SEEK™: A Program to Implement Evidence-Based Practice and Transform Oncology Nursing Practice
Background: Evidence-based practice (EBP) uses current and best evidence, clinical expertise, and patient values to drive clinical decisions. Organizations struggle with building and sustaining an EBP-focused culture.
Objectives: This article shares the development and implementation of SEEK™ (Spirit of Inquiry, Expanding EBP Knowledge), an educational initiative on how to apply EBP processes at a Magnet®- and National Cancer Institute– designated comprehensive cancer center.
Methods: Participants learned principles of the EBP process using didactic sessions, small group exercises, and article critiques. With mentor guidance, participants searched for and appraised evidence, proposed interventions, designed an implementation plan, and developed metrics to measure results.
Findings: To date, 56 SEEK projects are in various stages of development and implementation. Based on postprogram survey results, SEEK participants and mentors demonstrated increased EBP knowledge.
Jump to a section
Earn free contact hours: Click here to connect to the evaluation. Certified nurses can claim no more than 1 total ILNA point for this program. Up to 1 ILNA point may be applied to Nursing Practice OR Oncology Nursing Practice OR Professional Practice/Performance. See www.oncc.org for complete details on certification.
Evidence-based practice (EBP) is a problem-solving process that employs the current best evidence from studies and patient care data with clinician expertise as well as patient preferences and values to guide healthcare decisions (Melnyk et al., 2010; Titler, 2008). The EBP process includes the following five basic steps: (a) Identify a clinical inquiry, (b) acquire current best evidence through an unbiased search strategy, (c) appraise and synthesize the evidence for its worthiness and value, (d) apply the evidence to clinical practice, and (e) evaluate the effectiveness of the outcomes (American Nurses Association, n.d.). Using EBP to problem-solve clinical inquiries aligns with organizational values and missions to ensure excellence in cancer care and administer state-of-the-art treatments consistent with the latest research and technology (Speroni et al., 2020). A survey of chief nursing executives by Melnyk et al. (2016) revealed that despite hospitals’ low performance in key metrics, EBP remains a low priority because of financial constraints.
Li et al. (2019) performed a systematic review of knowledge, attitudes, implementation, facilitators, and barriers of EBP. The study identified that time and resources are barriers to EBP for staff nurses, and suggested organizations invest in resources (e.g., nursing workforce, mentorship to facilitate EBP initiatives to align with the organization’s values and mission) that are attainable for nurses at the bedside and are applied to real-time clinical scenarios (Li et al., 2019). The review found that there is a focus on the cultivation of EBP knowledge but not implementation (Li et al., 2019), and suggested that EBP initiatives are carried out by administrators who possess more authority and the ability to coordinate efforts. Ironically, younger, less experienced staff appeared more knowledgeable about EBP because of their academic training (Li et al., 2019). To create a sustainable and effective EBP environment, organizations can reconcile barriers with an investment in resources, nursing workforce, and mentorship. This facilitates EBP initiatives that are (a) aligned with the organization’s values and mission, (b) attainable for nurses at the bedside, and (c) applicable to real-time clinical scenarios.
In a descriptive study of 284 nurses from 50 primary healthcare centers in Saudi Arabia, Alqahtani et al. (2022) examined nurses’ perceived barriers to implementing EBP. The three most frequently reported barriers were that (a) results are not generalizable to their own setting, (b) physicians will not cooperate with implementation, and (c) facilities are inadequate for implementation. In their qualitative, descriptive study exploring the implementation of EBP in public hospitals in the Amhara Region of Ethiopia, 86 nurses and midwives participated in in-depth interviews (Dagne & Beshah, 2021). Similar to Algahtani et al. (2022) and Li et al. (2019), Dagne and Beshah (2021) found that limited organizational support in the form of time mismanagement, lack of resources and training, and lack of motivation to question traditional practices were key barriers to EBP implementation. The literature consistently describes the importance of EBP and offers similar barriers to implementation (Alqahtani et al., 2022; Dagne & Beshah, 2021; Mahmoud & Mohamed Abdelrasol, 2019; Yoo et al., 2019).
Based on a literature review, researchers have yet to describe the operational effectiveness and sustainability of EBP implementation with a clear infrastructure to enculturate EBP within an entire organization. SEEK™ (Spirit of Inquiry, Expanding EBP Knowledge) is a program developed by Memorial Sloan Kettering Cancer Center in New York, New York, to operationalize and perpetuate an EBP-focused culture throughout the Magnet®- and National Cancer Institute–designated comprehensive cancer center. It is designed to (a) teach EBP methodology to oncology nurses and interprofessional partners, (b) appraise and synthesize evidence, (c) implement recommendations, and (d) evaluate changes with metrics. SEEK empowers and supports oncology nurses to demonstrate exemplary professional practice and transform the organization by applying new knowledge and evidence to oncology nursing practice.
Purpose
This article describes the development, implementation, and dissemination of the SEEK program. It also illustrates how SEEK has increased oncology nurses’ EBP knowledge and skills while providing a structure to implement EBP to establish standards of oncology nursing practice and improve outcomes in patients with cancer.
Methods
Operational Structure
Oncology certified nurses with advanced degrees developed the SEEK program to educate and support staff nurses on the steps of the EBP process. To support this initiative, the institution’s department of nursing established an EBP Steering Committee to oversee the SEEK program. An EBP nursing specialist within the Department of EBP served as the program manager and oversaw all aspects of SEEK to ensure there was no duplication of efforts, optimized available resources, and facilitated the success of projects. The program manager scheduled the didactic sessions and workshops and matched participants with a mentor. With the members of the EBP Steering Committee, the program manager oversaw curriculum development for SEEK and its supporting programs and provided support for SEEK mentors.
SEEK cohorts are held twice per year and consist of 10–12 participant groups. Participants apply to the SEEK program with a clinical inquiry relevant to oncology practice, based on the program’s philosophy that all levels of clinicians have an important role in detecting inconsistencies, questioning current practices, and identifying changing trends. The program manager evaluates the potential topics with participants based on the priority and feasibility of the project, as well as the endorsement of the applicant and project by their direct supervisor, who grants paid in-service or meeting days to allow the participant to attend. The clinical inquiry then becomes their SEEK project.
Teaching Strategies
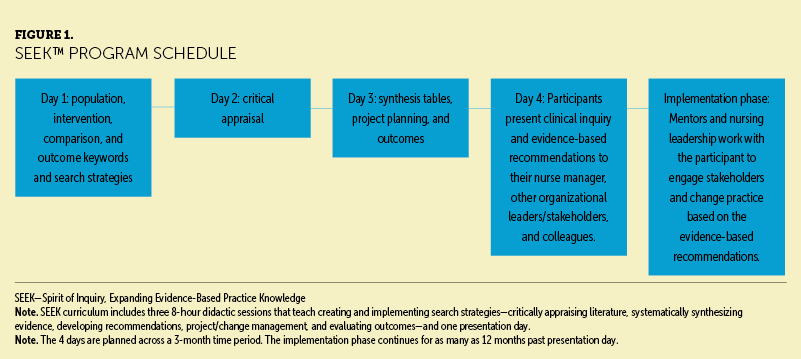
Participation in the SEEK program requires attending three virtual eight-hour didactic sessions and one presentation day. The didactic sessions teach creating and implementing search strategies, critically appraising literature, systematically synthesizing evidence, developing recommendations, managing projects or changes, and evaluating metrics (see Figure 1). Classes and assigned self-directed work are spaced over 12 weeks to allow participants time to apply the knowledge learned and demonstrate understanding in phases congruent with a predicted timeline for steady progress.
SEEK began in a virtual format in 2021 during the COVID-19 pandemic, which demonstrated the use of technology at a time when it was not solely used for nursing education programs at this institution. The program relies on teach-back methodology to facilitate learning and avoids common challenges associated with remote learning, such as distraction, lack of concentration, disconnect from teachers and peers, and loss of focus (Tulaskar & Turunen, 2022). Teach-back methodology is an evidence-based communication strategy that charges the person teaching with ensuring that the learner can verbalize and demonstrate their own understanding (Anderson et al., 2020). For example, participants learn how to develop population, intervention, comparison, and outcome keywords to create successful search terms. The participants generate these keywords and search strategies for their topics and then submit them onto a virtual whiteboard. All entries are reviewed and critiqued by fellow participants in the cohort who can comment and provide feedback to the whiteboard on how the submissions could be improved. To date, the SEEK program has continued as a virtual course because of the ability to include staff from all sites in the organization.
Project Implementation
Participants present their initial clinical inquiry and final evidence-based recommendations on the fourth and last day of the SEEK program to their nurse manager, other organizational leaders or stakeholders, and colleagues. The project then moves into the implementation phase, during which mentors and nursing leadership strategize with the participant to engage stakeholders, change practice based on the evidence-based recommendations, and determine appropriate metrics to measure success. Depending on the nature of the practice change, the group determines whether the project requires human subject review from the institutional review board. Six-month and one-year postpresentation check-ins are scheduled with all participants and mentors to follow up on the project’s implementation progress and readiness for dissemination.
An annual conference is held to showcase SEEK participants and their projects within and outside the organization. Upon completion of their SEEK projects, participants are advanced to a publishing workshop, which pairs nurses with a publishing mentor. The publishing workshop teaches novice writers how to write an outline, abstract, query letter, and article for a peer-reviewed journal.
Program Support
The ability to provide all participants with mentorship is unique and key to the program’s success. There are currently more than 50 mentors trained to be paired with participants. Potential mentors must have received EBP training (through SEEK or another formal EBP education program) and are first identified based on prior involvement in a successful EBP project, in which passion and excitement for the application of the methodology was observed. These individuals are sought out and asked to become a co-mentor for the SEEK program. Co-mentors are mentors in training and work with a mentor to develop their knowledge and skills related to teaching EBP and providing feedback to participants.
Mentors are paired with only one mentee or a group of as many as three mentees working on the same topic. Close attention is paid to mentor/co-mentor participant assignments; mentors and co-mentors are intentionally not matched with topics about which they have a great amount of knowledge to avoid unconscious bias. There is also an effort to pair individuals who normally do not work together to increase networking opportunities for all those involved in the program. Mentors work with their paired participant(s) between sessions to guide them through the complex skills of appraising relevant evidence and developing recommendations and metrics for evaluation for a real-time clinical scenario. After SEEK presentation day, participants continue to work with mentors to complete project implementation, evaluation of metrics, and publishing.
Ongoing mentor growth and development ensures the sustainability of the program. The EBP Steering Committee recognized the need for the SEEK program to continuously grow and sustain new talent, and created additional programs to support the development of new mentors and refine learned skills. Examples of these supplemental programs include a mentorship workshop to develop new mentors and a monthly journal club to provide a forum for mentors and staff to improve skills and practice verbalizing their knowledge within a small group.
Beyond their involvement with SEEK, there is an expectation for mentors to rotate teaching the monthly staff beginner-level EBP classes, which include a 90-minute introduction to the EBP course and/or a 90-minute critical appraisal workshop. It is also the mentors’ responsibility to participate in monthly journal clubs, when available, and abstract reviews for the annual conference, as needed. These additional opportunities are creative strategies to increase the range of the mentors. This development plan gives mentors access to improve their knowledge and skills and provides them with structured formats and tasks to ensure the continued practice of EBP.
Program Survey
EBP Steering Committee members developed a knowledge assessment that was administered pre- and post-SEEK. The preassessment survey was administered prior to beginning the program; the postassessment survey was given after the presentation day (day 4). The survey includes 3 questions measuring the participants’ self-rated knowledge and desire to use EBP in daily practice and 27 questions to determine their actual EBP knowledge or skill (e.g., components of a search strategy, database selection, critical appraisal terms). For self-rated knowledge, participants and mentors were asked to rate their knowledge of the EBP process on a Likert-type scale ranging from 0 (very low) to 5 (very high). Knowledge ratings of “high” or “very high” were considered positive responses.
Results
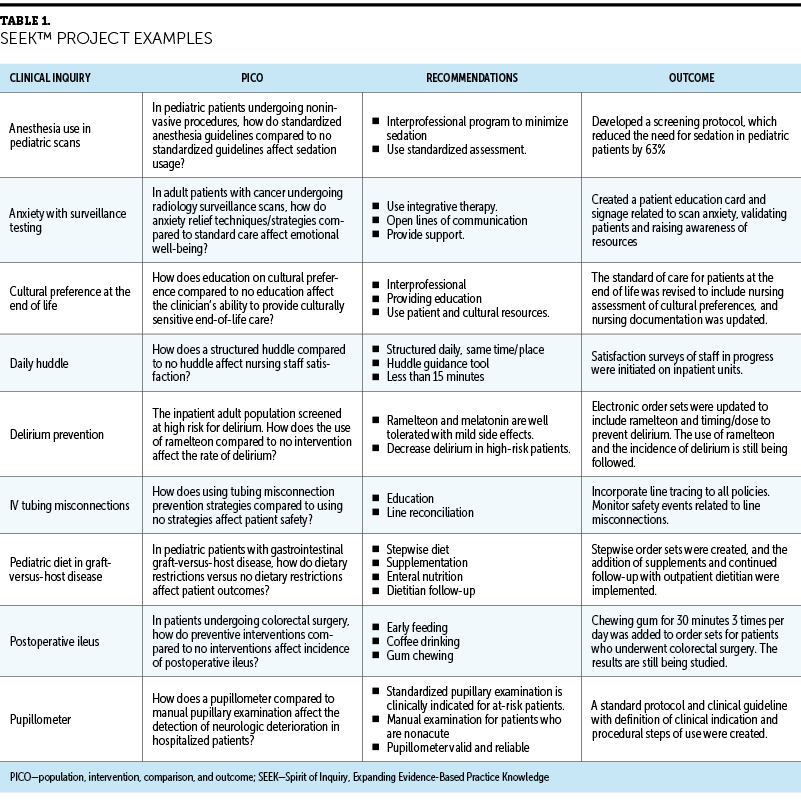
Since its inception in spring 2021, five cohorts have completed the program and 56 SEEK projects have been initiated, 45 of which are in the implementation process. Although many of the EBP initiatives’ outcomes are preliminary, the benefits of the SEEK program are visible on multiple levels. Some of the SEEK initiatives have led to policy and practice changes, whereas others have supported current practices (see Table 1).
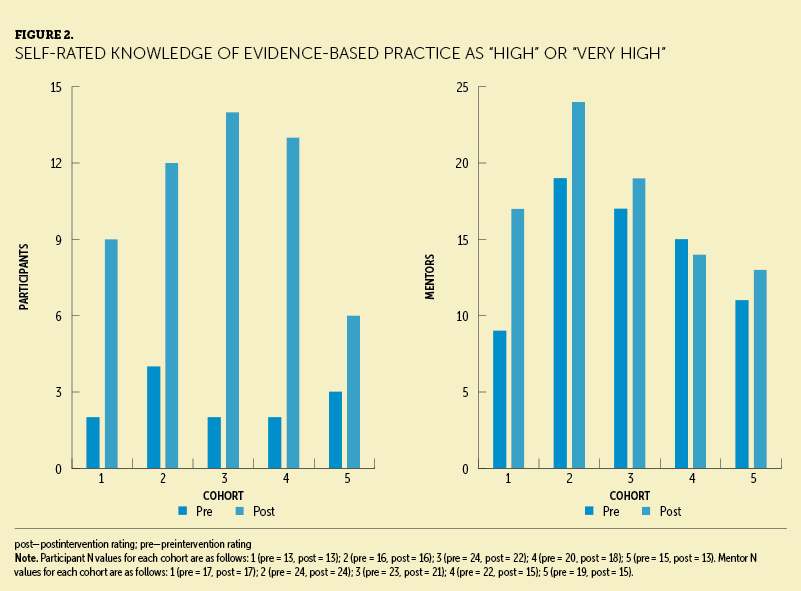
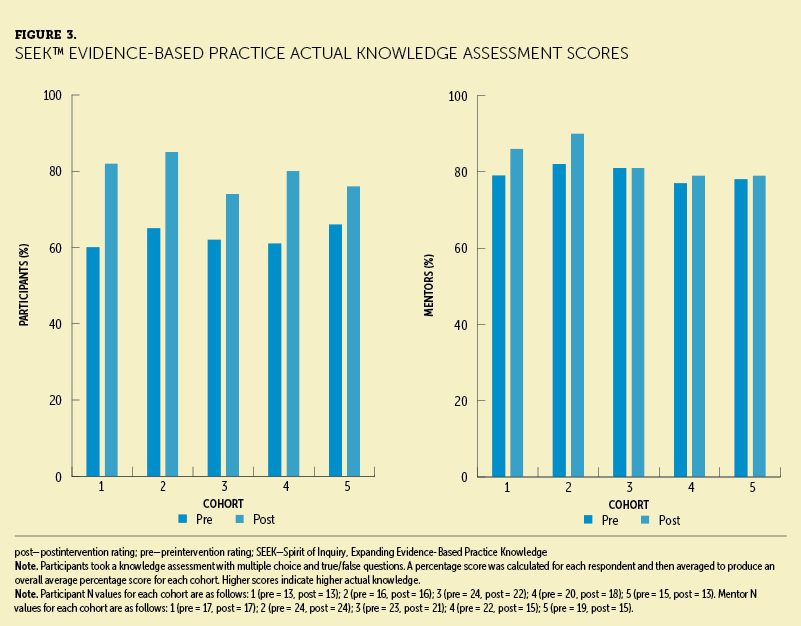
In addition to patient outcomes, the SEEK team measured clinical nurses’ professional growth and development. The self-rated knowledge scores for participants and mentors demonstrated a meaningful increase after participating in the SEEK program (see Figure 2). Scores from the actual EBP knowledge or skill questions validated self-rated learning, with significant improvement in scores for mentors and co-mentors (see Figure 3).
Discussion
The first two cohorts of SEEK were exclusive to nurses. However, interprofessional colleagues expressed interest, and the EBP Steering Committee quickly realized the importance of integrating varied colleagues into the program to foster collaboration. This builds relationships that foster the success of projects and further enculturates the EBP philosophy into the organization. Of 84 total participants across the 5 SEEK cohorts, 19 have been non-nurses, with members from the rehabilitation medicine, pharmacy, food and nutrition, and surgery departments. Several interprofessional colleagues champion EBP methodology in their departments and serve as mentors. The interest in and expansion of this nursing practice program to clinicians outside the department of nursing validates the program and shows how nurses can be leaders in the organizational enculturation of EBP.
SEEK demonstrates creative teaching techniques, strong interprofessional collaborations, and the development and use of mentors. A critical mass of EBP mentors is necessary to increase EBP competency and to implement and support an EBP-focused culture (Melnyk et al., 2021). Of note, Melnyk et al. (2021) reported that EBP-focused culture and mentorship positively affect nurse job satisfaction and retention. The SEEK program demonstrated a benefit for not only participants but also for the mentors and co-mentors in terms of continued learning.
As EBP takes hold within organizations, sharing the results of such initiatives provides value to others across the healthcare continuum, reducing redundancy in clinical inquiry (Dean et al., 2021). Since the inception of SEEK, the value from the projects can also be measured by the response from the oncology nursing community at large. Twelve SEEK participants have had their work accepted to national conferences for poster or podium presentations. Three articles have been accepted for publication and nine others are in progress within the SEEK publishing workshop. Two SEEK projects received grant money to fund the work.
At the authors’ organization, EBP is now the cornerstone of all shared governance meeting discussions and is embedded in the clinical advancement program, policies, procedures, and job descriptions of all nurses. This is in alignment with previous studies that confirmed that EBP is the foundation for high-quality care and promoted its inclusion in new nurse onboarding, job descriptions, clinical ladders, and yearly performance appraisals for success (Melnyk et al., 2017, 2021).
Limitations
SEEK implementation has several limitations. An initial limitation was mentorship availability. SEEK started with a small number of nurses trained and experienced in EBP who were used for mentoring the initial cohort in addition to taking part in their unit-based mentorship activities. In many cases, they were asked to teach the class content as well. This mandated a robust mentorship development program, placing additional burdens on a heavily used resource. Another limitation was staff knowledge of technology. Staff with varying technology skills needed to be considered, and preprogram technology sessions were added to best prepare participants with platform navigation and associated technological skill checks. An additional limitation was the time for staff to attend the sessions and complete the work needed for project implementation; the use of signed endorsement forms collected before the course by participants and leaders enforced the time needed and ensured support.
Implications for Nursing
Using evidence to guide healthcare practices and decisions is heavily supported in the literature (Li et al., 2019; Melnyk et al., 2021; Speroni et al., 2020); however, many institutions struggle to embed EBP into practice. Leaders can ensure nurses at all levels are educated and engaged in the EBP process (Speroni et al., 2020). Training leaders and staff about EBP is a large investment for any organization, but it is the ability to develop, sustain, and measure the return on investment with the continued generation of new knowledge, innovations, and improvements that has been challenging.
SEEK provides education and guidance within an organized structure to enable oncology nurses and interprofessional colleagues to fulfill the organization’s mission to use innovation to have a lasting, positive impact on the care of patients with cancer. The concrete strategic interventions within SEEK have built a solid infrastructure for the enculturation of EBP in the clinical setting. This program showcases how frontline nurses can apply the knowledge learned in a classroom and translate it to enhance patient care.
Creating an evidence-based forum and empowering clinical nurses to learn and embrace it is a worthy endeavor because it supports effective problem-solving, ultimately leading to better practices. This program, created by oncology nurses, can be duplicated within healthcare venues of various sizes that have a shared goal to transform the organization into an environment where practice constantly evolves based on new, evidence-based recommendations. The future of SEEK is to continue with biannual cohorts, including a leadership cohort focused on topics of operational priority, and to disseminate the many outcomes revealed through staff initiatives.
Conclusion
Many institutions have initiated a journey to EBP by attending initial trainings and gaining an understanding of the importance and value of EBP. However, preliminary knowledge and education about EBP does not always translate to skills on how to embed EBP within a clinical organization. SEEK is a creative strategy that promotes a spirit of inquiry by having clinical nurses question the status quo. It is unique in its structure, using multiple learning tools and mentorship to answer staff-selected practice inquiries. The program promotes individual professional growth and contributes to the enhancement of oncology nursing practice. Individual projects demonstrate cost avoidance by imploring less expensive EBPs and a return on investment by using best practices, highlighting the very essence of EBP.
The authors gratefully acknowledge Memorial Sloan Kettering executive leadership, the Evidence-Based Practice Steering Committee, and all the evidence-based practice mentors for their invaluable help in development, implementation and sustainment of the SEEK program.
About the Authors
Ashley Hole, DNP, FNP-BC, CPON®, EBP-C, is the program manager of evidence-based practice, Keri Wagner, DNP, RN, FNP-C, OCN®, EBP-C, is a nurse leader, and Lisa M. Wall, PhD, RN, CNS, AOCNS®, HEC-C, and Mary Elizabeth Davis, DNP, RN, CHPN®, AOCNS®, are clinical nurse specialists, all at Memorial Sloan Kettering Cancer Center in New York, NY. The authors take full responsibility for this content and did not receive honoraria or disclose any relevant financial relationships. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Hole can be reached at holea@mskcc.org, with copy to CJONEditor@ons.org. (Submitted May 2023. Accepted August 31, 2023.)
References
Alqahtani, J.M., Carsula, R.P., Alharbi, H.A., Alyousef, S.M., Baker, O.G., & Tumala, R.B. (2022). Barriers to implementing evidence-based practice among primary healthcare nurses in Saudi Arabia: A cross-sectional study. Nursing Reports, 12(2), 313–323.
American Nurses Association. (n.d.). What is evidence-based practice in nursing? https://www.nursingworld.org/practice-policy/nursing-excellence/evidenc…
Anderson, K.M., Leister, S., & De Rego, R. (2020). The 5Ts for teach back: An operational definition for teach-back training. Health Literacy Research and Practice, 4(2), e94–e103. https://doi.org/10.3928/24748307-20200318-01
Dagne, A.H., & Beshah, M.H. (2021). Implementation of evidence-based practice: The experience of nurses and midwives. PLOS ONE, 16(8), e0256600. https://doi.org/10.1371/journal.pone.0256600
Dean, J., Gallagher-Ford, L., & Connor, L. (2021). Evidence-based practice: A new dissemination guide. Worldviews on Evidence-Based Nursing, 18(1), 4–7.
Li, S., Cao, M., & Zhu, X. (2019). Evidence-based practice: Knowledge, attitudes, implementation, facilitators, and barriers among community nurses—Systematic review. Medicine, 98(39), e17209. https://doi.org/10.1097/MD.0000000000017209
Mahmoud, M.H., & Mohamed Abdelrasol, Z.F. (2019). Obstacles in employing evidence-based practice by nurses in their clinical settings: A descriptive study. Frontiers of Nursing, 6(2), 123–133. https://doi.org/10.2478/FON-2019-0019
Melnyk, B.M., Fineout-Overholt, E., Giggleman, M., & Choy, K. (2017). A test of the ARCC© model improves implementation of evidence-based practice, healthcare culture, and patient outcomes. Worldviews on Evidence-Based Nursing, 14(1), 5–9.
Melnyk, B.M., Fineout-Overholt, E., Stillwell, S.B., & Williamson, K.M. (2010). Evidence-based practice: Step by step: The seven steps of evidence-based practice. American Journal of Nursing, 110(1), 51–53. https://doi.org/10.1097/01.naj.0000366056.06605.d2
Melnyk, B.M., Gallagher-Ford, L., Thomas, B.K., Troseth, M., Wyngarden, K., & Szalacha, L. (2016). A study of chief nurse executives indicates low prioritization of evidence-based practice and shortcomings in hospital performance metrics across the United States. Worldviews on Evidence-Based Nursing, 13(1), 6–14. https://doi.org/10.1111/wvn.12133
Melnyk, B.M., Tan, A., Hsieh, A.P., & Gallagher-Ford, L. (2021). Evidence-based practice culture and mentorship predict EBP implementation, nurse job satisfaction, and intent to stay: Support for the ARCC© model. Worldviews on Evidence-Based Nursing, 18(4), 272–281.
Speroni, K.G., McLaughlin, M.K., & Friesen, M.A. (2020). Use of evidence-based practice models and research findings in Magnet-designated hospitals across the United States: National survey results. Worldviews on Evidence-Based Nursing, 17(2), 98–107. https://doi.org/10.1111/wvn.12428
Titler, M.G. (2008). The evidence for evidence-based practice implementation. In R.G. Hughes (Ed.), Patient safety and quality: An evidence-based handbook for nurses (pp. 1–49). Agency for Healthcare Research and Quality. https://www.ncbi.nlm.nih.gov/books/NBK2659
Tulaskar, R., & Turunen, M. (2022). What students want? Experiences, challenges, and engagement during emergency remote learning amidst COVID-19 crisis. Education and Information Technologies, 27(1), 551–587. https://doi.org/10.1007/s10639-021-10747-1
Yoo, J.Y., Kim, J.H., Kim, J.S., Kim, H.L., & Ki, J.S. (2019). Clinical nurses’ beliefs, knowledge, organizational readiness and level of implementation of evidence-based practice: The first step to creating an evidence-based practice culture. PLOS ONE, 14(12), e0226742. https://doi.org/10.1371/journal.pone.0226742




