Guideline-Recommended Symptom Management Strategies That Cross Over Two or More Cancer Symptoms
Problem Identification: Patients with cancer experience multiple symptoms, but current practice is driven by guidelines that address single symptoms. Identifying symptom management strategies recommended across two or more symptoms could relieve multiple symptoms and reduce patient burden.
Literature Search: The Oncology Nursing Society, National Comprehensive Cancer Network, and American Society of Clinical Oncology websites were searched to identify management guidelines for 15 symptoms.
Data Evaluation: The authors extracted symptom management strategies and recommendations. Recommendations were synthesized by symptom across the guidelines, and recommended strategies were compared across symptoms.
Synthesis: Among 32 guidelines reviewed, a total of 88 symptom management strategies (41 pharmacologic, 47 nonpharmacologic) were recommended across two or more symptoms.
Implications for Practice: Findings support the potential for coordinated selection of symptom management strategies that cross over multiple symptoms in a patient. Investigators should test these symptom management strategies in the context of co-occurring symptoms and develop guidelines that address multiple symptoms.
Jump to a section
Patients with cancer experience a substantial number of symptoms, particularly during the periods of diagnosis and treatment. In seminal work, Portenoy et al. (1994) estimated the average number to be as high as 12 symptoms. In more recent studies, investigators have identified from 8 to 19 symptoms experienced by more than 40% of patients (Kirkova et al., 2009; Reilly et al., 2013). The specific symptoms that patients experience are likely to vary over time; for example, pain related to oncologic surgery may resolve in the acute recovery period, and new symptoms of nausea, fatigue, sleep disturbance, and dry mouth may emerge with their own patterns and duration during chemotherapy or radiation therapy regimens. Some of these symptoms may be related and emerge as symptom clusters (i.e., stable groups of concurrent symptoms that are related to one another and distinct from other symptom clusters) (Barsevick, 2016; Miaskowski et al., 2004); others may occur unrelated to other symptoms. Regardless, patients must contend with the management of multiple, often co-occurring symptoms.
Although patients routinely experience multiple symptoms, current practice generally follows a siloed approach to treatment. That is, providers use single-symptom evidence-based guidelines to direct treatment recommendations. Organizations, such as the Oncology Nursing Society (ONS), have published individual guidelines and guidance for the management of cancer-related anxiety (ONS, 2017c), cancer-related fatigue (ONS, 2017k), and cancer-related sleep–wake disturbances (ONS, 2017r), but have not provided recommendations for the management of these three symptoms when they co-occur. For the purpose of this article, guidance and guidelines from these organizations are referred to as “guidelines.” Other organizations have published guidelines that address various symptoms caused by a particular treatment strategy (e.g., American Society of Clinical Oncology [ASCO] guidelines for adverse events from immune checkpoint inhibitor therapy) (Brahmer et al., 2018) or at a particular phase of illness (e.g., National Comprehensive Cancer Network [NCCN] survivorship [2017b] or palliative care [2018e] guidelines), but still direct treatment to individual symptoms. Although some experienced clinicians may recognize that certain medications may offer multiple benefits (e.g., olanzapine may relieve nausea and vomiting and also improve sleep), this is not standard symptom management practice. The current approach facilitates clinicians’ ability to target the treatment of individual symptoms, but coordinating treatment recommendations across symptoms could provide a more efficient, less burdensome, and more cost-effective approach.
Patient versions of professional guidelines for symptom management also use a single-symptom approach. Patients who report multiple symptoms are likely to receive educational materials for individual symptoms, each of which describes various medications and self-management strategies that target a single symptom. A patient reporting the common symptom cluster of co-occurring pain, fatigue, and sleep disturbance may receive (a) pain education materials that recommend analgesic medications, distraction, heat and cold application, and acupuncture; (b) fatigue education materials that recommend activity pacing and exercise, dietary changes, and stimulant medications; and (c) sleep education materials that recommend sleep hygiene, relaxation exercises, and sedative medications. These multiple treatment recommendations are made without consideration of how strategies for one symptom may influence other symptoms or interact with other treatments. Schenker et al. (2019) demonstrated that polypharmacy is common among individuals with cancer who have high symptom burden and may be at least partially because of the prescription of new medications to treat side effects of other medications. In the process of self-management, patients and families are challenged to select among multiple treatment recommendations for each symptom and to implement multiple strategies to effectively address multiple symptoms or to prioritize management of select symptoms over others and then suffer the remaining unrelieved symptom burden (Coolbrandt et al., 2016).
When a single underlying cause of multiple co-occurring symptoms cannot be identified or cannot be intervened upon (e.g., where the shared cause of symptoms is the cancer therapy), it may be possible to coordinate management strategies that are effective for more than one of the symptoms present. For example, guidelines for each of the four co-occurring symptoms of neuropathic pain, nausea, fatigue, and anxiety may recommend cognitive behavioral therapy as an effective strategy. Alternatively, the four symptoms may respond to a combination of two treatments—an antidepressant for pain and anxiety and meditation for nausea and fatigue.
The distress of experiencing multiple symptoms, the burden and cost of managing multiple treatment strategies, and the potential risks of polypharmacy might be reduced by leveraging current guidelines to identify treatment strategies with potential effects on more than one of the patient’s symptoms. Identifying treatment strategies that are recommended across two or more symptoms is an important first step in facilitating a shift in practice from single- to multi-symptom management. Findings may (a) encourage practitioners to select and recommend treatment options that may have multiple benefits and (b) provide direction for future development and testing of interventions that will inform evidence-based multi-symptom or symptom cluster management guidelines. The current authors undertook a review of symptom management guidelines from three oncology professional practice organizations in the United States: ASCO, NCCN, and ONS. The authors’ aims were as follows:
• Describe the number and types of symptom management strategies recommended in the guidelines.
• Identify symptom management strategies recommended across two or more symptoms.
In this first step, the objective was to demonstrate, in principle, the potential for coordinated management of multiple symptoms by highlighting where guidelines overlap across symptoms in the treatment strategies recommended. The authors do not make specific multi-symptom treatment recommendations or provide instructions for prescribing or implementing treatments.
Methods
In this initial attempt to evaluate the potential for coordinating management of multiple symptoms, the authors employed a review and synthesis of recommendations from a limited set of symptom management guidelines. Because no standardized approach exists for this novel purpose, a step-wise systematic approach was established that included the following:
• Selection of oncology organizations who publish symptom guidelines
• Identification of symptoms of interest
• Extraction of symptom management recommendations in duplicate
• Categorization of symptom management strategies
• Documentation of strategies and associated recommendations across symptoms
The authors selected three U.S.-based oncology organizations that publish widely used practice guidelines: ASCO, NCCN, and ONS. Guidelines from non-U.S. organizations were excluded because of differences in approval or availability of certain medications or nonpharmacologic treatment strategies. A total of 15 symptoms of interest were identified; 13 were recognized as core symptoms to be measured in adult cancer clinical trials by the Center for Medical Technology Policy (Basch et al., 2012) and the National Cancer Institute Symptom Management and Health-Related Quality of Life Steering Committee (Reeve et al., 2014), plus two additional symptoms recognized as being of high or increasing prevalence and for which symptom management guidelines were available (see Figure 1). Skin reactions were included as common side effects of targeted therapies, which are being increasingly used in precision management of cancer (Bryce & Boers-Doets, 2014). Hot flashes were included as prevalent and distressing side effects of the most common cancers (breast and prostate cancer), which may affect patients’ willingness to adhere to hormonal therapies (Fisher et al., 2013). Each organization’s website was then searched to identify the most recent (up to 2018) guidelines addressing any of the 15 symptoms. Guidelines from all three organizations provided recommendations for nausea and vomiting combined, which are, therefore, subsequently reported as a symptom pair. 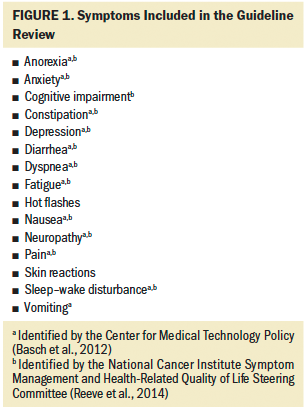
For each guideline, the authors identified the key characteristics, including the disciplines represented on the guideline panel, the evidence considered in developing the guideline, and the scope of the search. Each guideline was then examined for symptom management recommendations by at least two reviewers. The first reviewer extracted treatment strategies, associated recommendations, and the strength of evidence supporting the recommendation into symptom-specific tables. A second reviewer then double-checked the accuracy of the extraction and evaluated the guidelines for any relevant information missed by the first reviewer. For NCCN guidelines, the authors extracted strategies presented in the decision trees regardless of whether or not they were detailed in supporting text.
The research team subsequently reviewed all symptom management strategies and coded them into categories of pharmacologic (e.g., conventional medications, dietary supplements) or nonpharmacologic (e.g., physical, psychological, behavioral, complementary and alternative) approaches. Similar strategies were grouped together (e.g., medications in the same drug class, various meditation techniques). If levels of evidence differed among the strategies grouped together, the highest level of evidence cited within the group was reported.
Finally, recommendations across the three guidelines were summarized by symptom. Where there were disagreements between guidelines, the authors relied on the most recently conducted review (i.e., latest evidence). Treatment recommendations across all 15 symptoms were then compared to identify strategies recommended for two or more symptoms.
Characteristics of guideline development were summarized qualitatively. Descriptive statistics (n, %) were used to summarize the number and type of strategies recommended, including those recommended across two or more symptoms.
Results
Guideline Characteristics
A total of 32 guideline documents were reviewed and their recommendations included in the current synthesis (Anderson et al., 2014; Benson et al., 2004; Bower et al., 2014; Brahmer et al., 2018; Hesketh et al., 2017; Hirshman et al., 2014; NCCN, 2017a, 2017b, 2018a, 2018b, 2018c, 2018d, 2018e; ONS, 2017a, 2017b, 2017c, 2017d, 2017e, 2017f, 2017g, 2017h, 2017i, 2017j, 2017k, 2017l, 2017m, 2017n, 2017o, 2017p, 2017q, 2017r; Paice et al., 2016). The majority of ASCO and NCCN guideline panel members were physicians, but panels also included representatives from nursing, psychology, pharmacy, osteopathic medicine, social work, nutrition science, and patient advocacy, and (rarely) patients (Anderson et al., 2014; Benson et al., 2004; Bower et al., 2014; Brahmer et al., 2018; Hesketh et al., 2017; Hirshman et al., 2014; NCCN, 2017a, 2017b, 2018a, 2018b, 2018c, 2018d, 2018e; Paice et al., 2016). In contrast, panel members involved in writing ONS guidelines were all nurses (Johnson, 2014).
Databases used in ASCO searches varied across guidelines, with MEDLINE®, PubMed®, and Embase® used most frequently. Development of the neuropathy guideline also included searching the Allied and Complementary Medicine Database (Anderson et al., 2014; Benson et al., 2004; Bower et al., 2014; Brahmer et al., 2018; Hesketh et al., 2017; Hirshman et al., 2014; Paice et al., 2016). NCCN searches primarily used PubMed (NCCN, 2017a, 2017b, 2018a, 2018b, 2018c, 2018d, 2018e). Databases searched in developing ONS guidelines included PubMed and CINAHL® (Johnson, 2014). For ONS guidelines addressing pain management, the Cochrane Collaboration and NCCN were also searched (ONS, 2017a, 2017f, 2017p).
ASCO panels either adapted existing guidelines (i.e., anxiety and depressive symptoms, and fatigue) (Anderson et al., 2014; Bower et al., 2014) or developed new guidelines as needed (Benson et al., 2004; Brahmer et al., 2018; Hesketh et al., 2017; Hirshman et al., 2014; Paice et al., 2016). Where new guidelines were developed, evidence considered by ASCO teams varied by symptom, with some limited to randomized clinical trials and meta-analyses (e.g., antiemetics, neuropathy) (Hesketh et al., 2017; Hirshman et al., 2014) and others including a broader range of relevant literature, unpublished data, and professional experience (e.g., diarrhea) (Benson et al., 2004). Evidence considered in developing NCCN guidelines included clinical trials (phases 2–4), guidelines, meta-analyses, randomized controlled trials, systematic reviews, and validation studies (NCCN, 2017a, 2017b, 2018a, 2018b, 2018c, 2018d, 2018e). Evidence considered in developing ONS guidelines included intervention studies published as full research reports, systematic reviews, guidelines, or meta-analyses. All excluded gray literature, and most excluded descriptive studies (Johnson, 2014).
Guideline Recommendations
Symptom management strategies: A total of 167 treatment strategies were identified across the various symptom management guidelines. Of 102 pharmacologic strategies, 47 were conventional medications and 55 were dietary supplements (e.g., herbs, vitamins, probiotics, homeopathic or ayurvedic medicines). Among the 65 nonpharmacologic strategies, 25 were psychological strategies, 22 were physical strategies, 7 were behavioral strategies, and 11 were complementary and alternative therapies.
By symptom, the greatest number of strategies were identified for fatigue (n = 64), pain (n = 51), anxiety (n = 42), and depression (n = 39). The fewest number of strategies were identified for dyspnea (n = 17), skin reactions (n = 19), and constipation (n = 20). More than 20 strategies were identified for each of the remaining symptoms of anorexia, cognitive impairment, diarrhea, hot flashes, nausea and vomiting, neuropathy, and sleep–wake disturbance.
Consistent and conflicting recommendations: Strategies were noted as follows:
• Recommended (effective based on strong or moderate evidence)
• Potential benefit (based on expert opinion or weak evidence, effectiveness not established, advised to weigh potential benefits against harms)
• Not recommended (ineffective based on evidence of unlikely effectiveness or clear ineffectiveness)
A total of 456 recommendations were made. The vast majority of recommendations regarding a treatment strategy were made by a single guideline (e.g., distraction was recommended for fatigue in the NCCN guideline but was not mentioned in ONS or ASCO guidelines), or by multiple guidelines that were in full (e.g., yoga was recommended in ONS, NCCN, and ASCO guidelines for fatigue) or partial (e.g., massage was recommended in ONS and NCCN guidelines for fatigue, and the ASCO guidelines noted potential benefit) agreement. Disagreements in recommendations were identified for 4 of the 456 recommendations (less than 1%). One guideline (ONS, 2017k) noted a potential benefit of using an antidepressant for fatigue, and another guideline (NCCN, 2018b) indicated that antidepressants were not recommended. In three cases, recommendations conflicted. The use of cannabinoids for anorexia was recommended by NCCN (2017b) but not recommended for practice by ONS (2017b). Corticosteroids were recommended for certain types of pain by NCCN (2018a), recommended as having potential benefit by ONS (2017a, 2017f), and not recommended by ASCO (Paice et al., 2016). Similarly, mixed agonist/antagonist opioids were recommended for chronic pain by ONS (2017f) but not recommended by NCCN (2018a).
Strategies recommended for two or more individual symptoms: Among the 167 treatment strategies, 88 were identified as recommended or potentially beneficial for more than one symptom. These included 41 pharmacologic strategies (26 conventional medications and 15 dietary supplements) and 47 nonpharmacologic strategies (13 physical strategies, 4 behavioral strategies, 22 psychological strategies, and 8 complementary and alternative therapies). All 15 symptoms were addressed by one or more of these 88 strategies. Twenty-six strategies were identified as recommended or potentially beneficial for 2 symptoms, 16 strategies were similarly identified for 3 symptoms, 19 strategies were identified for 4 symptoms, and 27 strategies were identified for 5 or more symptoms.
Discussion
The review of guidelines identified a substantial number of symptom management strategies with potential benefit across multiple cancer symptoms, including conventional and complementary pharmacologic and nonpharmacologic approaches. Symptom management recommendations were relatively consistent across guidelines, and there were few conflicting recommendations. These initial findings suggest that it may be possible to coordinate selection of management strategies across a patient’s symptoms and decrease the number of strategies recommended to patients with multiple co-occurring symptoms, reducing patient self-management burden. For a patient with three co-occurring symptoms (e.g., pain, anxiety, and hot flashes), current clinical practice driven by single symptom guidelines could result in more than 40 different treatment recommendations; however, coordinating symptom management strategies and selecting those with overlap across symptoms substantially minimizes management burden (see Figure 2). Achieving the paradigm shift from single- to coordinated multi-symptom management, however, will require several additional steps that include building evidence around multi-symptom management, emphasizing patient-reported outcomes in research and clinical practice, revising and updating practice guidelines, and developing technological resources to facilitate operationalization of multi-symptom management. 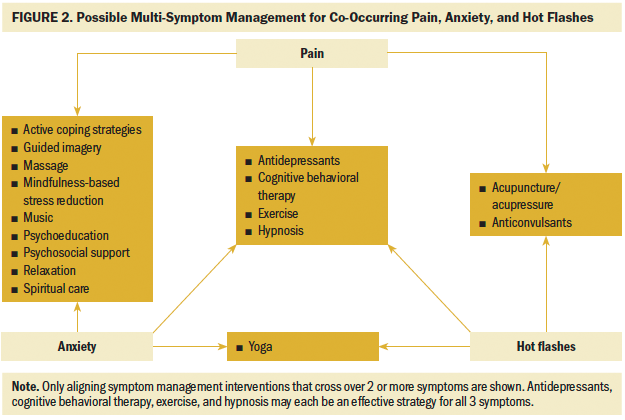
Future Research
Building evidence for multi-symptom management: About 20 years ago, when the concept of symptom clusters was initially introduced, Dodd et al. (2001) suggested that two symptoms may be addressed simultaneously. The current review identified 88 symptom management strategies that may benefit more than a single symptom. Five strategies were recommended for nine or more symptoms:
• Exercise (12 symptoms)
• Psychoeducation (11 symptoms)
• Antidepressants (9 symptoms)
• Acupuncture/acupressure (9 symptoms)
• Relaxation (9 symptoms)
However, very few of these strategies have been tested in studies designed to target management of multiple co-occurring symptoms. Tables 1–6 identify numerous symptom management strategies, the efficacy of which could be validated for multi-symptom management or treating known symptom clusters in large-scale trials. Such studies should carefully evaluate the symptom management strategies noted as being potentially beneficial in the current review to provide more definitive evidence of their usefulness. With respect to pharmacotherapies, factors such as specific drugs within a class, dosing recommendations, and priority (first- versus second- or third-line therapy) will need to be addressed in further development and testing of coordinated multi-symptom management interventions. 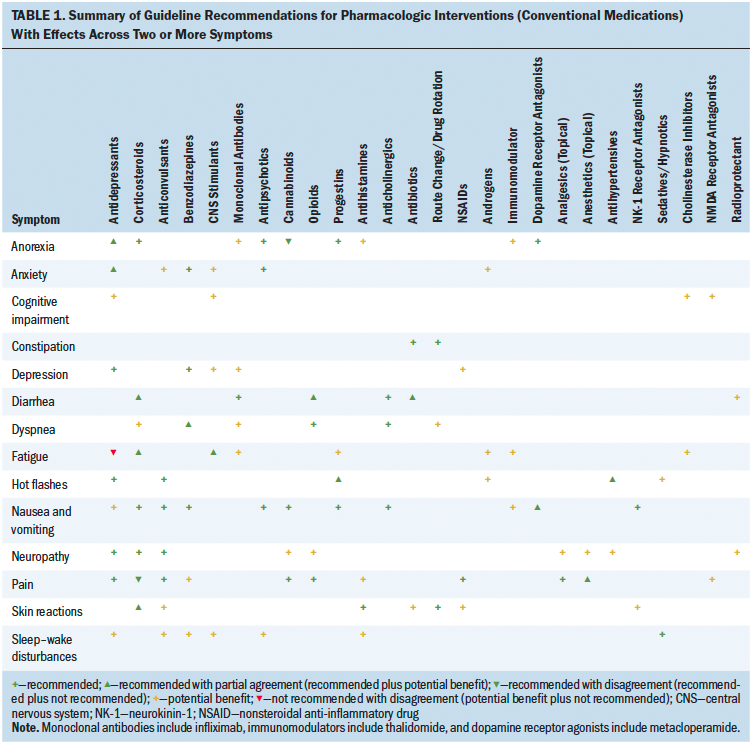
Emphasizing patient-reported outcomes: Management of multiple symptoms must begin with careful assessment of co-occurring symptoms. Researchers have long understood that people with cancer hesitate to report their symptoms for fear of distracting the oncologist from treating the cancer (Shun et al., 2009; Ward et al., 1993). The use of patient-reported outcomes in practice (particularly through automated systems that log symptoms in the electronic health record, notify clinicians when symptoms worsen, and even trigger a care referral) can facilitate improved symptom management (Yang et al., 2018) and quality of life (Basch et al., 2016) and potentially extend survival (Basch et al., 2017). Development and testing of multi-symptom management interventions should include similar symptom, functional status, and quality-of-life patient-reported outcomes to demonstrate the effects of interventions on overall patient burden and suffering. 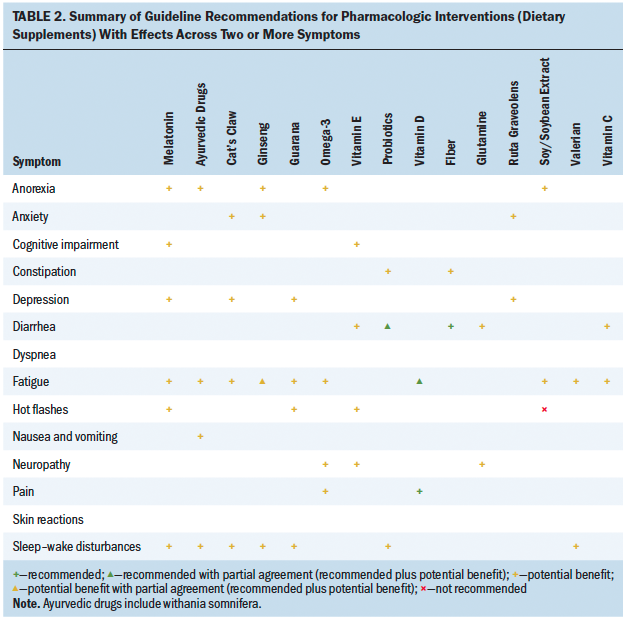
Revising and updating guidelines to address multi-symptom management: The authors recommend that guideline developers begin to consider addressing common symptom clusters by making recommendations for treatment strategies with efficacy across symptoms. Many organizations have already approached the symptom pair of nausea and vomiting in this way, and there is room for further development as common symptom clusters are identified and validated across studies (e.g., sickness behavior cluster of pain, fatigue, disturbed sleep, and lack of appetite; psychological cluster of feeling sad, worry, depression, and anxiety) (Ward Sullivan et al., 2018). The current authors intentionally limited the review to the guidelines of three U.S. organizations, but this could be expanded to achieve a broader, more global representation of strategies with potential for multi-symptom impact. 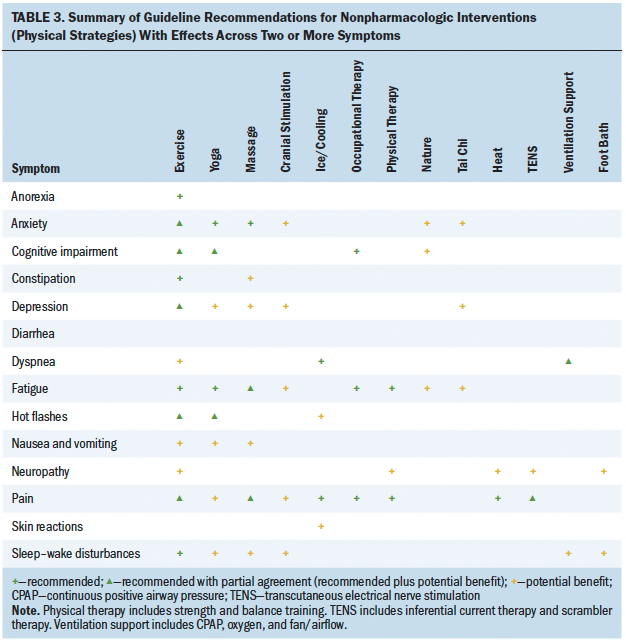
Development of multi-symptom management guidelines should use a thorough search to identify literature addressing pharmacologic and nonpharmacologic symptom management strategies. In the current review, the authors noted that ONS guidelines identified more nonpharmacologic approaches than did ASCO or NCCN guidelines. This is not surprising given that ASCO and NCCN guidelines had stronger representation of physicians, who more commonly have authority for prescribing pharmacologic therapies, and ONS guideline development was led by nurses, whose scope of practice directs the development and delivery of more physical, psychological, and behavioral symptom management strategies. That is, ONS guidelines may be more comprehensive of a variety of symptom management strategies because of the limited nature of pharmacologic prescribing among nurses. ONS guideline development also included searching the CINAHL database, where a greater number of studies of nonpharmacologic strategies are indexed as compared to medical databases. For example, a single search for the keyword yoga reveals nearly twice as many citations in CINAHL as compared to PubMed. 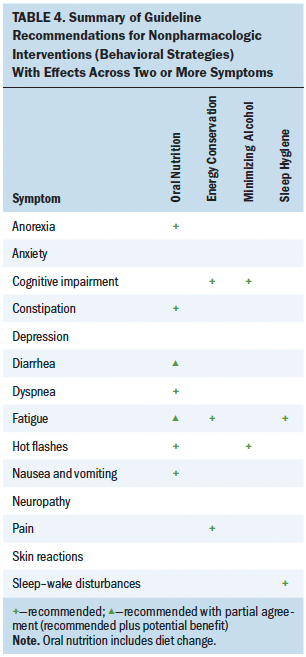
Patient representation on guideline development panels is also encouraged. Participation of all types of experts, including those who have experienced and attempted to manage multiple co-occurring symptoms, will be important as healthcare providers move toward more coordinated multi-symptom management plans. Patient representatives could provide professional panel members with insights about preferred treatment strategies, variables central to coordinating symptom management recommendations, and education and delivery modalities that foster efficient self-management of multiple symptoms. 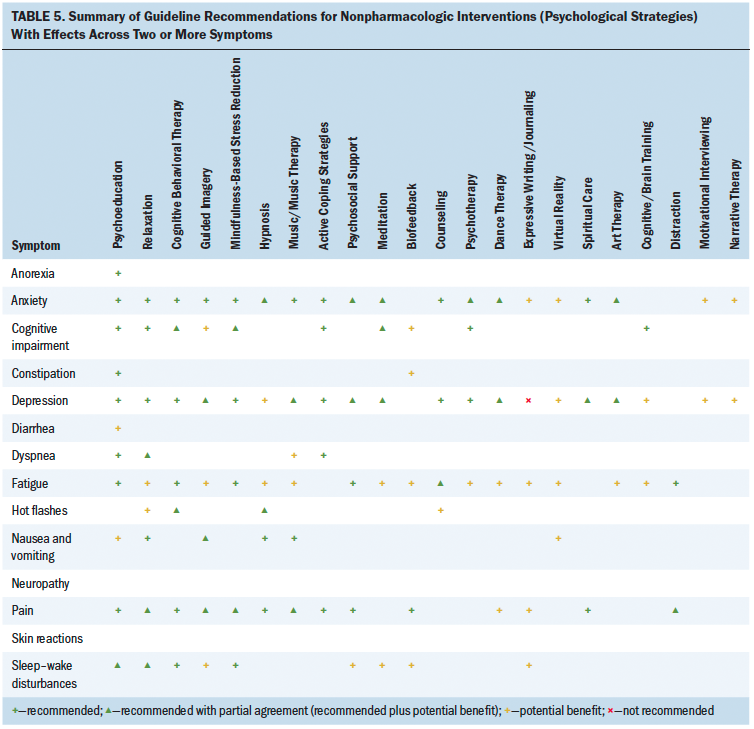
Developing technological resources to facilitate multi-symptom management: Findings from the current review suggest that it may be possible to more efficiently manage co-occurring symptoms. However, given the complex combinations of symptoms and unique clinical context (diagnosis, disease therapies), it is unlikely that a static guideline document can be used. Whether a single antidepressant can effectively treat two or more symptoms depends on the causal mechanism of the symptoms, their severity, and the specific antidepressant selected and its dosing, among other factors. Computer decision support will likely be necessary to facilitate rapid identification of symptom management recommendations across symptoms. At minimum, a searchable database is needed that allows clinicians to input co-occurring symptoms, disease, and treatment factors (or that collects them automatically from the electronic health record) to facilitate identification of coordinated treatment strategies. Decision support might be used to help providers in the clinical setting (Cooley et al., 2015) or built into self-management mobile applications that provide patients with education and training modules for recommended symptom management strategies. Patients could use these systems to track their symptoms and treatment effectiveness to support modifications in the symptom management plan. Findings from the current review suggest that coordinated management of multiple symptoms may be possible. With further testing of these strategies in the context of multiple symptoms and growing research in describing symptom phenotypes, healthcare providers may be able to intervene more efficiently and more precisely in managing co-occurring symptoms (Hickey et al, 2019; Miaskowski et al., 2017). 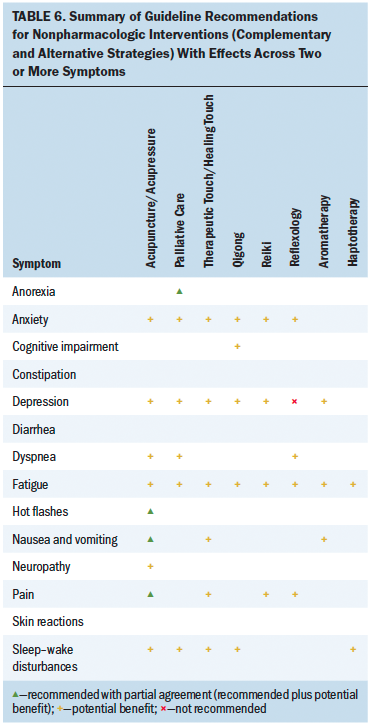
Implications for Practice
Findings of the current review can provide direction for the symptom management efforts of oncology nurses. When patients report symptoms, nurses can probe further to identify co-occurring symptoms through interview or using a structured multi-symptom assessment scale (Atkas et al., 2015). To systematically improve symptom assessment, nurses can advocate for clinical implementation of multi-symptom patient-reported outcome assessment completed in the home prior to appointments or in the clinical setting at the point of care (Mooney et al., 2018). In addition, oncology nurses can implement the symptom management guidelines endorsed by their employing institutions (Cooley & Siefert, 2016) and review recommendations for management strategies that overlap with two or more of the symptoms experienced by the patient. In selecting interventions, nurses without prescribing authority can emphasize nonpharmacologic self-management strategies and guide prescribing clinicians to consider medications with benefits across symptoms in an effort to reduce polypharmacy and potential drug–drug interactions (Schenker et al., 2019). Oncology nurses can also provide their expertise to evidence-based practice projects by developing system-level interventions to support nurses in identifying and implementing symptom management strategies with benefits across multiple symptoms. Oncology nurses can also participate in and facilitate interprofessional research that seeks to evaluate and build evidence for the effectiveness of multi-symptom management interventions. 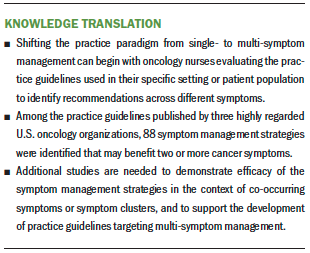
Conclusion
Patients with cancer, particularly those receiving treatment and those with advanced disease, face a high symptom burden that interferes with functional status, disrupts quality of life, and may contribute to mortality. Treating symptoms and delivering guideline-based symptom management is a critical component of high-quality cancer care. The current review advances knowledge and highlights the potential for efficient multi-symptom management through identification and implementation of strategies that are effective across two or more of the symptoms experienced. 
The authors gratefully acknowledge Loyda Braithwaite, MS, RN, AGPCNP, AOCNP®, ACHPN®, Kaitlyn Hopfensperger, BSN, RN, Kyung Soo Kim, PhD, RN, Sarah Loring, BSN, RN, and Sandra Ward, PhD, RN, FAAN, for their review and commentary on manuscript drafts.
About the Author(s)
Kristine L. Kwekkeboom, PhD, RN, FAAN, is a professor in the School of Nursing at the University of Wisconsin–Madison; Ann Wieben, MS, RN-BC, and Jennifer Stevens, MSN, RN, OCN®, are PhD students in the School of Nursing at the University of Wisconsin–Madison; Lauren Tostrud, BS, is a medical student at the Medical College of Wisconsin in Milwaukee; and Kathleen Montgomery, PhD, RN, PCNS-BC, CPHON®, is an assistant professor in the School of Nursing at the University of Wisconsin–Madison. No financial relationships to disclose. Kwekkeboom, Stevens, Tostrud, and Montgomery contributed to the conceptualization and design. Kwekkeboom, Wieben, Stevens, and Tostrud provided the analysis and completed the data collection. Kwekkeboom and Tostrud provided statistical support. All authors contributed to the manuscript preparation. Kwekkeboom can be reached at kwekkeboom@wisc.edu, with copy to ONFEditor@ons.org. (Submitted November 2019. Accepted April 29, 2020.)




