Depressive Symptoms and Associated Health-Related Variables in Older Adult Breast Cancer Survivors and Non-Cancer Controls
Objectives: To examine the prevalence of depressive symptoms and associated risk factors in older adult breast cancer survivors (BCS) and age-matched non-cancer controls.
Sample & Setting: Using the Surveillance, Epidemiology, and End Results–Medicare Health Outcome Survey linked dataset from 1998 to 2012, BCS and non-cancer controls aged 65 years or older were identified.
Methods & Variables: Depressive symptoms, comorbidities, functional limitations, socio-demographics, and health-related information were examined. Univariate and multivariable logistic regression and marginal models were performed.
Results: 5,421 BCS and 21,684 controls were identified. BCS and non-cancer controls had similar prevalence of depressive symptoms. Having two or more comorbidities and functional limitations were strongly associated with elevated risk of depressive symptoms in BCS and non-cancer controls.
Implications for Nursing: Having multiple comorbidities and multiple functional status are key factors associated with depressive symptoms in older adult BCS and non-cancer controls. Nurses are in an ideal position to screen older adult BCS and non-cancer controls at risk for depressive symptoms.
Jump to a section
Depressive symptoms are a common and serious problem experienced by many breast cancer survivors (BCS) that may lead to long-term quality-of-life issues (Jones et al., 2015). Numerous studies have evaluated the presence of depression among BCS, but prior studies are mainly focused on middle-aged women (aged 40–64 years). In a systematic review by Carreira et al. (2018) of 60 studies, only 5% of the entire combined study cohort were aged 70 years or older. Older BCS have been shown to be vulnerable to psychological problems, comorbid illnesses, and functional limitations, which could lead to depressive symptoms (Jones et al., 2015; Maass et al., 2015; Magnuson et al., 2019; Williams et al., 2016). Epidemiologic studies of older adults with cancer (aged 65 years or older) suggest that this population may be more vulnerable to depressive symptoms than older adults who do not have cancer (Avis & Deimling, 2008; Frazzetto et al., 2012; Mohile et al., 2011; Reyes-Gibby et al., 2006). However, few studies have focused on older BCS compared to older adults without a history of cancer.
Sociodemographic and health factors have been associated with depressive symptoms among older BCS (Caplette-Gingras & Savard, 2008; Mogal et al., 2017; Neuner et al., 2014; Patsou et al., 2018; Stommel et al., 2004; Williams et al., 2019). Specifically, the presence of comorbidities and functional limitations have been found to be significant risk factors for depressive symptoms in both the general geriatric population (Cahoon, 2012; Chang et al., 2016; Read et al., 2017; Vink et al., 2008) and older adults with cancer (Klapheke et al., 2020; Ladaninejad et al., 2019; Weiss Wiesel et al., 2015), including breast cancer (Azuero et al., 2014; Deckx et al., 2015; Perkins et al., 2007). A few studies also suggest that cancer and comorbidities can interact synergistically to affect physical and psychological outcomes in older cancer survivors (Bellizzi et al., 2008; Cavers et al., 2019; Deckx et al., 2012; Mandelblatt et al., 2014; Sarfati et al., 2016). In a qualitative systematic review study, the interaction between cancer and comorbidity emerged as a key theme (Cavers et al., 2019). Hewitt et al. (2003) found that cancer survivors with chronic disease had the greatest risk of depression, compared to non-cancer controls. Therefore, when investigating the effect of breast cancer on depressive symptoms, it is important to examine this relationship with respect to comorbidities.
Using a large population-based dataset, the current study aims to (a) examine the prevalence of depressive symptoms in older women with breast cancer and age-matched women without cancer and (b) identify factors, specifically comorbidities and functional limitations, associated with depressive symptoms in older BCS and non-cancer controls. The authors hypothesize that (a) older BCS will have a higher prevalence of depressive symptoms, (b) comorbidities and functional limitations will be significantly associated with depressive symptoms in both groups, and (c) interaction between breast cancer and comorbidities would increase the risk of presence of depressive symptoms.
Methods
Study data were retrieved from the Surveillance, Epidemiology, and End Results (SEER)–Medicare Health Outcomes Survey (MHOS) linked dataset. SEER is a population-based cancer registration program that routinely collects cancer cases in SEER regions (Eheman et al., 2012). The SEER data include information on demographics, date of cancer diagnosis, cancer-specific characteristics (e.g., tumor stage, size), surgical and radiation treatments, and survival status of individuals with cancer. The use of the SEER sample represents diverse racial/ethnic and geographic backgrounds from SEER regions (Ambs et al., 2008; Duggan et al., 2016). MHOS is a yearly survey that measures physical and mental health of Medicare beneficiaries enrolled in managed care plans. MHOS collects details on sociodemographic characteristics and physical and mental health, including self-rated health, impairments in activities of daily living (ADLs), and chronic medical conditions (Ambs et al., 2008). In this retrospective cross-sectional study, the authors used SEER-MHOS data collected from 1998 to 2012. Data were collected from 14 SEER regions. Additional details of the SEER-MHOS linked dataset have previously been published (Ambs et al., 2008; Kent et al., 2016). Following the application procedure (https://healthcaredelivery.cancer.gov/seer-mhos/obtain/overview.html), the current study’s authors received approval from the National Cancer Institute for the use of the SEER-MHOS dataset. The study was also approved by the institutional review board at the Wake Forest School of Medicine. This study is in accordance with the recommended Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (von Elm et al., 2007).
Study Population
Selection of breast cancer survivors: Women with histologically confirmed breast cancer were retrospectively identified from the SEER-MHOS linked dataset from 1998 to 2012. Inclusion criteria were community-dwelling women aged 65 years or older at first survey with complete information on depressive symptoms. Cancer-specific inclusion criteria for this study were a diagnosis of breast cancer verified by microscopy, malignant behavior, presence of breast cancer surgery, cancer diagnosis date available, and SEER and Medicare match date of birth and alive/death status. The authors excluded respondents who had a previous malignant disease or who had incomplete surgical records (e.g., unknown procedure, no record). For BCS who had completed two or more surveys, data from the first survey following cancer diagnosis were used.
Selection of non-cancer controls: The following inclusion criteria were applied: community-dwelling women aged 65 years or older at first survey, complete information for depressive symptoms, and no cancer history. The controls were matched for age at first survey (age difference of less than five years) and were randomly selected in a 4:1 ratio with BCS.
Measures
Depressive symptoms: The presence of depressive symptoms was defined as having both a score less than or equal to 42 on the Veterans Short Form (VR-12) mental health component score (MCS), and an affirmative response to one or more of the following diagnostic interview schedule questions: (a) “In the past year, have you had two weeks or more during which you felt sad, blue, or depressed, or when you lost interest or pleasure in things that you usually cared about or enjoyed?” (yes/no); (b) “In the past year, have you felt depressed or sad much of the time?” (yes/no); and (c) “Have you ever had two years or more in your life when you felt depressed or sad most days, even if you felt OK sometimes?” (yes/no) (Health Services Advisory Group, 2007; Quach et al., 2015; Rost et al., 1993). The VR-12 is a modified version of the SF-36®, which is a widely used health measure and has been validated for both individuals with chronic illnesses and the general population (Kazis et al., 2004; Kent et al., 2015; Selim et al., 2019). The VR-12 and the SF-36 are measures that can be used to compare groups with and without cancer using SEER-MHOS data (Kent et al., 2015). In the MHOS, the SF-36 was administered up to cohort 8 (1998–2005), and the VR-12 was used for the later cohorts (2006–2012). For cohorts 1 to 8 at baseline, the VR-12 equivalent scores were provided by the National Cancer Institute in the dataset. The MCS score of 42 or less shows a high-positive predictive value in classifying respondents with depression and was used as the cutoff value for the presence of depressive symptoms in the current study. Accordingly, individuals with an affirmative response and MCS scores of 42 or less were categorized as having depressive symptoms for the present analyses (McCall et al., 2002).
Comorbidities and functional limitations: Comorbidities were assessed using a self-reported chronic condition questionnaire and were categorized as none, one, and two or more of the following: hypertension, coronary artery disease, congestive heart failure, myocardial infarction or heart attack, other heart conditions, stroke, chronic lung disease (including emphysema, asthma, or chronic obstructive pulmonary disease), gastrointestinal diseases (including Crohn disease, ulcerative colitis, or inflammatory bowel disease), arthritis, sciatica, or diabetes. To measure functional limitations, presence of self-reported limitations (yes/no) in six facets of ADLs were assessed: bathing, dressing, eating, getting in or out of chairs, walking, and using the toilet. Functional limitations were categorized as none, one, and two or more.
Covariates: Risk factors for depressive symptoms among older adults and BCS, including age, race or ethnicity (dichotomized into White versus non-White), education (dichotomized into less than high school graduate versus high school graduate or greater), marital status (married versus not married), homeownership (yes/no), and current smoking status (yes/no), were included as covariates.
Statistical Analyses
Comparisons between BCS and non-cancer controls were first analyzed using the conditional logistic regression. The unadjusted and adjusted prevalence estimates of depressive symptoms between BCS and non-cancer controls were compared using the chi-square test and multivariable logistic regression with incorporating generalized estimating equations (GEEs), respectively. Age, race/ethnicity, education, marital status, homeownership, current smoking status, comorbidities (three categories), and functional limitations (three categories) were adjusted in the model. To examine associated risk factors for presence of depressive symptoms, the authors performed univariate and multivariable logistic regression analyses that estimate the odds ratios (ORs) and 95% confidence intervals (CIs) for BCS. Because non-cancer controls matched on the same case may not be independent to each other, the logistic regression with incorporating GEEs were used for analysis. Univariate variables with p < 0.05 were included into the multivariable logistic regression analyses (conventional logistic regression for BCS and GEE models for non-cancer controls). The authors also tested for potential interactions between breast cancer status and each of the significant risk factors using logistic regressions incorporating GEEs. For all analyses, p < 0.05 was considered statistically significant. All statistical analyses were performed using SAS®, version 9.4. 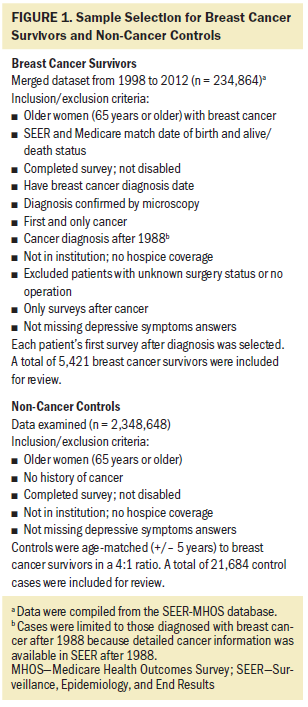
Results
Sample Characteristics
The study sample consisted of 5,421 BCS and 21,684 age-matched non-cancer controls. Figure 1 describes the study sample selection. Of the 234,864 cancer cases, the authors identified 5,421 breast cancer survivors who met the study inclusion criteria (e.g., breast cancer as the first and only cancer, diagnosis confirmed by microscopy, SEER and Medicare match date of birth, and alive/death status). The authors also selected older women without any cancer and initially identified 2,348,648 individuals who met the inclusion criteria for controls from the SEER-MHOS dataset of 1998–2012. After the matching procedure, 21,684 controls were available for the analyses. Table 1 summarizes the sociodemographic and health characteristics stratified by case-control status. The average age of the overall sample was 77.3 years (SD = 6.8 years). Mean time to survey was 7.1 years (SD = 5.1 years). The majority were White (78%), had education beyond high school (69%), and more than half were not married (61%). BCS were significantly more likely than controls to have an annual income of $30,000 or greater (p < 0.001) and be a homeowner (p < 0.001). Relative to BCS, non-cancer controls were more likely to be White (p < 0.001), not married (p < 0.001), a current smoker (p < 0.001), have less than a high school diploma (p < 0.001), no comorbidities (p < 0.001), and no functional limitations (p < 0.001). 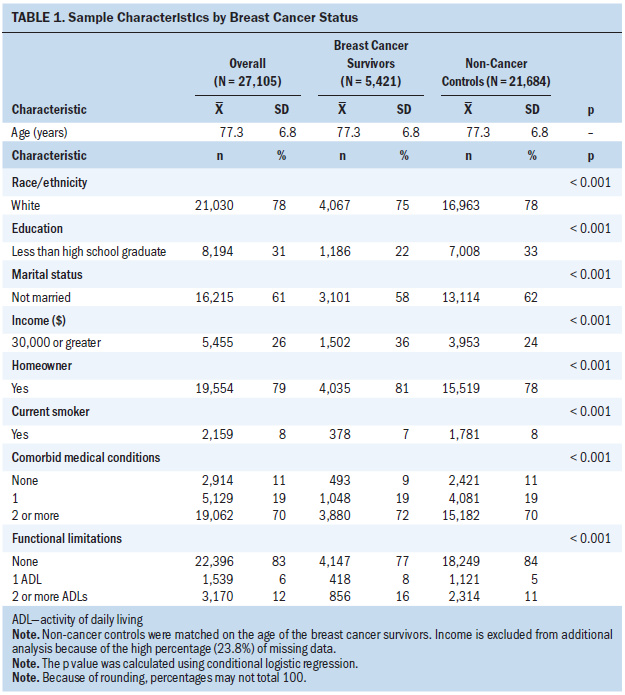
Prevalence of Depressive Symptoms
BCS had an unadjusted prevalence rate of 15.8% for depressive symptoms, compared to a rate of 16.1% in non-cancer controls (p = 0.57). Little difference was noted between cases and controls after adjusting for significant differences between the groups. Adjusted rate was 15.3% for BCS and 15.5% for non-cancer controls (p = 0.98).
Risk Factors for Presence of Depressive Symptoms
Table 2 presents risk factors associated with depressive symptoms for BCS and non-cancer controls based on univariate logistic regression analysis. Almost all variables were significantly related to increased risk for depressive symptoms for both cases and controls. Notably, in both BCS and controls, the presence of multiple comorbidities was strongly associated with depressive symptoms (OR = 5.13, 95% CI [3.32, 7.93] and OR = 3.37, 95% CI [2.85, 3.97], respectively). In addition, having multiple functional limitations was associated with three times greater likelihood of depressive symptoms in BCS (OR = 3.34, 95% CI [2.85, 3.96]) and controls (OR = 3.52, 95% CI [3.2, 3.87]). 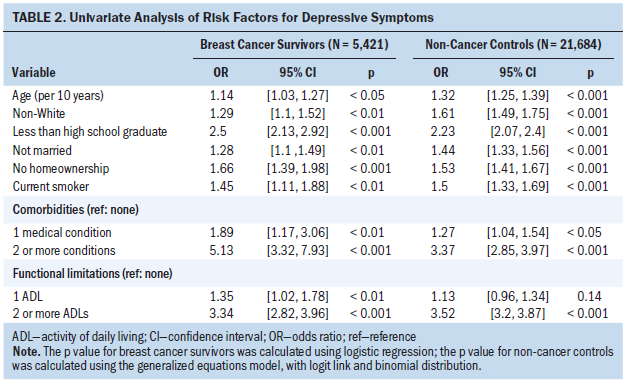
Lower education level, no homeownership, current smoking, any comorbid medical conditions, and two or more functional limitations were significant risk factors for depressive symptoms in BCS using multivariable analyses stratified by cancer status (all p < 0.05). Multiple comorbidities, two or more functional limitations, socioeconomic factors (older age, non-White ethnicity, high school or lower education, not married, no homeownership), and current smoking status were associated with depressive symptoms in non-cancer controls using multivariable analyses (see Table 3). In both BCS and controls, the existence of multiple comorbidities was the strongest factor associated with depressive symptoms (OR = 4.36, 95% CI [2.71, 6.99] and OR = 2.78, 95% CI [2.32, 3.34], respectively), followed by multiple functional limitations (OR = 2.78, 95% CI [2.32, 3.34] and OR = 2.63, 95% CI [2.35, 2.95], respectively). Evaluation of interactions between each study variable and breast cancer on depressive symptoms demonstrate that the only significant interaction was with subject age (interaction p = 0.01). This indicates that the effect of breast cancer on depressive symptoms is different by age group. 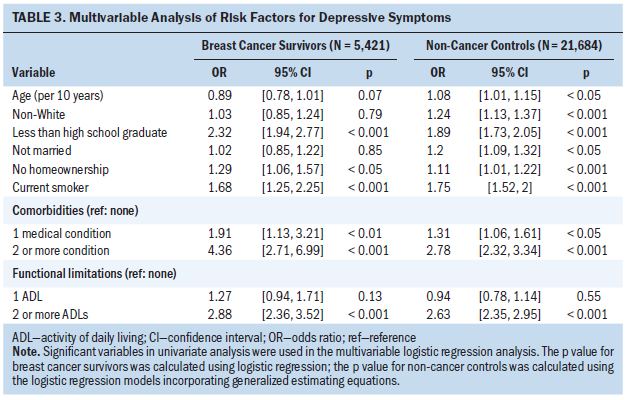
The results indicate that older BCS and women without cancer had a similar prevalence of depressive symptoms. The presence of two or more comorbidities and two or more functional limitations were found to be significantly associated with depressive symptoms in older BCS and the non-cancer group.
Discussion
In the current study, the authors examined the prevalence of depressive symptoms and associated risk factors in older BCS and age-matched non-cancer controls using a large population-based dataset. Approximately 16% of older BCS and non-cancer controls reported depressive symptoms. These prevalence rates were comparable to the previously reported rates (8%–16%) for depressive symptoms in community-dwelling older adults (Haigh et al., 2018; Meeks et al., 2011; Thapa et al., 2020) and BCS (10%–25%) (Fann et al., 2008; Krebber et al., 2014; Zainal et al., 2013). Although the authors hypothesized that depressive symptoms would be more prevalent among BCS than non-cancer controls, prevalence rates did not differ between the two groups in either unadjusted or adjusted analyses. Even after adjusting for significant factors, including comorbidities and function limitations, history of breast cancer was not associated with an increased prevalence of depressive symptoms.
Maass et al. (2015), in a systematic review of long-term depressive symptoms in BCS (one year or more after breast cancer) found inconsistent evidence regarding the depressive symptoms prevalence; a higher prevalence was found in BCS than in women without cancer in four studies, whereas no difference was found in the other four studies. A plausible explanation for no difference in prevalence in the current study may be because older adults are generally more psychologically resilient to stress, and their resilience could reduce depressive symptoms by alleviating breast cancer–related stresses and challenges (Campbell-Enns & Woodgate, 2017; Fradelos et al., 2017; Gooding et al., 2012). Another explanation is that because the median time from diagnosis to survey is approximately seven years, there may be no difference in prevalence between older BCS and controls due to healthy survival effects. This may also be because depressive symptoms may wane over time. A pooled analysis study of 51,381 long-term cancer survivors (mean time since diagnosis of 7.3 years) and 217,630 controls found no group difference in depressive symptoms (Mitchell et al., 2013). A meta-analysis study revealed that cancer survivors experienced twice as high depression prevalence than healthy controls, but the increased risk only lasts approximately two years (Mitchell et al., 2013). In other studies, BCS had significantly worse health-related quality-of-life outcomes during the diagnostic and treatment phases in comparison to non-cancer controls, but BCS improved substantially over time, resulting in no difference between the two groups after a few years (1–8 years) (Avis et al., 2020; Burgess et al., 2005; Dorval et al., 1998; Rottmann et al., 2016; Stover et al., 2014; Zainal et al., 2013).
The current study demonstrates that comorbidities and multiple functional limitations (impairments in ADLs) are significant risk factors associated with depressive symptoms in both older BCS and non-cancer controls. These findings are consistent with a growing body of geriatric research that finds a strong relationship between comorbid medical conditions and depressive symptoms in older adults (Chang et al., 2016; Vink et al., 2008) and BCS (Azuero et al., 2014; Suppli et al., 2014; Syrowatka et al., 2017). The significant association between functional limitations and depressive symptoms is also consistent with previous reports in older population (Chang et al., 2016; Conde-Sala et al., 2019; Thapa et al., 2020; Yang et al., 2015) and BCS (Chen et al., 2009; Deckx et al., 2015; Perkins et al., 2007; Syrowatka et al., 2017). This association may be related to loss of independence and social inactivity resulting from functional limitations. Depressive symptoms in older women are a key issue for physical and psychological well-being and can be identified and intervened by nurses. The authors’ finding implies that older women with multiple comorbidities and multiple functional limitations should be closely observed by geriatric and oncology nurses.
This study is strengthened by its population-based sample and its focus on an understudied comparative examination of depressive symptoms between older populations of BCS and non-cancer controls. The results of most previous comparative studies were relatively limited because they used small sample sizes with minimal representation of older BCS. The primary strength of this study is that the use of SEER-MHOS data produces reliable estimates by using a sufficiently large sample size.
The study has several limitations. First, depressive symptoms were assessed by a combination of self-reported three-item question and MCS score (42 or less), which is not a measure of clinical depression. Second, this study did not stratify by or control for time from diagnosis to survey. Some early studies suggested that differences exist in health-related outcomes between short- and long-term survivors (more than five years after diagnosis). Therefore, future studies should account for the time after diagnosis and the time after active treatment has ended. Third, this study used data from 1998 to 2012 because of the limited accessibility to a more recent dataset. However, the prevalence rates appear to be consistent with more recent studies of depression prevalence rates in BCS and older adults without a history of cancer (Haigh et al., 2018; Zainal et al., 2013). Fourth, the data lacks information on preexistence of depressive symptoms; therefore, the authors cannot determine whether the presence of depressive symptoms was preexistent or induced by breast cancer. In addition, the lack of detailed cancer-related clinical information (e.g., recurrence) may have limited the interpretation of results. Lastly, SEER-MHOS data only include older Medicare beneficiaries who are enrolled in the Medicare Advantage plan, and results may not be generalizable to beneficiaries with fee-for-service coverage.
Implications for Nursing
Late-in-life depressive symptoms affect overall health and health-related quality of life among older adult populations. Development of a more comprehensive understanding of older women at risk for depressive symptoms may be important in improving health-related quality of life. The current results suggest that multiple comorbidities and functional limitations may be key factors associated with depressive symptoms. Nursing professionals are ideally suited to screen for these factors and address these issues.
Older adults with cancer may be reluctant to disclose their depressive symptoms to healthcare providers (Noorani & Montagnini, 2007). Therefore, when providing routine care, nurses can be involved in screening and early identification of high-risk older women. In addition, older BCS often experience long-lasting functional changes and chronic health conditions throughout their survivorship. BCS have higher risks of developing new chronic comorbidities and having more limitations than women without cancer (Chavan et al., 2017; Ng et al., 2019). Oncology nurses and nurse navigators can play important roles in identifying and referring older BCS at risk for depressive symptoms, reflecting guidelines from the American Society of Clinical Oncology (Andersen et al., 2014). In addition, nurses have significant contact with patients and can play a core role in promoting active collaboration between primary care teams and mental health specialists through facilitating interprofessional communication and coordinating integrative care (Duarte et al., 2015; Ekers et al., 2013). The current study also has research implication for future studies. Although the authors identified that multiple comorbidities and functional limitations may be associated with risk of depressive symptoms, future studies are encouraged to explore how symptom clusters, such as specific comorbidities and functional limitations, may play a role in risk for depressive symptoms (Roiland & Heidrich, 2011). Obtaining this information may be helpful for nursing professionals to triage those who may be at greater risk for severity of depressive symptoms. In addition, although approximately 22% of the current study sample consisted of ethnic minorities, future studies are needed to replicate and extend the present findings in a more ethnically diverse sample. 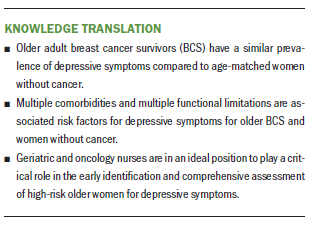
Conclusion
Approximately 16% of older BCS met criteria for depressive symptoms, consistent with rates of older non-cancer controls. Considering these very similar rates, it is important to note that depressive symptoms are substantial public health issues older women overall. Multiple comorbidities and functional limitations were significant risk factors associated with the presence of depressive symptoms, regardless of breast cancer status. Future studies are encouraged to identify specific comorbidities and functional limitations that may be significantly related to depressive symptoms in older BCS and women without cancer.
About the Author(s)
Min-So Paek, PhD, is an associate professor in the Department of Social Welfare at Konkuk University in South Korea; Shan S. Wong, PhD, is a clinical psychologist at the Hampton VA Medical Center in Virginia; Fang-Chi Hsu, PhD, is a professor and Nancy E. Avis, PhD, is a professor, both in the Division of Public Health Sciences at the Wake Forest School of Medicine in Winston-Salem, NC; Nora F. Fino, MS, is a biostatistician II in the Department of Internal Medicine at the University of Utah in Salt Lake City; and Clancy J. Clark, MD, is an associate professor of surgery at Wake Forest Baptist Health in Winston-Salem. Paek, Wong, and Avis were supported by a National Institutes of Health grant (R25CA122061) (principal investigator: Avis). All authors contributed to the conceptualization and design of the study, interpretation of the data, and drafting of the manuscript. Clark had access to all data in this study. Hsu and Fino provided the analysis. Paek can be reached at mpaek@kku.ac.kr, with copy to ONFEditor@ons.org. (Submitted August 2020. Accepted January 21, 2021.)




