An Ecologic Model for Identifying Coping Resources to Manage Psychological Distress Among Spanish-Speaking Latina Women Newly Diagnosed With Breast Cancer
Objectives: To examine associations of coping resources for psychological distress among newly diagnosed Spanish-speaking Latina women with breast cancer (LWBC).
Sample & Setting: Analyses used baseline data from a randomized controlled trial of a stress management intervention among 151 LWBC.
Methods & Variables: Dependent variables were health distress and anxiety. Coping resources at the intrapersonal, interpersonal, and organizational/community levels were included.
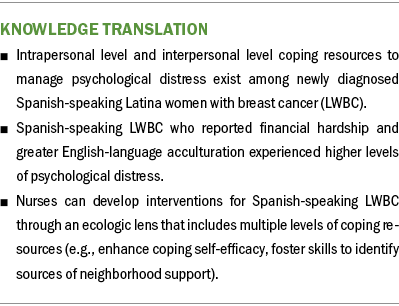
Results: At the intrapersonal level, self-efficacy for coping with breast cancer treatment was associated inversely with health distress and anxiety, and coping confidence with general problems was associated inversely with health distress. At the interpersonal level, having a sense of neighborhood cohesion was associated inversely with health distress. No organizational/community level resources were associated with health distress or anxiety.
Implications for Nursing: Interventions that enhance self-efficacy in coping and foster skills to identify sources of neighborhood support may decrease psychological distress for Spanish-speaking LWBC.
Jump to a section
Among Latina women, breast cancer is the most commonly diagnosed cancer type and is the leading cause of cancer-related death (American Cancer Society, 2021). Latina women are more likely to be diagnosed with later-stage and more aggressive breast cancer and are less likely to receive appropriate and timely treatment than White women, independent of age, socioeconomic status, and method of diagnosis (American Cancer Society, 2021).
Latina women with breast cancer (LWBC) in the United States are at higher risk for psychological distress than other racial/ethnic groups, reporting higher rates of anxiety and depression and worse health-related quality of life (HRQOL) (Samuel et al., 2020). These psychosocial health disparities among Latina cancer survivors may be attributable, in part, to the availability and use of coping resources to manage stressful events, such as a breast cancer diagnosis (Dean et al., 2018; Williams et al., 2016).
Coping is the process of attempting to manage the demands created by stressful events that are appraised as taxing or exceeding an individual’s resources (Lazarus & Folkman, 1984). Coping resources, such as a sense of mastery, self-esteem, and social support (Taylor & Stanton, 2007), affect coping processes. Coping resources can directly affect psychological and physical health during primary treatment and further along the cancer care continuum. Action-oriented or intrapsychic coping resources improve the ability to manage stressful events (Taylor & Stanton, 2007) and decrease psychological distress (Henselmans et al., 2010). The few studies that have examined coping resources among LWBC focus on English-speaking LWBC (Ream et al., 2021), small samples of primarily Colombian and Puerto Rican breast cancer survivors (Aguado Loi et al., 2013), or LWBC more than two years postdiagnosis (Ashing-Giwa et al., 2013; Nápoles et al., 2011). Despite these efforts, gaps exist in understanding of coping resources used among Spanish-speaking LWBC to mitigate psychological distress (Yoo et al., 2014).
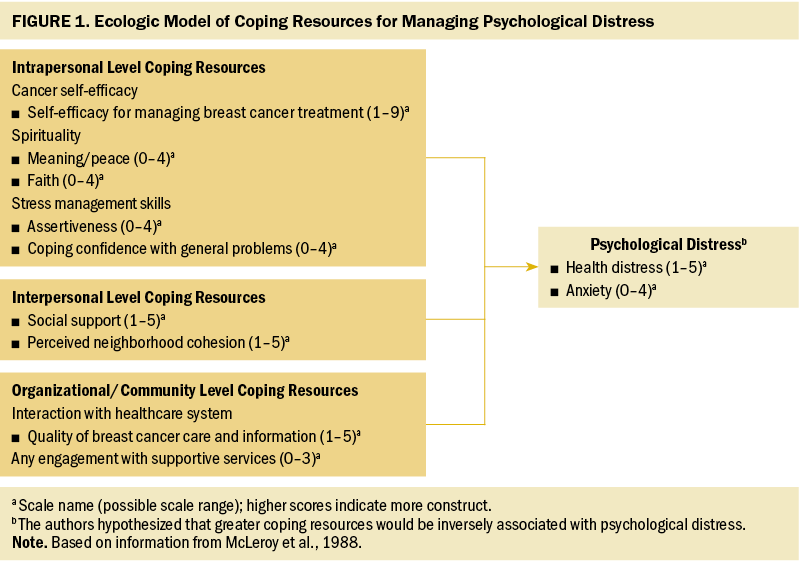
Latina women’s lived experiences and their responses to a breast cancer diagnosis affect how they will cope with a diagnosis and what coping resources they will call on during this stressful event. An ecologic perspective, which postulates that individual level behavior is influenced by multiple levels (McLeroy et al., 1988), can help to understand how coping resources at multiple levels affect psychological distress. According to the McLeroy ecologic model, these multiple levels comprise intrapersonal factors (characteristics of the individual, such as knowledge, attitudes, behavior, self-concept, and skills); interpersonal processes and primary groups (formal and informal social networks and support systems); institutional factors (social institutions with organizational characteristics and formal and informal rules); community factors (relationships among organizations and institutions, and informal networks within defined boundaries); and public policy (local, state, and national laws and policies) (McLeroy et al., 1988). With minor adaptations because of data limitations (not all levels were represented in available measures), the authors used this ecologic model because it views behavior as being affected and affecting the social environment and facilitates analysis of various levels and types of social influences and knowledge that can be used to develop appropriate interventions (McLeroy et al., 1988). Figure 1 presents an ecologic framework adapted from the McLeroy et al. (1988) model that depicts three levels of coping resources that affect psychological distress, including resources at the intrapersonal, interpersonal, and organizational/community levels. For this study, the authors combined organizational and community levels and did not include public policy.
In this study, intrapersonal level coping resources include cancer-specific self-efficacy, religiosity/spirituality, and stress management skills, which have been associated with positive adaptation to breast cancer. Among LWBC who completed treatment within two years, greater cancer-relevant self-efficacy was related to better overall HRQOL, less symptom burden, and less cancer-specific distress (Baik et al., 2020). Less is known about the role of cancer self-efficacy among Spanish-speaking LWBC. In a systematic review, Latino individuals with cancer reported higher levels of spiritual well-being and spirituality-based coping in studies examining racial/ethnic differences (Samuel et al., 2020); several of these studies found that higher levels of spirituality/religious coping were associated with better HRQOL (Samuel et al., 2020). Little is known about the specific individual stress management skills used among Spanish-speaking LWBC. Most research in this area is in the context of intervention strategies. Systematic reviews of intervention strategies among LWBC found that confidence-building activities in stress management improved confidence in self-care skills (Anderson & Armer, 2021; Samuel et al., 2020). Telephone-delivered interventions also demonstrated promise among LWBC and their caregivers in symptom reduction, global distress, self-efficacy for managing symptoms, and depression, depending on the intervention components (Badger et al., 2020).
According to the ecologic model, the interpersonal level refers to social networks and social support systems from family, friends, and neighbors (McLeroy et al., 1988). Cancer survivors’ perceived social support from family and peers has been positively associated with well-being in individuals with cancer (Samuel et al., 2020) and mitigated psychological distress among individuals with breast cancer (Friedman et al., 2006). Among LWBC, less emotional support from family and friends was associated with depression and poor physical and social functioning (Samuel et al., 2020). Family caregivers have been shown to play an important supportive role in the care of LWBC because of cultural norms of familismo, and they may experience elevated distress associated with their role (Segrin et al., 2021). Although Latino cancer survivors report family as a source of support more often than other racial/ethnic groups, they are less likely to pursue other sources of support (Samuel et al., 2020).
Perceived neighborhood cohesion is the perceived degree of connection among neighbors and people’s willingness to intervene for the common good (Berkman et al., 2014). Neighborhood cohesion affects individual mental health through two possible mediating mechanisms: perceived neighborhood disorder and social relationships (social support and neighborhood social ties) (Diez Roux, 2001; Kim, 2010). Neighborhood cohesion has been studied in the context of access to cancer screening (Hei et al., 2019), but less is known about its role as a coping resource among breast cancer survivors. A nationally representative survey of Latino individuals found that neighborhood cohesion was positively related to self-rated physical and mental health (Mulvaney-Day et al., 2007). A study examining neighborhood context and health outcomes among urban Black breast cancer survivors and English- and Spanish-speaking LWBC found that greater neighborhood stress was associated with poorer self-reported health (Wu et al., 2018).
The organizational and community levels, which were combined for this study, focus on the interaction between organizations and groups within a defined area (McLeroy et al., 1988). Organizational/community level coping resources can include engagement with supportive care services (e.g., patient navigators, cancer support groups) and cancer care providers. Abundant evidence shows that access to and use of supportive care services can reduce distress, improve quality of life, and enhance coping and social functioning (Roland et al., 2017). One study among LWBC found that a group with an enhanced patient navigation program had significantly improved quality of life compared to a control group (Ramirez et al., 2020). However, LWBC are less likely than their counterparts to receive supportive care for mental health issues and participate in support groups (Samuel et al., 2020), often being unaware of such support services (Nápoles-Springer et al., 2007).
Positive interactions with healthcare providers are associated with treatment adherence (Foglino et al., 2016) and better symptom control, patient–clinician communication, and HRQOL (Graupner et al., 2021). Because initial levels of distress predict later HRQOL, early interactions with providers can affect distress trajectories. Spanish-speaking LWBC have a harder time communicating with providers, receive less follow-up care, and receive less information than English-speaking underrepresented racial/ethnic groups (Rosales et al., 2014), possibly because of limited access to health care or structural barriers (e.g., distance to cancer centers) and limited availability of bilingual/bicultural providers and interpreters (Roy et al., 2021). Unmet supportive care from providers among LWBC persists, particularly among women with a more recent cancer diagnosis (Moreno et al., 2019).
The intersectionality of underrepresented racial/ethnic group, immigration, and low socioeconomic statuses can place Spanish-speaking LWBC at elevated risk for psychosocial morbidity. Gaps exist in the understanding of coping resources used among this group to mitigate psychological distress (Yoo et al., 2014). Guided by an ecologic model, the purpose of this article is to examine the extent to which coping resources at the intrapersonal, interpersonal, and organizational/community levels are associated with psychological distress (anxiety and health distress) among newly diagnosed Spanish-speaking LWBC. The authors hypothesized that greater coping resources would be inversely associated with levels of anxiety and distress.
Methods
This study is a cross-sectional secondary data analysis of baseline data from a six-month randomized controlled trial testing an eight-week, peer-delivered, cognitive behavioral stress management intervention, called Nuevo Amanecer (A New Dawn), for Spanish-speaking Latina women with nonmetastatic breast cancer (n = 151) who were recruited within the first year of diagnosis. Using community-based participatory research methods, women were recruited from clinical and community settings in five Northern California counties. A 60-minute baseline in-person survey that assessed coping resources and health perceptions was administered in Spanish by trained bilingual, bicultural community-based recruiters. Study procedures (Nápoles et al., 2014), the intervention (Nápoles et al., 2018), and study results (Nápoles et al., 2015) are described elsewhere. The study protocol was approved by the University of California, San Francisco Institutional Review Board, and written informed consent was obtained from all participants. Women received $30 for completing the survey.
Measures
For instruments unavailable in Spanish, translation was performed using forward and backward translation methods with team review and reconciliation of discrepancies, and cognitively pretested in Spanish with community residents meeting eligibility criteria (not included in the study). Psychometric properties of measures were examined in this sample.
Dependent measures: Two dependent variables assessed health distress and general anxiety. The health distress scale developed by the Stanford Patient Education Research Center (Lorig et al., 1996) is a modification of the Medical Outcomes Study scale. It measures the amount of time in the past month women felt discouraged or frustrated by health problems, fearful about their future health, or worried about their health. Scores range from 1 to 5, and higher scores indicate greater distress (internal consistency reliability = 0.87). Anxiety was measured with the Brief Symptom Inventory six-item anxiety scale, which assesses the extent to which women were bothered or distressed during the past seven days by symptoms of anxiety (Derogatis, 1993). Symptoms included feeling nervous or shaky, suddenly scared, fearful, tense or keyed up, or restless, and having panic spells. Scores range from 0 to 4, and higher scores indicate more anxiety (internal consistency reliability = 0.85).
Independent variables were intrapersonal, interpersonal, and organizational/community level coping resources. Intrapersonal level coping resources include self-efficacy for coping with breast cancer, spirituality, and ability to perform stress management techniques. Interpersonal level resources were social support and perceived neighborhood cohesion. Because the measure assessed women’s perceptions of the quality of their neighborhood, this is included as an interpersonal resource rather than a community level one. Organizational/community level coping resources were engagement with the healthcare system and supportive services.
Intrapersonal level measures: Self-efficacy for coping with cancer was measured with one scale from the Cancer Behavior Inventory–Brief, version 2.0 (Merluzzi et al., 2001), originally called the Coping With Side Effects. The authors relabeled the scale to Self-Efficacy for Managing Breast Cancer Treatment to be more precise (e.g., focuses on treatment more generally). Women rated their confidence that they could accomplish each behavior on a scale from 0 to 9, with a higher score indicating greater self-efficacy. The scoring was modified based on psychometric analyses in this sample, with written permission from scale developers. The Self-Efficacy for Managing Breast Cancer Treatment scale is a four-item scale assessing women’s confidence that they can manage breast cancer treatment (e.g., managing nausea and vomiting, coping with physical changes, remaining relaxed through treatment, waiting for appointments) (internal consistency reliability = 0.76).
For spirituality, the authors used two subscales of the Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being instrument for people with cancer, available in Spanish (Peterman et al., 2002). Respondents rate the extent to which each statement is true for them on a scale ranging from 0 to 4. Higher scores indicate greater levels of spirituality. The meaning/peace subscale assesses the extent to which respondents feel peaceful and have a sense of harmony, are able to find comfort within themselves, and have a reason to live. Based on psychometrics, the authors dropped two items that were negatively worded (my life lacks meaning/purpose, trouble feeling peace of mind). The internal consistency reliability was 0.81. The faith subscale is a four-item scale measuring the role of faith in illness (e.g., the extent to which illness has strengthened their faith and spiritual beliefs, the extent to which they find comfort and strength in their faith and spiritual beliefs) (internal consistency reliability = 0.9).
The authors used two measures of stress management skills (assertiveness and coping confidence) from the Measure of Current Status Part A. (Antoni et al., 2006). Women rated the extent to which they can do each technique when under stress using a five-point scale ranging from 0 (I cannot do this at all) to 4 (I can do this extremely well). Higher scores indicate more confidence. Assertiveness measures the extent to which women are able to ask for help or support and can clearly express their needs (internal consistency reliability = 0.7). Coping confidence measures their ability to reexamine their thoughts to gain a new perspective, decide how to cope with problems, generate emotionally balanced thoughts, and choose the best coping responses (internal consistency reliability = 0.89).
Interpersonal level measures: Social support was measured using the Medical Outcomes Study Social Support Survey short form (Moser et al., 2012). Women rated the extent to which various types of social support were available if needed during the past month (e.g., someone who understands their problems, someone to take them to the doctor, someone to help with chores, someone to love them and make them feel wanted). Scores range from 1 to 5, and higher scores indicate greater support (internal consistency reliability = 0.91).
The Neighborhood Cohesion scale assesses agreement with statements about the neighborhood in which they live (Kim et al., 2010). Based on psychometrics, two of five items were dropped (negatively worded items). The three-item scale included the following: people in this neighborhood can be trusted, people in this neighborhood are willing to help, and this is a close-knit neighborhood. Scores range from 0 to 4, and higher scores indicate greater cohesion (internal consistency reliability = 0.87).
Organizational/community level measures: Interactions with the healthcare system were assessed using a two-item scale the authors developed to assess perceived quality of breast cancer care and information received about their breast cancer. Women were asked to rate the care they received on a five-point scale as follows: 1 = poor, 2 = fair, 3 = good, 4 = very good, and 5 = excellent. Scores range from 1 to 5; higher scores indicate higher quality of care (internal consistency reliability = 0.86).
Engagement with supportive services was assessed by using a summary variable derived from three items that asked if they had interacted with a counselor or mental health professional, a cancer support group, and a patient navigator since being diagnosed with breast cancer (0 = no; 1 = yes, still using service; 2 = yes, but no longer using). Scores are the sum of “yes” responses (range = 0–3); higher scores indicate more engagement.
Covariates: Covariates included demographic and clinical characteristics. Demographic characteristics were self-reported age, education level, marital status, employment status, type of insurance, financial hardship, country of birth, years living in the United States, and the brief Marin language acculturation measure (Marin et al., 1987) on which higher scores indicate greater use of English (1 = Spanish only, 5 = English only). Clinical characteristics included self-reported history of depression and/or treatment and months since diagnosis (0 = 3 months or less, 1 = 3.1–6 months, or 2 = 6.1 months or more), type of breast cancer, stage, type of surgery, and adjuvant treatment, obtained through medical record review.
Statistical Analysis
Data from a total of 151 women enrolled in the parent study were used in this secondary analysis. The parent study was powered using an alpha level of 0.05 (two-sided) and power set at 0.8 for a sample size estimate of 170 participants with 80% retention at six months or target sample size of 136 participants. Using SAS, version 9.4, descriptive statistics, internal consistency reliability, and item-scale correlations of measures were performed. Simple linear regressions examined bivariate associations of independent and dependent variables. Because of the large number of independent variables, data analyses were conducted in a multiple-step approach. Only variables that were significantly associated with health distress or anxiety at p < 0.2 in bivariate analyses or supported by the literature were included. Hierarchical regression analysis was conducted to determine the association of the variables of interest with health distress and anxiety separately, as follows: model 1, covariates only; model 2, intrapersonal level coping resources were added; model 3, interpersonal level coping resources were added; and model 4, organizational/community level coping resources were added. Model fit was evaluated using a two-tailed test with a p < 0.05 level of significance.
Results
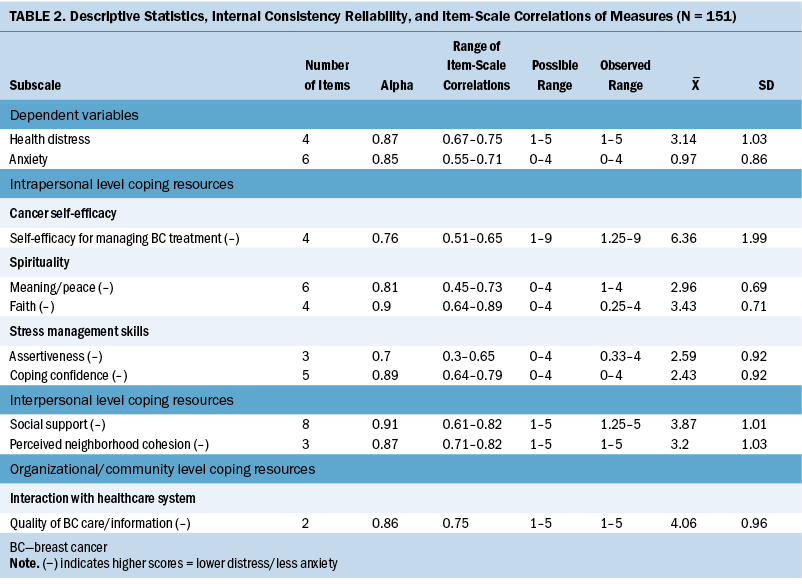
The 151 women were, on average, 50.5 years old. Most (66%) of the women had less than sixth-grade education, 78% had only public insurance, and 78% reported financial hardship in the past year (see Table 1). Most were Mexican immigrants (68%); English-language acculturation was low (mean = 1.3; SD = 0.6). The proportion who reported taking antidepressants prior to their breast cancer diagnosis was low (11%). About half (48%) of the women had received their breast cancer diagnosis within three months or less. More than half reported having a lumpectomy (56%); most received some form of adjuvant treatment.
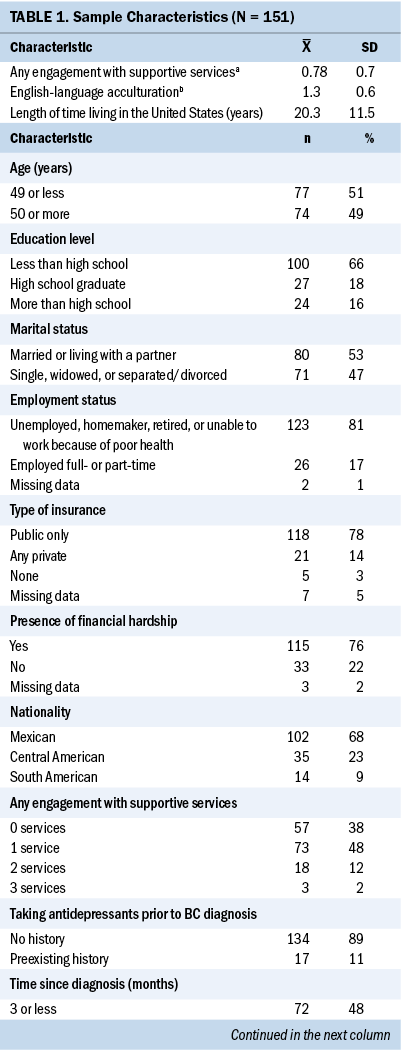
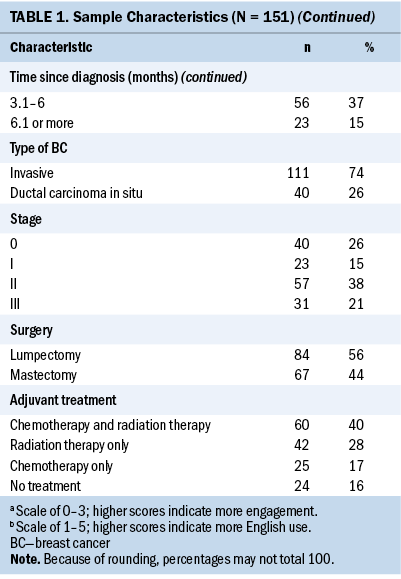
Table 2 presents descriptive statistics, internal consistency reliability, and item-scale correlations of independent and dependent variables. The mean health distress score was 3.14 (SD = 1.03), and the mean anxiety score was 0.97 (SD = 0.86).
Bivariate Correlations
Several demographic and clinical covariates were associated with the two dependent variables. Health distress was inversely associated with employment status and months since breast cancer diagnosis and positively associated with language acculturation at p < 0.2. English-language acculturation was positively associated with health distress. Health distress was not associated with age, education, marital status, or financial hardship, or clinical and treatment characteristics (history of taking antidepressants prior to breast cancer diagnosis, type of breast cancer surgery, or type of adjuvant treatment).
Anxiety was positively associated with financial hardship, English-language acculturation, history of taking antidepressants prior to breast cancer diagnosis, months since breast cancer diagnosis, and type of breast cancer surgery at p < 0.2. Anxiety was not associated with age, education, marital status, or employment status, or clinical and treatment characteristics (type of adjuvant treatment).
The correlation between health distress and anxiety was 0.55 (p < 0.0001). All measures of intrapersonal, interpersonal, and organizational/community level resources were significantly associated with health distress and anxiety, with correlations ranging from –0.43 to 0.14 for health distress and from –0.45 to 0.17 for anxiety. Using a p < 0.2 criteria, health distress was correlated with employment status, language acculturation, and time since breast cancer diagnosis; anxiety was correlated with financial hardship, history of antidepressants, and type of surgery.
Health Distress Models
Table 3 presents the results of the health distress models. In model 1, demographic and clinical covariates alone explained 11% of the variance in health distress (R2 = 0.1084; F[4, 144] = 4.37, p < 0.01). In model 1, being employed (β = –0.49, standard error [SE] = 0.22; p < 0.05) was inversely associated with health distress. Therefore, women who were employed had less health distress. English-language acculturation (β = 0.37, SE = 0.15; p < 0.05) was positively associated with health distress; therefore, those who were more English-language acculturated had higher levels of health distress. Compared to women diagnosed 6.1 months ago or more, women diagnosed within the past 3 months or less (β = 0.55, SE = 0.24; p < 0.05) or 3.1–6 months ago (β = 0.57, SE = 0.25; p < 0.05) reported higher levels of distress.
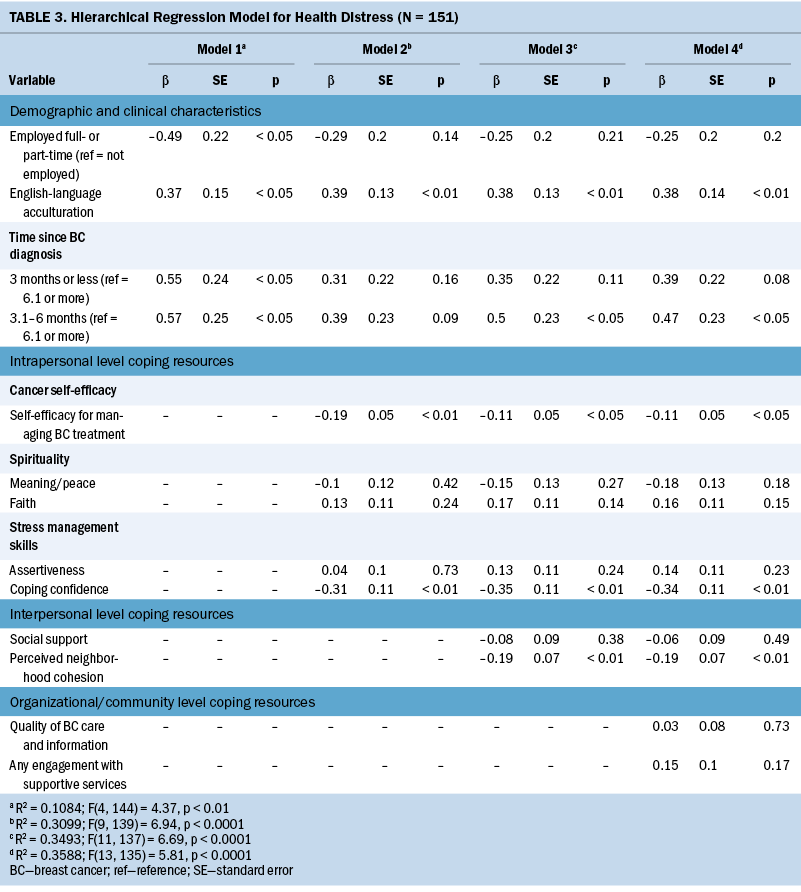
In model 2, adding intrapersonal level coping resources explained 31% of the variance in health distress (R2 = 0.3099; F[9, 139] = 6.94, p < 0.0001). Level of English-language acculturation continued to be positively associated with health distress (β = 0.39, SE = 0.13; p < 0.01). Self-efficacy for managing breast cancer treatment (β = –0.19, SE = 0.05; p < 0.01) and coping confidence (β = –0.31, SE = 0.11; p < 0.01) were inversely associated with health distress; those with greater self-efficacy and confidence had less distress.
Model 3, adding interpersonal level coping resources, explained 35% of the variance in health distress (R2 = 0.3493; F[11, 137] = 6.69, p < 0.0001). English-language acculturation remained positively associated with health distress (β = 0.38, SE = 0.13; p < 0.01). Compared to women diagnosed 6.1 months ago or more, women diagnosed 3.1–6 months ago (β = 0.5, SE = 0.23; p < 0.05) reported higher levels of health distress. Self-efficacy for managing breast cancer treatment (β = –0.11, SE = 0.05; p < 0.05) and coping confidence (β = –0.35, SE = 0.11; p < 0.01) remained inversely associated with health distress. Perceived neighborhood cohesion (β = –0.19, SE = 0.07; p < 0.01) was inversely associated with health distress; those in more cohesive neighborhoods reported less distress.
Model 4, adding organizational/community level coping resources, explained 36% of the variance in health distress (R2 = 0.3588; F[13, 135] = 5.81, p < 0.0001). English-language acculturation remained positively associated with health distress (β = 0.38, SE = 0.14; p < 0.01). Compared to women diagnosed 6.1 months ago or more, women diagnosed 3.1–6 months ago (β = 0.47, SE = 0.23; p < 0.05) reported greater health distress. Self-efficacy for managing breast cancer treatment (β = –0.11, SE = 0.05; p < 0.05), coping confidence (β = –0.34, SE = 0.11; p < 0.01), and perceived neighborhood cohesion (β = –0.19, SE = 0.07; p < 0.01) remained inversely associated with health distress. Organizational/community level resources were not associated with health distress.
Anxiety Models
Table 4 presents the results of the anxiety models. Model 1, which included personal and clinical covariates, only explained 16% of the variance in anxiety (R2 = 0.1567; F[6, 141] = 4.37, p < 0.001). In model 1, financial hardship (β = 0.51, SE = 0.16; p < 0.01), English-language acculturation (β = 0.26, SE = 0.12; p < 0.05), and history of taking antidepressants (β = 0.54, SE = 0.22; p < 0.05) were positively associated with anxiety. Compared to women diagnosed 6.1 months ago or more, women diagnosed 3.1–6 months ago (β = 0.42, SE = 0.21; p < 0.05) reported greater anxiety.
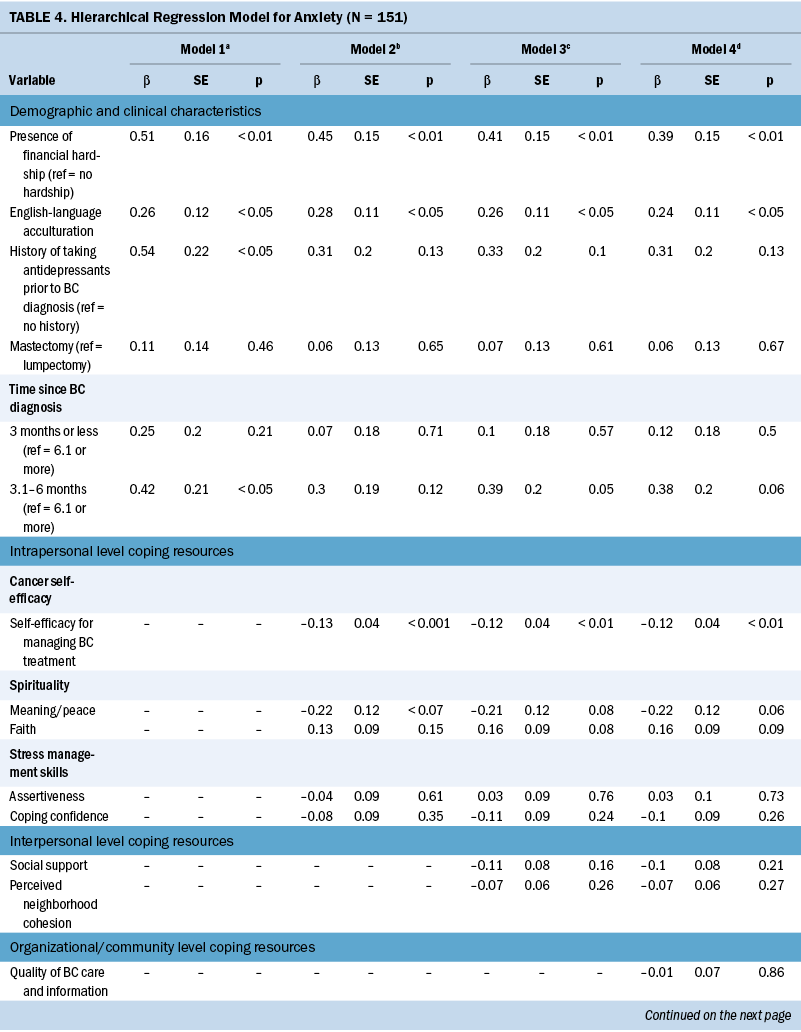
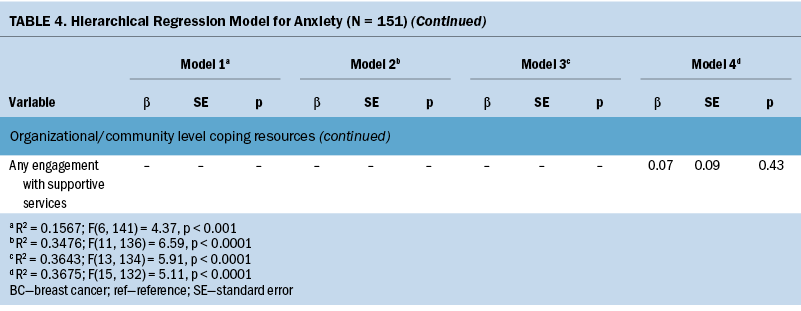
Model 2, adding intrapersonal level coping resources, explained 35% of the variance in anxiety (R2 = 0.3476; F[11, 136] = 6.59, p < 0.0001). Financial hardship (β = 0.45, SE = 0.15; p < 0.01) and English-language acculturation (b = 0.28, SE = 0.11; p < 0.05) remained significantly associated with anxiety. Self-efficacy for managing breast cancer treatment (β = –0.13, SE = 0.04; p < 0.001) was inversely associated with anxiety; those with greater self-efficacy for managing breast cancer treatment had less anxiety.
Model 3, adding interpersonal level coping resources, had a negligible effect on the amount of variance in anxiety explained (R2 = 0.3643; F[13, 134] = 5.91, p < 0.0001). Financial hardship (β = 0.41, SE = 0.15; p < 0.01) and English-language acculturation (β = 0.26, SE = 0.11; p < 0.05) remained positively associated with anxiety. Self-efficacy for managing breast cancer treatment (β = –0.12, SE = 0.04; p < 0.01) continued to be inversely associated with anxiety. None of the interpersonal level coping resources was associated with anxiety.
Model 4, adding organizational/community level coping resources, had no impact on the amount of variance in anxiety explained (R2 = 0.3675; F[15, 132] = 5.11, p < 0.0001). Financial hardship (β = 0.39, SE = 0.15; p < 0.01) and English-language acculturation (β = 0.24, SE = 0.11; p < 0.05) remained positively associated with anxiety. Self-efficacy for managing breast cancer treatment (β = –0.12, SE = 0.04; p < 0.01) continued to be inversely associated with anxiety, and none of the interpersonal level or organizational/community level coping resources was associated with anxiety.
Discussion
Applying an ecologic framework, this study assessed associations between intrapersonal, interpersonal, and organizational/community level coping resources and health distress and anxiety among newly diagnosed Spanish-speaking LWBC. Two intrapersonal resources (self-efficacy for managing breast cancer treatment and coping confidence) and one interpersonal resource (perceived neighborhood cohesion) were independently and inversely associated with health distress. Only one intrapersonal resource (self-efficacy for managing breast cancer treatment) was inversely associated with anxiety. At the organizational/community level, no resources were independently associated with either health distress or anxiety. In sum, the authors’ findings point to the importance of assessing the degree of a general sense of control that low-income, marginalized women with breast cancer have and their perceived internal and external resources for coping with cancer. These factors appear to have a significant impact on the levels of psychosocial distress that these women report.
One of the main challenges of a breast cancer diagnosis, particularly for Latina women who may have limited English proficiency, is managing the effects of their cancer treatment. When women feel confident to manage their treatment, this sense of control can ease distress associated with treatment side effects. Therefore, encouraging and providing Latina women with coping skills training, such as deep breathing or cognitive reframing, should be a mainstay of cancer care. Interventions that enhance self-efficacy in managing cancer side effects decrease feelings of psychological distress and anxiety for LWBC (Anderson & Armer, 2021). The authors’ findings also suggest that coping skills training that is general and not specific to handling treatment sequelae may not be adequate to assuage stronger distress levels in the form of anxiety among Spanish-speaking LWBC.
The authors’ findings suggest that fostering skills to identify and harness neighborhood support early on in the cancer care continuum may be helpful for reducing health distress, although these results require further confirmation. One study among urban Black breast cancer survivors and English- and Spanish-speaking post-treatment breast cancer survivors found that greater neighborhood stress was significantly associated with poorer self-reported health (Wu et al., 2018); therefore, how women perceive the resources and quality of their neighborhoods potentially affects their health perceptions.
Of the intrapersonal level coping resources, neither spirituality nor assertiveness in asking for help and expressing needs was associated with either health distress or general anxiety. The finding with respect to spirituality conflicts with prior evidence that religious coping is common among Latina women (Samuel et al., 2020), although those studies used religious coping resources and the current measures were related to a general sense of meaning and purpose in life and faith.
Of note, women who were more acculturated in their use of English experienced more health distress and anxiety. Greater English proficiency could mean more contact with mainstream populations and settings where discrimination, friction, and stress may be more prevalent than in ethnic enclaves, which may be protective. Despite the long-term residence in the United States of the study participants, they demonstrated fairly low acculturation levels, which could be indicative of residing in largely Latino enclave neighborhoods. In addition, immigrants may experience distress in being unable to use English fluently, compounding the difficulties they experience when accessing and using health services (Zhang et al., 2012). Healthcare professionals can decrease psychological distress among Spanish-speaking Latina women by offering and providing professional language interpretation services and engaging individuals in their health care. Patient-level interventions should provide information on individual rights to interpreter services and role play asking questions of healthcare professionals.
Financial hardship was independently and positively associated with anxiety, again reinforcing the importance of having adequate self-advocacy and communication skills and knowledge of legal protections for people with cancer. Subjective financial burden has been associated with poorer well-being and impaired HRQOL, regardless of health insurance coverage (Fenn et al., 2014). Referrals to oncology social workers or community resources can help with the costs of cancer treatments and patient advocacy with insurance companies and healthcare systems (Zafar et al., 2015). Patient level interventions can educate individuals on health insurance basics, potential costs of treatment, and patient assistance programs (Zafar et al., 2015).
Limitations
This study is limited to a sample that is not representative of all LWBC, because it primarily consisted of Spanish-speaking Mexican immigrants. Also, the data for this analysis are cross-sectional; therefore, causality of psychological distress cannot be determined. In addition, the authors applied the ecologic framework post hoc as an organizing analytic tool for this secondary data analysis project; therefore, not all levels or variables in the original framework are represented.
Implications for Nursing
The National Academies of Sciences, Engineering, and Medicine (2021) consensus report The Future of Nursing 2020–2030: Charting a Path to Achieve Health Equity calls for the nursing profession to leverage its whole person perspective and values to “lead the complex work of integrating the social and health sectors in support of the health and well-being of individuals, families, and communities” (p. xv). According to this report, nurses, by virtue of their presence across sectors and communities, can implement health system and point-of-care interventions to advance continuous care models that are individual- and population-centered and address upstream causes of health disparities. Core competencies for nurses include engaging individuals with chronic conditions in self-care and coordinating their care between the healthcare system and community and neighborhood resources. Because of improved survival for some of the most common cancers, cancer is often managed as a chronic condition. By virtue of their training and clinical experience, nurses are well-prepared for and vital to the development, testing, and implementation of culturally appropriate psychosocial support interventions for people with cancer. In addition, nurses are well-prepared to ensure that such interventions address cancer survivors’ social and economic contexts.
Conclusion
The results suggest that nurses can help develop, test, and implement linguistically and culturally tailored psychosocial interventions that can reduce psychosocial distress by assessing multilevel determinants of psychosocial distress among people with cancer, particularly those who are most vulnerable and marginalized. In the case of LWBC, nurses can personalize care plans and test interventions that leverage individuals’ support systems, including neighborhood support, and aid with developing cancer coping skills building and self-care care planning, efforts that can mitigate psychological distress among Spanish-speaking LWBC. With appropriate resources, nurses can address the social contexts of Latino people with cancer, incorporate their unique needs, and help ensure health and healthcare equity.
About the Authors
Jasmine Santoyo-Olsson, MS, is a project director in the Division of General Internal Medicine at the University of California, San Francisco and a doctoral candidate in the School of Public Health at the University of California, Berkeley; Anita L. Stewart, PhD, is a professor in the Institute for Health and Aging at the University of California, San Francisco; Carmen Ortiz, PhD, is the executive director of Circulo de Vida Cancer Support and Resource Center in San Francisco, CA; and Anna Maria Nápoles, PhD, MPH, is the scientific director at the National Institute on Minority Health and Health Disparities in Bethesda, MD. This research was supported by funds from the California Breast Cancer Research Grants Program Office of the University of California grants 15BB-1300 and 15BB-1301 and the Division of Intramural Research, National Institute on Minority Health and Health Disparities, National Institutes of Health. The opinions expressed in this article are the authors’ and do not reflect the views of the National Institutes of Health, the Department of Health and Human Services, or the U.S. government. All authors contributed to the conceptualization, design, and manuscript preparation. Santoyo-Olsson, Ortiz, and Nápoles completed the data collection. Santoyo-Olsson provided statistical support. Santoyo-Olsson, Stewart, and Nápoles provided the analysis. Santoyo-Olsson can be reached at jasmine.santoyo-olsson@ucsf.edu, with copy to ONFEditor@ons.org. (Submitted August 2021. Accepted January 4, 2022.)
References
Aguado Loi, C.X., Baldwin, J.A., McDermott, R.J., McMillan, S., Martinez Tyson, D., Yampolskaya, S., & VandeWeerd, C. (2013). Risk factors associated with increased depressive symptoms among Latinas diagnosed with breast cancer within 5 years of survivorship. Psycho-Oncology, 22(12), 2779-2788. https://doi.org/10.1002/pon.3357
American Cancer Society. (2021). Cancer facts and figures for Hispanic/Latino people, 2021–2023. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
Anderson, E.A., & Armer, J.M. (2021). Factors impacting management of breast cancer-related lymphedema (BCRL) in Hispanic/Latina breast cancer survivors: A literature review. Hispanic Health Care International, 19(3), 190–202. https://doi.org/10.1177/1540415321990621
Antoni, M.H., Lechner, S.C., Kazi, A., Wimberly, S.R., Sifre, T., Urcuyo, K.R., . . . Carver, C.S. (2006). How stress management improves quality of life after treatment for breast cancer. Journal of Consulting and Clinical Psychology, 74(6), 1143–1152. https://doi.org/10.1037/0022-006X.74.6.1152
Ashing-Giwa, K., Rosales, M., Lai, L., & Weitzel, J. (2013). Depressive symptomatology among Latina breast cancer survivors. Psycho-Oncology, 22(4), 845–853. https://doi.org/10.1002/pon.3084
Badger, T.A., Segrin, C., Sikorskii, A., Pasvogel, A., Weihs, K., Lopez, A.M., & Chalasani, P. (2020). Randomized controlled trial of supportive care interventions to manage psychosocial distress and symptoms in Latinas with breast cancer and their informal caregivers. Psychology and Health, 35(1), 87–106. https://doi.org/10.1080/08870446.2019.1626395
Baik, S.H., Oswald, L.B., Buitrago, D., Buscemi, J., Iacobelli, F., Perez-Tamayo, A., . . . Yanez, B. (2020). Cancer-relevant self-efficacy is related to better health-related quality of life and lower cancer-specific distress and symptom burden among Latina breast cancer survivors. International Journal of Behavioral Medicine, 27(4), 357–365. https://doi.org/10.1007/s12529-020-09890-9
Berkman, L.F., Kawachi, I., & Glymour, M.M. (2014). Social epidemiology (2nd ed.). Oxford University Press. https://doi.org/10.1093/med/9780195377903.001.0001
Dean, L.T., Gehlert, S., Neuhouser, M.L., Oh, A., Zanetti, K., Goodman, M., . . . Schmitz, K.H. (2018). Social factors matter in cancer risk and survivorship. Cancer Causes and Control, 29(7), 611–618. https://doi.org/10.1007/s10552-018-1043-y
Derogatis, L.R. (1993). BSI, brief symptom inventory: Administration, scoring, and procedures manual (4th ed.). National Computer Systems.
Diez Roux, A.V. (2001). Investigating neighborhood and area effects on health. American Journal of Public Health, 91(11), 1783–1789. https://doi.org/10.2105/ajph.91.11.1783
Fenn, K.M., Evans, S.B., McCorkle, R., DiGiovanna, M.P., Pusztai, L., Sanft, T., . . . Chagpar, A.B. (2014). Impact of financial burden of cancer on survivors’ quality of life. Journal of Oncology Practice, 10(5), 332–338. https://doi.org/10.1200/JOP.2013.001322
Foglino, S., Bravi, F., Carretta, E., Fantini, M.P., Dobrow, M.J., & Brown, A.D. (2016). The relationship between integrated care and cancer patient experience: A scoping review of the evidence. Health Policy, 120(1), 55–63. https://doi.org/10.1016/j.healthpol.2015.12.004
Friedman, L.C., Kalidas, M., Elledge, R., Chang, J., Romero, C., Husain, I., . . . Liscum, K.R. (2006). Optimism, social support and psychosocial functioning among women with breast cancer. Psycho-Oncology, 15(7), 595–603. https://doi.org/10.1002/pon.992
Graupner, C., Kimman, M.L., Mul, S., Slok, A.H.M., Claessens, D., Kleijnen, J., . . . Breukink, S.O. (2021). Patient outcomes, patient experiences and process indicators associated with the routine use of patient-reported outcome measures (PROMs) in cancer care: A systematic review. Supportive Care in Cancer, 29(2), 573–593. https://doi.org/10.1007/s00520-020-05695-4
Hei, A., Simon, M.A., & Dong, X. (2019). Association between neighborhood cohesion and cancer screening utilization in Chinese American older adults. Journal of Immigrant and Minority Health, 21(4), 830–836. https://doi.org/10.1007/s10903-018-0783-9
Henselmans, I., Helgeson, V.S., Seltman, H., de Vries, J., Sanderman, R., & Ranchor, A.V. (2010). Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychology, 29(2), 160–168. https://doi.org/10.1037/a0017806
Kim, D., Diez Roux, A.V., Kiefe, C.I., Kawachi, I., & Liu, K. (2010). Do neighborhood socioeconomic deprivation and low social cohesion predict coronary calcification?: The CARDIA study. American Journal of Epidemiology, 172(3), 288–298. https://doi.org/10.1093/aje/kwq098
Kim, J. (2010). Neighborhood disadvantage and mental health: The role of neighborhood disorder and social relationships. Social Science Research, 39(2), 260–271. https://doi.org/10.1016/j.ssresearch.2009.08.007
Lazarus, R.S., & Folkman, S. (1984). Stress, appraisal, and coping. Springer Publishing Company.
Lorig, K., Stewart, A.L., Lynch, J., Gonzales, V., & Ritter, P.L. (1996). Concepts and measures for evaluating outcomes of health education and other health interventions. Sage.
Marin, G., Sabogal, F., Marin, B.V., Otero-Sabogal, R., & Perez-Stable, E.J. (1987). Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences, 9(2), 183–205. https://doi.org/10.1177/07399863870092005
McLeroy, K.R., Bibeau, D., Steckler, A., & Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4), 351–377. https://doi.org/10.1177/109019818801500401
Merluzzi, T.V., Nairn, R.C., Hegde, K., Martinez Sanchez, M.A., & Dunn, L. (2001). Self-efficacy for coping with cancer: Revision of the cancer behavior inventory (version 2.0). Psycho-Oncology, 10(3), 206–217. https://doi.org/10.1002/pon.511
Moreno, P.I., Ramirez, A.G., San Miguel-Majors, S.L., Castillo, L., Fox, R.S., Gallion, K.J., . . . Penedo, F.J. (2019). Unmet supportive care needs in Hispanic/Latino cancer survivors: Prevalence and associations with patient-provider communication, satisfaction with cancer care, and symptom burden. Supportive Care in Cancer, 27(4), 1383–1394. https://doi.org/10.1007/s00520-018-4426-4
Moser, A., Stuck, A.E, Silliman, R.A., Ganz, P.A., & Clough-Gorr, K.M. (2012). The eight-item modified Medical Outcomes Study Social Support Survey: Psychometric evaluation showed excellent performance. Journal of Clinical Epidemiology, 65(10), 1107–1116. https://doi.org/10.1016/j.jclinepi.2012.04.007
Mulvaney-Day, N.E., Alegría, M., & Sribney, W. (2007). Social cohesion, social support, and health among Latinos in the United States. Social Science and Medicine, 64(2), 477–495.
Nápoles, A.M., Ortíz, C., O’Brien, H., Sereno, A.B., & Kaplan, C.P. (2011). Coping resources and self-rated health among Latina breast cancer survivors. Oncology Nursing Forum, 38(5), 523–531. https://doi.org/10.1188/11.ONF.523-531
Nápoles, A.M., Ortíz, C., Santoyo-Olsson, J., Stewart, A.L., Gregorich, S., Lee, H.E., . . . Luce, J. (2015). Nuevo Amanecer: Results of a randomized controlled trial of a community-based, peer-delivered stress management intervention to improve quality of life in Latinas with breast cancer. American Journal of Public Health, 105(53, Suppl. 3), e55–e63. https://doi.org/10.2105/AJPH.2015.302598
Nápoles, A.M., Santoyo-Olsson, J., Ortíz, C., Gregorich, S., Lee, H.E., Duron, Y., . . . Stewart, A.L. (2014). Randomized controlled trial of Nuevo Amanecer: A peer-delivered stress management intervention for Spanish-speaking Latinas with breast cancer. Clinical Trials, 11(2), 230–238. https://doi.org/10.1177/1740774514521906
Nápoles, A.M., Santoyo-Olsson, J., Stewart, A.L., Ortiz, C., & García-Jímenez, M. (2018). Evaluating the implementation of a translational peer-delivered stress management program for Spanish-speaking Latina breast cancer survivors. Journal of Cancer Education, 33(4), 875–884. https://doi.org/10.1007/s13187-017-1202-y
Nápoles-Springer, A.M., Ortíz, C., O’Brien, H., Díaz-Méndez, M., & Pérez-Stable, E.J. (2007). Use of cancer support groups among Latina breast cancer survivors. Journal of Cancer Survivorship, 1(3), 193–204. https://doi.org/10.1007/s11764-007-0029-7
National Academies of Sciences, Engineering, and Medicine. (2021). The future of nursing 2020-2030: Charting a path to achieve health equity. National Academies Press. https://doi.org/10.17226/25982
Peterman, A.H., Fitchett, G., Brady, M.J., Hernandez, L., & Cella, D. (2002). Measuring spiritual well-being in people with cancer: The Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being scale (FACIT-Sp). Annals of Behavioral Medicine, 24(1), 49–58.
Ramirez, A.G., Muñoz, E., Long Parma, D., Perez, A., & Santillan, A. (2020). Quality of life outcomes from a randomized controlled trial of patient navigation in Latina breast cancer survivors. Cancer Medicine, 9(21), 7837–7848. https://doi.org/10.1002/cam4.3272
Ream, M.E., Pester, M.S., Goodman, Z.T., Bainter, S.A., & Antoni, M.H. (2021). Elucidating mechanisms of quality-of-life disparities in Hispanic women with breast cancer: An examination of disease stage, coping, and affect. Psycho-Oncology, 30(4), 623–631. https://doi.org/10.1002/pon.5611
Roland, K.B., Milliken, E.L., Rohan, E.A., DeGroff, A., White, S., Melillo, S., . . . Young, P.A. (2017). Use of community health workers and patient navigators to improve cancer outcomes among patients served by federally qualified health centers: A systematic literature review. Health Equity, 1(1), 61–76. https://doi.org/10.1089/heq.2017.0001
Rosales, M., Ashing, K., & Napoles, A. (2014). Quality of cancer follow-up care: A focus on Latina breast cancer survivors. Journal of Cancer Survivorship, 8(3), 364–371. https://doi.org/10.1007/s11764-014-0343-9
Roy, M., Purington, N., Liu, M., Blayney, D.W., Kurian, A.W., & Schapira, L. (2021). Limited English proficiency and disparities in health care engagement among patients with breast cancer. JCO Oncology Practice, 17(12), e1837-e1845. https://doi.org/10.1200/OP.20.01093
Samuel, C.A., Mbah, O.M., Elkins, W., Pinheiro, L.C., Szymeczek, M.A., Padilla, N., . . . Corbie-Smith, G. (2020). Calidad de Vida: A systematic review of quality of life in Latino cancer survivors in the USA. Quality of Life Research, 29(10), 2615–2630. https://doi.org/10.1007/s11136-020-02527-0
Segrin, C., Badger, T., & Sikorskii, A. (2021). Psychological distress and social support availability in different family caregivers of Latinas with breast cancer. Journal of Transcultural Nursing, 32(2) 103–110. https://doi.org/10.1177/1043659619896824
Taylor, S.E., & Stanton, A.L. (2007). Coping resources, coping processes, and mental health. Annual Review of Clinical Psychology, 3(1), 377–401. https://doi.org/10.1146/annurev.clinpsy.3.022806.091520
Williams, D.R., Mohammed, S.A., & Shields, A.E. (2016). Understanding and effectively addressing breast cancer in African American women: Unpacking the social context. Cancer, 122(14), 2138–2149. https://doi.org/10.1002/cncr.29935
Wu, C., Ashing, K.T., Jones, V.C., & Barcelo, L. (2018). The association of neighborhood context with health outcomes among ethnic minority breast cancer survivors. Journal of Behavioral Medicine, 41(1), 52–61. https://doi.org/10.1007/s10865-017-9875-6
Yoo, G.J., Levine, E.G., & Pasick, R. (2014). Breast cancer and coping among women of color: A systematic review of the literature. Supportive Care in Cancer, 22(3), 811–824. https://doi.org/10.1007/s00520-013-2057-3
Zafar, S.Y., Ubel, P.A., Tulsky, J.A., & Pollak, K.I. (2015). Cost-related health literacy: A key component of high-quality cancer care. Journal of Oncology Practice, 11(3), 171–173.
Zhang, W., Hong, S., Takeuchi, D.T., & Mossakowski, K.N. (2012). Limited English proficiency and psychological distress among Latinos and Asian Americans. Social Science and Medicine, 75(6), 1006–1014. https://doi.org/10.1016/j.socscimed.2012.05.012




