Factors Influencing Patients’ Intention to Perform Physical Activity During Hematopoietic Cell Transplantation
Objectives: To examine theoretical and medical variables influencing a patient’s intention to perform physical activity during hospitalization for hematopoietic cell transplantation (HCT).
Sample & Setting: 54 patients undergoing HCT at the Seidman Cancer Center in Cleveland, Ohio.
Methods & Variables: A longitudinal, prospective cohort design was used. Instruments included the Self-Report Habit Index, tailored to assess exercise habit, the Memorial Symptom Assessment Scale–Short Form, and an investigator-constructed survey of intention, attitude, control, and subjective norm toward physical activity. Descriptive statistics, univariate logistic regression, and linear regression were used.
Results: Intention for physical activity remained high at all time points. Previous exercise habits were not related to intention. Inverse relationships between symptom distress and the theoretical constructs that influence intention occurred at the critical time points of nadir and discharge during transplantation.
Implications for Nursing: Nurses should reinforce physical activity regardless of exercise habits. Symptom distress may influence physical activity differently during the transplantation trajectory.
Jump to a section
Hematopoietic cell transplantation (HCT) is a potentially curative treatment modality for many malignant hematologic diseases. Because of the complexity of the transplantation course and the numerous types of interventions involved, patients often experience declines in physical activity, quality of life, physical functionality, and mental status (Jacobsen et al., 2014). Physical activity also declines immediately following transplantation. Potential causes include fatigue, environmental limitations, need for contact precautions, and periods of critical monitoring (Steinberg, Asher, Bailey, & Fu, 2015). Patients also experience increases in symptom burden and depressive symptoms and decrease in quality of life during hospitalization (El-Jawahri et al., 2014). A study by Cohen et al. (2012) provided a comprehensive overview of symptom severity and quality of life throughout the transplantation trajectory. They identified that, as time progressed during the acute transplantation phase, symptom severity increased and quality of life decreased.
The American Cancer Society (ACS) 2012 Nutrition and Physical Activity Guidelines for Cancer Survivors endorsed the use of physical activity in the general population of patients with cancer as a means to improve functional status and quality of life (Rock et al., 2012). Physical activity is defined as bodily movement that requires energy expenditure. In comparison, exercise involves structured, planned, and repetitive physical activity (Caspersen, Powell, & Christenson, 1985). More specifically, patients with malignant hematologic cancers and those undergoing HCT experience additional health benefits of physical activity in the dimensions of fatigue and cardiorespiratory fitness (Rock et al., 2012). In 2014, the Oncology Nursing Society (ONS) deemed exercise as its only evidence-based recommended practice intervention for combating cancer-related fatigue (Mitchell et al., 2014). More recent reviews of the literature support the findings and recommendations by the ACS regarding physical activity in the HCT population (Oberoi et al., 2018; Steinberg et al., 2015).
Despite evidence supporting the use of physical activity in the HCT setting, clinicians are challenged to engage patients in recommended physical activity during hospitalization for HCT. One factor, which may contribute to inactivity and has not been well examined in the empirical literature, is the patient’s own perspective toward performing physical activity during hospitalization. Patients undergoing HCT are vulnerable for inactivity because of high symptom burden, a limiting hospital environment, and periodic times of intense medical monitoring. More research to better understand the factors that influence their activity is needed. The current study addressed this gap by examining the relationships among key theoretical, medical, and individual factors. The aims of the study were as follows:
• To describe the intentions to engage in physical activity of adult patients who were undergoing HCT at baseline (i.e., before admission), within nadir (i.e., at lowest neutrophil count), and upon discharge
• To examine the effects of previous exercise habits on intention to perform physical activity
• To examine the relationships between intention to perform physical activity and the theoretical constructs of attitude, subjective norm, and perceived control
• To examine the relationships between symptom distress and the theoretical constructs of attitude, subjective norm, and perceived control
Theoretical Framework
The theory of planned behavior guided the design of this study. This theory, which posits that the individual’s intention to perform a behavior is an important and immediate determinant of the actual activity, has been used widely across disciplines (Ajzen, 1991; Glanz, Rimer, & Viswanath, 2008). Intention to perform the behavior is influenced by one’s attitude toward the behavior, perceived control of when and how the behavior will be performed, and subjective norm, which is the perceived social pressure to either engage or not engage in a behavior (Fishbein & Ajzen, 2010). According to this theory, other external variables may also influence intention, such as personal characteristics and personality traits (Glanz et al., 2008).
The intention to perform physical activity of an individual undergoing HCT could also be influenced by symptom distress and previous habits related to exercise. Symptom distress does not necessarily pertain solely to the most intense or frequent symptom; it also includes the patient’s perception of how bothersome or distressing the symptom is (McClement, Woodgate, & Degner, 1997). The concept of habit involves a set of characteristics that includes a history of repetition of unconscious acts toward achieving a satisfactory end goal. These acts are ultimately carried out because the individual identifies the need to achieve the goal (Verplanken & Orbell, 2003). Finally, other potential influencing factors toward physical activity that have not been well studied include demographic and medical variables, such as disease characteristics and transplantation modalities. A descriptive investigation of factors that may influence the patient’s intention to perform physical activity is needed to design effective, feasible interventions for patients undergoing HCT.
Methods
Design
A longitudinal, prospective cohort design was used to investigate factors that may influence patients’ intention to perform physical activity during their hospitalization. These factors include the patients’ attitude, subjective norm, perceived control, and intention toward physical activity, along with symptom distress, previous exercise habits, medical variables, and demographics.
Sample and Setting
The study was conducted at University Hospitals Seidman Cancer Center’s Adult Blood and Marrow Transplant inpatient unit in Cleveland, Ohio. The study received approval from the University Hospitals Cleveland Medical Center Institutional Review Board (IRB). A convenience sample was used. Transplantation coordinators, trained in the procedures for the study, identified and approached potential patients during their mandatory pretransplantation education session in the clinic from December 2016 to October 2017. Inclusion criteria were adult patients aged 18 years or older admitted to University Hospitals Seidman Cancer Center’s inpatient Adult Blood and Marrow Transplant unit undergoing HCT for a hematologic malignancy who were able to speak and understand English and provided evidence to support that they were aware of person, place, and time. Patients were excluded if they were placed on physician-ordered bed rest or were terminally ill.
Measures
Demographic and medical variables: Demographic variables included age, gender, race, marital status, employment status, educational degree achieved/attained, annual household income, current living arrangement, date of cancer diagnosis, and type of cancer. Variables collected from the patient’s medical record included type of transplantation (allogeneic versus autologous), source of hematopoietic cells, preparative regimen, number of chemotherapy and/or radiation cycles, months since diagnosis, and months since previously completed treatment.
Previous exercise habits: Verplanken and Orbell’s (2003) Self-Report Habit Index (SRHI) was used to measure a patient’s previous exercise habits. This index consists of 12 statements to measure the repetition, automaticity, and expression of identity related to a specific behavior. For this study, it was tailored toward previous exercise habits. Patients were given statements that included the following:
• Exercising is something I do frequently.
• Exercising is something I do automatically.
• Exercising is something I do without having to consciously remember.
Respondents rated their agreement or disagreement for each statement on a Likert-type scale from 1 (strong disagreement) to 10 (strong agreement). A mean score was calculated for all 12 items, with higher scores indicating greater habit strength. Psychometric properties of the SRHI were established in four studies of undergraduate students, with demonstration of good test-retest reliability (pre- and post-test coefficient alphas of 0.89 and 0.92, respectively) (Verplanken & Orbell, 2003). Convergent validity was supported with strong and significant correlation (r = 0.58, p < 0.001) with a response-frequency measure of transportation habit. The Cronbach alpha was 0.97 in the current study.
Symptom distress: The Memorial Symptom Assessment Scale–Short Form (MSAS-SF) was used to measure physical and psychological symptom distress (Chang, Hwang, Feuerman, Kasimis, & Thaler, 2000). Respondents were asked to rate the distress or bother associated with each symptom on a five-point Likert-type scale from 0 (not at all) to 4 (very much). Only symptoms the participant experienced during the past week were rated. Scoring of the MSAS-SF is based on three subscales: the global distress index (GDI), the physical symptom subscale (PHYS), and the psychological symptom subscale (PSYCH). A total MSAS-SF score was calculated, and higher scores indicated higher distress. Chang et al. (2000) reported good criterion validity and internal reliability (Cronbach alphas ranging from 0.76 to 0.87) of the MSAS-SF in a study of 299 patients with mixed cancer diagnoses. Construct validity of the MSAS-SF PSYCH was supported in a sample of patients with advanced cancer (Webber & Davies, 2011). Across time points in the current study, the Cronbach alphas for the total ranged from 0.84 to 0.87 for the MSAS-SF scale, 0.73 to 0.77 for the PSYCH, 0.76 to 0.77 for the PHYS, and 0.74 to 0.79 for the GDI.
Theory of planned behavior measures: An extensive literature search did not identify an appropriate survey for this population that assessed intention and the multiple factors that influence activity during transplantation. Therefore, an investigator-constructed survey, consistent with Fishbein and Ajzen’s (2010) recommendations, was used to self-report a patient’s attitude, perceived subjective norm, perceived control, and intention toward physical activity using the theory of planned behavior. Nine questions were developed and subsequently reviewed by a nurse scientist, an HCT-certified nurse practitioner, and a Blood and Marrow Transplant Certified Nurse (BMTCN®) to support content validity prior to use. The questions focused on physical activity above and beyond the expected habits of a patient undergoing HCT, such as walking to the bathroom. Patients were asked to answer three statements pertaining to attitude and perceived subjective norm toward physical activity, two statements relating to perceived control toward physical activity, and one associated with intention toward physical activity. Patients rated all of their responses on a seven-point Likert-type scale from 1 to 7. For example, a statement eliciting the patient’s attitude was as follows: For me, performing physical activity (sitting in a chair, walking around my room, or walking the halls) at least twice per day for the next three days would be unpleasant (1) to pleasant (7). An example of a statement to assess perceived subjective norm was as follows: Most people who are important to me think that I should perform physical activity (sitting in a chair, walking around my room, or walking the halls) at least twice per day for the next three days. This was rated on a scale of 1 (false) to 7 (true). Perceived control was assessed in the following statement: I have the ability to choose to perform physical activity (sitting in a chair, walking around my room, or walking the halls) at least twice per day for the next three days. This statement was rated on a scale of 1 (disagree) to 7 (agree). Intention was evaluated by a single statement: I intend to perform physical activity (sitting in a chair, walking around my room, or walking the halls) at least twice per day for the next three days. This statement was rated on a scale of 1 (unlikely) to 7 (likely). A mean score was calculated for each subcategory of questions. Higher scores indicate a greater positive impression toward each targeted subcategory.
Procedure
The anticipated trajectory for a patient’s white blood cell counts during their transplantation hospitalization helped to standardize the time at which instruments were administered. The expectation exists that a patient’s absolute neutrophil count (ANC) will be within normal range prior to admission; however, this is not true in circumstances when a patient is transitioning immediately from antineoplastic treatment to transplantation because of more aggressive disease status. Following the administration of the patient’s preparative regimen, the patient’s white blood cell count will drop from normally acceptable levels to profound neutropenia within days (Ezzone, 2013). After a period of time (days to weeks), a patient is expected to engraft, which refers to an improvement and subsequent stabilization of a patient’s hematopoietic function as a result of the infused hematopoietic cell graft (Ezzone, 2013). Discharge from the hospital occurs after engraftment and resolution of life-threatening complications that may have occurred in the immediate post-transplantation period. Complications can occur from the preparative treatment directly (e.g., anemia, thrombocytopenia, neutropenia, nausea, vomiting, diarrhea, mucositis, fevers, infection), from additional medications used to suppress the immune system, or from the engrafted donor hematopoietic cells (e.g., graft-versus-host disease in recipients of allogeneic transplantations) (Ezzone, 2013; Steinberg et al., 2015).
Relying on this anticipated trajectory, three survey administration time points were identified. For baseline measures, time point 1 (T1) surveys were completed prior to hospital admission during the pretransplantation education session. Time point 2 (T2) surveys were completed within nadir, or when the patient’s ANC was less than 500 cells/mcl. Time point 3 (T3) surveys were completed within discharge, or when a patient’s ANC was greater than 1,000 cells/mcl and the patient could theoretically be discharged in the absence of complications or other miscellaneous issues according to institution policy. The time frame for the designated time points varied depending on the type of transplantation, with autologous transplantations occurring in a shorter span of time than allogeneic transplantations. For patients undergoing autologous transplantation, T2 corresponded with hospital day 7 and T3 with hospital day 14. For patients undergoing allogeneic transplantation, T2 took place on hospital day 10 and T3 on hospital day 21. To ensure that the time points accurately captured the predicted change in patient status with the trajectory of the patient’s ANC, a three-day window was allotted in case a patient did not meet blood count criteria for survey administration.
Prior to the accrual period, the principal investigator (PI) met with the transplantation nurse coordinators and IRB-approved study members to discuss and standardize the study procedure. The transplantation nurse coordinators’ responsibility included obtaining informed consent and administering the survey at T1, including the demographic self-reporting survey, the SRHI, the MSAS-SF, and the theory of planned behavior questionnaire. Surveys at T2 and T3 included the MSAS-SF and the theory of planned behavior questionnaire, which were administered by the PI and study team in the patient’s room.
Data Analysis
A descriptive analysis of the sample characteristics, including previous exercise habit, symptom distress, and intentions was generated using IBM SPSS Statistics, version 25.0. For each time point, univariate linear regression was used with the outcomes of total attitude score, total control score, and total norm score and the covariates (also known as predictors) of MSAS-SF total score and subscale scores. Univariate logistic regression was used to model the binary outcome of an intention score of 7 versus an intention score of less than 7 with the covariates total attitude score, total control score, and total norm score at each time point. Alpha was set at 0.05.
Results
Sample Characteristics
A total of 73 patients were screened, and 59 were invited to participate. Of these, 54 consented, resulting in a 92% enrollment rate. This study was done as part of a hospital-based research internship designed to teach clinical nurses the knowledge and skills associated with nursing research. With mentorship from nurse scientists, interns learned about the importance of research, its implications for practice, and development and implementation of a research project. The limiting factors for the sample size in this study were the number of patients actually referred for transplantation at this institution and a finite number of months to complete the study within the research internship. The mean age of the sample was 58.06 years (SD = 12.34). The mean number of months from cancer diagnosis to enrollment was 22.36 (SD = 40.48). Sample characteristics are shown in Table 1. 
Intention to Engage in Physical Activity
Across all three time points, patients undergoing HCT reported high levels of intention to perform physical activity. The mean average intention scores were 6.7 (SD = 0.6), 6.36 (SD = 1.05), and 6.51 (SD = 1.05) at the three respective time points (range = 1–7). Because of the lack of variability in intention scores, the analysis of the relationship between intention and the theoretical constructs of attitude, subjective norm, and perceived control over time shifted to examining the odds of a patient reporting a high intention score—specifically, the odds of a patient reporting an intention score of 7, with the covariates being the theoretical constructs. At T1, greater odds of having an intention score of 7 were significantly associated with higher scores for attitude, subjective norm, and control. For every point increase in a patient’s attitude, subjective norm, and perceived control, the odds of their intention score being 7 increased by 87%, 242%, and 7,685%, respectively. A similar significant association was found at T2. For every point increase in a patient’s attitude, subjective norm, and perceived control, the odds of their intention score being 7 increased by 178%, 182%, and 794%, respectively. Finally, at T3, only a patient’s perceived control toward physical activity had a significant association with a score of 7. Every point increase in a patient’s perceived control score led to an increase in the odds of their intention score being 7 by 1,104%. See Table 2 for the univariate logistic regression models. 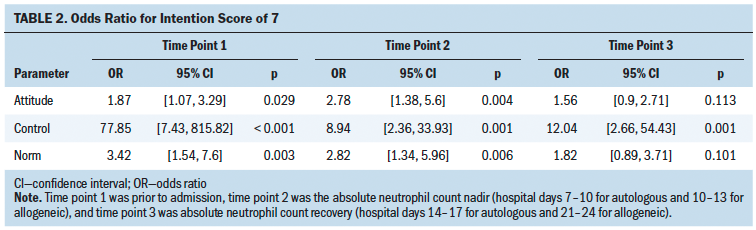
In addition, demographic and medical variables were assessed as predictors for an association of a patient reporting an intention score of 7. Having a college degree versus a high school diploma/GED was the only demographic variable statistically associated with an intention score of 7 at T3. Having a college degree compared to a high school diploma or GED decreased the odds of having an intention score of 7 by 83% (p = 0.02). Medical variables, including type of cancer, type of transplantation, time since diagnosis, relapse status or new diagnosis, and number of previous chemotherapy and radiation therapy treatments were not found to be statically associated for a patient to report an intention score of 7 at any time point.
Previous Exercise Habit
Participants had a mean previous exercise habit score of 3.59 (SD = 1.7) prior to admission. Exercise habit score was not statistically related to intention, subjective norm, attitude, and perceived control measured at T1, T2, or T3. 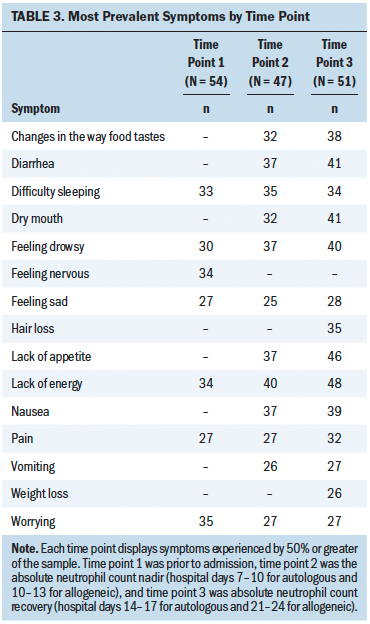
Symptom Distress
Patients reported experiencing a mean of 9.28 symptoms at T1, 14 at T2, and 15.73 at T3. The most prevalent and most distressing symptoms at each time point are listed in Tables 3 and 4, respectively. 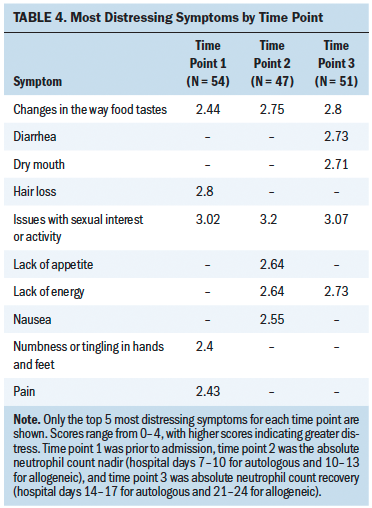
The relationship between symptom distress and the theoretical constructs at each time point were analyzed using univariate linear regression (see Table 5). At T1, greater psychological distress was associated with greater positive impressions in attitude, perceived control, and subjective norm. At T2, greater global distress was significantly associated with less perceived control toward physical activity. At T3, greater psychological and global distress were significantly associated with a less positive attitude toward physical activity, and greater physical and global distress were significantly associated with less perceived control toward physical activity. 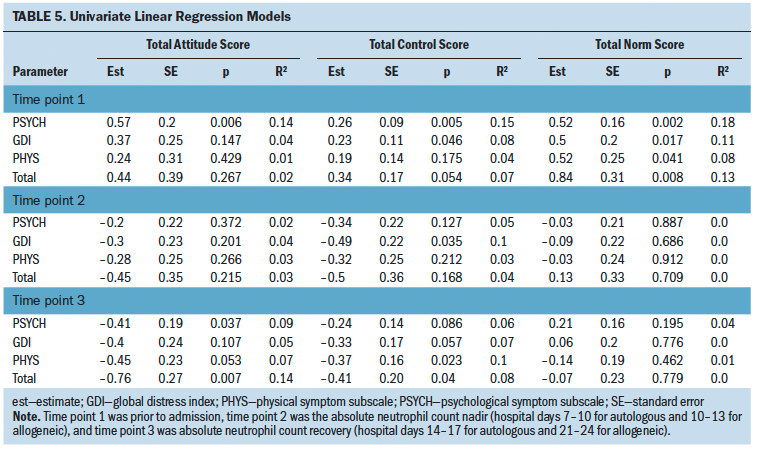
Discussion
In this study, the authors conducted prospective measures of intention to perform physical activity, attitude toward physical activity, perceived control of physical activity, and subjective norm toward physical activity in patients undergoing HCT. Scores were measured at baseline (T1), within nadir (T2), and upon discharge (T3). Patients reported strong intentions to conduct physical activity at all time points, and participants’ perceived control toward physical activity was found to have the strongest odds for having the highest level of intention. However, wide confidence intervals for the odds ratios of perceived control indicate that the models nearly did not converge and lowers the authors’ confidence in the relationship between the perceived control and an intention score of 7. Therefore, a larger sample size is necessary to determine if perceived control is a potential target for intervention. Self-efficacy, which is a related concept to perceived control, refers to the perceived confidence to perform a specific behavior (Glanz et al., 2008). It is possible that the patients in this study had high levels of perceived self-efficacy toward activity during HCT, potentially explaining the lack of variability in intention scores. Although the theory of planned behavior posits that, if a person has the intention to perform the activity, they will do so, nurses should follow through with patients expressing strong intentions for physical activity to make sure that the behavior occurred.
Another important finding in this study was that patients undergoing HCT reported relatively low levels of previous exercise habit prior to transplantation. In addition, exercise habit levels were not significantly associated with intention for physical activity. Therefore, nurses need to consistently reinforce the importance of physical activity for every patient undergoing HCT and not assume that previous exercise habits will translate to physical activity upon admission to the hospital.
Several significant findings related to the description of symptom distress during hospitalization of HCT were found. First, lack of energy was the most prevalent symptom at all time points except at T1, where it was second to worrying. This finding of lack of energy as a frequently experienced symptom is consistent with previous literature (Bevans, Mitchell, & Marden 2008; Cohen et al., 2012). However, El-Jawahri et al. (2015), who measured symptoms of patients undergoing HCT with the Functional Assessment of Cancer Therapy–Bone Marrow Transplantation (FACT-BMT), found insomnia, nausea, bowel trouble, and pain to be the most prevalent symptoms.
Second, issues with sexual interest or activity was found to be the most distressing symptom at all three time points. Changes in the way food tastes and lack of energy were the second and third most distressing symptoms at all time points except at baseline, when only changes in the way food tastes was in the top three. Although there is research that describes the severity or frequency of symptoms experienced during HCT, few studies examine the concept of symptom distress. Cohen et al. (2012) found that the symptoms of fatigue, sleep disturbance, physical weakness, drowsiness, and lack of appetite to be the most severe, but not necessarily most distressing. Declines in sexual activity and function post-HCT regardless of demographic and medical characteristics are well documented (Yi & Syrjala, 2009). More recent literature continues to support sexual dissatisfaction and dysfunction reported by female patients undergoing HCT (Tierney, Palesh, & Johnston, 2015). El-Jawahri et al. (2018) observed that distress from sexual dysfunction commonly affects patients following HCT.
Third, the number of symptoms experienced during the transplantation trajectory is substantial. Prior to admission, patients undergoing HCT reported experiencing a mean average of about nine symptoms. The number of experienced symptoms continued to increase to about 14 at nadir and 16 at discharge. Therefore, patients are leaving the hospital not only with the burden of post-transplantation care, but also experiencing more symptoms than prior to admission. El-Jawahri et al. (2016) found that quality of life and depressive symptoms experienced during a patient’s hospitalization were predictive of future depressive and post-traumatic stress disorder symptoms six months after HCT.
Finally, symptom distress was found to have several significant relationships with the theoretical constructs of attitude, perceived control, and subjective norm toward physical activity. The inverse relationships found between symptom distress and the theoretical constructs at nadir (T2) and discharge (T3) highlight the need for nurses to understand and recognize these critical time points in a patient’s hospitalization regarding potential complications, as well as intention for physical activity.
Limitations
This study used an investigator-developed survey to measure the key constructs of intention, perceived control, subjective norm, and attitude toward physical activity during transplantation. One issue with the survey was the lack of variability among items in each subscale, particularly at T1 and T2. The limited variability found in this study may be because of response bias, such as participants consistently choosing extreme scores regardless of the item or providing scores that are thought to be socially desirable. The lack of variability in intention scores, which was measured with a single item, required conversion to a lower level of measurement using a dichotomous outcome measure of the patient having or not having an intention score of 7.
Further refinement of the survey and psychometric testing are needed to establish reliability and validity of the survey. The challenge faced by the investigators was to balance the number of items for this critically ill population with the need to address methodologic development of a new tool. Each scale consisted of a small number of items that grouped all types of physical activities that a patient can do in the hospital into one question. A greater number of items for each construct with questions that are specific for each type of activity could improve description of each construct and perhaps improve variability in responses. The survey was not burdensome to patients in this study, so lengthening the measurement of each construct would be acceptable.
Generalizability of the study’s findings are limited by use of a convenience sample that was predominantly Caucasian and educated. Another limitation was that the patient’s physical activity was not directly measured because of feasibility and resource constraints. However, the theory of planned behavior provided a theoretical means to estimate whether physical activity would occur (HusebØ, Dyrstad, SØreide, & Bru, 2013).
In addition, missing data occurred at nadir because of refusals. This was anticipated given the nature of transplantation and the symptoms experienced at that time. Finally, the study did not assess actual or perceived environmental factors that may influence a patient’s physical activity.
Implications for Nursing
Although a future larger study is needed to confirm whether a patient’s perceived control toward performing physical activity has the strongest influence on intention, the current findings suggest it could be a potential opportunity for nursing intervention. Giving control back to patients undergoing HCT by way of discussing the plan of care for the day and allowing the patient to choose a time to perform physical activity within the constraints of HCT care (e.g., when safely feasible given the current medical status, to be disconnected from devices and monitors) could improve their sense of control and subsequent intention toward physical activity.
A second and possibly more relevant nursing implication corresponds to the identification of two critical time points during the transplantation trajectory. With the previously identified increase in experienced symptoms throughout the transplantation process and the inverse relationship between symptom distress and a patient’s attitude, control, and subjective norm toward physical activity during nadir and discharge, these two time points require increased attention by nurses. Early recognition of these relationships translates to better control of patient’s symptom distress, improving the theoretical constructs and positively affecting intention for physical activity and possibly additional self-care measures.
In addition to enhanced awareness at nadir and discharge, there are several implications for nursing practice related to the extremely high symptom burden observed in this study, particularly at these two time points. El-Jawahri et al. (2016) identified the predictive ability of depressive symptoms and quality of life during a patient’s hospitalization for HCT to outcomes six months after transplantation. There is a need for comprehensive and systematic assessment of the symptom experience, including symptom distress. Implementation of a validated and reliable symptom distress assessment tool into a nurse’s daily assessment could help capture the patient’s current symptom status and guide intervention.
In addition to identifying a high symptom burden at nadir and discharge, the authors observed that concerns regarding sexuality remain the most distressing symptom reported by patients undergoing HCT at all time points. The symptom remains underdiscussed, underidentified, and underaddressed in the clinical setting and is not exclusive to patients undergoing HCT (Katz, 2007). Compounding this problem, a significant number of healthcare providers in the oncology setting not only identify a level of discomfort when discussing a patient’s sexuality, but also indicate a lack of specific training in this subject (Leonardi-Warren et al., 2016). This highlights the continued need to train nurses in performing an assessment of symptoms and concerns related to sexuality of patients undergoing HCT to recognize these common complaints and facilitate interventions to relieve these symptoms. 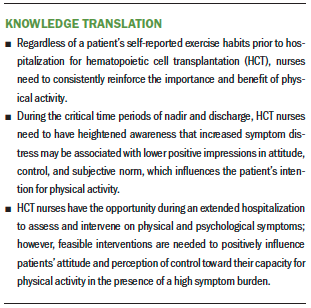
Conclusion
Using the theory of planned behavior as a framework, this longitudinal, prospective, descriptive study identified factors associated with intention for physical activity in patients hospitalized for HCT. Intention for physical activity was not related to previous exercise habit. Patients reported strong intentions for physical activity at all time points, and a patient’s perceived control toward physical activity was found to have the strongest odds for having the highest level of intention. The increase in the number of experienced symptoms throughout the transplantation course is significant. Issues with sexual interest or activity was identified as the most distressing symptom to patients, regardless of patient’s status in the transplantation process. Preliminary evidence was found of inverse relationships between symptom distress and the theoretical constructs of attitude, perceived control, and subjective norm at nadir and discharge. Further development and psychometric testing of the investigator-constructed survey is needed to confirm these relationships and identify potential targets for interventions to increase physical activity in patients with a high symptom burden. [[{"fid":"53741","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
About the Author(s)
Samantha M. Kolke, BSN, RN, BMTCN®, is an advanced clinical nurse; Megan Kuhlenschmidt, MSN, CNP, OCN®, is a nurse practitioner, and Erica Bauer, BSN, RN, BMTCN®, is an assistant head nurse, both at the Seidman Cancer Center, all at the University Hospitals Cleveland Medical Center; Mary K. Anthony, PhD, RN, is the director of nursing research at the University Hospitals Cleveland Medical Center and a professor and associate dean of research in the College of Nursing at Kent State University; Haley Gittleman, MS, is a biostatistician in the Case Comprehensive Cancer Center and Paolo F. Caimi, MD, is an associate professor in the Division of Hematology and Oncology, both in the School of Medicine at Case Western Reserve University in Cleveland; and Susan R. Mazanec, PhD, RN, AOCN®, is an assistant professor in the Frances Payne Bolton School of Nursing at Case Western Reserve University and a nurse scientist in the Seidman Cancer Center at the University Hospitals Cleveland Medical Center, all in Ohio. No financial relationships to disclose. Kolke, Anthony, Caimi, and Mazanec contributed to the conceptualization and design. Kolke, Kuhlenschmidt, and Bauer completed the data collection. Kolke, Gittelman, and Mazanec provided statistical support and analysis. Kolke, Kuhlenschmidt, Anthony, Gittelman, Caimi, and Mazanec contributed to the manuscript preparation. Kolke can be reached at samanthakolke@gmail.com, with copy to ONFEditor@ons.org. (Submitted February 2019. Accepted June 20, 2019.)
References
Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179–211. https://doi.org/10.1016/0749-5978(91)90020-T
Bevans, M.F., Mitchell, S.A., & Marden, S. (2008). The symptom experience in the first 100 days following allogeneic hematopoietic stem cell transplantation (HSCT). Supportive Care in Cancer, 16, 1243–1254. https://doi.org/10.1007/s00520-008-0420-6
Caspersen, C.J., Powell, K.E., & Christenson, G.M. (1985). Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Reports, 100, 126–131.
Chang, V.T., Hwang, S.S., Feuerman, M., Kasimis, B.S., & Thaler, H.T. (2000). The Memorial Symptom Assessment Scale Short Form (MSAS-SF). Cancer, 89, 1162–1171.
Cohen, M.Z., Rozmus, C.L., Mendoza, T.R., Padhye, N.S., Neumann, J., Gning, I., . . . Cleeland, C.S. (2012). Symptoms and quality of life in diverse patients undergoing hematopoietic stem cell transplantation. Journal of Pain and Symptom Management, 44, 168–180. https://doi.org/10.1016/j.jpainsymman.2011.08.011
El-Jawahri, A., Fishman, S.R., Vanderklish, J., Dizon, D.S., Pensak, N., Traeger, L., . . . Temel, J.S. (2018). Pilot study of a multimodal intervention to enhance sexual function in survivors of hematopoietic stem cell transplantation. Cancer, 124, 2438–2446. https://doi.org/10.1002/cncr.31333
El-Jawahri, A., Traeger, L., Kuzmuk, K., Eusebio, J., Gallagher, E., VanDusen, H., . . . Temel, J. (2014) Physical and psychological symptom burden and prognostic understanding during hospitalization for hematopoietic stem cell transplantation. Biology of Blood and Marrow Transplantation, 20(Suppl.), S193. https://doi.org/10.1016/j.bbmt.2013.12.319
El-Jawahri, A.R., Traeger, L.N., Kuzmuk, K., Eusebio, J.R., Vandusen, H.B., Shin, J.A., . . . Temel, J.S. (2015). Quality of life and mood of patients and family caregivers during hospitalization for hematopoietic stem cell transplantation. Cancer, 121, 951–959. https://doi.org/10.1002/cncr.29149
El-Jawahri, A.R., Vandusen, H.B., Traeger, L.N., Fishbein, J.N., Keenan, T., Gallagher, E.R., . . . Temel, J.S. (2016). Quality of life and mood predict posttraumatic stress disorder after hematopoietic stem cell transplantation. Cancer, 122, 806–812. https://doi.org/10.1002/cncr.29818
Ezzone, S.A. (2013). Hematopoietic stem cell transplantation: A manual for nursing practice (2nd ed.). Pittsburgh, PA: Oncology Nursing Society.
Fishbein, M., & Ajzen, I. (2010). Predicting and changing behavior: The reasoned action approach. New York, NY: Psychology Press.
Glanz, K., Rimer, B.K., & Viswanath, K. (2008). Health behavior and health education: Theory, research, and practice. San Francisco, CA: John Wiley and Sons.
Husebø, A.M., Dyrstad, S.M., Søreide, J.A., & Bru, E. (2013). Predicting exercise adherence in cancer patients and survivors: A systematic review and meta-analysis of motivational and behavioural factors. Journal of Clinical Nursing, 22(1–2), 4–21. https://doi.org/10.1111/j.1365-2702.2012.04322.x
Jacobsen, P.B., Le-Rademacher, J., Jim, H., Syrjala, K., Wingard, J.R., Logan, B., . . . Lee, S.J. (2014). Exercise and stress management training prior to hematopoietic cell transplantation: Blood and Marrow Transplant Clinical Trials Network (BMT CTN) 0902. Biology of Blood and Marrow Transplantation, 20, 1530–1536. https://doi.org/10.1016/j.bbmt.2014.05.027
Katz, A. (2007). Breaking the silence on cancer and sexuality: A handbook for healthcare providers. Pittsburgh, PA: Oncology Nursing Society.
Leonardi-Warren, K., Neff, I., Mancuso, M., Wenger, B., Galbraith, M., & Fink, R. (2016). Sexual health: Exploring patient needs and healthcare provider comfort and knowledge [Online exclusive]. Clinical Journal of Oncology Nursing, 20, E162–E167. https://doi.org/10.1188/16.CJON.E162-E167
McClement, S.E., Woodgate, R.L., & Degner, L. (1997). Symptom distress in adult patients with cancer. Cancer Nursing, 20, 236–243.
Mitchell, S.A., Hoffman, A.J., Clark, J.C., DeGennaro, R.M., Poirier, P., Robinson, C.B., & Weisbrod, B.L. (2014). Putting evidence into practice: An update of evidence-based interventions for cancer-related fatigue during and following treatment. Clinical Journal of Oncology Nursing, 18(Suppl. 3), 38–58. https://doi.org/10.1188/14.CJON.S3.38-58
Oberoi, S., Robinson, P.D., Cataudella, D., Culos-Reed, S.N., Davis, H., Duong, N., . . . Sung, L. (2018). Physical activity reduces fatigue in patients with cancer and hematopoietic stem cell transplant recipients: A systematic review and meta-analysis of randomized trials. Critical Reviews in Oncology/Hematology, 122, 52–59. https://doi.org/10.1016/j.critrevonc.2017.12.011
Rock, C.L., Doyle, C., Demark-Wahnefried, W., Meyerhardt, J., Courneya, K.S., Schwartz, A.L., . . . Gansler, T. (2012). Nutrition and physical activity guidelines for cancer survivors. CA: A Cancer Journal for Clinicians, 62, 243–274. https://doi.org/10.3322/caac.21142
Steinberg, A., Asher, A., Bailey, C., & Fu, J.B. (2015). The role of physical rehabilitation in stem cell transplantation patients. Supportive Care in Cancer, 23, 2447–2460. https://doi.org/10.1007/s00520-015-2744-3
Tierney, D.K., Palesh, O., & Johnston, L. (2015). Sexuality, menopausal symptoms, and quality of life in premenopausal women in the first year following hematopoietic cell transplantation. Oncology Nursing Forum, 42, 488–497. https://doi.org/10.1188/15.ONF.488-497
Verplanken, B., & Orbell, S. (2003). Reflections on past behavior: A self-report index of habit Strength. Journal of Applied Social Psychology, 33, 1313–1330. https://doi.org/10.1111/j.1559-1816.2003.tb01951.x
Webber, K., & Davies, A.N. (2011). Validity of the Memorial Symptom Assessment Scale–Short Form psychological subscales in advanced cancer patients. Journal of Pain and Symptom Management, 42, 761–767. https://doi.org/10.1016/j.jpainsymman.2011.02.007
Yi, J.C., & Syrjala, K.L. (2009). Sexuality after hematopoietic stem cell transplantation. Cancer Journal, 15, 57–64. https://doi.org/10.1097/PPO.0b013e318198c758




