Perianal Injury Prevention in Patients With Leukemia
Background: Perianal injuries in adults with hematologic malignancies can result in sepsis or death. Patients on a 36-bed acute care oncology unit experienced increased perianal injuries from 2018 to 2021 based on a chart review, which revealed that 24 patients with leukemia, all of whom had received cytarabine, developed perianal injuries.
Objectives: This study examined whether a nurse-led educational intervention would decrease perianal injuries.
Methods: A survey examined baseline nurse knowledge on perianal injuries. Nurses received a 10-minute in-service education session about perianal injuries, their predisposing factors, and prevention strategies followed by a survey to test their knowledge. Twenty nurses completed the pre- and postintervention surveys.
Findings: After the intervention, staff knowledge increased by 33%. One year postintervention, perianal injuries had decreased by more than 50%. Nurse and patient education are vital to decrease perianal injuries in patients with leukemia.
Jump to a section
Earn free contact hours: Click here to connect to the evaluation. Certified nurses can claim no more than 1 total ILNA point for this program. Up to 1 ILNA point may be applied to Symptom Management, Palliative Care, Supportive Care OR Treatment. See www.oncc.org for complete details on certification.
Hematologic malignancies are liquid tumors that include leukemias, lymphomas, and multiple myeloma. Leukemias, some of the most common hematologic malignancies, originate in the bone marrow and cause proliferation of different cell types, most commonly the white blood cells. Immature white blood cells, known as leukocytes, crowd the bone marrow and prohibit adequate cell production from other cell types like red blood cells and platelets. According to the American Cancer Society (2023), 59,610 new cases of leukemia were estimated to have been diagnosed in 2023, and 23,710 people were estimated to have died from the disease. Acute myeloid leukemia (AML) is one of the most diagnosed types of leukemia among adults, comprising 31% of all leukemias (American Cancer Society, 2023). Patients with AML have an overall survival rate of 30% and can have severe life-threatening complications from treatment (Di Francia et al., 2021). Various modalities can be used to treat leukemia including chemotherapy, sometimes in combination with targeted therapies.
Cytarabine is a frequently used chemotherapeutic agent to treat leukemia in combination with other agents. Cytarabine is classified as an anthracycline, which is effective in the treatment of acute leukemias and lymphomas like AML and acute lymphoblastic leukemia (ALL) (Faruqi & Tadi, 2023). The most serious side effect of cytarabine is severe myelosuppression, which leads to neutropenia, thrombocytopenia, and anemia. Myelosuppression can be dose-limiting and even life-threatening. Patients with neutropenia are at higher risk for infection, and patients with thrombocytopenia are at higher risk for bleeding, injury, and delayed healing (Loureiro et al., 2018). Patients are most vulnerable when they are in the nadir period, which typically occurs around 7–12 days following chemotherapy administration (Olsen et al., 2019). It is important to closely monitor patients during this time and intervene promptly when they exhibit signs and symptoms of infection (Brant et al., 2020). Gastrointestinal disturbances are additional side effects of cytarabine, but these are rarely mentioned in the literature (Isabella & Adnyana, 2022). Boussios et al. (2012) noted that cytarabine can cause oral and anal inflammation or ulceration. This inflammation, combined with constipation and thrombocytopenia, can lead to a perianal injury.
Types of Perianal Injuries
A perianal injury can be described as a rectal fissure (small tear in the anal canal), abscess, or fistula (see Table 1). Patients and healthcare providers may confuse anal fissures with hemorrhoids more than 35% of the time because patients with both conditions present with mild rectal bleeding and pain (Lu et al., 2021). However, there is a distinct difference in the duration and severity of pain between the two; hemorrhoids rarely cause persistent rectal pain for more than a day, and the pain is typically attributed to attempts at toileting. Patients with persistent rectal pain need a more extensive examination to ensure that no perianal injury is present.
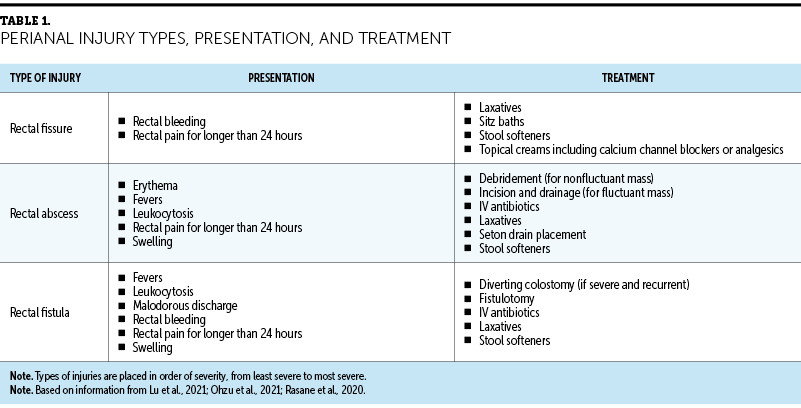
A rectal abscess, defined as “the presence of a firm or fluctuant tender mass located close to the anus,” is caused by an infection of the anal glands (Rasane et al., 2020, p. 824). Rectal fissures, if not identified and treated, can create a means of entry for bacteria and develop into an abscess. The risk of such complications is increased during the nadir period when patients are most immunocompromised (Chen et al., 2013). Prompt initiation of IV antibiotics, as well as incision and drainage, is important for patients who have fluctuant abscesses to prevent progressive inflammation and infection and to relieve pain. Abscess progression can look like sepsis or Fournier gangrene, and the abscess can develop into a fistula (Ohzu et al., 2021). It is estimated that one-third of rectal abscesses will progress to chronic fistula formation (Chen et al., 2013).
Rectal fistulas are characterized by “chronic inflammation and the epithelialization of a tract connecting the inciting anal gland with the perianal skin”; secretions from or around the anus travel through this tract (Ohzu et al., 2021, p. 2). Patients with rectal fistulas present with perianal pain, malodorous discharge, rectal bleeding, and swelling. Treatment for patients with fistulas includes a fistulotomy and can lead to a diverting colostomy to control the secretions, decrease exacerbation of the injury, and heal the fistula. For all perianal injuries, the provider conducts a bedside examination. If the patient is unable to tolerate the examination, it can be performed under anesthesia to adequately assess the extent of the injury. Patients with fistulas require prompt initiation of IV antibiotics to prevent the progression of infection. Creating a treatment plan for these patients can be difficult because of neutropenia, slow wound healing, and the risk of increased bleeding (Chen et al., 2013).
Predisposing Factors
It is important to identify the risk factors for perianal injuries to educate patients about predisposing factors and their effects (see Figure 1). One of the most common predisposing factors is receiving cytarabine. Cytarabine has been shown to cause anal inflammation, which, in combination with constipation, can lead to a perianal injury (Boussios et al., 2012). Constipation is the lack of passing fecal matter or difficulty when passing stool. Patients with cancer are known to experience constipation from treatment, pain medications, or decreased food and/or fluid intake (Hay et al., 2019). Because of the differing perceptions of what constipation is and the irregularity of bowel movements in the general population (Dimidi et al., 2019), patient education about stool softeners and laxatives in cancer care is important. Complications from constipation can quickly arise in patients receiving cancer treatment. Providers should educate patients to report when they have not had a bowel movement in more than 24 hours.
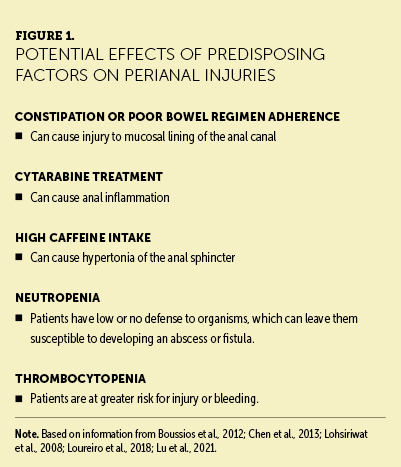
Another risk factor for perianal injuries is high caffeine intake. Caffeine is a diuretic, and an increased intake of caffeine can lead to constipation because of decreased water content in the stool; this leads to straining when defecating because of hard fecal matter (Fowler, 2011). Caffeine can also cause hypertonia of the anal sphincter, which is defined as increased contractility of the muscle. With hypertonia of the anal sphincter, the anal canal narrows, which increases the risk of anal injury from hard fecal matter. In addition, contraction of the sphincter reduces blood flow and increases risk of delayed wound healing. Lack of ability to relax the anal sphincter potentiates constipation because there is a decreased sensory threshold for the desire to defecate (Lohsiriwat et al., 2008).
Signs and Symptoms
Patient presentation for any perianal injury includes rectal pain that persists for more than 24 hours and rectal bleeding. Perianal injuries can become exacerbated with each bowel movement. Patients with abscesses tend to present with rectal pain, swelling, erythema, fever, and leukocytosis. However, patients with hematologic malignancies may not present in classic ways because of the absence of inflammatory cells and a lack of a visual inflammatory response (e.g., redness, edema, erythema) (Solmaz et al., 2016). These patients may or may not present with leukocytosis, but this is often associated with leukemia and may not always be attributed to a perianal infection. It may also be difficult to identify a rectal abscess in this patient population because of neutropenic fevers following chemotherapy administration, as the fevers may be attributed to the disease process.
A challenge when treating perianal injuries is their high recurrence rate. In one study of anorectal complications in neutropenic patients, 73.7% of patients who were neutropenic experienced a recurrence of perianal injuries. Patients with active disease were more likely to develop anorectal complications, compared to those whose disease was controlled or in remission (67% versus 40%) (Solmaz et al., 2016). Although reports of perianal injury have been noted for many years, this is not a complication that is commonly discussed in the literature and is not always part of the education that patients receive prior to starting chemotherapy. However, educating patients about predisposing factors, prevention, early identification, and prompt interventions is key for reducing morbidity and mortality (Loureiro et al., 2018).
Background
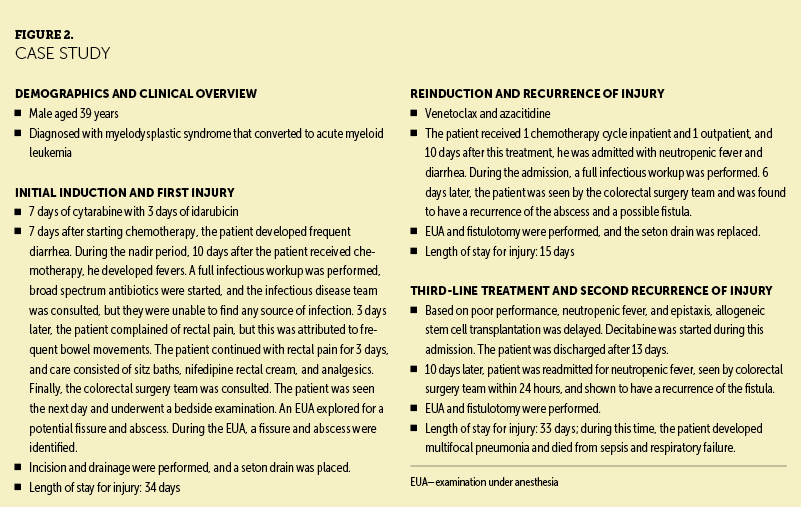
In early 2021, perianal injuries increased in Walter Tower 14, an inpatient acute care oncology unit at Houston Methodist Hospital in the Texas Medical Center. Patients with leukemia were noted to have had increased development of severe rectal pain, bleeding, and fevers, as well as increased admissions for and recurrence of perianal injuries. Nurses on the unit recalled walking through the hallways and hearing patients screaming and crying because of the pain they experienced when having a bowel movement. The pain was so severe for some patients that an opioid premedication was administered for pain management prior to using the restroom. Patients who developed these perianal injuries also experienced treatment delays and longer hospitalizations. In instances where detection and treatment of the perianal injury was delayed, patients became septic. Figure 2 illustrates a case study of a patient who experienced perianal injuries.
Recognizing this difficulty among patients, a small group of oncology nurses from the acute care oncology unit formed a team to try to find the cause and potential contributing factors of these perianal injuries and formulate a plan to improve patient outcomes. The team also consulted physicians in the malignant hematology-oncology group and internal medicine department.
A chart review was conducted for patients diagnosed with a hematologic malignancy who had developed a perianal injury. Of all patients seen from January 2018 to December 2021, 33 were identified from the initial review. To refine the search, only patients who underwent induction chemotherapy and were diagnosed with leukemia were included. Exclusion criteria were having a history of a perianal injury prior to receiving chemotherapy or having any perianal injury diagnosis that was not a fissure, abscess, or fistula. The following demographic and clinical characteristics of 24 patients with perianal injuries were reviewed in detail: diagnosis, perianal injury type, surgical interventions, age, gender, race, significant medical history, absolute neutrophil count at the time of injury, chemotherapy received, and mortality. The common factor in all 24 patients was the receipt of cytarabine chemotherapy. This information was presented to unit leadership and the nurse scientist department, which approved pursuing this issue and finding a way to prevent perianal injuries and improve care.
Purpose
The purpose of this article is to raise awareness of perianal injuries in patients with leukemia and report the experience from an inpatient adult oncology unit where a nurse-led educational intervention for nurses and other healthcare providers helped to decrease perianal injury rates and improve patient outcomes.
Methods
Quality Improvement Project
After analyzing the data retrieved from the search, the team developed an education plan for healthcare providers and patients, focusing on predisposing factors, prevention, and early identification of perianal injuries in patients with leukemia receiving cytarabine. To better understand the care team’s knowledge of the topic, nurses on the acute care oncology unit answered a five-question survey to gauge baseline knowledge about perianal injuries. This survey was developed by the team of oncology nurses based on a literature review. Twenty nurses from both shifts completed the preintervention survey. After this survey was completed, nurses were educated about perianal injuries.
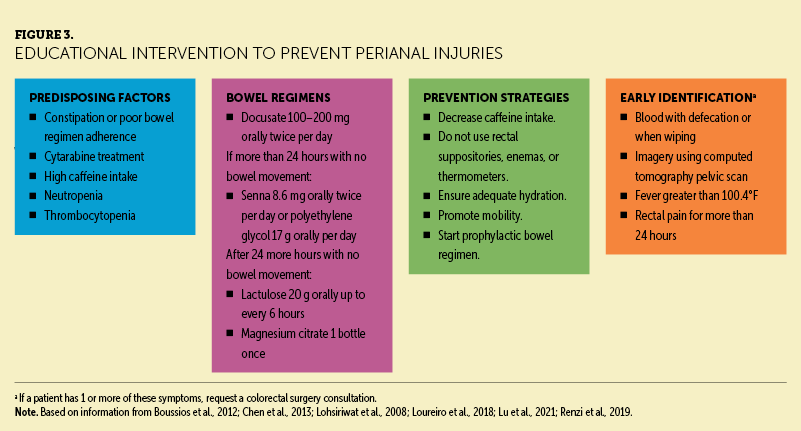
Education consisted of information about predisposing factors, bowel regimens, prevention, and early identification of perianal injuries (see Figure 3). Using an interprofessional, collaborative approach with internal medicine physicians and the malignant hematology-oncology group, a standard bowel regimen was created for patients at risk. The regimen consisted of five medications to be provided if a patient did not have a bowel movement for 24 hours, and medications could be held if the patient had more than two watery bowel movements in a day. Nurses were also educated about signs and symptoms of perianal injuries, including rectal pain persisting for more than 24 hours, fevers, and bleeding with bowel movements. Education emphasized that persistent rectal pain, regardless of the presence of fever or bleeding, should be escalated to the physician for a bedside examination, and a consultation from a colorectal physician or surgeon should be requested. A poster at the nurses’ station reinforced this information, and short in-service education sessions were held at change of shift for two weeks. The same 20 nurses who completed the preintervention survey were then asked to answer a postintervention survey.
Results
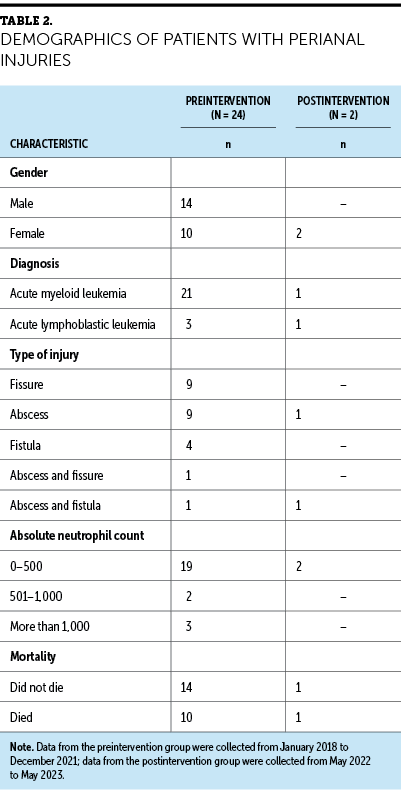
Charts of all patients seen from May 2022 to May 2023 were reviewed to determine whether the incidence of perianal injuries in patients with a hematologic malignancy had decreased. Only two patients developed a perianal injury during this time. One of these patients was nonadherent to prevention strategies and had missed outpatient follow-up visits; the other patient had behavioral comorbidities that limited her ability to report her symptoms. Previously, an average of six injuries per year was found from 2018 to 2021; this indicated a more than 50% reduction in perianal injuries after education was implemented (see Table 2). Postintervention, nurses on the acute care oncology unit had a 33% increase in knowledge about perianal injuries.
Discussion
Before the educational intervention, it was common for patients on this unit to refuse stool softeners and laxatives because of lack of knowledge and understanding of their risk of developing gastrointestinal complications like perianal injury. After the intervention, patients admitted to the acute care oncology unit were counseled at the bedside by their nurses about the risk factors and prevention strategies for perianal injury prior to the start of cytarabine. Knowledge focused on predisposing factors and prevention strategies for perianal injuries in patients with leukemia receiving cytarabine equipped nurses to educate their patients more confidently about these injuries, and it empowered patients to be active participants in their preventive care. With this specific nurse education in place, patients were noted to be more forthcoming about their bowel patterns, and adherence to bowel regimens and medications increased.
The data collected from 2018 to 2023 indicate that patients with AML have a higher risk of developing perianal injuries than patients with other types of leukemia including ALL. This could be related to the receipt of continuous and frequent cytarabine infusions compared to patients with ALL or lymphoma. A continuous infusion of 100 mg/m2 per day for seven days is the standard regimen for patients with AML receiving induction chemotherapy with cytarabine. By contrast, patients with ALL receive 3,000 mg/m2 every 12 hours on days 2 and 3 (Faruqui & Tadi, 2023). Although the dose is lower in milligrams for patients with AML, the continuous regimen may cause more toxicity than the intermittent high dose because the patient is exposed to the drug for an extended period (Faruqui & Tadi, 2023).
Another consideration is that patients with AML are neutropenic for longer periods of time and can have more severe mucositis than those with ALL or lymphoma (Chen et al., 2013). Patients with an absolute neutrophil count of less than 500 had the greatest risk of injury. Of the patients identified for this study from the chart review pre- and postintervention, 14 males developed a perianal injury, and 12 females also developed this complication. There was not a large difference in the number of injuries in one gender versus the other, although other studies have mentioned that males have higher rates of perianal injuries (Loureiro et al., 2018; Vogel et al., 2016). In the participants in this review, the most common injuries were fissures and abscesses (10 fissures, 11 abscesses). Fistulas were not as common because the care team caught perianal injuries earlier rather than later, preventing the formation of a fistula. It was also common for a patient to have more than one type of perianal injury or a recurrence in perianal injury. Preintervention, 5 of 24 patients had an abscess or fistula recurrence; no patients had a recurrence following the intervention.
Limitations
Several limitations were identified during this project. Because this project consisted of only one hospital and one inpatient unit, there was a small sample size of patients and nurses. Another limitation was that the mortality rates may be higher than indicated because patients’ families do not necessarily notify their oncologist when patients die in hospice or outside of the hospital. Even if this is communicated, it is not always documented in the electronic health record. Recurrence rates were also limited because they were accurate only if the patient had not died during their hospital stay and if they had continued follow-up visits at the project site. Length of stay may have also been affected by count recovery times, socioeconomic issues, delays in discharge planning, death, or other complications. Age and race were not included in the patient demographics because they did not add to the results. The patients’ ages ranged from 19 to 65 years. Finally, no statistical analysis was used in this study.
Implications for Nursing
Education is a powerful tool used by healthcare providers to empower staff, improve patient outcomes, and potentially save lives through the adoption of best practices. The literature indicates that patients who are educated about their treatment plan, risk factors, and possible complications tend to have better outcomes than those who are not (Kean et al., 2016). Perianal injury prevention should be included in chemotherapy conversations, and education about having these conversations is essential for providers and nurses. This will alert patients of the possible complications of perianal injury and engage them in preventing their occurrence. Although perianal injuries are not commonly discussed with patients, either because of lack of knowledge on the topic or because it may be an uncomfortable topic, patients need to know their risk factors to make informed decisions about their care and medications.
Conclusion
Education is vital in the prevention of perianal injuries in patients with leukemia. If patients are engaged in their care, their outcomes may be more favorable because they feel like part of the team that includes their healthcare providers. Working together, patients and care providers can decrease possible complications of perianal injuries. It is important for patients with leukemia to be educated about perianal injuries, as well as for nurses and providers to identify and provide early treatment for this patient population that is severely immunocompromised. Perianal injuries should be discussed with patients and oncology providers (e.g., nurses, physicians, advanced practice RNs) to address this long-standing issue and decrease its occurrence. Although education seems like a simple intervention, it can improve outcomes for patients receiving oncology care.
The authors gratefully acknowledge the oncology nurses on Walter Tower 14 for their compassion and care for the patients and their hard work with this initiative; Alanda Phillips, MSN, RN, OCN®, for her care and idea to further investigate the issue of perianal injuries; and Shuang Li, MD, Satish Dinakar, MD, Shilpan Shah, MD, Nickolaus Escobedo, DNP, RN, OCN®, NE-BC, and Jean Konicke, MSN, RN, OCN®, NE-BC, for their support of this project.
About the Authors
Cindy Paredes, MSN, RN, OCN®, is an RN IV, Katie Reed, MSN, RN, OCN®, CPHQ, is a senior quality outcome specialist, and LaTarvia Moore, MSN, RN, OCN®, BMTCN®, NPD-BC, is a professional practice leader, all at Houston Methodist Hospital in Texas; and Jeannine M. Brant, PhD, APRN, AOCN®, FAAN, is the executive director of clinical science and innovation at City of Hope National Medical Center in Duarte, CA. The authors take full responsibility for this content and did not receive honoraria or disclose any relevant financial relationships. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Paredes can be reached at clopez7@houstonmethodist.org, with copy to CJONEditor@ons.org. (Submitted October 2023. Accepted December 19, 2023.)
References
American Cancer Society. (2023). Cancer facts and figures, 2023. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
Boussios, S., Pentheroudakis, G., Katsanos, K., & Pavlidis, N. (2012). Systemic treatment-induced gastrointestinal toxicity: Incidence, clinical presentation and management. Annals of Gastroenterology, 25(2), 106–118.
Brant, J.M., Cope, D.G., & Garzo Saria, M. (Eds.). (2020). Core curriculum for oncology nursing (6th ed.). Elsevier.
Chen, C.-Y., Cheng, A., Huang, S.-Y., Sheng, W.-H., Liu, J.-H., Ko, B.-S., . . . Tien, H.-F. (2013). Clinical and microbiological characteristics of perianal infections in adult patients with acute leukemia. PLOS ONE, 8(4), e60624. https://doi.org/10.1371/journal.pone.0060624
Di Francia, R., Crisci, S., De Monaco, A., Cafiero, C., Re, A., Iaccarino, G., . . . Pinto, A. (2021). Response and toxicity to cytarabine therapy in leukemia and lymphoma: From dose puzzle to pharmacogenomic biomarkers. Cancers, 13(5), 966. https://doi.org/10.3390/cancers13050966
Dimidi, E., Cox, C., Grant, R., Scott, S.M., & Whelan, K. (2019). Perceptions of constipation among the general public and people with constipation differ strikingly from those of general and specialist doctors and the Rome IV criteria. American Journal of Gastroenterology, 114(7), 1116–1129. https://doi.org/10.14309/ajg.0000000000000267
Faruqi, A. & Tadi, P. (2023). Cytarabine. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557680
Fowler, A. (2011). Anal fissure and its management. In S. Brown, J. Hartley, J. Hill, N. Scott, & J. Williams (Eds.), Contemporary coloproctology (pp. 37–46). Springer. https://doi.org/10.1007/978-0-85729-889-8_3
Hay, T., Bellomo, R., Rechnitzer, T., See, E., Abdelhamid, Y.A., & Deane, A.M. (2019). Constipation, diarrhea, and prophylactic laxative bowel regimens in the critically ill: A systematic review and meta-analysis. Journal of Critical Care, 52, 242–250. https://doi.org/10.1016/j.jcrc.2019.01.004
Isabella, K., & Adnyana, W.L. (2022). Neurotoxic effects of cytarabine in a patient with acute myeloblastic leukemia: A case report. International Journal of Research and Review, 9(3), 365–371. https://doi.org/10.52403/ijrr.20220341
Kean, C.C., Iverson, L., & Boylan, A. (2016). Evaluation of a chemotherapy and medication education process for patients starting cancer treatment. Clinical Journal of Oncology Nursing, 20(4), 364–366. https://doi.org/10.1188/16.CJON.364-366
Lohsiriwat, S., Kongmuang, P., & Leelakusolvong, S. (2008). Effects of caffeine on anorectal manometric findings. Diseases of the Colon and Rectum, 51(6), 926–931. https://doi.org/10.1007/s10350-008-9271-y
Loureiro, R.V., Borges, V.P., Tomé, A.L., Bernardes, C.F., Silva, M.J., & Bettencourt, M.J. (2018). Anorectal complications in patients with haematological malignancies. European Journal of Gastroenterology and Hepatology, 30(7), 722–726. https://doi.org/10.1097/MEG.0000000000001133
Lu, Y., Kwaan, M.R., & Lin, A.Y. (2021). Diagnosis and treatment of anal fissures in 2021. JAMA, 325(7), 688–689. https://doi.org/10.1001/jama.2020.16705
Ohzu, M., Takazawa, H., Furukawa, S., & Komeno, Y. (2021). Anorectal abscess in a patient with neutropenia and refractory acute myeloid leukemia: To operate or not to operate? American Journal of Case Reports, 22, e931589. https://doi.org/10.12659/AJCR.931589
Olsen, M.M., LeFebvre, K.B., & Brassil, K.J. (Eds.). (2019). Chemotherapy and immunotherapy guidelines and recommendations for practice. Oncology Nursing Society.
Rasane, R.K., Centeno Coleoglou, A.A., Horn, C.B., Torres, M.B., Nohra, E., Zhang, Q., . . . Bochicchio, G.V. (2020). Inadequate antibiotic therapy results in higher recurrence rate after drainage of complicated peri-rectal abscess. Surgical Infections, 21(10), 823–827. https://doi.org/10.1089/sur.2019.308
Renzi, S., Bartram, J., Ali, S., Portwine, C., Mitchell, D., Dix, D., . . . Sung, L. (2019). Perianal infections in children with acute myeloid leukemia: A report from the Canadian Infection in Acute Myeloid Leukemia Research Group. Journal of the Pediatric Infectious Diseases Society, 8(4), 354–357. https://doi.org/10.1093/jpids/piy081
Solmaz, S., Korur, A., Gereklioğlu, C., Asma, S., Büyükkurt, N., Kasar, M., . . . Ozdoğu, H. (2016). Anorectal complications during neutropenic period in patients with hematologic diseases. Mediterranean Journal of Hematology and Infectious Diseases, 8(1), e2016019. https://doi.org/10.4084/MJHID.2016.019
Vogel, J., Johnson, E., Morris, A., Paquette, I., Saclarides, T., Feingold, D., & Steele, S. (2016). Clinical practice guideline for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula. Diseases of the Colon and Rectum, 59(12), 1117–1133. https://doi.org/10.1097/DCR.0000000000000733

