SMART Oncology Nursing: Literacy, Goals, Coaching, and Empowerment
Problem Statement: This study assesses the effect of a nurse-designed SMART educational intervention on goal attainment, patient empowerment, and satisfaction.
Design: A mixed-methods study design was used.
Data Sources: 68 adults with cancer were recruited from an oncology research center and randomized to the immediate or waitlist control group. Empowerment was measured using the Patient Empowerment Scale, and health literacy was measured using the Cancer Health Literacy Test.
Analysis: Measures were completed by the immediate group at enrollment and by the waitlist control group after an eight-week waiting period to establish an updated baseline. Participants received four learning modules on goal setting and coaching to facilitate learning and activation of knowledge. Visit data were collected by nurses based on participants’ written and oral responses.
Findings: Goal attainment ranged from 67% to 100%. Patient empowerment scores were high at baseline and throughout. No significant differences were noted among the groups on goal attainment, empowerment, or satisfaction.
Implications for Nursing: RNs can deliver a SMART educational intervention using a universal health literacy approach to support adults with cancer in creating symptom management strategies and attaining self-care goals.
Jump to a section
Many adults with cancer have difficulty accessing, understanding, and applying health information. Patient education is often lacking a comprehensive approach to sharing health information in a manner that is sensitive to all levels of health literacy. Collaboration between healthcare clinicians and patients to apply health information and attain meaningful goals is often incomplete. Wittenberg et al. (2018) emphasized the importance of assessing patient understanding and adapting communication according to health literacy needs to ensure high-quality care. When health literacy needs are unmet, patients report difficulty with decision-making (Cohen et al., 2013).
According to the National Academies of Sciences, Engineering, and Medicine (2015), “For more than two decades, scientists and practitioners alike have acknowledged health literacy as a major determinant of individuals’ health status and disease prevention behaviors” (p. 5). The Centers for Disease Control and Prevention (2021) reported that an estimated 9 of 10 adults have difficulty understanding and using health information, which may be further limited by stress and anxiety. Decreased health literacy has been associated with nonadherence, medication errors, and poor disease self-management (Christensen, 2016). Evidence demonstrates that effective health literacy interventions can improve outcomes for patients (Berkman et al., 2011). An educational intervention was developed using the universal approach to health literacy recommended by the Agency for Healthcare Research and Quality (AHRQ, 2015). This approach assumes that all people have difficulty understanding health-related information, as well as creates an environment conducive to learning and improves self-management by simplifying information and confirming understanding to reduce miscommunication (AHRQ, 2015). Cohen et al. (2013) found that having adequate time for the nurse to assess understanding and identify additional needs is essential.
Research demonstrates that nurses tend to overestimate patient health literacy, which can lead to misunderstanding and inferior outcomes (Dickens et al., 2013). It is critical for nurses to avoid assuming an individual’s health literacy level based on their age or education level (Parnell, 2015). Universal literacy precautions and teach-back methods are important strategies to avoid negative outcomes associated with low health literacy. Oncology nurses are uniquely qualified to use evidence-based oral and written communication strategies to promote health literacy and empower their patients (Ballard & Hill, 2016).
Zimmerman (1995) described the importance of empowerment as when “people create or are given opportunities to . . . influence the decisions that affect their lives” (p. 583). According to a systematic review by Eskildsen et al. (2017), empowerment leads to improved health, lower health costs, and greater patient satisfaction. Patients become more active participants in their care and are empowered by improving coping, self-efficacy, and decision-making skills (Bulsara et al., 2006). If simple interventions are used to encourage patient participation in decision-making, patients are often more engaged and more informed (Koh et al., 2013). The National Academies of Sciences, Engineering, and Medicine (2020) noted core elements needed to support patients in the oncology setting, including “increasing confidence to manage symptoms and illness, supporting self-monitoring, facilitating knowledge and uptake of health behaviors, and supporting the development of skills for communicating with a team” (p. 37).
Using SMART (specific, measurable, achievable, realistic, timely) goals is important when providing education (Lawlor & Hornyak, 2012). SMART goals are created by the patient and require putting knowledge into action. The creation of a SMART goal allows a larger goal, such as wellness, to be segmented into smaller, easily attainable goals (Reddy, 2019). The use of a goal-setting, action-planning approach improves self-efficacy, assists with behavior change, and improves health outcomes (Lenzen et al., 2017). Strategies focused on improving health literacy also enhance self-management through assessment, goal setting, action planning, and problem solving (Koh et al., 2013).
Problem Statement
Cancer treatment is complex and creates unique needs for educational and psychosocial support. Delivering self-care and symptom management education using a universal approach to health literacy can empower patients to understand, apply, and activate information to make informed health decisions. It is imperative that the healthcare team is confident that patients understand and can apply information to make decisions and actively participate in their care. A SMART educational intervention consisting of coaching and goal setting can put knowledge into action, and a universal approach to health literacy can influence goal attainment, empowerment, and patient satisfaction. The aim of this study was to assess the feasibility and acceptability of a structured educational intervention using SMART methodology to improve patient outcomes.
Methods
A mixed-methods feasibility study of a SMART educational intervention was conducted with adults with cancer receiving treatment at HonorHealth Research and Innovation Institute in Scottsdale, Arizona. The SMART intervention is an evidence-based educational intervention delivered by oncology nurses.
A convenience sample of patients undergoing cancer treatment at the cancer research center was recruited. Eligibility criteria included being aged 18 years or older and having received a cancer diagnosis more than three months prior to study enrollment. Because the educational materials were only available in English, patients who did not read or speak English were excluded. No exclusions were made based on gender, race, or ethnicity.
Recruitment Procedures
The study was conducted at a nonprofit oncology research clinic providing ambulatory oncology research and treatment in a large integrated healthcare system. RNs in the clinic were asked to administer the SMART intervention based on their personal interest and time availability. All study personnel were trained on the intervention protocol. Prior to study initiation, nurses who volunteered to deliver the intervention received health literacy education and engaged in role-play and simulation to facilitate consistent content delivery. Potentially eligible patients were identified through a chart review of upcoming appointments. Patients were approached by an oncology nurse during their scheduled clinic visits and provided with the study details and informed consent form to review. If the patient was interested, a time was scheduled to review and sign the informed consent form.
Intervention
Participants were block-randomized by cancer type (breast, ovarian, pancreatic, and other) into either the immediate intervention or waitlist control (WLC) intervention group in a 1:1 format to control for disease trajectory variation. Participants randomized to the immediate group began the educational intervention after informed consent. The WLC group received standard medical and nursing care for eight weeks prior to beginning the educational intervention procedures while hospitalization and emergency department usage data were collected. Figure 1 illustrates participant enrollment, randomization, and progression through the study. 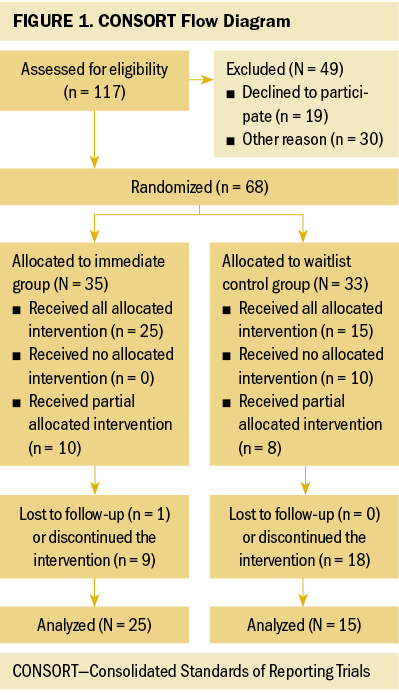
Education topics included (a) individualized medication review; (b) nutrition related to diarrhea, constipation, and nausea and vomiting; (c) anxiety and coping; and (d) sleep and fatigue. Topics were selected through patient input and a collaborative needs assessment led by oncology nurses. The education content of each module included didactic instruction, written information, and supplementary video content based on research evidence and current practice. Tools were revised based on feedback from health literacy experts before study initiation.
Each education module included two or three associated learning objectives and a core script of related information. Each script included definitions of topic components, explanations of how the topic or symptoms may affect the participant, symptom management strategies, and recommendations for how to communicate health needs. Education was personalized through discussion of past and current experiences, symptoms, personal preferences, and participant questions. Participants were asked to identify at least one meaningful goal when new information was presented surrounding each topic. The nurse provided guidance, if needed. The goal was written using the SMART format, with the intention of improving symptom management and/or quality of life.
To identify steps toward goal achievement, an action plan was created. Possible obstacles were identified and discussed. Participants were asked to rate their confidence in being able to successfully complete the goal on a scale ranging from 0 (not sure) to 10 (very sure). If their confidence was low, then the goal and/or action plan was revised. If their confidence was high, steps toward achieving the goal were initiated. Goals were reviewed at each visit, and progress was determined to be “met,” “in progress,” or “not met.”
Intervention follow-up visits were conducted via telephone or in person and completed at least one week after each educational intervention visit. Follow-up included determining the participant’s success in meeting their goals by asking review questions. All prior action plans were reviewed, and goal attainment was evaluated. Real-time reeducation was provided if necessary. Emergency department visits and hospitalization services used were also documented at each follow-up visit.
Throughout the intervention, nurses allocated time to establish relationships, provide education, and motivate participants to make changes and meet goals. Teach-back communication methods were included to confirm that participants understood the information provided by repeating it back in their own words. This conversation included wording to allow for open communication (e.g., “What questions do you have for me?” versus “Do you have any questions?”).
Data Sources
Data collection began at time of consent and was completed at the four-week follow-up visit. The length of time for each participant varied based on their randomization group, clinic schedule, and time availability. Screening data were collected by a protocol-trained nurse based on study eligibility criteria.
Immediately following consent, the nurse collected baseline demographic and clinical data from the medical record and participant written responses. Data included race, ethnicity, education level, cancer diagnosis, hospital admissions, and emergency department use within the past three months.
The Cancer Health Literacy Test (CHLT-30) was used to evaluate cancer health literacy. Items evaluated knowledge, skills, and ability for synthesis of knowledge. Internal consistency has been reported (Cronbach’s alpha = 0.88), with test–retest reliability at two weeks (Cronbach’s alpha = 0.9) and six months (Cronbach’s alpha = 0.92). The number of correct answers is summed, yielding a maximum of 30 points. Higher total scores indicate a higher level of health literacy (Dumenci et al., 2014).
The 15-item Patient Empowerment Scale (PES) measures empowerment among adults with cancer and their ability to adapt to the disease and engage proactively in treatment. Items are ranked from 1 (strongly disagree) to 5 (strongly agree). Scores are summed, with higher scores indicating greater feelings of empowerment. The maximum score for the PES is 60 points. The Pearson Separation Index was 0.79, indicating reliability (Bulsara & Styles, 2013). Validation was completed using literature, experts, patients, and family members (Bulsara et al., 2006).
Study Visits, Follow-Up, and End of Treatment
The immediate group completed the instruments at enrollment. The WLC group completed the instruments at enrollment and then again following the eight-week waiting period to establish an updated baseline. Study visit data were collected by the nurse based on participant written and oral responses.
Each participant was scheduled to receive four education sessions during the intervention according to a schedule approved by the participant. The sessions occurred a minimum of one week apart. Sessions were conducted during a clinic visit or by telephone. After each session, learning was assessed, reeducation occurred if needed, and the nurse guided the participant to develop a SMART goal and action plan. The AHRQ’s medication review form was used to document findings, develop an education plan, and complete the other visit intervention components.
The nurse collected follow-up data from participant written and oral responses in addition to clinical documentation from the medical record. During study follow-up sessions, which occurred at least one week after each education visit, the nurse documented progress toward goal attainment. If the goal was not met, additional education and coaching were provided, and reassessment occurred at the next scheduled visit or sooner. If goals were met, continued progress was monitored, with reassessments for knowledge retention occurring at subsequent visits. Health literacy and empowerment were reassessed using the CHLT-30 (Dumenci et al., 2014) and the PES (Bulsara & Styles, 2013) within one week of the final follow-up visit.
Four weeks after the final follow-up visit (end of treatment), health literacy and empowerment were assessed again using the CHLT-30 (Dumenci et al., 2014) and the PES (Bulsara & Styles, 2013). Reevaluation documented knowledge retention of all prior learning objectives, goal attainment results, necessity for reeducation, and hospital and emergency department use during the study. The Adapted Short Assessment of Patient Satisfaction survey was used to measure patient satisfaction with the intervention (Hawthorne et al., 2014). A five-point Likert-type scale was used to evaluate participants’ experience with the study. The questions addressed the effects of the educational intervention, choices in decisions affecting health care, care received in the clinic, and time spent with the nurses providing education (Hawthorne et al., 2014). Participant comments and suggestions regarding the study were documented. Details regarding progress toward goals and other study content that required situational explanations were also recorded.
Analysis
Summary statistics, including means (standard deviations) and percentages, as appropriate, are provided. A generalized estimating approach was used to evaluate changes in CHLT-30 and PES scores across visits. The interaction between group and visit was tested before combining groups to evaluate differential change over visits. Means, standard errors, and 95% confidence intervals are provided for these models. The Mann–Whitney U test was used to compare numbers of emergency department and hospital visits across groups postenrollment. Spearman’s correlation coefficients were calculated between participants’ highest education level and CHLT-30 and PES scores at first visit. IBM SPSS Statistics, version 27.0, was used for all analyses. An alpha of 0.05 was used as the criterion for statistical significance.
Findings
Sixty-eight adults with cancer participated in the study (see Table 1). Forty-six participants were female and had a college degree or higher. Most participants were White (n = 63). These statistics reflect the demographics of the community surrounding the clinic, which is more than 88% White (U.S. Census Bureau, 2019). Twenty-six participants had pancreatic cancer, 13 had ovarian/endometrial cancer, and 10 had breast cancer. During the study, the majority of participants were stage IV. The median time frame from diagnosis to study consent was 30 months, with a range of 3–52.9 months. 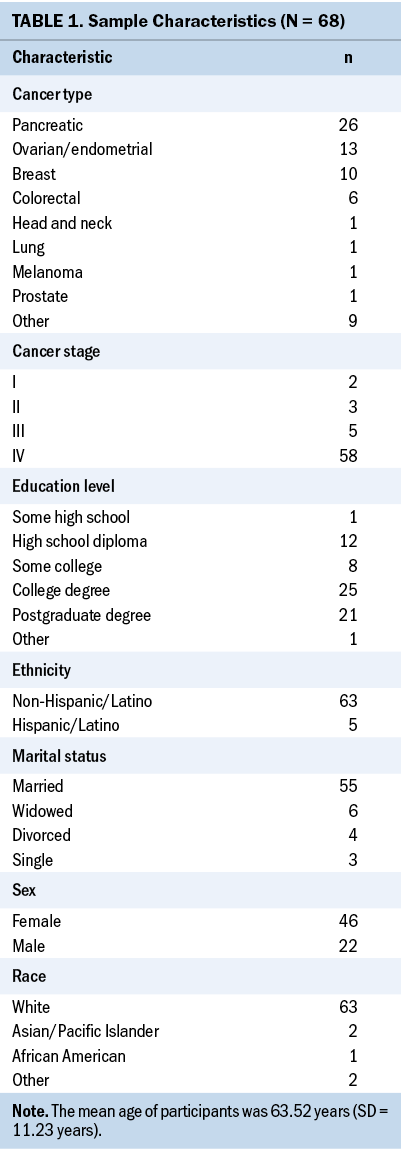
Some participants discontinued the study prior to completion for a variety of reasons, including a decline in health, death, or a change in cancer care center. Two participants felt that they did not need education, were doing well, and declined further participation. The WLC group had a lower completion rate than the immediate group. 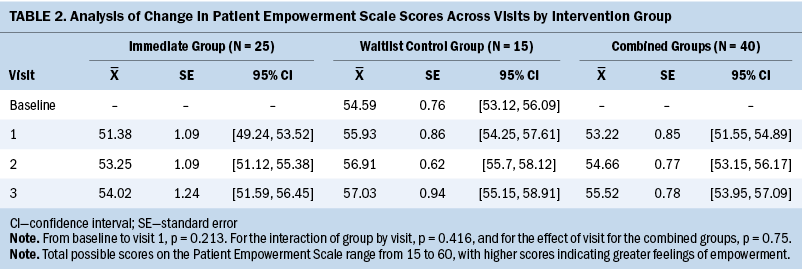
The analysis of changes in PES and CHLT-30 scores are presented in Tables 2 and 3, respectively. Twenty-five participants from the immediate group and 15 from the WLC group provided sufficient data to be included in these analyses. For both outcomes, scores for the WLC group increased marginally, although not significantly from baseline to first visit, indicating substantial stability. Participants in the WLC group received no intervention aside from routine care during this period. The interaction between group and visit was not significant for either outcome measure, so the groups were combined to test the effect of visit on empowerment (PES) and health literacy (CHLT-30). Scores on both measures increased slightly in the combined group, but the changes were not statistically significant (p = 0.075 for the PES and p = 0.598 for the CHLT-30). An ancillary analysis showed that, as expected, having attained a higher education level was associated with CHLT-30 scores during the first visit (rs = 0.5, p < 0.001) but not with PES scores (rs = –0.012, p = 0.933). 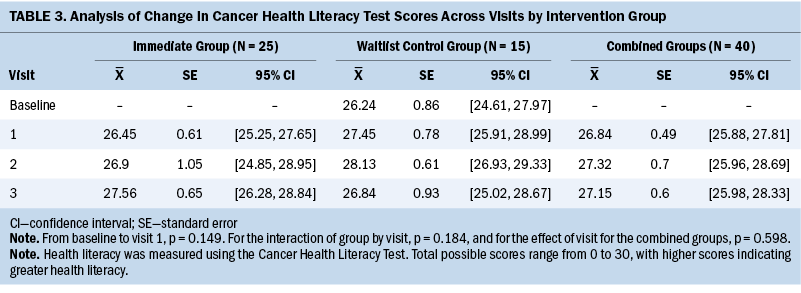
The two emergency department visits for the immediate group and three visits for the WLC group postenrollment did not differ significantly (p = 0.543). Similarly, the 11 hospitalizations for the immediate group and 13 for the WLC group did not differ (p = 0.137). These visits were deemed to be unavoidable by the study team. Goal attainment rates were high for participants. With the support of nurses, participants successfully completed the goals they found meaningful. At study completion, the number of participants who met their set goals was 33 for the medicine module, 28 for the nutrition module, 25 for the anxiety and coping module, and 22 for the sleep and fatigue module.
Participant satisfaction at study completion indicated that 26 participants were very satisfied with the effects of the educational intervention, and 7 indicated that they were satisfied. Regarding the choices that participants had in decisions affecting their care, 27 indicated being very satisfied, and 6 were satisfied. When asked how satisfied they were with the time they had with the nurse who provided the education, all participants responded that they were very satisfied. An open-ended question asked participants to describe how they will use what was learned during the study. A summary of the responses is included in Figure 2. 
While providing education and follow-up, nurses sat at eye-level with participants, and sessions did not have a time limit. These actions allowed for conversations and learning opportunities that would not have happened if the encounter had occurred under different circumstances. Experiences with implementation of the study protocol offered lessons to optimize the way education is provided. An example of this was finding a need for flexibility in education session timing. The following intrinsic and extraneous factors affected the ability to provide education during the scheduled time windows:
• Participants were sometimes overwhelmed with new information and were unable to process more information at the time.
• Participants sometimes needed additional support and found benefit in revisiting a prior module topic.
• Visits were delayed at times when nurses’ schedules prevented them from meeting a participant before their treatment ended on that specific day.
There was opportunity to provide education by telephone; however, participants voiced preference for receiving in-person education.
Sessions provided opportunities for education and guidance. For example, during the individualized medication review, participants were asked to bring all prescription and over-the-counter medications. They were asked to name each medication and explain the reason for taking it. In addition, they were asked to explain whether there were circumstances in which they would hold a specific medication. Discussions about the cost of each medication resulted in financial assistance referrals, if needed. Discussions related to missed doses of medications and unwanted side effects also occurred. During one meeting, it was discovered that a participant had naloxone hydrochloride because of prescribed high doses of narcotics. This patient resided with her son who was not aware of how to use the naloxone, so education was provided.
When receiving nutritional education, participants were provided reference sheets with suggested foods to consume or avoid for diarrhea, constipation, and nausea and vomiting. Participants were encouraged to have these foods available at home. The nurses involved in the study tailored nutritional education based on dietary restrictions, such as limited fiber, celiac disease, fluid restrictions, and diabetes. Participants reported hanging the reference sheets in their kitchen where they could quickly review them if any symptoms occurred. Nutritional education required more reeducation than the other topics.
The coping and anxiety education session provided information and resources to participants, as well as support, a listening ear, and a shoulder to cry on at times. Participants were introduced to coping strategies, such as meditation, deep breathing, and journaling. One participant created a goal to try journaling to cope with anxiety. He reported that during journaling, he wrote down his wishes and as a result, held a family meeting and discussed next steps if the cancer progressed and treatment was no longer effective. There was a sense of relief by the participant and his family. Goals of care discussions also resulted from education provided in these sessions. Another participant had considered requesting an antidepressant prescription prior to the coping and anxiety session because of her depressed mood. After the education session, she felt empowered to try alternative coping strategies and no longer wanted to begin taking an antidepressant. This participant also discovered the importance of focusing on her mental health and self-compassion. Another participant verbalized that mental health needs should be assessed and discussed regularly, asking, “How can we expect people to come here and go through treatment if they do not feel their life is worth living?” Many participants reported not knowing about available resources, including the chaplain and social worker, prior to the education session.
The sleep and fatigue education session provided participants with strategies to improve sleep and decrease fatigue. The modules reviewed strategies to improve overall sleep habits and patterns. Many participants created goals to increase their activity to combat fatigue. Often, the goal of increasing activity was viewed as a daunting task for participants, particularly for those who were experiencing symptoms of deconditioning. The nurse assessed each participant’s current activity level and limitations to develop an achievable first step toward the goal. The plan was customized based on the participant’s preferences for timing of exercise, timing of pain medicine dosing, exercises found enjoyable, and companions to accompany the participant in working toward their goals. Referrals were made to physical therapy, as appropriate.
Participants noted that “knowledge is power” and “this study filled in the gaps.” One participant reported that she learned how to “live with cancer and not just survive.” Participants discussed the importance of trust and building strong relationships with the nurses. Multiple participants reported that they felt the nurse providing the education truly cared about them. Participants also reported appreciating support in developing meaningful goals and achieving those goals. One participant stated, “I feel very lucky to be part of this study.” Another participant said, “I was able to set goals and when I got up every morning, this gave me something to strive for.” An additional comment included, “I had someone to help me achieve a better quality of life.”
Limitations
Some participants experienced a health decline, were no longer receiving treatment at the clinic, or died by the end of the waiting period for the WLC group. Of the 68 participants, 40 completed all study sessions.
The clinic population and study sample were also limited in diversity, which, in turn, limits the generalizability of the findings. The sample recruited was largely literate and empowered, which resulted in a ceiling effect and meant that improvement or differences could not be demonstrated because many participants had little room for improvement using the instruments chosen.
Implications for Practice
The nurses involved in the study developed an understanding of the importance of meeting the person where they were in their journey in terms of health literacy, education needs, and support. Because of the relationships that had been built, some participants asked to meet with specific nurses to discuss issues, resources, and support needed, even after completing the study. This was a reminder of the strong relationship that had been built and that participants remembered to ask for help when needed. Another key takeaway was the reminder to ask participants, “What questions do you have for me?” instead of “Do you have any questions?” because this wording opened the door for conversation, and participants viewed the nurse as having time and a genuine interest.
Although this study supports the feasibility of implementing the nurse-designed SMART educational intervention in a similar clinic-based setting, future research is needed to determine whether other delivery methods are also feasible and effective. Telehealth may provide an alternate delivery method, but many participants in the current study preferred to receive in-person education sessions. The acceptability of delivering the educational intervention using telehealth needs to be determined. There is also a need to determine whether this educational intervention is feasible and acceptable in a clinic where participant demographics are more diverse.
Future research is needed to examine potential correlations between nurse characteristics and a satisfactory educational intervention. To fully understand this intervention’s translation into practice, it would be beneficial to examine the effects of nurse education, training, satisfaction, and other attributes. In addition, caregivers voiced the desire to have this education and goal setting and attainment intervention provided to them, so future studies are needed to evaluate the feasibility of a nurse-driven, SMART educational intervention for caregivers. 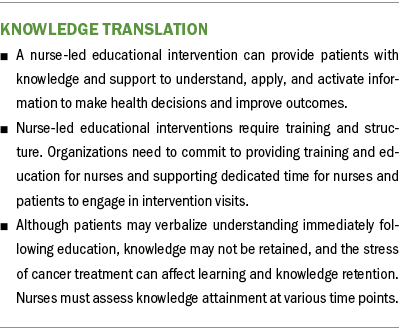
Conclusion
The relationship between patients and their nurses has the potential to be pivotal in health outcomes. Education provided using SMART goals, an engaging format, and an individualized process with a universal approach to health literacy creates a solid foundation for patients’ well-being. Once literacy is addressed, patients can begin to work on achieving their health-related goals.
The authors gratefully acknowledge Melodi Priddy, BSN, RN, Wendy Booher, BSN, RN, Monica Fulk, RN, OCN®, Margaux Steinbach, BSN, RN, OCN®, Somya Bhatnagar, BA, Saheba Bhatnagar, BS, and Evonda Copeland, MLIS, for their contributions to this project.
About the Author(s)
Amy Mirabella, PhD, RN, CHPN, and Amber Vrana, MSN-L, RN, OCN®, are oncology research nurses at HonorHealth Research and Innovation Institute in Scottsdale, AZ; R. Curtis Bay, PhD, is a professor of biostatistics in the Department of Interdisciplinary Health Sciences at A.T. Still University in Mesa, AZ; Alexandra Slater, BS, is a research administrative assistant at HonorHealth Research and Innovation Institute in Scottsdale; and Melanie A. Brewer, DNSc, RN, FNP-BC, NEA-BC, FAANP, is the director of research in the Center for Clinical Excellence and a nurse practitioner at HonorHealth Research and Innovation Institute in Scottsdale and a professor of clinical nursing in the Edson College of Nursing and Health Innovation at Arizona State University in Phoenix. This article was funded by a grant (# JPB-2019-056) from the DAISY Foundation. Mirabella, Vrana, Bay, and Brewer contributed to the conceptualization and design and provided the analysis. Mirabella, Vrana, Slater, and Brewer completed the data collection. Mirabella, Bay, Slater, and Brewer provided statistical support. All authors contributed to the manuscript preparation. Mirabella can be reached at amirabella@honorhealth.com, with copy to ONFEditor@ons.org. (Submitted April 2021. Accepted September 27, 2021.)

