Experiences and Needs of African American Children and Adolescents in Supportive Care Roles for a Relative With Breast Cancer
Purpose: To explore the experiences and needs of African American (AA) children and adolescents who were identified by a cancer survivor in their family as providing substantial supportive care during diagnosis and treatment.
Participants & Setting: 5 AA young adults who provided care and support to a family member with cancer when they were aged 7–19 years and 4 cancer survivors from a northeastern U.S. city.
Methodologic Approach: Focus groups and interviews were conducted, recorded, transcribed, and analyzed using content analysis until thematic saturation was reached.
Findings: Themes focused on AA young supporters’ lack of cancer-related information, reduced ability to communicate needs, and challenged views of themselves, relationships, faith, and the future at the time that they provided support.
Implications for Nursing: Nurses can support AA children and adolescents in caregiving roles by assessing their needs and providing information on diagnosis and treatment. In addition, nurses can conduct research on culturally adapted interventions that can better support AA children and adolescents caring for a parent or grandparent with cancer.
Jump to a section
Breast cancer is the most common cancer diagnosed and the second leading cause of cancer death among African American (AA) women (American Cancer Society [ACS], 2019]. AA women’s ability to cope with breast cancer is often challenged by disease factors, such as being diagnosed at a younger age and advanced-stage disease and having higher mortality than other racial and ethnic groups (ACS, 2019). Because the incidence of breast cancer among AA women has increased to that of White women in the United States, supporting the ability of AA women and their families to cope with a breast cancer diagnosis is a growing concern in cancer care (ACS, 2017).
Background
Previous research has reported that AA women with cancer often cite family members and friends as potential sources of support; however, these women also report the need to care for family members and friends, the stigma and fear surrounding cancer, and cultural norms that limit discussion about cancer as barriers to their seeking and accepting support (Haynes-Maslow et al., 2016; Yoo et al., 2010). According to Yoo et al. (2010), commonly reported coping strategies for AA cancer survivors include managing their support system by avoiding negative people, negative thoughts, and disclosure of feelings that may burden family members and friends. Unfortunately, these avoidant behaviors are generally linked to increased distress and reduced social support, which have been associated with reduced survival rates among AA women with cancer (Soler-Vila et al., 2003; Yoo et al., 2014).
Family members and friends of cancer survivors share in the survivorship experience (National Cancer Institute, n.d.), have similar needs, and experience psychological distress not unlike that of diagnosed individuals (Northouse et al., 2012). In addition, there is growing recognition that family members, including children and adolescents, are co-survivors in the cancer experience whose needs are often neglected (Niemelä et al., 2016). According to Weaver et al. (2010), an estimated 562,000 U.S. minor children live with a parent in the early stages of cancer treatment. Children and adolescents living with a parent with cancer desire knowledge about cancer, experience role changes, and rely on family and the community for communication and normalcy in their lives (Shah et al., 2017). Adolescents are particularly at risk for internalizing problems, depression, and anxiety to a greater degree than their parents may realize (Shah et al., 2017).
Research on the experiences of children and adolescents coping with parental cancer is limited (Davey et al., 2011, 2012, 2013). In their study, Kissil et al. (2010) reported that AA adolescents living with a parent with breast cancer may cope through avoidance and distraction, engage in positive activities and prayer, and experience growth from the experience of living with a parent with cancer. Although previous studies have examined children and adolescents as part of the family cancer experience, few studies have explored the experiences of children and adolescents who are providing substantial supportive care to a family member with cancer. This may be particularly relevant to AA families, in which parents with cancer report relying on their children for practical and emotional support (Davey et al., 2013). In a systematic review focused on adolescents and young adults providing care for family members with cancer, Marziliano et al. (2014) found that only one group of studies of this population originated in the United States (Gates & Lackey, 1998; Lackey & Gates, 1997, 2001), which included a total of 15 AA participants aged 19 years or younger who provided care for an adult family member with cancer. Although one of the studies by Gates and Lackey (1998) focused on AA children and adolescents (N = 11) caring for a family member with cancer, none focused exclusively on the perspective of these children and adolescents in supportive care roles. Young caregivers in minority households often report that there are few people to help them (Hunt et al., 2005), and AA children and adolescents also live with the awareness that cancer carries a higher incidence and mortality rate for their relatives when compared to other racial and ethnic groups (DeSantis et al., 2019), as well as a stigma and fear that limits discussions about cancer in AA families (Haynes-Maslow et al., 2016). Therefore, it is essential that additional research explores the experiences of AA children and adolescents who are supporting a family member with cancer in their own words and through their own cultural lens (Kagawa-Singer et al., 2010).
This study retrospectively explored the experiences and needs of AA children and adolescents who were identified by their mother or grandmother with breast cancer as being a significant support individual for them at the time of diagnosis and treatment. Breast cancer survivors who received support also reported on the efforts and experiences of their children and grandchildren at the time of their initial diagnosis and treatment. This study contributes to the existing evidence pertaining to the needs and experiences of children and adolescents with a parent or close relative with breast cancer by specifically focusing on: (a) AA children and adolescents assuming supportive care roles, (b) the initial period following diagnosis in which patient and caregiver needs may be greatest, and (c) beliefs and actions of the mothers and grandmother receiving support from children or grandchildren. In this article, the term “young supporters” is used to describe the participants who were child or adolescent co-survivors during the time that they provided support to their mother or grandmother with breast cancer. The mothers and grandmother in this study are referred to as survivors.
Methods
Participants and Setting
Participants were recruited by posting informational flyers within a large cancer institute in the northeastern United States, through word of mouth within the local AA community, and from the principal investigator’s (PI’s) previous study participants. Potential participants were offered the opportunity to participate in either a focus group or an interview to suit their comfort and convenience (Lambert & Loiselle, 2008).
Recruited breast cancer survivors were asked to identify a young adult child or grandchild who was a child or adolescent at the time that they provided support to their mother or grandmother. Three focus groups were held with a total of six participants. The first focus group consisted of the breast cancer survivors, the second group consisted of the young supporters, and the third group consisted of all participants. Except for a granddaughter who lived near her grandmother, breast cancer survivors and young supporters lived together currently and when the support was provided.
Following the focus groups, six interviews were conducted with four participants (i.e., one interview with each participant, and interviews as pairs) to gain more in-depth knowledge of young supporters’ experiences at the time since diagnosis, as well as at differing ages, and to integrate interview data with focus group data for greater completeness (Lambert & Loiselle, 2008). Focus groups and interviews were held at the study institution’s School of Nursing, which is located in a community where a number of AA individuals reside. Free parking and accessible public transportation were available. It was believed that this location would be more acceptable to AA breast cancer survivors than the cancer center where they had received treatment and would also allow the researchers to access the building for evening and weekend focus groups and interviews for participant convenience.
Procedures
This study used multiple methods of data collection (focus groups and interviews) and sources of data (cancer survivors and young supporters) to enhance the quality and credibility of the findings (Patton, 2015). The study was approved by the Social and Behavioral Science Institutional Review Board at the PI’s university.
Survivors and young supporters provided written consent and completed a brief demographic information form. The PI moderated the survivor focus group and interviews. A local AA focus group moderator (B.B.), who was an experienced moderator and long-time local resident, conducted the focus group and interviews with the young supporters. B.B. was culturally concordant with the supporters and selected to facilitate the young supporters’ focus group and interviews to gather more robust data by promoting a comfortable atmosphere for them (Fryer et al., 2015; Krueger & Casey, 2015). The PI and B.B. jointly moderated the focus group and interviews with young supporters and breast cancer survivors together.
Focus groups were conducted using procedures outlined by Krueger and Casey (2015), which included welcoming participants, initiating an ice-breaker question, reminding participants to maintain confidentiality, and ensuring an opportunity for each participant to speak through the use of pauses, probing questions, and direct invitation by the moderator(s). Research assistants attended to practical needs of participants and took notes on participant interactions during the focus groups (Krueger & Casey, 2015). During the focus groups, a semistructured interview guide was used to collect data (see Figure 1). The interview guide was modified for the interviews based on the themes that developed from the initial analysis of the focus groups (Lambert & Loiselle, 2008). Because reflection is required to share one’s complete experience (Patton, 2015), participants were asked to reflect on their support experience. Each focus group lasted about one hour; interviews lasted about 30 minutes. After the focus groups were completed, the PI, B.B., and research assistants debriefed, with all team members developing a summary of their observations and impressions of the participants’ interactions, nonverbal responses, and statements (Krueger & Casey, 2015). Participants received free parking, a light meal, and a $50 grocery or gasoline gift card from a local store of their choosing for their participation. 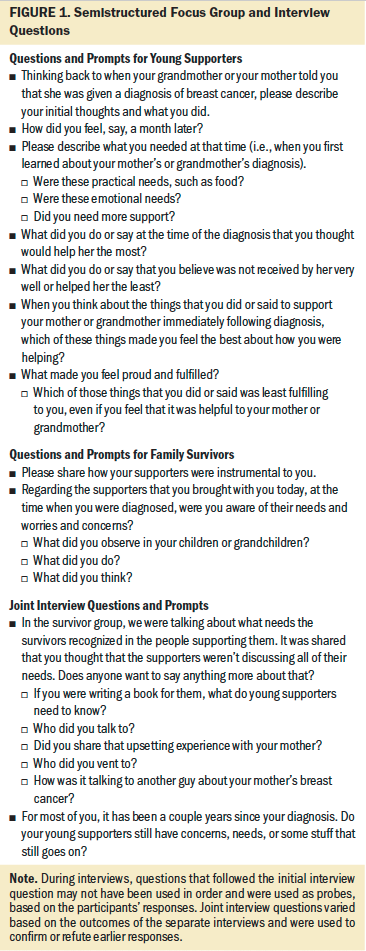
Data Analysis
Focus groups and interviews were digitally recorded, professionally transcribed, and deidentified for confidentiality.
The PI and research assistants independently read and coded the transcripts of the focus groups using qualitative conventional content analysis. Conventional content analysis was chosen so that themes originated from the data rather than from previously assumed knowledge of the phenomena (Hsieh & Shannon, 2005). The researchers shared their initial coding and generated preliminary joint coding and themes that were entered into ATLAS.ti, version 5.0. The local moderator, B.B., shared her impressions to support the analysis. Notes from the researchers’ debriefing after the focus groups also informed the analysis.
Conventional content analysis was also used to analyze the interview data. The research assistants independently coded the initial interview transcripts line by line and developed themes (Hsieh & Shannon, 2005). Existing focus group themes were combined with the interview themes and discussed among the researchers until thematic saturation was achieved. When differences occurred, the transcribed data were reviewed to determine the solution that most closely represented the data. As a validation check on saturation, a research assistant, who had not been involved in data collection and could provide an objective viewpoint (Patton, 2015), independently coded the interview transcripts using directed content analysis. When no additional themes emerged, recruitment and data collection were completed.
To enhance the credibility of the findings, data were also reviewed using participant inquiry and expert review (Patton, 2015). A summary of the developing themes was mailed to participating families, inviting their input into the generated themes. A draft of the results was provided to a prominent local AA breast cancer advocate, survivor, author, and mother of young children who experienced her diagnosis and treatment. She provided input on whether the themes were consistent with her experiences and those of AA families with whom she is involved in the local community. Comments that were received by email and telephone supported the themes found in this study and influenced the researchers’ thinking as findings were written to ensure that issues important to the participants were described.
In addition to triangulating methods and sources of data in this analysis (Lambert & Loiselle, 2008), the credibility and quality of this study was further supported by: (a) the collaboration of multiple researchers in the analysis of these data, several of whom shared the same race/ethnicity and were concordant in age with the young supporters (Fryer et al., 2015; Patton, 2015), (b) a PI experienced in qualitative research and psycho-oncology who personally trained members of the research team in focus group and analysis techniques, (c) the interprofessional contribution to the analysis and writing of this work by a psychologist (J.H.) with expertise in care of women with breast cancer and a psychology student who participated in the study’s conduct and interpretation of findings, (d) ongoing analysis throughout the data collection period that informed subsequent data collection, and (e) completing written documentation of all steps and decisions in the analysis (Patton, 2015).
Results
For young supporters, mean age when providing support was 15.6 years (SD = 4.98), with a range of 7–19 years. The mean current age of young supporters was 21.2 years (SD = 2.55), with a range of 18–24 years. The mean current age of family survivors was 55.25 years (SD = 4.11), with a range of 50–59 years. The mean number of years since diagnosis for family survivors was 5.5 years (SD = 5.74). All survivors had undergone surgery and received chemotherapy to treat their breast cancer. One survivor was currently receiving oral endocrine therapy. Sample demographic information is presented in Table 1. 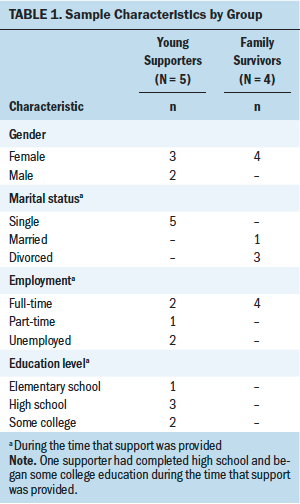
Young supporters in this study primarily provided tangible support for their mother or grandmother with breast cancer in the form of housecleaning, errands, ironing school clothes, cooking, physical care, and transportation for siblings or their mother or grandmother. One young supporter also described taking time off from her job and school to “do our mother’s job.” Emotional support was described less often by participants, but some young supporters reported conveying emotional support through prayer, presence, supportive text messages, and by helping survivors with their physical appearance. Young supporters who were daughters and granddaughters informed their mother or grandmother that they were praying for them, which was perceived as supportive for the survivor, who the young supporters described as faith based. It was important to female young supporters, as well as emotionally supportive to the survivors, to assist with the survivor’s personal appearance (e.g., hair or wigs, nails, skin care, makeup). Young supporters and survivors reported that they benefited from the sense of normalcy brought about by engaging in activities that helped to maintain the survivor’s usual, healthy appearance as much as possible.
Based on the findings from the focus groups and interviewers, young supporters’ experiences yielded 4 primary themes and 11 subthemes; survivors’ experiences yielded 3 primary themes and 3 subthemes (see Figure 2). Themes and subthemes are discussed further in the following sections. 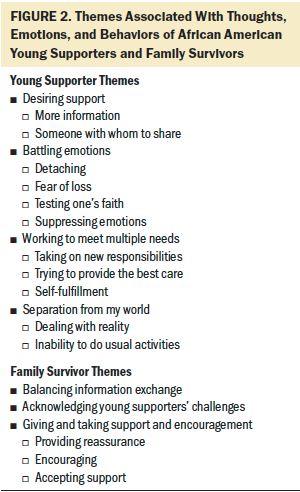
Young Supporter Themes
Desiring support: Young supporters expressed a strong need for support, particularly in the form of cancer-related information. Young supporters did not know where to find answers to their questions, such as how to feel and act when a loved one is diagnosed. Young supporters also reported that healthcare providers did not speak with them, and the resources that supporters identified were geared toward women with cancer, not families or adolescents: “If there was a book . . . I would have read it” (Participant 3). Reassurance that their mother or grandmother was going to survive was desperately needed; however, young supporters reported that this was a difficult question and one they were not comfortable asking: “You don’t want to ask what you don’t think they want to hear” (Participant 4).
Young supporters also desired support in the form of someone with whom to share. In this study, young supporters described being filled with anger and fear and having many unanswered questions, but they saw no opportunity to share these feelings with another individual who understood their experience: “I just really needed someone to talk to. . . . I didn’t have anyone to turn to” (Participant 2). Although a close friend at school may have provided an outlet, young supporters considered the cancer diagnosis to be personal and did not share that information widely in school: “I just didn’t want them to know” (Participant 1). Young supporters also reported that they feared upsetting their mother or grandmother by sharing their questions, worries, and fears. According to the young supporters, matriarchs of the AA households were perceived to be off-limits for questioning, and their families and the community generally avoided talking about cancer overall. One participant said the following:
It’s difficult because you don’t want to trouble the patient with your emotions, and you don’t want to talk about negativity among the family. [They say], “Let’s not talk about it. Let’s pray. Let’s think positive.” There’s nowhere to go in the community to speak about things to anyone. It’s like no one knows that African Americans and minorities are having cancer. You don’t know where to go. (Participant 4)
Battling emotions: Feeling that they were unable to ask questions and share their feelings, young supporters described how they battled with their emotions. Young supporters reported that they previously felt they had close relationships with their mother or grandmother and openly shared feelings and emotions, but a cancer diagnosis created a change. The change was described by participants as detaching from the previous patterns of sharing everything about themselves and their day with their mother or grandmother and becoming wary and cautious because their family member may be ill, worried, or having a bad day. Instead of talking to their mother or grandmother, young survivors found distractions: “I put distance between my grandmother [and me]. She didn’t seem like my grandmother anymore. It’s like, it’s over . . . a death sentence” (Participant 4).
The fear of loss and the emotional wall that young supporters felt existed between them and their mother or grandmother also created feelings of selfishness. One participant described battling these emotions as follows:
I was scared. I didn’t want to lose her, and I felt selfish. . . . I didn’t know how to be there for her because I was so wrapped in my own emotions. It was like fighting demons within myself because I’m like, she’s going through it . . . potentially losing her life, and I’m thinking about my own emotions. . . . I was angry at myself because I couldn’t control my own emotions. (Participant 3)
Feeling detached, fearful, and selfish often tested the faith of young supporters and led to them suppressing emotions, sometimes in destructive ways. Although some young supporters reported that prayer might be used to cope, the cancer diagnosis created a crisis of faith for others:
No, prayer’s not going to work. I had no faith, and I was raised faith based, and that shattered it for me. I just wanted to suppress these feelings that she was probably going to die . . . subconsciously get rid of her in my mind. . . . I was a young teenager, erratic. I would drink and hang out. (Participant 4)
Working to meet multiple needs: Young supporters often experienced multiple pressures to meet their own and their families’ needs. Taking on new responsibilities at home added to their existing responsibilities at school and work:
I felt a need to hold the family together. I can’t do this. I was like, “I’m not ready for this,” and I was just trying to balance working 45 hours a week, going to school, doing things around the house, like cooking dinner every night and being able to clean the house, just like, holding everything together. (Participant 1)
Being a caregiver to a loved one with cancer was an unfamiliar role, one at which the young supporters wanted to excel. However, trying to provide the best care posed additional challenges, for example:
She likes to know the truth, but I was afraid to tell her. Her health was deteriorating. She looked completely different, and I didn’t know the right thing to say, so I just continued to pray and say, “You look great.” “It’s in God’s hands.” “Let’s go pick out some wigs.” I started wearing a wig with her. Whatever to cope and make her feel better, I would do and say. (Participant 3)
The young supporters in this study self-reported missteps that they believed were not supportive to their mothers or grandmother. In hindsight, being overemotional and panicked and quitting jobs when the pressures became overwhelming was regretted by the young supporters. Regardless of the challenges and uncertainties they experienced, young supporters acknowledged that their new role was a source of self-fulfillment:
Where I can show something that she taught me in how I’m supporting her, that’s when I feel like I’m really proud of myself because it has taken a lot to get to this point, from being completely shut off, drinking, and just throwing my life down the drain. . . . I think God put that [diagnosis] in my life for me to realize how bad it can get and how you will be delivered. (Participant 4)
Separation from my world: While balancing their personal growth and the challenges associated with meeting their mother’s or grandmother’s needs, young supporters also felt pulled away from the person that they knew themselves to be and their reality—an internal and external separation from their world. Externally, the young supporters found that they had an inability to do their usual activities:
I was in a lot of after-school activities and stuff, but after school, I was like, “Go right home after school.” . . . Whatever she needed . . . I have to say even though it made her feel happy, I did not [feel happy]. I was missing out on my senior year of high school. . . . I felt like I was forced to grow up faster than other people. (Participant 1)
Internally, young supporters struggled with dealing with reality. Although they attempted to keep cancer from affecting all aspects of their lives, those realities continually collided. The struggle was described as “I just want to be able to live my life. Like, I have to face that [cancer] at home; I don’t want to face it everywhere I go” (Participant 1). Forgetting and realizing the potential gravity of the diagnosis weighed heavily on the young supporters in this study. For example:
Telling jokes [with grandmother], when the laughter would die, the realness and reality would settle back in. How do you stop pretending that everything is okay and really deal with it . . . at the matter of where it is? That was the biggest thing for me. (Participant 3)
Additional exemplars from the young supporter focus groups and interviews are presented in Figure 3. 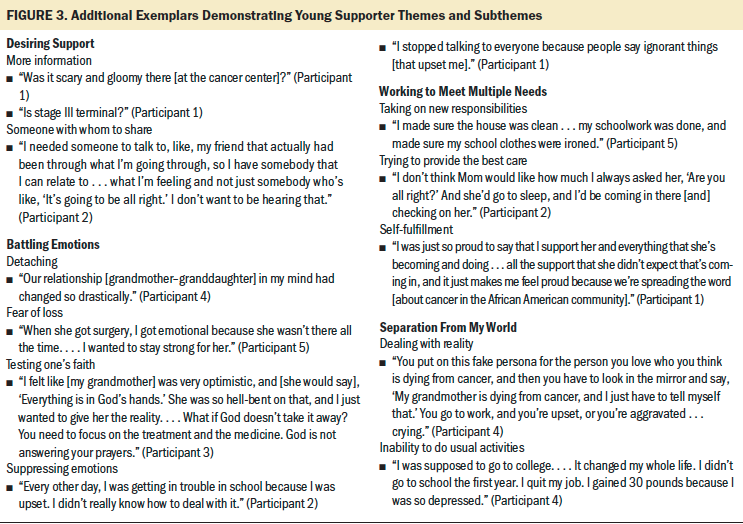
Survivor Themes
Balancing information exchange: Managing information on the breast cancer diagnosis and treatment was handled according to the usual parenting behaviors of the survivors in this study. Survivors reported that they balanced what they thought their children needed to know against what they would keep to themselves. One participant said, “How many times we as parents kept certain things from our kids, and they know that. They know Mom’s not telling me something” (Participant 8). Desiring support, the survivors found balancing information and emotional exchange to be challenging and, in retrospect, recommended open communication with young supporters from the time of initial diagnosis through their cancer trajectory:
I think it’s very important in your [survivor] piece if you can communicate and say, “It’s okay. . . . These emotions you are experiencing are okay” . . . so they don’t have to put the mask on [to hide their fears]. (Participant 6)
Acknowledging young supporters’ challenges: While relying on their young supporters for help, survivors reported acknowledging the challenges of their cancer diagnosis and the supportive role that it placed on their children and grandchildren. They also recognized that supporters’ themes of fear of loss and dealing with reality were particularly challenging. Despite survivors’ efforts to withhold their greatest fears, they understood that their children and grandchildren feared their death. Survivors reported shared experiences of being checked on by young supporters who feared they would die in their sleep. Although survivors believed their young supporters had moments of normality, symptoms, such as hair loss or visible fatigue, were perceived to jolt young supporters out of their world and back into the reality of cancer, regardless of the reassurances that the survivors provided. One participant reflected, “When I started losing my hair, then that’s when he said to himself, ‘I’m wondering what’s actually going on’” (Participant 7).
Outbursts of anger, frequent phone calling, and “going from 0 to 300” with volatile emotions demonstrated by young supporters were perceived by survivors as expressions of fear, “pent-up emotions,” and unanswered questions. Survivors emphatically expressed the need for young supporters to have healthcare professionals, support groups, or people outside of the family with whom they could express their actual fears and emotions and receive accurate answers to their questions. Survivors also reported that support for their children and grandchildren was not available and was particularly lacking for male young supporters.
Giving and taking support and encouragement: Survivors reported that there was a mutual give-and-take between themselves and the children or grandchildren providing them with support. Although survivors encouraged the young supporters and provided reassurance, they also accepted support in return. Encouragement came naturally for the survivors in this study; they maintained their desire for their children to fulfill their dreams and responsibilities as if nothing had changed. One participant said, “I was like, ‘Don’t worry about me. What I want you to do, I want you to finish school’” (Participant 7). Survivors encouraged their young supporters to talk about their concerns even when this was met by resistance. The survivors also perceived that the young supporters were driven by their fears and required their mother’s or grandmother’s reassurance: “Some days he didn’t want to go to school, but I told him, ‘I’m going to be here when you get back’” (Participant 7).
Receiving a cancer diagnosis and undergoing treatment raised survivors’ expectations for their children and grandchildren. In this study, survivors reported that it was comforting and, at times, necessary that the young supporters returned home immediately after school to do housework, provide child care, cook, and complete errands the survivors had not been able to do throughout the day. One participant acknowledged that this was not easy for her child, saying that “it was physically difficult, but she . . . over time, she just took the role of the caretaker” (Participant 6). Survivors also expressed pride that their children rose to the occasion and into their supportive care role despite its challenges.
Discussion
This study contributes new knowledge about the needs and experiences of young AA supporters of a family member with breast cancer, as well as perspectives of AA breast cancer survivors who received support from their children at the time of diagnosis and during treatment. The findings of a previous study by Walczak et al. (2018) on the coping needs of children and adolescents living in families affected by parental cancer indicate that children require strong communication and additional cancer-related information and that these needs often go unmet. These findings are consistent with the findings of the current study. In a study by Davey et al. (2011), AA young supporters did their best to provide emotional and practical support for their parents with cancer while they experienced feelings of isolation and loss, as well as changes in their interactions with the parent with cancer. Similar to Davey et al.’s (2011) findings, young supporters in the current study reported using distractions to cope and recommended that support groups be developed for young supporters of parents with cancer. Consistent with the findings of a study by Kissil et al. (2010), the young supporters in the current study also believed that they experienced personal growth from their caregiving experience. Importantly, in the current study and previous studies (Davey et al., 2011; Lackey & Gates, 2001), the need for healthcare providers to acknowledge children and adolescents in supportive care roles as co-survivors in the parental cancer experience was strongly endorsed.
The current study provides new data beyond the existing literature by focusing on children’s needs when in a supportive care role for a family member with cancer. For example, whereas Davey et al. (2011) found that prayer and wishful thinking were used to decrease anxiety among children and adolescents living with a parent with cancer, young supporters in the current study used prayer less for themselves but more as a form of emotional support for their family member. Young supporters in this study reflected on their faith, questioned God, and reported crises in their own faith following their family member’s cancer diagnosis. In addition, Davey et al. (2011) found that AA children and adolescents engaged in helpful behaviors to cope and turned to other family members for support, whereas young supporters in the current study expressed the desire to emotionally and mentally process their own experience and looked outside the family for support. Families in the current study reported that they purposefully avoided talking about cancer and sharing emotions. As a result of finding little support in the AA community, some of the young supporters reported that, in some instances, they coped by acting out, losing or quitting jobs, and abusing alcohol.
In this study, information sharing was strikingly absent from the reports of young AA supporters. Universally, young supporters in this study described being kept “in the dark” about their family members with cancer and where to locate additional education or cancer-related information, both personally and within the AA community. Although the Internet was available to them, young supporters did not report that they obtained additional information on cancer online. This may be a result of distrusting information found on the Internet and not having a trusted individual with whom to validate the information that they may have found. Clinicians did not provide young supporters with education resources, nor did young supporters request additional information from clinicians, which is an unsurprising finding because overlooking the needs of survivors’ children has been previously documented (Lewis, 2007). Young AA supporters may not ask for additional information because of what is referred to as disenfranchised grief (Davey et al., 2011), a feeling of young supporters in which they view that their validity as supporters and information seekers is questioned in the eyes of clinicians and the community. Comparatively, peers of the young supporters in this study who had similar experiences validated the young supporters’ caregiving role and became trusted sources of information when they were available, despite the risk of receiving misinformation. These findings highlight the importance of creating culturally appropriate interventions for AA children and adolescents who may experience greater distrust and disenfranchisement from the healthcare system than White children and adolescents (Davey et al., 2013; Halbert et al., 2006).
Although about 2–14 years had passed since the cancer diagnosis of the survivors in this study, survivors and young supporters had not discussed many issues surrounding their experience as co-survivors of cancer until the study began. Young supporters reported believing that their mother or grandmother did not understand what they were experiencing during the cancer trajectory, which was partially true based on reports from survivors. The findings demonstrated that survivors acknowledged some of the feelings of their young supporters at the time of this experience, such as fear of loss and difficulty dealing with the new reality of the cancer, which is consistent with previous research on children and parental cancer (Davey et al., 2012). However, according to the reports of young supporters in this study, the survivors’ actions or words were not successful in helping them to cope, and, in some cases, precluded them from getting their needs met. The survivors acknowledged that the joint interview after the individual interviews and focus groups provided them with greater awareness of the extent to which their cancer affected their children and grandchildren.
Limitations
Although steps were taken to support the rigor of this study, several limitations should be considered when reviewing the findings. The size of the AA population of women and their young adult children who were available and willing to participate in the study was limited, and, therefore, findings from a larger sample size may have varied. In addition, the study institution’s School of Nursing was selected as the location to conduct the focus groups and interviews; it is unknown whether choosing a different setting would have been accessible to more women with breast cancer and their children and increased participation. Because the study was conducted in a larger urban city in the northeastern United States, findings may not be generalizable across other AA populations.
Implications for Nursing
The findings of this study suggest that it is important for oncology nurses to continue to explore the needs of AA families and develop and implement culturally adapted interventions for AA women with breast cancer receiving treatment and their children and adolescents in supportive care roles. Interventions for young AA supporters should include age-appropriate information on cancer survival, treatments, and side effects, as well as guidance on how to maintain a relationship with, communicate with, and support parents or grandparents with breast cancer. Nurses should educate parents and grandparents on the stressors that are associated with being a child or adolescent in a supportive care role for a family member with cancer. Encouraging mutual discussions about young AA supporters’ roles can help to align parents’ and grandparents’ expectations with that of their children. Nurses should also promote open and honest communication among young AA supporters and their parents and grandparents. Given the disparate burden of cancer and lower survival rates for AAs compared to other racial and ethnic groups, nurses should navigate discussions about prognosis whenever possible, which can mitigate fears and anxiety for young AA supporters. Based on the study’s findings, it is suggested that oncology nurses assess whether AA women with breast cancer desire and expect their children to be included in their clinical appointments and which roles they wish nurses and healthcare providers to play in sharing information about their cancer with their children. In addition, the findings suggest that nurses are essential in acknowledging young AA supporters as potential caregivers and, with parental support, recommending support groups or additional resources for counseling to improve their experience in a supportive care role for a parent or grandparent with cancer. 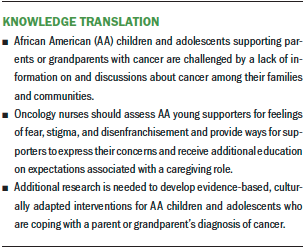
Conclusion
Research exploring the experiences of AA children and adolescents caring for a parent or grandparent with cancer is limited. Similar to previous research on parental cancer and children, family communication, support, and information were identified by the participants in this study as significant needs for young AA supporters following a parent or grandparent’s diagnosis. In addition, young AA supporters report experiencing fear of their family members’ death and taking on many new time-intensive responsibilities that can disrupt school and work and negatively influence emotional and physical well-being. Nurses caring for AA women with breast cancer are in a key position to assess the family support structure and address information and family communication needs. Additional research is needed to determine how to efficiently and effectively deliver psychosocial and informational interventions to young AA supporters that is age-appropriate and culturally adapted to best meet their needs when their family is affected by breast cancer. 
The authors gratefully acknowledge Ameera Fayad, RN, BSN, Beverly Burch, and Christopher Moon, BSN, RN, for their contributions to the conduct of this study, and Mercedes Wilson for review of the manuscript and expert consultation.
About the Author(s)
Robin M. Lally, PhD, RN, MS, BA, AOCN®, FAAN, is a professor in the College of Nursing at the University of Nebraska Medical Center and the Fred and Pamela Buffett Cancer Center in Omaha; and Jennifer Hydeman, PhD, is a psychologist in the Department of Psychology at the Roswell Park Comprehensive Cancer Center; Catherine Brooks, BA, is a graduate student at D’Youville College; Halima Akter, BA, is a graduate student in the School of Public Health and Health Professions at the University at Buffalo; and Megan T. Yoerg, BSN, RN, is an RN at Mercy Hospital, all in Buffalo, NY. This research was supported, in part, by an American Cancer Society Mentored Research Scholar Grant (MRSG-11-101-01-CPPB) and the Community Foundation of Greater Buffalo. Lally has received additional support from the Fred and Pamela Buffett Cancer Center, the Great Plains IDeA-CTR of the University of Nebraska, and Pfizer in collaboration with the National Comprehensive Cancer Network Oncology Research Program. Lally and Hydeman contributed to the conceptualization and design. Lally and Brooks completed the data collection. All authors provided the analysis and contributed to the manuscript preparation. Lally can be reached at robin.lally@unmc.edu, with copy to ONFEditor@ons.org. (Submitted March 2019. Accepted September 23, 2019.)
References
American Cancer Society. (2017). Breast cancer facts and figures, 2017–2018. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
American Cancer Society. (2019). Cancer facts and figures for African Americans, 2019–2021. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
Davey, M.P., Kissil, K., Lynch, L., Harmon, L., & Hodgson, N. (2013). A culturally adapted family intervention for African American families coping with parental cancer: Outcomes of a pilot study. Psycho-Oncology, 22(7), 1572–1580. https://doi.org/10.1002/pon.3172
Davey, M.P., Niño, A., Kissil, K., & Ingram, M. (2012). African American parents’ experiences navigating breast cancer while caring for their children. Qualitative Health Research, 22(9), 1260–1270. https://doi.org/10.1177/1049732312449211
Davey, M.P., Tubbs, C.Y., Kissil, K., & Niño, A. (2011). “We are survivors too”: African-American youths’ experiences of coping with parental breast cancer. Psycho-Oncology, 20(1), 77–87. https://doi.org/10.1002/pon.1712
DeSantis, C.E., Miller, K.D., Sauer, A.G., Jemal, A., & Siegel, R.L. (2019). Cancer statistics for African Americans, 2019. CA: A Cancer Journal for Clinicians, 69(3), 211–233. https://doi.org/10.3322/caac.21555
Fryer, C.S., Passmore, S.R., Maietta, R.C., Petruzzelli, J., Casper, E., Brown, N.A., . . . Quinn, S.C. (2015). The symbolic value and limitations of racial concordance in minority research engagement. Qualitative Health Research, 26(6), 830–841. https://doi.org/10.1177/1049732315575708
Gates, M.F., & Lackey, N.R. (1998). Youngsters caring for adults with cancer. Image: The Journal of Nursing Scholarship, 30(1), 11–15. https://doi.org/10.1111/j.15475069.1998.tb01229.x
Halbert, C.H., Armstrong, K., Gandy, O.H., & Shaker, L. (2006). Racial differences in trust in health care providers. Archives of Internal Medicine, 166(8), 896–901. https://doi.org/10.1001/archinte.166.8.896
Haynes-Maslow, L., Allicock, M., & Johnson, L. (2016). Cancer support needs for African American breast cancer survivors and caregivers. Journal of Cancer Education, 31(1), 166–171. https://doi.org/10.1007/s13187-015-0832-1
Hsieh, H.F., & Shannon, S.E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. https://doi.org/10.1177/1049732305276687
Hunt, G., Levine, C., & Naiditch, L. (2005). Young caregivers in the U.S.: Findings from a national survey. National Alliance for Caregiving. https://www.caregiving.org/pdf/research/youngcaregivers.pdf
Kagawa-Singer, M., Padilla, G.V., & Ashing-Giwa, K. (2010). Health-related quality of life and culture. Seminars in Oncology Nursing, 26(1), 59–67. https://doi.org/10.1016/j.soncn.2009.11.008
Kissil, K., Niño, A., Jacobs, S., Davey, M., & Tubbs, C.Y. (2010). “It has been a good growing experience for me”: Growth experiences among African American youth coping with parental cancer. Families, Systems, and Health, 28(3), 274–289. https://doi.org/10.1037/a0020001
Krueger, R.A, & Casey, M.A. (2015). Focus groups: A practical guide for applied research (5th ed.). Sage.
Lackey, N.R., & Gates, M.F. (1997). Combining the analyses of three qualitative data sets in studying young caregivers. Journal of Advanced Nursing, 26(4), 664–671. https://doi.org/10.1046%2Fj.1365-2648.1997.00367.x
Lackey, N.R., & Gates, M.F. (2001). Adults’ recollections of their experiences as young caregivers of family members with chronic physical illnesses. Journal of Advanced Nursing, 34(3), 320–328. https://doi.org/10.1046/j.1365-2648.2001.01761.x
Lambert, S.D., & Loiselle, C.G. (2008). Combining individual interviews and focus groups to enhance data richness. Journal of Advanced Nursing, 62(2), 228–237. https://doi.org/10.1111/j.13652648. 2007.04559.x
Lewis, F.M. (2007). Parental cancer and dependent children: Selected issues for future research. Psycho-Oncology, 16(2), 97–98. https://doi.org/10.1002/pon.1141
Marziliano, A., Moyer, A., & Applebaum, A. (2014). Challenges facing adolescent and young adult cancer caregivers: A systematic review [Abstract P1-47]. Psycho-Oncology, 23(Suppl. 1), 1–144. https://doi.org/10.1002/pon.3478
National Cancer Institute. (n.d.). NCI dictionary of cancer terms: Survivorship. Retrieved from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/survi…
Niemelä, M., Marshall, C.A., Kroll, T., Curran, M., Koerner, S.S., Räsänen, S., & García, F. (2016). Family-focused preventive interventions with cancer cosurvivors: A call to action. American Journal of Public Health, 106(8), 1381–1387. https://doi.org/10.2105/AJPH.2016.303178
Northouse, L.L., Katapodi, M.C., Schafenacker, A.M., & Weiss, D. (2012). The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Seminars in Oncology Nursing, 28(4), 236–245. https://doi.org/10.1016/j.soncn.2012.09.006
Patton, M.Q. (2015). Qualitative research and evaluation methods (4th ed.). Sage.
Shah, B.K., Armaly, J., & Swieter, E. (2017). Impact of parental cancer on children. Anticancer Research, 37(8), 4025–4028. https://doi.org/10.21873/anticanres.11787
Soler-Vila, H., Kasl, S.V., & Jones, B.A. (2003). Prognostic significance of psychosocial factors in African-American and white breast cancer patients: A population-based study. Cancer, 98(6), 1299–1308. https://doi.org/10.1002/cncr.11670
Walczak, A., McDonald, F., Patterson, P., Dobinson, K, & Allison, K. (2018). How does parental cancer affect adolescent and young adult offspring? A systematic review. International Journal of Nursing Studies, 77, 54–80. https://doi.org/10.1016/j.ijnurstu.2017.08.017
Weaver, K.E., Rowland, J.H., Alfano, C.M., & McNeel, T.S. (2010). Parental cancer and the family: A population-based estimate of the number of US cancer survivors residing with their minor children. Cancer, 116(18), 4395–4401. https://doi.org/10.1002/cncr.25368
Yoo, G.J., Aviv, C., Levine, E.G., Ewing, C., & Au, A. (2010). Emotion work: Disclosing cancer. Supportive Care in Cancer, 18(2), 205–215. https://doi.org/10.1007/s00520-009-0646-y
Yoo, G.J., Levine, E.G., & Pasick, R. (2014). Breast cancer and coping among women of color: A systematic review of the literature. Supportive Care in Cancer, 22(3), 811–824. https://doi.org/10.1007/s00520-013-2057


