr.29040
Korol, E.E., Wang, S., Johnston, K., Ravandi-Kashani, F., Levis, M., & van Nooten, F. (2017). Health-related quality of life of patients with acute myeloid leukemia: A systematic literature review. Oncology and Therapy, 5, 1–16. https://doi.org/10.1007/s40487-016-0039-6
McQuellon, R.P., & Duckworth, K.E. (2016). Psychosocial issues in hematopoietic cell transplantation. In S.J. Forman, R.S. Negrin, J.H. Antin, & F.R. Appelbaum (Eds.), Thomas’ hematopoietic cell transplantation: Stem cell transplantation (5th ed., pp. 384–391). Hoboken, NJ: Wiley-Blackwell.
Negrin, R.S. (2018). Patient education: Hematopoietic cell transplantation (bone marrow transplantation): Beyond the basics. In A.G. Rosmarin, UpToDate. Retrieved from https://www.uptodate.com/contents/hematopoietic-cell-transplantation-bo…
Papadopoulou, C., Johnston, B., & Themessl-Huber, M. (2013). The experience of acute leukaemia in adult patients: A qualitative thematic synthesis. European Journal of Oncology Nursing, 17, 640–648. https://doi.org/10.1016/j.ejon.2013.06.009
Rautenberg, C., Germing, U., Haas, R., Kobbe, G., & Schroeder, T. (2019). Relapse of acute myeloid leukemia after allogeneic stem cell transplantation: Prevention, detection, and treatment. International Journal of Molecular Sciences, 20, E228. https://doi.org/10.3390/ijms20010228
Rha, S.Y., Park, Y., Song, S.K., Lee, C.E., & Lee, J. (2015). Caregiving burden and the quality of life of family caregivers of cancer patients: The relationship and correlates. European Journal of Oncology Nursing, 19, 376–382. https://doi.org/10.1016/j.ejon.2015.01.004
Rosenkranz, M.A., Lutz, A., Perlman, D.M., Bachhuber, D.R., Schuyler, B.S., MacCoon, D.G., & Davidson, R.J. (2016). Reduced stress and inflammatory responsiveness in experienced meditators compared to a matched healthy control group. Psychoneuroendocrinology, 68, 117–125. https://doi.org/10.1016/j.psyneuen.2016.02.013
Rouleau, C.R., Garland, S.N., & Carlson, L.E. (2015). The impact of mindfulness-based interventions on symptom burden, positive psychological outcomes, and biomarkers in cancer patients. Cancer Management and Research, 7, 121–131. https://doi.org/10.2147/CMAR.S64165
Sauer-Zavala, S.E., Walsh, E.C., Eisenlohr-Moul, T.A., & Lykins, E.L.B. (2013). Comparing mindfulness-based intervention strategies: Differential effects of sitting meditation, body scan, and mindful yoga. Mindfulness, 4, 383–388. https://doi.org/10.1007/s12671-012-0139-9
Stonnington, C.M., Darby, B., Santucci, A., Mulligan, P., Pathuis, P., Cuc, A., . . . Sood, A. (2016). A resilience intervention involving mindfulness training for transplant patients and their caregivers. Clinical Transplantation, 30, 1466–1472. https://doi.org/10.1111/ctr.12841
Tang, Y.Y., Tang, R., & Gross, J.J. (2019). Promoting psychological well-being through an evidence-based mindfulness training program. Frontiers in Human Neuroscience, 13, 237. https://doi.org/10.3389/fnhum.2019.00237
Zhang, M.F., Wen, Y.S., Liu, W.Y., Peng, L.F., Wu, X.D., & Liu, Q.W. (2015). Effectiveness of mindfulness-based therapy for reducing anxiety and depression in patients with cancer: A meta-analysis. Medicine, 94(45), e0897-0. https://doi.org/10.1097/MD.0000000000000897
Zimmermann, C., Yuen, D., Mischitelle, A., Minden, M.D., Brandwein, J.M., Schimmer, A., . . . Rodin, G. (2013). Symptom burden and supportive care in patients with acute leukemia. Leukemia Research, 37, 731–736. https://doi.org/10.1016/j.leukres.2013.02.009




