The 2014–2018 Oncology Nursing Society Research Agenda
Purpose/Objectives: To identify priority areas of research for the Oncology Nursing Society (ONS) Research Agenda for 2014–2018, consistent with ONS’s mission to promote excellence in oncology nursing and quality cancer care.
Data Sources: Review of the literature, 2013 ONS Research Priorities Survey, National Institute of Nursing Research, and the National Cancer Institute research foci.
Data Synthesis: Multimethod consensus-building approach by content leaders and content experts of the ONS Research Agenda Project Team.
Conclusions: The 2014–2018 Research Agenda Project Team identified eight high-priority research areas: symptoms, late effects of cancer treatment and survivorship care, palliative and end-of-life care, self-management, aging, family and caregivers, improving healthcare systems, and risk reduction. In addition, four cross-cutting themes were identified: biomarkers, bioinformatics, comparative effectiveness research, and dissemination and implementation science.
Implications for Nursing: The Research Agenda is a synthesis of the state of the science in cancer and identifies gaps and directions for the conduct and dissemination of research. Oncology nurses can use the agenda to inform clinical practice, develop research proposals, inform policy makers, support interdisciplinary research efforts, and promote scientist and clinician collaborations in targeted patient-centered research.
Jump to a section
The Oncology Nursing Society (ONS) developed its first Research Agenda in 2001 and has updated the agenda every four years. The dual purpose of the ONS Research Agenda is to determine priority topics for research consistent with the ONS mission to promote excellence in oncology nursing and quality cancer care and to provide the ONS Foundation with the data needed to support the decision-making process for funding oncology nursing research. ONS identified content leaders and experts from the membership for the 2014–2018 Research Agenda Project Team. This team used a multimethod consensus-building approach that was informed by the results of the 2013 ONS Research Priorities Survey (Lobiondo-Wood et al., 2014), a comprehensive literature review, and a review of the national priorities for cancer and nursing research (see Figure 1). Since 2001, the ONS research priorities have reflected the disciplinary perspective of nursing and the mission of ONS. Management of physical and psychological symptoms, health promotion, patient and caregiver issues, end-of-life care, survivorship, and healthcare delivery systems have consistently shaped the Research Agenda. Dynamic progress in understanding the biology of cancer and identification of targets for therapeutic interventions have resulted in the widespread concept of personalized medicine to treat cancer. An understanding of both inter-patient variability and biologic mechanisms are equally important to interpretation of patient responses and to the development and testing of interventions. The increasing national emphasis on evidence-based practice and patient-centered care, as identified by Institute of Medicine reports related to cancer care and the Patient-Centered Outcomes Research Institute, further support the research areas and cross-cutting themes. The 2014–2018 Research Agenda Project Team identified eight high-priority research areas: symptoms, late effects of cancer treatment and survivorship care, palliative and end-of-life care, self-management, aging, family and caregivers, improving the healthcare systems, and risk reduction, as well as four cross-cutting themes: biomarkers, bioinformatics, comparative effectiveness research, and dissemination and implementation science.
The data supporting these research areas were summarized in the form of a draft agenda and posted on the ONS website in the fall of 2014 for public comment. Comments from the members were reviewed by the content leaders and content experts of the Research Agenda Project Team and revised for a final Research Agenda draft that was forwarded to the ONS Board of Directors. The Research Agenda was approved by the ONS Board of Directors in October 2014 and is available on the ONS website as a complete report (ONS, 2015a), and an Executive Summary (ONS, 2015b). The purpose of this article is to disseminate the findings from the Executive Summary to inform the ONS membership and the larger interdisciplinary oncology community.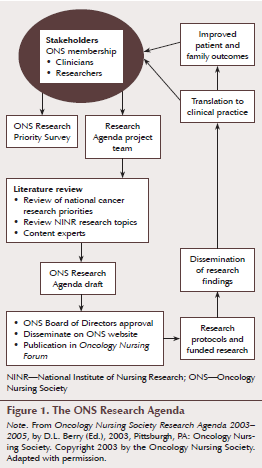
The Oncology Nursing Society’s 2014–2018 Research Priority Areas
A. Symptoms
• Evaluate interventions that integrate symptom management into systems of care and their efficacy on outcomes of care, which includes symptom control, quality of life, and costs of care.
• Examine the underlying biobehavioral mechanisms for individual and co-occurring symptoms and test mechanistic hypotheses within the context of intervention research.
• Determine factors associated with racial or ethnic disparities in symptom severity and develop and evaluate interventions that address these disparities.
1. Fatigue
• Explore motivational factors and barriers to increase the uptake of interventions.
• Disseminate exercise interventions in community settings.
• Gain a better understanding of the underlying biologic mechanisms associated with fatigue.
• Examine whether combining nonpharmacologic and pharmacologic approaches enhances the effects of individual treatments.
2. Pain
• Implement systems-level interventions that promote uptake of evidence-based pain management.
• Understand factors associated with racial disparities and the undertreatment of pain and evaluate interventions that address disparities.
3. Sleep disturbances
• Focus on other homogeneous groups of patients other than women with breast cancer (e.g., men, older adults).
• Determine optimal dose, frequency, and duration of interventions.
• Compare various treatments to determine the most effective approaches to decrease sleep disturbances.
4. Symptom clusters
• Develop a taxonomy of symptom clusters that can guide future intervention studies.
• Understand the underlying biobehavioral mechanisms associated with symptom clusters.
• Include more racially diverse samples of patients to test interventions.
5. Cancer- and cancer treatment–related cognitive impairment
• Identify sensitive and clinically useful cognitive assessment measures.
• Identify risk factors (e.g., demographic, treatment, genetic factors) of post-treatment cognitive decline because only a subset of patients experience long-term cognitive changes.
• Develop longitudinal studies that examine cognitive changes in context to age-related decline to thoroughly understand their implications.
• Develop translational evidence-based interventions to address cognitive performance and enhance coping with cognitive changes.
6. Chemotherapy-induced peripheral neuropathy (CIPN)
• Identify well-validated, reliable, and clinically useful assessment measures of CIPN, including physiological markers.
• Identify risk factors for patients with severe and/or irreversible CIPN symptoms.
• Develop evidence-based pharmacologic and non-pharmacologic treatment options.
7. Psychological distress
• Identify predictors of distress for cancer survivors and their families.
• Develop translational research to foster successful implementation of distress screening in clinical practice.
• Develop large-scale, well-designed trials establishing evidence of the effect of nonpharmacologic interventions and psychosocial support that are feasible to deliver and cost effective.
B. Late Effects of Cancer Treatment and Survivorship Care
1. Develop or test and implement interventions to prevent or minimize adverse outcomes related to long-term or late effects and risks associated with the development of comorbid illnesses.
• Conduct intervention trials to reduce long-term risks from cancer therapy with special attention to high-risk populations, specifically childhood cancer survivors and adults at risk for cardiovascular toxicity and bone loss.
• Design healthy lifestyle behavior interventions to maintain a healthy weight; improve physical, functional, and psychological outcomes; decrease recurrence; and improve survival.
• Conduct interventions that address social and work reintegration issues during and after therapy.
• Evaluate outcomes of survivorship intervention research on healthcare use.
2. Explore factors associated with the delivery of quality cancer care to survivors.
• Develop and test the effects and efficiency of models of care to support the Institute of Medicine’s recommendations for survivorship care (e.g., treatment summaries, surveillance, health promotion recommendations). Inherent in this effort is attention to unique needs of specific populations.
• Explore approaches that address system barriers to implementation of IOM recommendations.
• Participate in health informatics initiatives to enhance cancer survivorship care delivery.
• Explore effective ways to care for the growing number of survivors, with attention to older survivors and minority populations.
• Explore challenges facing oncology care and the oncology nursing workforce related to survivorship.
C. Palliative and End-of-Life Care
1. Research to enhance communication and shared decision making
• Explore models for training providers to effectively communicate with patients in palliative care and end-of-life phases of care.
• Evaluate team-based approach models of communication on patient and family outcomes.
• Explore and test interventions to improve shared decision making in palliative care and end-of-life phases of care.
• Explore preferences for decision making and care in the palliative and end-of-life phases of care among the growing and diverse U.S. population.
2. Focus on palliative care for children.
• Evaluate symptom management intersections for children at end of life.
• Examine effects of advanced care planning on pediatric patients with cancer and family outcomes.
• Explore models of palliative and end-of-life care from hospital to community for pediatric patients with cancer and their families.
3. Explore and test models of palliative care delivery, including but not limited to the interdisciplinary team, cost-benefit of services, timeliness of referrals, continuity of care and care coordination, and use of technology.
4. Explore the use of electronic health records to identify unmet palliative care needs.
5. Research how to best support and evaluate professional education and development models for improving palliative and end-of-life care.
D. Self-Management
1. Develop and test measures of self-management outcomes across the cancer care continuum.
• Develop and test new and established self-management measures for multiple populations, including various minority groups, ethnicities, and those with coexisting comorbidities.
• Develop and test new and established measures to access self-management outcomes across the cancer care continuum.
2. Develop and test models of care in self-management across the cancer care continuum.
• Identify the needs of patients and family caregivers regarding self-management during periods of transition from treatment to survivorship.
• Develop and test new and established models of care in self-management for multiple populations, including various minority groups, ethnicities, and those with coexisting comorbidities.
• Develop and test models of care to improve coordinated care across disciplines or specialties to improve self-management at all phases of the cancer care continuum.
3. Develop and test self-management interventions directed at the individual and/or the family caregivers that address health-related outcomes across the cancer care continuum.
• Develop strategies that promote self-management in children, adults, and family caregivers across cultures and ethnicities.
• Conduct intervention studies to improve patient engagement in self-management activities.
• Develop and test interventions to improve care coordination and address the changing self-management needs of individuals with cancer and their family caregivers over time.
• Develop and test self-management interventions to assist patients in managing their cancer and other preexisting chronic conditions.
4. Develop and test interventions to improve adherence with prescribed and/or recommended plans of care.
• Develop and test strategies for improving adherence with prescribed treatment regimens.
• Develop and test strategies for improving adherence with self-management recommendations prescribed in cancer care plans across the care continuum.
E. Aging
1. Carry out descriptive work to obtain information needed to fill the knowledge gap.
• Describe how lifestyle factors, such as nutrition, exercise, smoking, and alcohol intake, affect the symptom burden and treatment responses of older adult patients.
• Explore the impact of age, cancer, and biased decisions related to stigma on older adult patient outcomes.
• Evaluate the relationship between predictive factors (e.g., performance status, age, physical and psychological comorbidities, polypharmacy) of chemotherapy toxicity and symptom burden across geriatric age groups from the youngest old to the oldest old.
2. Develop, test, and implement interventions to improve the care of older adult patients.
• Test interventions that promote engaged treatment decision making based on risks assessed through a comprehensive geriatric assessment (CGA). Determine which components of the CGA predict treatment outcomes (e.g., functional status, health-related quality of life).
• Determine how to adapt symptom management interventions, to decrease risk and enhance protective factors, and to promote positive outcomes in older adult patients.
• Test interventions for palliative, supportive, and end-of-life care for older adults who are unable to tolerate active curative treatment.
• Test interventions to improve outcomes in family caregivers with chronic medical conditions who are caring for an older adult with cancer.
• Test interventions to improve patient-clinician communication and self-management for the patient.
• Identify those older adult patients with cancer at higher risk of poorer outcomes, and target interventions to maintain or improve outcomes.
3. Evaluate factors associated with the delivery of cancer care.
• Evaluate how multiple comorbidities (e.g., diabetes, obesity, heart failure, arthritis) affect the symptom burden and treatment responses of older adults with cancer.
• Evaluate factors that influence the delivery of quality and safety of care, as well as healthcare use among older adults with cancer.
• Evaluate the efficacy of using technology to improve outcomes in older adults undergoing cancer treatment.
• Investigate patient outcomes (at levels of frailty and function) beyond progression and survival (e.g., impact of disease and treatment on health-related quality of life, function, cognition, independence).
F. Family and Caregivers
1. Identify the impact of caregiver outcomes on patient outcomes.
• Conduct studies that examine the influence of the caregiver on the quality of patient care delivered.
• Conduct studies that determine the extent to which caregiver distress influences patient and system resource use, such as symptom severity, emergency department visits, patient distress, and adherence to treatment.
• Conduct intervention trials focused on the dyad or family to improve patient outcomes across the care continuum.
2. Determine the impact of the stress of providing care on the caregiver’s physiologic health.
• Conduct studies that examine cellular response to providing care to identify key biomarkers for future work.
• Examine longitudinal cohort studies to determine whether changes at the cellular level translate into meaningful changes in caregivers’ comorbid conditions.
• Conduct intervention trials focused on psychosocial and physiological strategies to improve overall health.
3. Explore, define, and determine the extent of economic burden and its impact on families of patients with cancer.
• Explore the impact of economic burden on caregiver and patient outcomes, including quality-of-life outcomes as well as outcomes related to the use of supportive medication and adherence to treatment regimens.
• Describe ways in which caregivers and families of patients with cancer make short- and long-term lifestyle changes to afford cancer care.
• Implement interventions that provide strategies to ameliorate employment and economic burden.
G. Improving Healthcare Systems
1. Expand the knowledge of patient-centered cancer nursing care.
• Evaluate best practices for oncology nurse–led care coordination.
• Examine interventions for improving nurse-patient communication and their effect on patient outcomes.
• Design and test cost-efficient patient care models for improving patient outcomes across the cancer care continuum.
2. Evaluate the effect of nursing care on promoting and maintaining treatment quality and safety.
• Understand predictors (risk models), cost settings, side effects, educational approaches, population health literacy, and cognitive changes associated with adherence to self-care.
• Evaluate the influence of various care providers and cost effectiveness on quality and safety.
• Evaluate strategies for the identification and prevention of adverse events related to quality and safety.
• Develop and test interventions that support delivery of quality care indicators.
H. Risk Reduction
1. Develop and/or test interventions to sustain cancer screening behavior beyond completion of one-time screening.
• Develop and/or test interventions to increase first-time and interval cancer screening for under-served and understudied populations (e.g., ethnic minorities, urban poor, rural residents, older adults, sexual minorities).
• Develop or test culturally responsive interventions, including those that enhance healthcare providers’ cultural competence.
• Apply findings from other areas with more extensive research (e.g., breast cancer screening) to increase screening for other cancers.
• Conduct comparative effectiveness trials to apply evidence-based intervention strategies in cancer screening to clinical and community practice settings.
2. Develop and/or test innovative and cost-effective interventions to change multiple health behaviors in a population that can reduce or prevent cancer (e.g., obesity, tobacco cessation).
• Develop and test interventions to adopt or maintain health behaviors that prevent or reduce the risk for cancer (e.g., reductions in tobacco use and alcohol abuse, dietary change, physical activity, weight management, reductions in exposure to ultraviolet light).
• Develop and/or test innovative and cost-effective interventions for health behavior change.
• Develop and/or test culturally appropriate heath behavior interventions for minority and underserved groups.
3. Develop and/or test dissemination and implementation of evidence-based interventions in screening.
• Adapt and test efficacious interventions for implementation in clinic or community settings.
• Implement and evaluate dissemination and implementation models for translating evidence-based interventions to practice.
• Develop and test academic-practice partnerships to accelerate dissemination and implementation models.
• Collaborate with healthcare systems and practices to test models of dissemination and implementation of efficacious interventions to enhance sustainability.
I. Cross-Cutting Themes
Four innovative cross-cutting themes were identified: bioinformatics, biomarkers, comparative effectiveness research, and dissemination and implementation science.
1. Bioinformatics
• Use large data sets to explain patient outcomes and increase understanding of the complexity of disease, treatment, and patient responses.
• Create predictive models.
2. Biomarkers
• Identify underlying mechanisms for a particular condition or symptom.
• Identify patients at high risk for poorer outcomes.
• Develop interventions that are tailored to address inter-individual variability.
• Test interventions to improve patient outcomes.
3. Comparative effectiveness research
• Compare benefits and harms of a specific treatment or intervention.
• Evaluate applicability of evidence generated through randomized, controlled trials to practice.
• Investigate effects of treatments on morbidity, quality of life, and survival outcomes.
4. Dissemination and implementation science
• Studies of strategies (e.g., audit and feedback, clinician reminders or alerts, decision support, practice facilitation) that promote the adoption of cost-effective interventions
• Studies that examine the extent to which research-tested interventions (e.g., exercise for fatigue, cognitive-behavioral therapy for sleep, cancer screening) can be tailored to a wide variety of service delivery models while, at the same time, maintaining efficacy
• Evaluate research-practice partnerships that increase the likelihood that cost-effective interventions can be embedded within care delivery processes.
• Studies to enhance the usability, acceptability, and integration into workflow of informatics and other technologies that support the delivery of patient-centered, guideline-concordant care
• Test system-wide efforts to routinely achieve evidence-based care, including the development, implementation, and evaluation of point-of-care information collection using patient-reported outcomes and sensor devices, as well as point-of-care testing coupled with clinical decision support.
Conclusion
The Research Agenda is a synthesis of the state of the science in cancer and identifies gaps and directions for the conduct and dissemination of research. Oncology nurses can use the agenda to inform clinical practice, develop research proposals, inform policy makers, support interdisciplinary research efforts, and promote scientist and clinician collaborations in targeted patient-centered research.
The 2014–2018 ONS Research Agenda Project Team gratefully acknowledges the support of the ONS Foundation for development of the agenda. The team also thanks Jenny Brown and Kerri Moriarty, MLS, at ONS for their assistance throughout the development and completion of the ONS Research Agenda.
References
LoBiondo-Wood, G., Brown, C.G., Knobf, M.T., Lyon, D., Mallory, G., Mitchell, S. A., . . . Fellman, B. (2014). Priorities for oncology nursing research: The 2013 national survey. Oncology Nursing Forum, 41, 67–76. doi:10.1188/ONF.14.67–76
Oncology Nursing Society. (2015a). Oncology Nursing Society 2014–2018 Research Agenda. Retrieved from https://www.ons.org/sites/default/files/2014-2018%20ONS%20Research%20Ag…
Oncology Nursing Society. (2015b). Executive summary ONS research agenda. Retrieved from https://www.ons.org/sites/default/files/2014-2018%20ONS%20Research%20Ag…
Bibliography
A. Symptoms
Ahles, T.A., Root, J.C., & Ryan, E.L. (2012). Cancer- and cancer treatment-associated cognitive change: An update on the state of the science. Journal of Clinical Oncology, 30, 3675–3686. doi:10.1200/JCO.2012.43.0116
Anderson, K.O., Green, C.R., & Payne, R. (2009). Racial and ethnic disparities in pain: Causes and consequences of unequal care. Journal of Pain, 10, 1187–1204. doi:10.1016/j.jpain.2009.10.002
Barsevick, A.M., Irwin, M.R., Hinds, P., Miller, A., Berger, A., Jacobsen, P., . . . Cella, D. (2013). Recommendations for high-priority research on cancer-related fatigue in children and adults. Journal of the National Cancer Institute, 105, 1432–1440. doi:10.1093/jnci/djt242
Barton, D.L., Liu, H., Dakhil, S.R., Linquist, B., Sloan, J.A., Nichols, C.R., . . . Loprinzi, C.L. (2013). Wisconsin Ginseng (Panax quinquefolius) to improve cancer-related fatigue: A randomized, double-blind trial, N07C2. Journal of the National Cancer Institute, 105, 1230–1238. doi:10.1093/jnci/djt181
Bender, C.M., & Thelen, B.D. (2013). Cancer and cognitive changes: The complexity of the problem. Seminars in Oncology Nursing, 29, 232–237. doi:10.1016/j.soncn.2013.08.003
Berger, A.M., Yennu, S., & Million, R. (2013). Update on interventions focused on symptom clusters: What has been tried and what have we learned? Current Opinion in Supportive and Palliative Care, 7, 60–66. doi:10.1097/SPC.0b013e32835c7d88
Berry, D.L., Hong, F., Halpenny, B., Partridge, A.H., Fann, J.R., Wolpin, S., . . . Ford, R. (2014). Electronic self–report assessment for cancer and self-care support: Results of a multicenter randomized trial. Journal of Clinical Oncology, 32, 199–205. doi:10.1200/jco.2013.48.6662
Brinkman, T.M., Zhu, L., Zeltzer, L.K., Recklitis, C.J., Kimberg, C., Zhang, N., . . . Krull, K.R. (2013). Longitudinal patterns of psychological distress in adult survivors of childhood cancer. British Journal of Cancer, 109, 1373–1381. doi:10.1038/bjc.2013.428
Brown, J.C., Huedo-Medina, T.B., Pescatello, L.S., Pescatello, S.M., Ferrer, R.A., & Johnson, B.T. (2011). Efficacy of exercise interventions in modulating cancer-related fatigue among adult cancer survivors: A meta-analysis. Cancer Epidemiology Biomarkers and Prevention, 20, 123–133. doi:10.1158/1055-9965.epi-10-0988
Brown, J.K., Cooley, M.E., Chernecky, C., & Sarna, L. (2011). A symptom cluster and sentinel symptom experienced by women with lung cancer. Oncology Nursing Forum, 38, E425–E435. doi:10.1188/11.ONF.E425-E435
Cooley, M.E., Blonquist, T.M., Catalano, P.J., Lobach, D.F., Halpenny, B., McCorkle, R., . . . Abrahm, J.L. (2015). Feasibility of using algorithm-based clinical decision support for symptom assessment and management in lung cancer. Journal of Pain and Symptom Management, 49, 13–26.
de Raaf, P.J., de Klerk, C., Timman, R., Busschbach, J.J., Oldenmenger, W.H., & van der Rijt, C.C. (2013). Systematic monitoring and treatment of physical symptoms to alleviate fatigue in patients with advanced cancer: A randomized controlled trial. Journal of Clinical Oncology, 31, 716–723. doi:10.1200/jco.2012.44.4216
Dhruva, A., Aouizerat, B.E., Cooper, B., Paul, S.M., Dodd, M., West, C., . . . Miaskowski, C. (2015). Cytokine gene associations with self-report ratings of morning and evening fatigue in oncology patients and their family caregivers. Biological Research for Nursing, 17, 175–184. doi:10.1177/1099800414534313
Donovan, K.A., Grassi, L., McGinty, H.L., & Jacobsen, P.B. (2014). Validation of the distress thermometer worldwide: State of the science. Psycho-Oncology, 23, 241–250. doi:10.1002/pon.3430
Donovan, K.A., & Jacobsen, P.B. (2013). Progress in the implementation of NCCN guidelines for distress management by member institutions. Journal of the National Comprehensive Cancer Network, 11, 223–226.
Drwecki, B.B., Moore, C.F., Ward, S.E., & Prkachin, K.M. (2011). Reducing racial disparities in pain treatment: The role of empathy and perspective-taking. Pain, 152, 1001–1006. doi:10.1016/j.pain.2010.12.005
Fisch, M.J., Lee, J.W., Weiss, M., Wagner, L.I., Chang, V.T., Cella, D., . . . Cleeland, C.S. (2012). Prospective, observational study of pain and analgesic prescribing in medical oncology outpatients with breast, colorectal, lung, or prostate cancer. Journal of Clinical Oncology, 30, 1980–1988. doi:10.1200/jco.2011.39.2381
Given, C.W., Bradley, C., You, M., Sikorskii, A., & Given, B. (2010). Costs of novel symptom management interventions and their impact on hospitalizations. Journal of Pain and Symptom Management, 39, 663–672. doi:10.1016/j.jpainsymman.2009.07.014
Han, Y., & Smith, M.T. (2013). Pathobiology of cancer chemotherapy-induced peripheral neuropathy (CIPN). Frontiers in Pharmacology, 4, 156. doi:10.3389/fphar.2013.00156
Hershman, D.L., Lacchetti, C., Dworkin, R.H., Lavoie Smith, E.M., Bleeker, J., Cavaletti, G., . . . Loprinzi, C.L. (2014). Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. Journal of Clinical Oncology, 32, 1941–1967. doi:10.1200/JCO.2013.54.0914
Holland, J., Watson, M., & Dunn, J. (2011). The IPOS new International Standard of Quality Cancer Care: Integrating the psychosocial domain into routine care. Psycho-Oncology, 20, 677–680. doi:10.1002/pon.1978
Holohan, K.N., Von Ah, D., McDonald, B.C., & Saykin, A.J. (2013). Neuroimaging, cancer and cognition: State of the knowledge brief. Seminars in Oncology Nursing, 29, 280–287. doi:10.1016/j.soncn.2013.08.008
Jacobsen, P.B., & Wagner, L.I. (2012). A new quality standard: The integration of psychosocial care into routine cancer care. Journal of Clinical Oncology, 30, 1154–1159. doi:10.1200/JCO.2011.39.5046
Jansen, C.E. (2013). Cognitive changes associated with cancer and cancer therapy: Patient assessment and education. Seminars in Oncology Nursing, 4, 270–279. doi:10.1016/j.soncn.2013.08.007
Jansen, C.E., Miaskowski, C., Dodd, M., Dowling, G., & Kramer, J. (2005). A meta-analysis of studies of the effects of cancer chemotherapy on various domains of cognitive function. Cancer, 104, 2222–2233. doi:10.1002/cncr.21469
Jim, H.S., Jacobsen, P.B., Phillips, K.M., Wenham, R.M., Roberts, W., & Small, B.J. (2013). Lagged relationships among sleep disturbance, fatigue, and depressed mood during chemotherapy. Health Psychology, 32, 768–774. doi:10.1037/a0031322
Kim, H.J., Barsevick, A.M., Fang, C.Y., & Miaskowski, C. (2012). Common biological pathways underlying the psychoneurological symptom cluster in cancer patients. Cancer Nursing, 35, E1–E20. doi:10.1097/NCC.0b013e318233a811
Koller, A., Miaskowski, C., De Geest, S., Opitz, O., & Spichiger, E. (2012). A systematic evaluation of content, structure, and efficacy of interventions to improve patients’ self-management of cancer pain. Journal of Pain and Symptom Management, 44, 264–284. doi:10.1016/j.jpainsymman.2011.08.015
Lai, J.S., Wagner, L.I., Jacobsen, P.B., & Cella, D.F. (2014). Self-reported cognitive concerns and abilities: Two sides of one coin? Psycho-Oncology, 23, 1133–1141. doi:10.1002/pon.3522
Langford, D.J., Lee, K., & Miaskowski, C. (2012). Sleep disturbance interventions in oncology patients and family caregivers: A comprehensive review and meta-analysis. Sleep Medicine Reviews, 16, 397–414. doi:10.1016/j.smrv.2011.07.002
LoBiondo-Wood, G., Brown, C.G., Knobf, M.T., Lyon, D.E., Mallory, G., Mitchell, S.A., . . . Fellman, B. (2014). Priorities for oncology nursing: The 2013 National Survey. Oncology Nursing Forum, 41, 67–76. doi:10.1188/14.ONF.67-76
Miaskowski, C., Dodd, M., Lee, K., West, C., Paul, S.M., Cooper, B.A., . . . Aouizerat, B.E. (2010). Preliminary evidence of an association between a functional interleukin-6 polymorphism and fatigue and sleep disturbance in oncology patients and their family caregivers. Journal of Pain and Symptom Management, 40, 531–544. doi:10.1016/j.jpainsymman.2009.12.006
Miltenburg, N.C., & Boogerd, W. (2014). Chemotherapy-induced neuropathy: A comprehensive survey. Cancer Treatment Reviews, 40, 872–882. doi:10.1016/j.ctrv.2014.04.004
Mooney, K.H., Beck, S.L., Friedman, R.H., Farzanfar, R., & Wong, B. (2014). Automated monitoring of symptoms during ambulatory chemotherapy and oncology providers’ use of the information: A randomized controlled clinical trial. Supportive Care in Cancer, 22, 2343–2350. doi:10.1007/s00520-014-2216-1
Myers, J.S. (2013). Cancer- and chemotherapy-related cognitive changes: The patient experience. Seminars in Oncology Nursing, 29, 300–307. doi:10.1016/j.soncn.2013.08.010
National Comprehensive Cancer Network. (2013). NCCN Clinical Practice Guidelines in Oncology: Distress management. Journal of the National Comprehensive Cancer Network, 11, 190–209.
Pirl, W.F., Fann, J.R., Green, J.A., Braun, I., Deshields, T., Fulcher, C., . . . Bardwell, W.A. (2014). Recommendations for the implementation of distress screening programs in cancer centers: Report from the American Psychosocial Oncology Society (APOS), Association of Oncology Social Work (AOSW) and Oncology Nursing Society (ONS) joint task force. Cancer, 120, 2946–2954. doi:10.1002/cncr.28750
Reeve, B.B., Mitchell, S.A., Dueck, A.C., Basch, E., Cella, D., Reilly, C.M., . . . Bruner, D.W. (2014). Recommended patient-reported core set of symptoms to measure in adult cancer treatment trials. Journal of the National Cancer Institute, 106(7), dju129. doi:10.1093/jnci/dju129
Schumacher, K.L., Plano Clark, V.L., West, C.M., Dodd, M.J., Rabow, M.W., & Miaskowski, C. (2014). Pain medication management processes used by oncology outpatients and family caregivers part I: Health systems contexts. Journal of Pain and Symptom Management, 48, 770–783. doi:10.1016/j.jpainsymman.2013.12.242
Schumacher, K.L., Plano Clark, V.L., West, C.M., Dodd, M.J., Rabow, M.W., & Miaskowski, C. (2014b). Pain medication management processes used by oncology outpatients and family caregivers part II: Home and lifestyle contexts. Journal of Pain and Symptom Management, 48, 784–796. doi:10.1016/j.jpainsymman.2013.12.247
Sheinfeld Gorin, S., Krebs, P., Badr, H., Janke, E.A., Jim, H.S., Spring, B., . . . Jacobsen, P.B. (2012). Meta-analysis of psychosocial interventions to reduce pain in patients with cancer. Journal of Clinical Oncology, 30, 539–547. doi:10.1200/jco.2011.37.0437
Siefert, M.L., Hong, F., Valcarce, B., & Berry, D.L. (2014). Patient and clinician communication of self-reported insomnia during ambulatory cancer care clinic visits. Cancer Nursing, 37, E51–E59. doi:10.1097/NCC.0b013e318283a7bc
Sikorskii, A., Given, C.W., Siddiqi, A.E., Champion, V., McCorkle, R., Spoelstra, S.L., & Given, B.A. (2014). Testing the differential effects of symptom management interventions in cancer. Psycho-Oncology, 24, 25–32. doi:10.1002/pon.3555
Skerman, H.M., Yates, P.M., & Battistutta, D. (2012). Identification of cancer-related symptom clusters: An empirical comparison of exploratory factor analysis methods. Journal of Pain and Symptom Management, 44, 10–22. doi:10.1016/j.jpainsymman.2011.07.009
Smith, E.M. (2013). Current methods for the assessment and management of taxane-related neuropathy. Clinical Journal of Oncology Nursing, 17(Suppl. 1), S22–S34. doi:10.1188/13.CJON.S1.22-34
Smith, E.M., Pang, H., Cirrincione, C., Fleishman, S., Paskett, E.D., Ahles, T., . . . Sharpiro, C.L. (2013). Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: A randomized clinical trial. JAMA, 309, 1359–1367. doi:10.1001/jama.2013.2813
Stubblefield, M.D., Burstein, H.J., Burton, A.W., Custodio, C.M., Deng, G.E., Ho, M., . . . Von Roenn, J. (2009). NCCN Task Force Report: Management of neuropathy in cancer. Journal of the National Comprehensive Cancer Network, 7(Suppl. 5), S1–S28.
Tofthagen, C., Visovsky, C., & Berry, D.L. (2012). Strength and balance training for adults with peripheral neuropathy and high risk of fall: Current evidence and implications for future research [Online exclusive]. Oncology Nursing Forum, 39, E416–E424. doi:10.1188/12.ONF.E416-E424
Von Ah, D., Carpenter, J.S., Saykin, A., Monahan, P.O., Wu, J., Yu, M., . . . Unverzagt, F. (2012). Advanced cognitive training for breast cancer survivors: A randomized controlled trial. Breast Cancer Research and Treatment, 135, 799–809. doi:10.1007/s10549-012-2210-6
Von Ah, D., Jansen, C., Allen, D.H., Schiavone, R.M., & Wulff, J. (2011). Putting Evidence Into Practice: Evidence-based interventions for cancer and cancer treatment-related cognitive impairment. Clinical Journal of Oncology Nursing, 15, 607–615. doi:10.1188/11.CJON.607-615
Wefel, J.S., Vardy, J., Ahles, T., & Schagen, S.B. (2011). International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncology, 12, 703–708. doi:10.1016/S1470-2045(10)70294-1
Xiao, C., Bruner, D.W., Jennings, B.M., & Hanlon, A.L. (2014). Methods for examining cancer symptom clusters over time. Research in Nursing and Health, 37, 65–74. doi:10.1002/nur.21572
B. Late Effects of Cancer Treatment and Survivorship Care
American Cancer Society. (2014). Cancer treatment and survivorship facts and figures 2014–2015. Retrieved from http://www.cancer.org/acs/groups/content/@research/documents/document/a…
Aziz, N. (2007). Late effects of cancer treatment. In P.A. Ganz (Ed.), Cancer survivorship (pp. 54–76). New York, NY: Springer.
Halpern, M.T., Viswanathan, M., Evans, T.S., Birken, S.A., Basch, E., & Mayer, D.K. (2014). Models of cancer survivorship care: Overview and summary of current evidence. Journal of Oncology Practice. Retrieved from http://jop.ascopubs.org/content/early/2014/09/09/JOP.2014.001403.abstra…
Harrington, C.B., Hansen, J.A., Moskowitz, M., Todd, B.L., & Feuerstein, M. (2010). It’s not over when it’s over: Long-term symptoms in cancer survivors—A systematic review. International Journal of Psychiatry Medicine, 40, 163–181. doi:10.2190/PM.40.2.c
Hewitt, M., Rowland, J.H., & Yancik, R. (2003). Cancer survivors in the United States: Age, health, and disability. Journals of Gerontology. Series A: Biological Sciences and Medical Sciences, 58, M82–M91. doi:10.1093/gerona/58.1.M82
Hoekstra, R.A., Heins, M.J., & Korevaar, J.C. (2014). Health care needs of cancer survivors in general practice: A systematic review. BMC Family Practice, 15, 94. doi:10.1186/1471-2296-15-94
Mayer, D.K., Birken, S.A., Check, D.K., & Chen, R.C. (2015). Summing it up: An integrative review of studies of cancer survivorship care plans (2006–2013). Cancer, 21, 978–996. doi:10.1002/cncr.28884
McCorkle, R., Ercolano, E., Lazenby, M., Schulman-Green, D., Schilling, L.S., Lorig, K., & Wagner, E.H. (2011). Self-management: Enabling and empowering patients living with cancer as a chronic illness. CA: A Cancer Journal for Clinicians, 61, 50–62.
National Cancer Institute. (n.d.a). NCI dictionary of cancer terms. Late effect. Retrieved from http://www.cancer.gov/dictionary?CdrID=390292
National Cancer Institute. (n.d.b). NCI dictionary of cancer terms. Long-term side effect. Retrieved from http://www.cancer.gov/dictionary?CdrID=693593
National Cancer Institute. (n.d.c). NCI dictionary of cancer terms. Survivorship. Retrieved from http://www.cancer.gov/dictionary?CdrID=445089
Nekhlyudov, L., & Wenger, N. (2014). Institute of Medicine recommendations for improving the quality of cancer care: What do they mean for the general internist? Journal of General Internal Medicine, 29, 1404–1409. doi:10.1007/s11606-014-2931-9
Oeffinger, K.C., & McCabe, M.S. (2006). Models for delivering survivorship care. Journal of Clinical Oncology, 24, 5117–5124. doi:10.1200/JCO.2006.07.0474
Shi, Q., Smith, T.G., Michonski, J.D., Stein, K.D., Kaw, C., & Cleeland, C.S. (2011). Symptom burden in cancer survivors 1 year after diagnosis: A report from the American Cancer Society’s studies of cancer survivors. Cancer, 117, 2779–2790. doi:10.1002/cncr.26146
Snyder, C.F., Frick, K.D., Herbert, R.J., Blackford, A.L., Neville, B.A., Wolff, A.C., . . . Earle, C.C. (2013). Quality of care for comorbid conditions during the transition to survivorship: Differences between cancer survivors and noncancer controls. Journal of Clinical Oncology, 31, 1140–1148. doi:10.1200/JCO.2012.43.0272
Weaver, K.E., Forsythe, L.P., Reeve, B.B., Alfano, C.M., Rodriguez, J.L., Sabatino, S.A., . . . Rowland, J.H. (2012). Mental and physical health-related quality of life among U.S. cancer survivors: Population estimates from the 2010 National Health Interview Survey. Cancer Epidemiology, Biomarkers and Prevention, 21, 2108–2117. doi:10.1158/1055-9965.EPI-12-0740
Wu, H.S., & Harden, J.K. (2015). Symptom burden and quality of life in survivorship: A review of the literature. Cancer Nursing, 38, E29–E54. doi:10.1097/NCC.0000000000000135
Yabroff, K.R., Lawrence, W.F., Clauser, S., Davis, W.W., & Brown, M.L. (2004). Burden of illness in cancer survivors: Findings from a population-based national sample. Journal of the National Cancer Institute, 96, 1322–1330. doi:10.1093/jnci/djh255
Zucca, A.C., Boyes, A.W., Linden, W., & Girgis, A. (2012). All’s well that ends well? Quality of life and physical symptom clusters in long-term cancer survivors across cancer types. Journal of Pain and Symptom Management, 43, 720–731. doi:10.1016/j.jpainsymman.2011.04.023
C. Palliative and End-of-Life Care
Adams, J.A., Bailey, D.E., Jr., Anderson, R.A., & Docherty, S.L. (2011). Nursing roles and strategies in end-of-life decision making in acute care: A systematic review of the literature. Nursing Research and Practice. Retrieved from http://www.hindawi.com/journals/nrp/2011/527834
Administration on Aging. (2011). A profile of older americans: 2011. Retrieved from http://www.aoa.gov/Aging_Statistics/Profile/2011/docs/2011profile.pdf
Aziz, N.M., Grady, P.A., & Curtis, J.R. (2013). Training and career development in palliative care and end-of-life research: Opportunities for development in the U.S. Journal of Pain and Symptom Management, 46, 938–946. doi:10.1016/j.jpainsymman.2013.02.008
Bakitas, M., Lyons, K.D., Hegel, M.T., Balan, S., Brokaw, F.C., Seville, J., . . . Ahles, T.A. (2009). Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: The Project ENABLE II randomized controlled trial. JAMA, 302, 741–749. doi:10.1001/jama.2009.1198
Bona, K., Bates, J., & Wolfe, J. (2011). Massachusetts’ Pediatric Palliative Care Network: Successful implementation of a novel state-funded pediatric palliative care program. Journal of Palliative Medicine, 14, 1217–1223. doi:10.1089/jpm.2011.0070
Bruera, E., & Hui, D. (2010). Integrating supportive and palliative care in the trajectory of cancer: Establishing goals and models of care. Journal of Clinical Oncology, 28, 4013–4017. doi:10.1200/JCO.2010.29.5618
Carpenter, K.M., Stoner, S.A., Schmitz, K., McGregor, B.A., & Doorenbos, A.Z. (2014). An online stress management workbook for breast cancer. Journal of Behavioral Medicine, 37, 458–468. doi:10.1007/s10865-012-9481-6
Carr, D. (2012). Racial and ethnic differences in advance care planning: Identifying subgroup patterns and obstacles. Journal of Aging and Health, 24, 923–947. doi:10.1177/0898264312449185
Cheng, M.J., King, L.M., Alesi, E.R., & Smith, T.J. (2013). Doing palliative care in the oncology office. Journal of Oncology Practice, 9, 84–88. doi:10.1200/JOP.2013.000885
Curtis, J.R., Back, A.L., Ford, D.W., Downey, L., Shannon, S.E., Doorenbos, A.Z., . . . Engelberg, R.A. (2013). Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: A randomized trial. JAMA, 310, 2271–2281. doi:10.1001/jama.2013.282081
Dahlin, C. (Ed.). (2013). Clinical practice guidelines for quality palliative care (3rd ed.). Retrieved from http://www.nationalconsensusproject.org/NCP_Clinical_Practice_Guideline…
Demiris, G., Parker Oliver, D., Wittenberg-Lyles, E., Washington, K., Doorenbos, A., Rue, T., & Berry, D. (2012). A non-inferiority trial of a problem-solving intervention for hospice caregivers: In person vs. videophone. Journal of Palliative Medicine, 15, 653–660. doi:10.1089/jpm.2011.0488
Doorenbos, A.Z., Starks, H., Bourget, E., McMullan, D.M., Lewis-Newby, M., Rue, T.C., . . . Wilfond, B.S. (2013). Examining palliative care team involvement in automatic consults for children on extracorporeal life support (ECLS) in the pediatric intensive care unit. Journal of Palliative Medicine, 16, 492–495. doi:10.1089/jpm.2012.0536
Epstein, R.M., & Street, R.L., Jr. (2007, October). Patient-centered communication in cancer care: Promoting healing and reducing suffering (NIH Publication No. 07-6225). Retrieved from http://appliedresearch.cancer.gov/areas/pcc/communication/pcc_monograph…
Feudtner, C., Womer, J., Augustin, R., Remke, S., Wolfe, J., Friebert, S., & Weissman, D. (2013). Pediatric palliative care programs in children’s hospitals: A cross-sectional national survey. Pediatrics, 132, 1063–1070. doi:10.1542/peds.2013-1286
Fletcher, D., & Panke, J. (2012). Improving value in healthcare: Opportunities and challenges for palliative care professionals in the age of health reform. Journal of Hospice and Palliative Nursing, 14, 452–461. doi:10.1097/NJH.0b013e3182604df2
Gelfman, L.P., Du, Q., & Morrison, R.S. (2013). An update: NIH research funding for palliative medicine 2006 to 2010. Journal of Palliative Medicine, 16, 125–129. doi:10.1089/jpm.2012.0427
Gwilliam, B., Keeley, V., Todd, C., Gittins, M., Roberts, C., Kelly, L., . . . Stone, P.C. (2011). Development of Prognosis in Palliative Care Study (PIPS) predictor models to improve prognostication in advanced cancer: Prospective cohort study. BMJ, 343, d4920. doi:10.1136/bmj.d4920
Haozous, E., Doorenbos, A.Z., Demiris, G., Eaton, L.H., Towle, C., Kundu, A., & Buchwald, D. (2012). Role of telehealth/videoconferencing in managing cancer pain in rural American Indian communities. Psycho-Oncology, 21, 219–223. doi:10.1002/pon.1887
Head, B.A., Schapmire, T., Hermann, C., Earnshaw, L., Faul, A., Jones, C., . . . Pfeifer, M. (2014). The Interdisciplinary Curriculum for Oncology Palliative Care Education (iCOPE): Meeting the challenge of interprofessional education. Journal of Palliative Medicine, 17, 1107–1114. doi:10.1089/jpm.2014.0070
Institute of Medicine. (1997). Approaching death: Improving care at the end of life. Retrieved from http://www.nap.edu/openbook.php?record_id=5801
Institute of Medicine. (2001). Improving palliative care for cancer. Retrieved from http://www.nap.edu/openbook.php?record_id=10149
Johnson, K.S. (2013). Racial and ethnic disparities in palliative care. Journal of Palliative Medicine, 16, 1329–1334.
Krishnan, M., Temel, J.S., Wright, A.A., Bernacki, R., Selvaggi, K., & Balboni, T. (2013). Predicting life expectancy in patients with advanced incurable cancer: A review. Journal of Supportive Oncology, 11, 68–74. doi:10.12788/j.suponc.0004
Lotz, J.D., Jox, R.J., Borasio, G.D., & Führer, M. (2013). Pediatric advance care planning: A systematic review. Pediatrics, 131, e873–e880. doi:10.1542/peds.2012-2394
Mack, J.W., Paulk, M.E., Viswanath, K., & Prigerson, H.G. (2010). Racial disparities in the outcomes of communication on medical care received near death. Archives of Internal Medicine, 170, 1533–1540. doi:10.1001/archinternmed.2010.322
Morrison, R.S., Augustin, R., Souvanna, P., & Meier, D.E. (2011). America’s care of serious illness: A state-by-state report card on access to palliative care in our nation’s hospitals. Journal of Palliative Medicine, 14, 1094–1096. doi:10.1089/jpm.2011.9634
Murphy, A., Siebert, K., Owens, D., & Doorenbos, A.Z. (2013). Health care utilization by patients whose care is managed by a primary palliative care clinic. Journal of Hospice and Palliative Nursing, 15, 372–379. doi:10.1097/NJH.0b013e3182a02b9d
National Institute of Nursing Research. (2013). Building momentum: The science of end-of-life and palliative care. A review of research trends and funding, 1997–2010. Retrieved from http://www.ninr.nih.gov/sites/www.ninr.nih.gov/files/NINR-Building-Mome…
Pritchard, M., Burghen, E.A., Gattuso, J.S., West, N.K., Gajjar, P., Srivastava, D.K., . . . Hinds, P.S. (2010). Factors that distinguish symptoms of most concern to parents from other symptoms of dying children. Journal of Pain and Symptom Management, 39, 627–636. doi:10.1016/j.jpainsymman.2009.08.012
Smith, A.K., Walter, L.C., Miao, Y., Boscardin, W.J., & Covinsky, K.E. (2013). Disability during the last two years of life. JAMA Internal Medicine, 173, 1506–1513. doi:10.1001/jamainternmed.2013.8738
Smith, T.J., Temin, S., Alesi, E.R., Abernethy, A.P., Balboni, T.A., Basch, E.M., . . . Von Roenn, J.H. (2012). American Society of Clinical Oncology provisional clinical opinion: The integration of palliative care into standard oncology care. Journal of Clinical Oncology, 30, 880–887. doi:10.1200/JCO.2011.38.5161
Temel, J.S., Greer, J.A., Muzikansky, A., Gallagher, E.R., Admane, S., Jackson, V.A., . . . Lynch, T.J. (2010). Early palliative care for patients with metastatic non–small-cell lung cancer. New England Journal of Medicine, 363, 733–742. doi:10.1056/NEJMoa1000678
Volandes, A.E., Paasche-Orlow, M.K., Mitchell, S.L., El-Jawahri, A., Davis, A.D., Barry, M.J., . . . Temel, J.S. (2013). Randomized controlled trial of a video decision support tool for cardiopulmonary resuscitation decision making in advanced cancer. Journal of Clinical Oncology, 31, 380–386. doi:10.1200/JCO.2012.43.9570
Waite, K.R., Federman, A.D., McCarthy, D.M., Sudore, R., Curtis, L.M., Baker, D.W., . . . Paasche‐Orlow, M.K. (2013). Literacy and race as risk factors for low rates of advance directives in older adults. Journal of the American Geriatrics Society, 61, 403–406. doi:10.1111/jgs.12134
Walling, A., Lorenz, K.A., & Dy, S.M. (2008). Evidence-based recommendations for information and care planning in cancer care. Journal of Clinical Oncology, 26, 3896–3902.
Wendler, D., & Rid, A. (2011). Systematic review: The effects on surrogates of making treatment decisions for others. Annals of Internal Medicine, 154, 336–346. doi:10.7326/0003-4819-154-5-201103010-00008
White, D.B., Cua, S.M., Walk, R., Pollice, L., Weissfeld, L., Hong, S., . . . Arnold, R.M. (2012). Nurse-led intervention to improve surrogate decision making for patients with advanced critical illness. American Journal of Critical Care, 21, 396–409. doi:10.4037/ajcc2012223
Wolfe, J., Grier, H.E., Klar, N., Levin, S.B., Ellenbogen, J.M., Salem-Schatz, S., . . . Weeks, J.C. (2000). Symptoms and suffering at the end of life in children with cancer. New England Journal of Medicine, 342, 326–333. doi:10.1056/NEJM200002033420506
World Health Organization. (2014). WHO definition of palliative care. Retrieved from http://www.who.int/cancer/palliative/definition/en
Yennurajalingam, S., Parsons, H.A., Duarte, E.R., Palma, A., Bunge, S., Palmer, J.L., . . . Bruera, E. (2013). Decisional control preferences of Hispanic patients with advanced cancer from the United States and Latin America. Journal of Pain and Symptom Management, 46, 376–385. doi:10.1016/j.jpainsymman.2012.08.015
Youngwerth, J., & Twaddle, M. (2011). Cultures of interdisciplinary teams: how to foster good dynamics. Journal of Palliative Medicine, 14, 650–654. doi:10.1089/jpm.2010.0395
Zier, L.S., Sottile, P.D., Hong, S.Y., Weissfeld, L.A., & White, D.B. (2012). Surrogate decision makers’ interpretation of prognostic information: A mixed-methods study. Annals of Internal Medicine, 156, 360–366. doi:10.7326/0003-4819-156-5-201203060-00008
D. Self-Management
Banning, M. (2012). Adherence to adjuvant therapy in post-menopausal breast cancer patients: A review. European Journal of Cancer Care, 21, 10–19. doi:10.1111/j.1365-2354.2011.01295.x
Bassan, F., Peter, F., Houbre, B., Brennstuhl, M.J., Costantini, M., Speyer, E., & Tarquinio, C. (2014). Adherence to oral antineoplastic agents by cancer patients: Definition and literature review. European Journal of Cancer Care, 23, 22–35. doi:10.1111/ecc.12124
Bender, C.M., Gentry, A.L., Brufsky, A.M., Casillo, F.E., Cohen, S.M., Dailey, M.M., . . . Sereika, S.M. (2014). Influence of patient and treatment factors on adherence to adjuvant endocrine therapy in breast cancer. Oncology Nursing Forum, 41, 274–285. doi:10.1188/14.ONF.274-285
Corbin, J., & Strauss, A. (1985). Managing chronic illness at home: Three lines of work. Qualitative Sociology, 8, 224–247. doi:10.1007/BF00989485
Dingley, C, & Roux, G. (2014). The role of inner strength in quality of life and self-management in women survivors of cancer. Research in Nursing and Health, 37, 32–41. doi:10.1002/nur.21579
Fee-Schroeder, K., Howell, L., Kokal, J., Bjornsen, S., Christensen, S., Hathaway, J., . . . Vickers, K.S. (2013). Empowering individuals to self-manage chemotherapy side effects. Clinical Journal of Oncology Nursing, 17, 369–371. doi:10.1188/13.CJON.369-371
Given, B., Given, C.W., McCorkle, R., Kozachik, S., Cimprich, B., Rahbar, M.H., & Wojcik, C. (2002). Pain and fatigue management: Results of a nursing randomized clinical trial. Oncology Nursing Forum, 29, 949–956. doi:10.1188/02.ONF.949-956
Given, C., Given, B., Rahbar, M., Jeon, S., McCorkle, R., Cimprich, B., . . . Bowie, E. (2004). Effect of a cognitive behavioral intervention on reducing symptom severity during chemotherapy. Journal of Clinical Oncology, 22, 507–516. doi:10.1200/JCO.2004.01.241
Hammelef, K.J., Friese, C.R., Breslin, T.M., Riba, M., & Schneider, S.M. (2014). Implementing distress management guidelines in ambulatory oncology: A quality improvement project. Clinical Journal of Oncology Nursing, 18(Suppl. 1), 31–36. doi:10.1188/14.CJON.S1.31–36
Hershey, D.S., Tipton, J., Given, B., & Davis, E. (2012). Perceived impact of cancer treatment on diabetes self-management. Diabetes Educator, 38, 779–790. doi:10.1177/0145721712458835
Improving Chronic Illness Care. (2014). The Chronic Care Model. Retrieved from http://www.improvingchroniccare.org/index.php?p=The_Chronic_Care_Model&…
Institute of Medicine. (2012). Living well with chronic illness: A call for public action. Retreived from http://books.nap.edu/openbook.php?record_id=13272&page=R1
Jerofke, T., Weiss, M., & Yakusheva, O. (2014). Patient perceptions of patient-empowering nurse behaviours, patient activation and functional health status in postsurgical patients with life-threatening long-term illnesses. Journal of Advanced Nursing, 70, 1310–1322. doi:10.1111/jan.12286
Koller, A., Hasemann, M., Jaroslawski, K., De Geest, S., & Becker, G. (2014). Testing the feasibility and effects of a self-management support intervention for patients with cancer and their family caregivers to reduce pain and related symptoms (ANtiPain): Study protocol of a pilot study. Open Journal of Nursing, 4, 85–94. doi:10.4236/ojn.2014.42012
Koller, A., Miaskowski, C., De Geest, S., Opitz, O., & Spichiger, E. (2013a). Results of a randomized controlled pilot study of a self-management intervention for cancer pain. European Journal of Oncology Nursing, 17, 284–291. doi:10.1016/j.ejon.2012.08.002
Koller, A., Miaskowski, C., De Geest, S., Opitz, O., & Spichiger, E. (2013b). Supporting self-management of pain in cancer patients: Methods and lessons learned from a randomized controlled pilot study. European Journal of Oncology Nursing, 17, 1–8. doi:10.1016/j.ejon.2012.02.006
Lovell, M., Agar, M., Luckett, T., Davidson, P.M., Green, A., & Clayton, J. (2013). Australian survey of current practice and guideline use in adult cancer pain assessment and management: Perspectives of palliative care physicians. Journal of Palliative Medicine, 16, 1403–1409. doi:10.1089/jpm.2013.0245
Martin, F., Turner, A., Bourne, C., & Batehup, L. (2013). Development and qualitative evaluation of a self-management workshop for testicular cancer survivor-initiated follow-up. Oncology Nursing Forum, 40, E14–E23. doi:10.1188/13.ONF.E14-E23
McConigley, R., Holloway, K., Smith, J., Halkett, G., Keyser, J., Aoun, S., & Monterosso, L. (2011). The diagnosis and treatment decisions of cancer patients in rural Western Australia. Cancer Nursing, 34(4), E1–E9. doi:10.1097/NCC.0b013e3181f795e7
McCorkle, R., Ercolano, E., Lazenby, M., Schulman‐Green, D., Schilling, L.S., Lorig, K., & Wagner, E.H. (2011). Self‐management: Enabling and empowering patients living with cancer as a chronic illness. CA: A Cancer Journal for Clinicians, 61, 50–62. doi:10.3322/caac.20093
Miaskowski, C., Dodd, M., West, C., Schumacher, K., Paul, S.M., Tripathy, D., & Koo, P. (2004). Randomized clinical trial of the effectiveness of a self-care intervention to improve cancer pain management. Journal of Clinical Oncology, 22, 1713–1720. doi:10.1200/JCO.2004.06.140
Ozdilli, J., Wilkinson, A., & Frew, G. (2013). Improving patient outcomes following a cancer diagnosis. British Journal of Community Nursing, 18, 318–321. doi:10.12968/bjcn.2013.18.7.318
Palmer, N.R., Bartholomew, L.K., McCurdy, S.A., Basen-Engquist, K.M., & Naik, A.D. (2013). Transitioning from active treatment: Colorectal cancer survivors’ health promotion goals. Palliative and Supportive Care, 11, 101–109. doi:10.1017/S1478951512000788
Regan, M., Mills, J., & Ristevski, E. (2012). Cancer care coordinators’ relationships with the multidisciplinary team and patients: Everything to everyone. Australian Journal of Cancer Nursing, 13, 12–19.
Rustøen, T., Valeberg, B.T., Kolstad, E., Wist, E., Paul, S., & Miaskowski, C. (2014). A randomized clinical trial of the efficacy of a self-care intervention to improve cancer pain management. Cancer Nursing, 37, 34–43. doi:10.1097/NCC.0b013e3182948418
Salvatore, A., Ahn, S., Jiang, L., Lorig, K., & Ory, M. (n.d.). National study of chronic disease self-management: Six and twelve-month findings among cancer survivors and non-cancer survivors. Retrieved from https://apha.confex.com/apha/142am/webprogram/Paper312325.html
Sarradon-Eck, A., Pellegrini, I., Largillier, R., Duran, S., Tallet, A., Tarpin, C., & Julian-Reynier, C. (2012). Self-management strategies adopted by breast cancer survivors to improve their adherence to tamoxifen. Breast Journal, 18, 389–391. doi:10.1111/j.1524-4741.2012.01258.x
Schulman-Green, D., Bradley, E.H., Knobf, M., Prigerson, H., DiGiovanna, M.P., & McCorkle, R. (2011). Self-management and transitions in women with advanced breast cancer. Journal of Pain and Symptom Management, 42, 517–525. doi:10.1016/j.jpainsymman.2010.12.007
Schulman‐Green, D., Jaser, S., Martin, F., Alonzo, A., Grey, M., McCorkle, R., . . . Whittemore, R. (2012). Processes of self-management in chronic illness. Journal of Nursing Scholarship, 44, 136–144. doi:10.1111/j.1547-5069.2012.01444.x
Sheppard, C. (2007). Breast cancer follow-up: Literature review and discussion. European Journal of Oncology Nursing, 11, 340–347. doi:10.1016/j.ejon.2006.09.001
Sherwood, P., Given, B.A., Given, C.W., Champion, V.L., Doorenbos, A.Z., Azzouz, F., . . . Monahan, P.O. (2005). A cognitive behavioral intervention for symptom management in patients with advanced cancer. Oncology Nursing Forum, 32, 1190–1198. doi:10.1188/05.ONF.1190-1198
Spoelstra, S.L., Given, B.A., Given, C.W., Grant, M., Sikorskii, A., You, M., & Decker, V. (2013). An intervention to improve adherence and management of symptoms for patients prescribed oral chemotherapy agents: An exploratory study. Cancer Nursing, 36, 18–28. doi:10.1097/NCC.0b013e3182551587
Stang, I., & Mittelmark, M.B. (2010). Intervention to enhance empowerment in breast cancer self-help groups. Nursing Inquiry, 17, 47–57. doi:10.1111/j.1440-1800.2009.00465.x
Stevinson, C., Lydon, A., & Amir, Z. (2014). Adherence to physical activity guidelines among cancer support group participants. European Journal of Cancer Care, 23, 199–205. doi:10.1111/ecc.12145
Wagner, E., & McCorkle, R. (2010). Self-management support. In J. Holland (Ed.), Psycho-oncology (2nd ed., pp. 464–486). New York, NY: Oxford University Press.
Wagner, E.H. (1998). Chronic disease management: What will it take to improve care for chronic illness? Effective Clinical Practice. Retrieved from http://ecp.acponline.org/augsep98/cdm.pdf
E. Aging
Lichtman, S.M., Hurria, A., & Jacobsen, P.B. (2014). Geriatric oncology: An overview. Journal of Clinical Oncology, 32, 2521–2522. doi:10.1200/JCO.2014.57.4822
Naeim, A., Aapro, M., Subbarao, R., & Balducci, L. (2014). Supportive care considerations for older adults with cancer. Journal of Clinical Oncology, 32, 2627–2634. doi:10.1200/JCO.2014.55.3065
Rowland, J.H., & Bellizzi, K.M. (2014). Cancer survivorship issues: Life after treatment and implications for an aging population. Journal of Clinical Oncology, 32, 2662–2668. doi:10.1200/JCO.2014.55.8361
Wildiers, H., Heeren, P., Puts, M., Topinkova, E., Janssen-Heijnen, M.L., Extermann, M., . . . Hurria, A. (2014). International Society of Geriatric Oncology consensus on geriatric assessment in older patients with cancer. Journal of Clinical Oncology, 32, 2595–2603. doi:10.1200/JCO.2013.54.8347
F. Family and Caregivers
Applebaum, A.J., & Breitbart, W. (2013). Care for the cancer caregiver: A systematic review. Palliative and Supportive Care, 11, 231–252. doi:10.1017/S1478951512000594
Collinge, W., Kahn, J., Walton, T., Kozak, L., Bauer-Wu, S., Fletcher, K., . . . Soltysik, R. (2013). Touch, caring, and cancer: Randomized controlled trial of a multimedia caregiver education program. Supportive Care in Cancer, 21, 1405–1414. doi:10.1007/s00520-012-1682-6
Francis, L.E., Bowman, K.F., Kypriotakis, G., & Rose, J.H. (2011). Relationships and emotional wellbeing among African American and White advanced cancer caregivers. Patient Education and Counseling, 85, 446–453. doi:10.1016/j.pec.2011.01.023
Godwin, K.M., Mills, W.L., Anderson, J.A., & Kunik, M.E. (2013). Technology-driven interventions for caregivers of persons with dementia: A systematic review. American Journal of Alzheimer’s Disease and Other Dementias, 28, 216–222. doi:10.1177/1533317513481091
Houser, A.N., & Gibson, M.J. (2008, November). Valuing the invaluable: The economic value of family caregiving, 2008 update. Retrieved from http://www.aarp.org/relationships/caregiving/info-11-2008/i13_caregivin…
Kim, Y., Carver, C.S., Schulz, R., Lucette, A., & Cannady, R.S. (2013). Finding benefit in bereavement among family cancer caregivers. Journal of Palliative Medicine, 16, 1040–1047. doi:10.1089/jpm.2013.0049
Kim, Y., Carver, C.S., Spillers, R.L., Crammer, C., & Zhou, E.S. (2011). Individual and dyadic relations between spiritual well-being and quality of life among cancer survivors and their spousal caregivers. Psycho-Oncology, 20, 762–770. doi:10.1002/pon.1778
Kim, Y., Carver, C.S., Spillers, R.L., Love-Ghaffari, M., & Kaw, C.K. (2012). Dyadic effects of fear of recurrence on the quality of life of cancer survivors and their caregivers. Quality of Life Research, 21, 517–525. doi:10.1007/s11136-011-9953-0
Kim, Y., Shaffer, K.M., Carver, C.S., & Cannady, R.S. (2014). Prevalence and predictors of depressive symptoms among cancer caregivers 5 years after the relative’s cancer diagnosis. Journal of Consulting and Clinical Psychology, 82, 1–8. doi:10.1037/a0035116
Kim, Y., & Spillers, R.L. (2010). Quality of life of family caregivers at two years after a relative’s cancer diagnosis. Psycho-Ooncology, 19, 431–440. doi:10.1002/pon.1576
Kim, Y., Spillers, R.L., & Hall, D.L. (2012). Quality of life of family caregivers 5 years after a relative’s cancer diagnosis: Follow-up of the national quality of life survey for caregivers. Psycho-Oncology, 21, 273–281. doi:10.1002/pon.1888
Lengacher, C.A., Kip, K.E., Barta, M., Post-White, J., Jacobsen, P.B., Groer, M., . . . Shelton, M.M. (2012). A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. Journal of Holistic Nursing, 30, 170–185. doi:10.1177/0898010111435949
Northouse, L.L., Katapodi, M.C., Schafenacker, A.M., & Weiss, D. (2012). The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Seminars in Oncology Nursing, 28, 236–245. doi:10.1016/j.soncn.2012.09.006
Northouse, L.L., Katapodi, M.C., Song, L., Zhang, L., & Mood, D.W. (2010). Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. CA: A Cancer Journal for Clinicians, 60, 317–339. doi:10.3322/caac.20081
Regan, T.W., Lambert, S.D., Girgis, A., Kelly, B., Kayser, K., & Turner, J. (2012). Do couple-based interventions make a difference for couples affected by cancer?: A systematic review. BMC Cancer, 12, 279. doi:10.1186/1471-2407-12-279
Rocke, D.J., Beumer, H.W., Thomas, S., & Lee, W.T. (2014). Effect of physician perspective on allocation of Medicare resources for patients with advanced cancer. Otolaryngology—Head and Neck Surgery, 150, 792–800. doi:10.1177/0194599814520689
Savundranayagam, M.Y. (2014). Receiving while giving: The differential roles of receiving help and satisfaction with help on caregiver rewards among spouses and adult‐children. International Journal of Geriatric Psychiatry, 29, 41–48. doi:10.1002/gps.3967
Silveira, M.J., Given, C.W., Cease, K.B., Sikorskii, A., Given, B., Northouse, L.L., & Piette, J.D. (2011). Cancer carepartners: Improving patients’ symptom management by engaging informal caregivers. BMC Palliative Care, 10, 21. doi:10.1186/1472-684X-10-21
Thomas, K.S., Bower, J.E., Williamson, T.J., Hoyt, M.A., Wellisch, D., Stanton, A.L., & Irwin, M. (2012). Post-traumatic disorder symptoms and blunted diurnal cortisol production in partners of prostate cancer patients. Psychoneuroendocrinology, 37, 1181–1190. doi:10.1016/j.psyneuen.2011.12.008
von Känel, R., Mills, P.J., Mausbach, B.T., Dimsdale, J.E., Patterson, T.L., Ziegler, M.G., . . . Grant, I. (2012). Effect of Alzheimer caregiving on circulating levels of C-reactive protein and other biomarkers relevant to cardiovascular disease risk: A longitudinal study. Gerontology, 58, 354–365. doi:10.1159/000334219
Waldron, E.A., Janke, E.A., Bechtel, C.F., Ramirez, M., & Cohen, A. (2013). A systematic review of psychosocial interventions to improve cancer caregiver quality of life. Psycho-Oncology, 22, 1200–1207. doi:10.1002/pon.3118
Williams, A.L., & McCorkle, R. (2011). Cancer family caregivers during the palliative, hospice, and bereavement phases: A review of the descriptive psychosocial literature. Palliative and Supportive Care, 9, 315–325. doi:10.1017/S1478951511000265
Wittenberg-Lyles, E., Parker Oliver, D., Demiris, G., Swarz, J., & Rendo, M. (2014). YouTube as a tool for pain management with informal caregivers of cancer patients: A systematic review. Journal of Pain and Symptom Management, 48, 1200–1210. doi:10.1016/j.jpainsymman.2014.02.015
Yabroff, K.R., Borowski, L., & Lipscomb, J. (2013). Economic studies in colorectal cancer: Challenges in measuring and comparing costs. Journal of the National Cancer Institute. Monographs, 2013, 62–78. doi:10.1093/jncimonographs/lgt001
Yennurajalingam, S., Noguera, A., Parsons, H.A., Torres-Vigil, I., Duarte, E. R., Palma, A., . . . Bruera, E. (2013). A multicenter survey of Hispanic caregiver preferences for patient decision control in the United States and Latin America. Palliative Medicine, 27, 692–698. doi:10.1177/0269216313486953
G. Improving Healthcare Systems
American Nurses Association. (2011). The value of nurse care coordination: A white paper of the American Nurses Association. Retrieved from http://www.nursingworld.org/carecoordinationwhitepaper
Berry, D.L., Hong, F., Halpenny, B., Partridge, A., Fox, E., Fann, J.R., . . . Ford, R. (2014). The electronic self-report assessment and intervention for cancer: Promoting patient verbal reporting of symptom and quality of life issues in a randomized controlled trial. BMC Cancer, 14, 513. doi:10.1186/1471-2407-14-513
Cook, W.A., Morrison, M.L., Eaton, L.H., Theodore, B.R., & Doorenbos, A.Z. (2014). The use and quality of cost effectiveness analysis in U.S. nursing research 1997–2011: A 15 year review. Manuscript submitted for publication.
Crane-Okada, R. (2013). Evaluation and outcome measures in patient navigation. Seminars in Oncology Nursing, 29, 128–140. doi:10.1016/j.soncn.2013.02.008
Drummond, M.F., Sculpher, M.J., Torrance, G.W., O’Brien, B.J., & Stoddart, G.L. (2005). Methods for the economic evaluation of health care programmes (3rd ed.). Oxford, England: Oxford University Press.
Eagle, D. & Sprandio, J. (2011). A care model for the future: The oncology medical home. Oncology, 25, 571, 575–576.
Farrington, M., Cullen, L., & Dawson, C. (2010). Assessment of oral mucositis in adult and pediatric oncology patients: An evidence-based approach. ORL—Head and Neck Nursing, 28(3), 8–15.
Fox, J. (2013). Lessons from an oncology medical home collaborative. American Journal of Managed Care. Retrieved from http://www.ajmc.com/publications/evidence-based-oncology/2013/2013-1-vo…
Hines, S., Ramis, M.A., Pike, S., & Chang, A.M. (2014). The effectiveness of psychosocial interventions for cognitive dysfunction in cancer patients who have received chemotherapy: A systematic review. Worldviews on Evidence-Based Nursing, 11, 187–193. doi:10.1111/wvn.12042
Institute of Medicine. (2013). Delivering high-quality cancer care: Charting a new course for a system in crisis. Retrieved from http://books.nap.edu/openbook.php?record_id=18359
Kiely, D. (2014). Timeliness in breast cancer care as an indicator of quality. Clinical Journal of Oncology Nursing, 18, 82–88. doi:10.1188/14.CJON.82-88
Kuntz, G., Tozer, J., Snegosky, J., Fox, J., & Neumann, K. (2014). Michigan oncology medical home demonstration project: First-year results. Journal of Oncology Practice, 10, 294–297. doi:10.1200/JOP.2013.001365
Mason, H., DeRubeis, M.B., Foster, J.C., Taylor, J.M., & Worden, F.P. (2013). Outcomes evaluation of a weekly nurse practitioner-managed symptom management clinic for patients with head and neck cancer treated with chemoradiotherapy. Oncology Nursing Forum, 40, 581–586. doi:10.1188/13.ONF.40-06AP
Mattsson, T.O., Knudsen, J.L., Lauritsen, J., Brixen, K., & Herrstedt, J. (2013). Assessment of the global trigger tool to measure, monitor and evaluate patient safety in cancer patients: Reliability concerns are raised. BMJ Quality and Safety, 22, 571–579. doi:10.1136/bmjqs-2012-001219
Mayer, D.K., Gerstel, A., Walton, A.L., Triglianos, T., Sadiq, T.E., Hawkins, N.A., & Davies, J.M. (2014). Implementing survivorship care plans for colon cancer survivors. Oncology Nursing Forum, 41, 266–273. doi:10.1188/14.ONF.266-273
McDonald, K.M., Sundaram, V., Bravata, D.M., Lewis, R., Lin, N., Kraft, S.A., . . . Owens, D.K. (2007). Closing the quality gap: A critical analysis of quality improvement strategies. Technical Review 9. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK44015
McFarlane, K., Dixon, L., Wakeman, C.J., Robertson, G.M., Eglinton, T.W., & Frizelle, F.A. (2012). The process and outcomes of a nurse-led colorectal cancer follow-up clinic. Colorectal Disease, 14, e245–249. doi:10.1111/j.1463-1318.2011.02923.x
Patient-Centered Outcomes Research Institute. (2013). Patient-Centered Outcomes Research Institute. Retrieved from http://www.pcori.org/research-we-support/priorities-agenda
Preyde, M. & Synnott, E. (2009). Psychosocial intervention for adults with cancer: A meta-analysis. Journal of Evidence Based Social Work, 6, 321–347. doi:10.1080/15433710903126521
Pritham, W., Cureton, A., & Royce, M. (2009) Breast cancer survivorship clinic: A nurse practitioner-led model. Retrieved from http://www.empr.com/breast-cancer-survivorship-clinic-a-nurse-practitio…
Prouty, C.D., Mazor, K.M., Greene, S.M., Roblin, D.W., Firneno, C.L., Lemay, C.A., . . . Gallagher, T.H. (2014). Providers’ perceptions of communication breakdowns in cancer care. Journal of General Internal Medicine, 29, 1122–1130. doi:10.1007/s11606-014-2769-1
Qamar, N., Pappalardo, A.A., Arora, V.M., & Press, V.G. (2011). Patient-centered care and its effect on outcomes in the treatment of asthma. Patient Related Outcomes Measures, 2, 81–109. doi:10.2147/PROM.S12634
Rask, M.T., Jensen, M.L., Andersen, J., & Zachariae, R. (2009). Effects of an intervention aimed at improving nurse-patient communication in an oncology outpatient clinic. Cancer Nursing, 32, E1–E11. doi:10.1097/01.NCC.0000343365.13871.12
Robles, L., Slogoff, M., Ladwig-Scott, E., Zank, D., Larson, M.K., Aranha, G., & Shoup, M. (2011). The addition of a nurse practitioner to an inpatient surgical team results in improved use of resources. Surgery, 150, 711–717. doi:10.1016/j.surg.2011.08.022
Ruegg, T.A. (2013). A nurse practitioner-led urgent care center: Meeting the needs of the patient with cancer [Online exclusive]. Clinical Journal of Oncology Nursing, 17, E52–E57. doi:10.1188/13.CJON.E52-E57
Tavernier, S.S. (2014). Translating research on the distress thermometer into practice. Clinical Journal of Oncology Nursing, 18(Suppl. 1), 26–30. doi:10.1188/14.CJON.S1.26-30
Tetuan, T.M., Ohm, R., Herynk, M.H., Ebberts, M., Wendling, T., & Mosier, M.C. (2014). The Affordable Health Care Act annual wellness visits: The effectiveness of a nurse-run clinic in promoting adherence to mammogram and colonoscopy recommendations. Journal of Nursing Administration, 44, 270–275. doi:10.1097/NNA.0000000000000066
Wittenberg-Lyles, E., Goldsmith, J., & Ferrell, B. (2013). Oncology nurse communication barriers to patient-centered care. Clinical Journal of Oncology Nursing, 17, 152–158. doi:10.1188/13.CJON.152-158
H. Risk Reduction
Agency for Health Research and Quality. (2014, May). 2013 National Healthcare Disparities Report (AHRQ Publication No. 14-0005). Retrieved from http://www.ahrq.gov/research/findings/nhqrdr/nhdr13/2013nhdr.pdf
American Cancer Society. (2010). Cancer facts and figures 2010. Atlanta, GA: Author.
Anhang, R., Goodman, A., & Goldie, S.J. (2004). HPV communication: Review of existing research and recommendations for patient education. CA: A Cancer Journal for Clinicians, 54, 248–259. doi:10.3322/canjclin.54.5.248
Atkin, W.S., Edwards, R., Kralj-Hans, I., Wooldrage, K., Hart, A.R., Northover, J., . . . Cuzick, J. (2010). Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: A multicentre randomised controlled trial. Lancet, 375, 1624–1633. doi:10.1016/S0140-6736(10)60551-X
Bach, P.B., Mirkin, J.N., Oliver, T.K., Azzoli, C.G., Berry, D.A., Brawley, O.W., . . . Detterbeck, F.C. (2012). Benefits and harms of CT screening for lung cancer: A systematic review. JAMA, 307, 2418–2429. doi:10.1001/jama.2012.5521
Berg, C.J., Thomas, A.N., Mertens, A.C., Schauer, G.L., Pinsker, E.A., Ahluwalia, J.S., & Khuri, F.R. (2012). Correlates of continued smoking versus cessation among survivors of smoking-related cancers. Psycho-Oncology. doi:10.1002/pon.30n77
Bowen, D.J., Moinpour, C., Thompson, B., Anderson, M.R., Meischke, H., & Cochrane, B. (2009). Creation of a theoretical framework for public health intervention design. In S.M. Miller, D.J. Bowen, R.T. Croyle, & J.H. Rowland (Eds.), Handbook of cancer control and behavioral science: A resource for researchers, practitioners, and policymakers (pp. 43–56). Washington, DC: American Psychological Association.
Boyle, R., Solberg, L., & Fiore, M. (2011). Use of electronic health records to support smoking cessation. Cochrane Database of Systematic Reviews, 12, CD008743. doi:10.1002/14651858.CD008743.pub2
Breen, N., Wagener, D.K., Brown, M.L., Davis, W.W., & Ballard-Barbash, R. (2001). Progress in cancer screening over a decade: Results of cancer screening from the 1987, 1992, and 1998 National Health Interview Surveys. Journal of the National Cancer Institute, 93, 1704–1713. doi:10.1093/jnci/93.22.1704
Britton, J., & Bogdanovica, I (2014). Electronic cigarettes A report commissioned by Public Health England. Retrieved from https://www.gov.uk/government/uploads/system/uploads/attachment_data/fi…
Cancer Research UK. (2014). Diet causing cancer. Retrieved from http://www.cancerresearchuk.org/about-cancer/cancers-in-general/causes-…
Caponnetto, P., Russo, C., Bruno, C.M., Alamo, A., Amaradio, M.D., & Polosa, R. (2013). Electronic cigarette: a possible substitute for cigarette dependence. Monaldi Archives for Chest Disease, 79, 12–19.
Carroll Chapman, S.L., & Wu, L.T. (2014). E-cigarette prevalence and correlates of use among adolescents versus adults: A review and comparison. Journal of Psychiatric Research, 54, 43–54. doi:10.1016/j.jpsychires.2014.03.005
Cataldo, J.K., Dubey, S., & Prochaska, J.J. (2010). Smoking cessation: An integral part of lung cancer treatment. Oncology, 78(5–6), 289–301.
Cheng, T. (2014). Chemical evaluation of electronic cigarettes. Tobacco Control, 23(Suppl. 2), ii11–ii17. doi:10.1136/tobaccocontrol-2013-051482
Cokkinides, V., Bandi, P., Siegel, R., Ward, E.M., & Thun, M.J. (2007). Cancer prevention and early detection facts and figures 2008. Retrieved from http://www.cancer.org/acs/groups/content/@nho/documents/document/cped_2…
Cooley, M.E., Lundin, R., & Murray, L. (2009). Smoking cessation interventions in cancer care: Opportunities for oncology nurses and nurse scientists. Annual Review of Nursing Research, 27, 243–272.
Doll, R., Peto, R., Boreham, J., & Sutherland, I. (2004). Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ, 328, 1519.
Duffy, S.A., Khan, M.J., Ronis, D.L., Fowler, K.E., Gruber, S.B., Wolf, G.T., & Terrell, J.E. (2008). Health behaviors of head and neck cancer patients the first year after diagnosis. Head and Neck, 30, 93–102.
Duffy, S.A., Reeves, P., Hermann, C., Karvonen, C., & Smith, P. (2008). In-hospital smoking cessation programs: What do VA patients and staff want and need? Applied Nursing Research, 21, 199–206.
Duffy, S.A., Ronis, D.L., McLean, S., Fowler, K.E., Gruber, S.B., Wolf, G.T., & Terrell, J.E. (2009). Pretreatment health behaviors predict survival among patients with head and neck squamous cell carcinoma. Journal of Clinical Oncology, 27, 1969–1975.
Duffy, S.A., Ronis, D.L., Valenstein, M., Lambert, M.T., Fowler, K.E., Gregory, L., . . . Terrell, J.E. (2006). A tailored smoking, alcohol, and depression intervention for head and neck cancer patients. Cancer Epidemiology, Biomarkers and Prevention, 15, 2203–2208. doi:10.1158/1055-9965.epi-05-0880
Emmons, K.M., Puleo, E., Sprunck-Harrild, K., Ford, J., Ostroff, J.S., Hodgson, D., . . . Tyc, V. (2013). Partnership for health-2, a web-based versus print smoking cessation intervention for childhood and young adult cancer survivors: randomized comparative effectiveness study. Journal of Medical Internet Research, 15, e218. doi:10.2196/jmir.2533
Eyre, H., Kahn, R., Robertson, R.M., Clark, N.G., Doyle, C., Gansler, T., . . . Thun, M.J. (2004). Preventing cancer, cardiovascular disease, and diabetes: A common agenda for the American Cancer Society, the American Diabetes Association, and the American Heart Association. CA: A Cancer Journal for Clinicians, 54, 190–207. doi:10.3322/canjclin.54.4.190
Fisher, T.L., Burnet, D.L., Huang, E.S., Chin, M.H., & Cagney, K.A. (2007). Cultural leverage interventions using culture to narrow racial disparities in health care. Medical Care Research and Review, 64(Suppl. 5), 243S–282S. doi:10.1177/1077558707305414
Grana, R., Benowitz, N., & Glantz, S.A. (2014). E-cigarettes: A scientific review. Circulation, 129, 1972–1986. doi:10.1161/circulationaha.114.007667
Gritz, E.R., Carr, C.R., Rapkin, D., Abemayor, E., Chang, L.J., Wong, W.K., . . . Ward, P.H. (1993). Predictors of long-term smoking cessation in head and neck cancer patients. Cancer Epidemiology, Biomarkers and Prevention, 2, 261–270.
Gritz, E.R., Dresler, C., & Sarna, L. (2005). Smoking, the missing drug interaction in clinical trials: Ignoring the obvious. Cancer Epidemiology, Biomarkers and Prevention, 14, 2287–2293.
Gritz, E.R., Lam, C.Y., Vidrine, D.J., & Fingeret, M.C. (2011). Cancer prevention: Tobacco dependence and its treatment. In V. De Vita, T.S. Lawrence, & S. Rosenberg (Eds.), Cancer: Principles and practice of oncology (9th ed., pp. 529–542). Philadelphia, PA: Lippincott Williams and Wilkins.
Gutierrez, A., Suh, R., Abtin, F., Genshaft, S., & Brown, K. (2013). Lung cancer screening. Seminars Intervention Radiology, 30, 114–120. doi:10.1055/s-0033-1342951
Hajek, P., Etter, J.F., Benowitz, N., Eissenberg, T., & McRobbie, H. (2014). Electronic cigarettes: Review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction, 109, 1801–1810. doi:10.1111/add.12659
Hajek, P., Taylor, T.Z., & Mills, P. (2002). Brief intervention during hospital admission to help patients to give up smoking after myocardial infarction and bypass surgery: Randomised controlled trial. BMJ, 324, 87–89.
Harrell, P.T., Simmons, V.N., Correa, J.B., Padhya, T.A., & Brandon, T.H. (2014). Electronic nicotine delivery systems (“e-cigarettes”): Review of safety and smoking cessation efficacy. Otolaryngology: Head and Neck Surgery, 151, 381–393. doi:10.1177/0194599814536847
Hyman, D.J., Pavlik, V.N., Taylor, W.C., Goodrick, G.K., & Moye, L. (2007). Simultaneous vs sequential counseling for multiple behavior change. Archives of Internal Medicine, 167, 1152–1158. doi:10.1001/archinte.167.11.1152
Institute of Medicine. (2004). Health literacy: A prescription to end confusion. Retrieved from http://books.nap.edu/openbook.php?record_id=10883&page=R1
International Agency for Research on Cancer. (2002). IARC handbooks of cancer prevention, volume 6: Weight control and physical activity. Retrieved from http://www.iarc.fr/en/publications/pdfs-online/prev/handbook6
Johnson, C.D., Chen, M.H., Toledano, A.Y., Heiken, J.P., Dachman, A., Kuo, M.D., . . . Limburg, P.J. (2008). Accuracy of CT colonography for detection of large adenomas and cancers. New England Journal of Medicine, 359, 1207–1217. doi:10.1056/NEJMoa0800996
Katz, D.A., Holman, J., Johnson, S., Hillis, S.L., Ono, S., Stewart, K., . . . Vander Weg, M.W. (2013). Implementing smoking cessation guidelines for hospitalized veterans: Effects on nurse attitudes and performance. Journal of General Internal Medicing, 28, 1420–1429. doi:10.1007/s11606-013-2464-7
Kawahara, M., Ushijima, S., Kamimori, T., Kodama, N., Ogawara, M., & Matsui, K.F. (1998). Second primary tumours in more than 2-year disease-free survivors of small-cell lung cancer in Japan: The role of smoking cessation. British Journal of Cancer, 78, 402–412. doi:10.1038/bjc.1998.507
Land, S. (2013). Tobacco Control Research Branch, Behavioral Research Program, Division of Cancer Control and Population Sciences. Tobacco use by cancer patients in clinical trials. Retrieved from http://deainfo.nci.nih.gov/advisory/ctac/1113/Tobacco%20Use%20by%20Canc…
Lawrence, L. (2014, August 27). Cancer faces a growing crisis: Obesity. ASCO Connection. Retrieved from http://connection.asco.org/Magazine/Article/ID/3997/Cancer-Care-Faces-a…
Levin, B., Lieberman, D.A., McFarland, B., Andrews, K.S., Brooks, D., & Bond, J. (2008). Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: A joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology, 134, 1570–1595. doi:10.1053/j.gastro.2008.02.002
Levy-Storms, L., Bastani, R., & Reuben, D.B. (2004). Predictors of varying levels of nonadherence to mammography screening in older women. Journal of the American Geriatrics Society, 52, 768–773. doi:10.1111/j.1532-5415.2004.52216.x
Lomas, A., Leonardi-Bee, J., & Bath-Hextall, F. (2012). A systematic review of worldwide incidence of nonmelanoma skin cancer. British Journal of Dermatology, 166, 1069–1080. doi:10.1111/j.1365-2133.2012.10830.x
Lukwago, S.N., Kreuter, M.W., Holt, C.L., Steger-May, K., Bucholtz, D.C., & Skinner, C.S. (2003). Sociocultural correlates of breast cancer knowledge and screening in urban African American women. American Journal of Public Health, 93, 1271–1274. doi:10.2105/AJPH.93.8.1271
Manassa, E.H., Hertl, C.H., & Olbrisch, R.R. (2003). Wound healing problems in smokers and nonsmokers after 132 abdominoplasties. Plastic and Reconstructive Surgery, 111, 2082–2087
Mandel, J.S., Church, T.R., Bond, J.H., Ederer, F., Geisser, M.S., Mongin, S.J., . . . Schuman, L.M. (2000). The effect of fecal occult-blood screening on the incidence of colorectal cancer. New England Journal of Medicine, 343, 1603–1607. doi:10.1056/NEJM200011303432203
Manser, R., Lethaby, A., Irving, L.B., Stone, C., Byrnes, G., Abramson, M.J., & Campbell, D. (2013). Screening for lung cancer. Cochrane Database of Systematic Reviews, 6, Cd001991. doi:10.1002/14651858.CD001991.pub3
Mariotto, A.B., Yabroff, K.R., Shao, Y., Feuer, E.J., & Brown, M.L. (2011). Projections of the cost of cancer care in the United States: 2010–2020. Journal of the National Cancer Institute, 103, 117–128. doi:10.1093/jnci/djq495
McBride, C.M., & Ostroff, J.S. (2003). Teachable moments for promoting smoking cessation: the context of cancer care and survivorship. Cancer Control, 10, 325–333.
Meissner, H.I., Smith, R.A., Rimer, B.K., Wilson, K.M., Rakowski, W., Vernon, S.W., & Briss, P. (2004). Promoting cancer screening: Learning from experience. Cancer, 101(Suppl. 5), 1107–1117. doi:10.1002/cncr.20507
Moller, A.M., Villebro, N., Pedersen, T., & Tonnesen, H. (2002). Effect of preoperative smoking intervention on postoperative complications: A randomised clinical trial. Lancet, 359, 114–117.
Morgan, G., Schnoll, R.A., Alfano, C.M., Evans, S.E., Goldstein, A., Ostroff, J., . . . Cox, L.S. (2011). National Cancer Institute Conference on Treating Tobacco Dependence at Cancer Centers. Journal of Oncology Practice, 7, 178–182. doi:10.1200/jop.2010.000175
Moyer, V.A. (2014). Screening for cognitive impairment in older adults: U.S. Preventive Services Task Force recommendation statement. Annals of Internal Medicine, 160, 791–797. doi:10.7326/m14-0496
National Cancer Institute. (2014). Fact sheet: Physical activity and cancer. Retrieved from http://www.cancer.gov/cancertopics/factsheet/prevention/physicalactivity
National Cancer Institute. (2014). It doesn’t matter where you start. Just start. Retrieved from http://smokefree.gov
National Center for Chronic Disease Health Promotion Office. (2014). The health consequences of smoking—50 years of progress: A report of the surgeon general. Atlanta, GA: Centers for Disease Control and Prevention.
National Guideline Clearinghouse. (n.d.). Guideline synthesis: Screening for breast cancer. Retrieved from http://www.guideline.gov
Odum, L.E., O’Dell, K.A., & Schepers, J.S. (2012). Electronic cigarettes: Do they have a role in smoking cessation? Journal of Pharmacologic Practice, 25, 611–614. doi:10.1177/0897190012451909
Pasick, R.J., & Burke, N.J. (2008). A critical review of theory in breast cancer screening promotion across cultures. Annual Review of Public Health, 29, 351–368. doi:10.1146/annurev.publhealth.29.020907.143420
Patsakham, K.M., Ripley-Moffitt, C., & Goldstein, A.O. (2009). Tobacco use and dependence treatment: A critical component of cancer care. Clinical Journal of Oncology Nursing, 13, 463–464.
Parkin, D.M. (2011). Cancers attributable to consumption of alcohol in the UK in 2010. British Journal of Cancer, 105(Suppl. 2), S14–S18. doi:10.1038/bjc.2011.476
Poghosyan, H., Kennedy Sheldon, L., & Cooley, M.E. (2012). The impact of computed tomography screening for lung cancer on smoking behaviors: A teachable moment? Cancer Nursing, 35, 446–475. doi:10.1097/NCC.0b013e3182406297
Rakowski, W., Breen, N., Meissner, H., Rimer, B.K., Vernon, S.W., Clark, M.A., & Freedman, A.N. (2004). Prevalence and correlates of repeat mammography among women aged 55–79 in the Year 2000 National Health Interview Survey. Preventive Medicine, 39, 1–10. doi:10.1016/j.ypmed.2003.12.032
Rawl, S., Menon, U., Breslau, E., & Burniss, A. (2012). Interventions to promote colorectal cancer screening: An integrative review. Nursing Outlook, 60, 172–181.
Rice, V.H., Hartmann-Boyce, J., & Stead, L.F. (2013). Nursing interventions for smoking cessation. Cochrane Database of Systematic Reviews, 8, CD001188. doi:10.1002/14651858.CD001188.pub4
Rice, V.H., & Stead, L.F. (2008). Nursing interventions for smoking cessation. Cochrane Database of Systematic Reviews, 1, CD001188.
Rigotti, N., Munafo, M., Murphy, M., & Stead, L. (2005). Interventions for smoking cessation in hospitalized patients. Cochrane Database of Systematic Reviews, 4, CD001837.
Rigotti, N., Munafo, M., & Stead, L. (2008). Smoking cessation interventions for hospitalized smokers: A systematic review. Archives of Internal Medicine, 168, 1950–1960.
Rigotti, N.A., Clair, C., Munafo, M.R., & Stead, L.F. (2012). Interventions for smoking cessation in hospitalized patients. Cochrane Database of Systematic Reviews, 5, CD001837. doi:10.1002/14651858.CD001837.pub3
Ryerson, A.B., Benard, V.B., & Major, A.C. (2002). National Breast and Cervical Cancer Early Detection Program 1991–2002 national report. Retrieved from http://www.cdc.gov/cancer/nbccedp/pdf/national_report.pdf
Samat, J.M., & Yoon, S.Y. (Eds.). (2010). Gender, women and the tobacco epidemic. Retrieved from http://www.who.int/tobacco/publications/gender/women_tob_epidemic/en
Sardari Nia, P., Weyler, J., Colpaert, C., Vermeulen, P., Van Marck, E., & Van Schil, P. (2005). Prognostic value of smoking status in operated non-small cell lung cancer. Lung Cancer, 47, 351–359. doi:10.1016/j.lungcan.2004.08.011
Sarna, L., Bialous, S.A., Wells, M., Kotlerman, J., Wewers, M.E., & Froelicher, E.S. (2009). Frequency of nurses’ smoking cessation interventions: Report from a national survey. Journal of Clinical Nursing, 18, 2066–2077. doi:10.1111/j.1365-2702.2009.02796.x
Saslow, D., Boetes, C., Burke, W., Harms, S., Leach, M.O., Lehman, C.D., . . . Russell, C.A. (2007). American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA: A Cancer Journal for Clinicians, 57, 75–89. doi:10.3322/canjclin.57.2.75
Schnoll, R.A., Zhang, B., Rue, M., Krook, J.E., Spears, W.T., Marcus, A.C., & Engstrom, P.F. (2003). Brief physician-initiated quit-smoking strategies for clinical oncology settings: A trial coordinated by the Eastern Cooperative Oncology Group. Journal of Clinical Oncology, 21, 355–365.
Schwartz, M.D., Taylor, K.L., & Willard, K.S. (2003). Prospective association between distress and mammography utilization among women with a family history of breast cancer. Journal of Behavioral Medicine, 26, 105–117. doi:10.1023/A:1023078521319
Seeff, L.C., Royalty, J., Helsel, W.E., Kammerer, W.G., Boehm, J.E., Dwyer, D.M., . . . Tangka, F.K. (2013). Clinical outcomes from the CDC’s colorectal cancer screening demonstration program. Cancer, 119(Suppl. 15), 2820–2833. doi:10.1002/cncr.28163
Smith, R.A., Cokkinides, V., & Brawley, O.W. (2009). Cancer screening in the United States, 2009: A review of current American Cancer Society guidelines and issues in cancer screening. CA: A Cancer Journal for Clinicians, 59, 27–41. doi:10.3322/caac.20008
Stead, L.F., Buitrago, D., Preciado, N., Sanchez, G., Hartmann-Boyce, J., & Lancaster, T. (2013). Physician advice for smoking cessation. Cochrane Database of Systematic Reviews, 5, CD000165. doi:10.1002/14651858.CD000165.pub4
Stead, L.F., & Lancaster, T. (2012). Behavioral interventions as adjuncts to pharmacotherapy for smoking cessation. Cochrane Database of Systematic Reviews, 12, CD009670. doi:10.1002/14651858.CD009670.pub2
Taylor, C.B., & Curry, S.J. (2004). Implementation of evidence-based tobacco use cessation guidelines in managed care organizations. Annals of Behavioral Medicine, 27, 13–21. doi:10.1207/s15324796abm2701_3
Tu, S.P., Yasui, Y., Kuniyuki, A.A., Schwartz, S.M., Jackson, J.C., Hislop, T.G., & Taylor, V. (2003). Mammography screening among Chinese-American women. Cancer, 97, 1293–1302. doi:10.1002/cncr.11169
Tucker, M.A., Murray, N., Shaw, E.G., Ettinger, D.S., Mabry, M., Huber, M.H., . . . Johnson, B.E. (1997). Second primary cancers related to smoking and treatment of small-cell lung cancer. Journal of the National Cancer Institute, 89, 1782–1788. doi:10.1093/jnci/89.23.1782
Underwood, J.M. (2012). Persistent cigarette smoking and other tobacco use after a tobacco-related cancer diagnosis. Journal of Cancer Survivorship, 6, 333–344. doi:10.1007/s11764-012-0230-1
U.S. Department of Health and Human Services. (2004). The health consequences of smoking: A report of the surgeon general, 2004. Rockville, MD: Author.
U.S. Preventive Services Task Force. (2003). Counseling to prevent tobacco use and tobacco-caused disease: Recommendation statement. Rockville, MD: Agency for Healthcare Research and Quality.
van der Aalst, C.M., van den Bergh, K.A.M., Willemsen, M.C., de Koning, H.J., & van Klaveren, R.J. (2010). Lung cancer screening and smoking abstinence: 2 year follow-up data from the Dutch–Belgian randomised controlled lung cancer screening trial. Thorax, 65, 600–605. doi:10.1136/thx.2009.133751
Varner, A., & Murph, P. (2010). Cancer patient navigation: Where do we go from here? Oncology Issues. Retrieved from http://accc-cancer.org/oncology_issues/articles/mayjune10/MJ10-VarnerMu…
Walker, M.S., Vidrine, D.J., Gritz, E.R., Larsen, R.J., Yan, Y., Govindan, R., & Fisher, E.B. (2006). Smoking relapse during the first year after treatment for early-stage non-small-cell lung cancer. Cancer Epidemiology, Biomarkers and Prevention, 15, 2370–2377.
Warnecke, R.B., Oh, A., Breen, N., Gehlert, S., Paskett, E., Tucker, K.L., . . . Hiatt, R.A. (2008). Approaching health disparities from a population perspective: The National Institutes of Health Centers for Population Health and Health Disparities. American Journal of Public Health, 98, 1608–1615. doi:10.2105/AJPH.2006.102525
Warner, M.A., Offord, K.P., Warner, M.E., Lennon, R.L., Conover, M.A., & Jansson-Schumacher, U. (1989). Role of preoperative cessation of smoking and other factors in postoperative pulmonary complications: A blinded prospective study of coronary artery bypass patients. Mayo Clinic Proceedings, 64, 609–616.
Weaver, K.E., Danhauer, S.C., Tooze, J.A., Blackstock, A.W., Spangler, J., Thomas, L., & Sutfin, E.L. (2012). Smoking cessation counseling beliefs and behaviors of outpatient oncology providers. Oncologist, 17, 455–462.
Wilhelmsson, S., & Lindberg, M. (2007). Prevention and health promotion and evidence-based fields of nursing—A literature review. International Journal of Nursing Practice, 13, 254–265. doi:10.1111/j.1440-172X.2007.00635.x
Willaing, I., & Ladelund, S. (2004). Smoking behavior among hospital staff still influences attitudes and counseling on smoking. Nicotine and Tobacco Research, 6, 369–375.
World Cancer Research Fund International. (n.d.). Link between lifestyle and cancer risk. Retrieved from http://www.wcrf.org/int/cancer-facts-figures/link-between-lifestyle-can…
World Cancer Research Fund International. (2009). Policy and action for cancer prevention. Food, nutrition, and physical activity: A global perspective. Retrieved from http://www.dietandcancerreport.org/cancer_resource_center/downloads/Pol…
World Health Organization. (2013). Tobacco Free Initiative (TFI): Questions and answers on electronic cigarettes or electronic nicotine delivery systems (ENDS). Retrieved from https://web.archive.org/web/20130721131331/http://www.who.int/tobacco/c…
Yuan, J.M., Butler, L.M., Stepanov, I., & Hecht, S.S. (2014). Urinary tobacco smoke-constituent biomarkers for assessing risk of lung cancer. Cancer Research, 74, 401–411.
Zapka, J.G., & Lemon, S.C. (2004). Interventions for patients, providers, and health care organizations. Cancer, 101(Suppl. 5), 1165–1187. doi:10.1002/cncr.20504
Zapka, J.G., Taplin, S.H., Solberg, L.I., & Manos, M.M. (2003). A framework for improving the quality of cancer care: The case of breast and cervical cancer screening. Cancer Epidemiology Biomarkers and Prevention, 12, 4–13.
I. Cross-Cutting Themes
Alfaro, E., Dhruva, A., Langford, D.J., Koetters, T., Merriman, J.D., West, C., . . . Miaskowski, C. (2014). Associations between cytokine gene variations and self-reported sleep disturbance in women following breast cancer surgery. European Journal of Oncology Nursing, 18, 85–93. doi:10.1016/j.ejon.2013.08.004
Anders, C.K., Zagar, T.M., & Carey, L.A. (2013). The management of early-stage and metastatic triple-negative breast cancer: A review. Hematology Oncology Clinics of North America, 27, 737–749. doi:10.1016/j.hoc.2013.05.003
Brekke, J.S., Ell, K., & Palinkas, L.A. (2007). Translational science at the National Institute of Mental Health: Can social work take its rightful place?. Research on Social Work Practice, 17, 123–133. doi:10.1177/1049731506293693
Chen, R.C. (2014). Comparative effectiveness research in oncology: The promise, challenges, and opportunities. Seminars in Radiation Oncology, 24, 1–4. doi:10.1016/j.semradonc.2013.08.001
Du, W., & Elemento, O. (2014). Cancer systems biology: Embracing complexity to develop better anticancer therapeutic strategies. Oncogene. Advance online publication. doi:10.1038/onc.2014.291
Flowers, E., Froelicher, E.S., & Aouizerat, B.E. (2013). Measurement of MicroRNA: A regulator of gene expression. Biological Research for Nursing, 15, 167–178. doi:10.1177/1099800411430380
Gilbertson-White, S., Aouizerat, B.E., & Miaskowski, C. (2011). Methodologic issues in the measurement of cytokines to elucidate the biological basis for cancer symptoms. Biological Research for Nursing, 13, 15–24. doi:10.1177/1099800410379497
Hsiao, C.P., Araneta, M., Wang, X.M., & Saligan, L.N. (2013). The association of IFI27 expression and fatigue intensification during localized radiation therapy: Implication of a para-inflammatory bystander response. International Journal of Molecular Sciences, 14, 16943–16957. doi:10.3390/ijms140816943
Hsiao, C.P., Wang, D., Kaushal, A., & Saligan, L. (2013). Mitochondria-related gene expression changes are associated with fatigue in patients with nonmetastatic prostate cancer receiving external beam radiation therapy. Cancer Nursing, 36, 189–197. doi:10.1097/NCC.0b013e318263f514
Institute of Medicine. (2009). Initial national priorities for comparative effectiveness research. Retrieved from http://www.iom.edu/~/media/FilesReport%20Files/2009/ComparativeEffectiv…
Institute of Medicine. (2010). A foundation for evidence-driven practice: A rapid learning system for cancer care—Workshop summary. Retrieved from http://books.nap.edu/openbook.php?record_id=12868&page=R1
Institute of Medicine. (2012). Informatics needs and challenges in cancer research—Workshop summary. Retrieved from http://books.nap.edu/openbook.php?record_id=13425&page=R1
Lam, S.W., Jimenez, C.R., & Boven, E. (2014). Breast cancer classification by proteomic technologies: Current state of knowledge. Cancer Treatment Reviews, 40, 129–138. doi:10.1016/j.ctrv.2013.06.006
Merelli, I., Pérez-Sánchez, H., Gesing, S., & D’Agostino, D. (2014). Managing, analysing, and integrating big data in medical bioinformatics: Open problems and future perspectives. BioMed Research International, 2014, 134023. doi:10.1155/2014/134023
Mitchell, S.A., Fisher, C.A., Hastings, C.E., Silverman, L.B., & Wallen, G.R. (2010). A thematic analysis of theoretical models for translational science in nursing: Mapping the field. Nursing Outlook, 58, 287–300. doi:10.1016/j.outlook.2010.07.001
National Cancer Institute. (n.d.). NCI dictionary of cancer terms: Biomarker. Retrieved from http://www.cancer.gov/dictionary?CdrID=45618
National Research Council. (2011). Toward precision medicine: Building a knowledge network for biomedical research and a new taxonomy of disease. Retrieved from http://www.nap.edu/openbook.php?record_id=13284
Sanoff, H.K., Deal, A.M., Krishnamurthy, J., Torrice, C., Dillon, P., Sorrentino, J., . . . Muss, H.B. (2014). Effect of cytotoxic chemotherapy on markers of molecular age in patients with breast cancer. Journal of the National Cancer Institute, 106, dju057. doi:10.1093/jnci/dju057
Shaikh, A.R., Butte, A.J., Schully, S.D., Dalton, W.S., Khoury, M.J., & Hesse, B.W. (2014). Collaborative biomedicine in the age of big data: The case of cancer. Journal of Medical Internet Research, 16, e101. doi:10.2196/jmir.2496
Stephens, K., Cooper, B.A., West, C., Paul, S.M., Baggott, C.R., Merriman, J.D., . . . Aouizerat, B.E. (2014). Associations between cytokine gene variations and severe persistent breast pain in women following breast cancer surgery. Journal of Pain, 15, 169–180. doi:10.1016/j.jpain.2013.09.015
Stephens, K.E., Miaskowski, C.A., Levine, J.D., Pullinger, C.R., & Aouizerat, B.E. (2013). Epigenetic regulation and measurement of epigenetic changes. Biological Research for Nursing, 15, 373–381. doi:10.1177/1099800412444785
Tabak, R.G., Khoong, E.C., Chambers, D.A., & Brownson, R.C. (2012). Bridging research and practice: Models for dissemination and implementation research. American Journal of Preventive Medicine, 43, 337–350. doi:10.1016/j.amepre.2012.05.024
About the Author(s)
M. Tish Knobf, PhD, RN, AOCN®, FAAN, is a professor in the School of Nursing at Yale University in Orange, CT; Mary E. Cooley, PhD, RN, FAAN, is a nurse scientist at the Dana Farber Cancer Center for Nursing Research in Boston, MA; Sonia Duffy, PhD, RN, FAAN, is a professor in the College of Nursing at Ohio State University in Columbus; Ardith Doorenbos, PhD, RN, FAAN, is a professor in the School of Nursing at the University of Washington in Seattle; Linda Eaton, PhD, RN, AOCN®, is a postdoctoral fellow in the College of Nursing at the University of Utah in Salt Lake City and a research project coordinator in the School of Nursing at the University of Washington; Barbara Given, PhD, RN, FAAN, is a professor in the College of Nursing at Michigan State University in East Lansing; Deborah K. Mayer, PhD, RN, AOCN®, FAAN, is a professor in the School of Nursing at the University of North Carolina at Chapel Hill; Ruth McCorkle, PhD, RN, FAAN, is a professor in the School of Nursing at Yale University; Christine Miaskowski, PhD, RN, FAAN, is a professor in the Department of Physiological Nursing at the University of California, San Francisco; Sandra Mitchell, PhD, CRNP, AOCN®, is a research scientist in the Outcomes Research Branch of the National Cancer Institute in Bethesda, MD; Paula Sherwood, PhD, CNRN, FAAN, is a professor and vice chair of research in the School of Nursing at the University of Pittsburgh in Pennsylvania; Catherine Bender, PhD, RN, FAAN, is a professor and doctoral program director in the School of Nursing at the University of Pittsburgh; Janine Cataldo, PhD, RN, is an associate professor in the School of Nursing at the University of California, San Francisco; Denise Hershey, PhD, FNP, is an assistant professor in the College of Nursing at Michigan State University; Maria Katapodi, PhD, RN, FAAN, is a professor in the Institute of Nursing Science at the University of Basel in Switzerland; Usha Menon, PhD, RN, FAAN, is a centennial professor of nursing in the College of Nursing at Ohio State University; Karen Schumacher, PhD, RN, is an associate professor in the College of Nursing at the University of Nebraska Medical Center in Omaha; Virginia Sun, PhD, RN, is an assistant professor in the Nursing Education and Research Department at the City of Hope National Medical Center in Duarte, CA; Diane Von Ah, PhD, RN, FAAN, is an associate professor in the College of Nursing at Indiana University in Indianapolis; Geri LoBiondo-Wood, PhD, RN, FAAN, is a professor and coordinator of doctoral programs in the Health Science School of Nursing at the University of Texas in Houston; and Gail Mallory, PhD, RN, NEA-BC, is the director of research at the Oncology Nursing Society in Pittsburgh. No financial relationships to disclose. Knobf can be reached at tish.knobf@yale.edu, with copy to editor at ONFEditor@ons.org. (Submitted April 2015. Accepted for publication April 22, 2015.)

