Secondary Exposure of Family Members to Cyclophosphamide After Chemotherapy of Outpatients With Cancer: A Pilot Study
Purpose/Objectives: To measure the total amount of cyclophosphamide (CPA) excreted in the urine of patients with cancer and their cohabitating family members seven days after CPA administration.
Design: Biological monitoring.
Setting: Home setting with outpatients receiving chemo-therapy.
Sample: 8 patients administered CPA, 10 cohabitating family members, and 10 control participants.
Methods: During the first seven days after CPA administration, urine samples were collected from the participants. The samples were analyzed for the unchanged form of CPA using gas chromatography in tandem with mass spectroscopy.
Main Research Variables: CPA levels.
Findings: CPA was detected in 112 of 276 patient urine samples. The last sample containing detectable CPA levels was collected after more than 48 hours in 63% of the patients, with a maximum length of five days post-treatment. In addition, 243 urine samples were collected from family members, and CPA was detected in the samples of five family members (17–252 ng per member). CPA was not detected in any control participants.
Conclusions: These findings indicate that family members in close contact with patients receiving CPA are at high risk for drug exposure as many as seven days post-treatment.
Implications for Nursing: Nurses should educate patients and their family members about preventing exposure to antineoplastic drugs in the home setting.
Jump to a section
Antineoplastic drugs treat malignant tumor cells, but they also affect normal cells, leading to adverse effects. Healthcare workers such as the pharmacists and nurses who prepare or administer these drugs are aware of the risks of occupational exposure. The adverse effects of occupational exposure to antineoplastic drugs include acute symptoms such as allergic reactions (Kusnetz & Condon, 2003; Walusiak, Wittczak, Ruta, & Palczynski, 2002), genotoxicity (Burgaz et al., 2002; McDiarmid, Oliver, Roth, Rogers, & Escalante, 2010), teratogenicity (Hemminki, Kyyronen, & Lindbohm, 1985; Meirow & Schiff, 2005), reproductive effects (Cardonick & Iacobucci, 2004; Fransman et al., 2007), and carcinogenicity (Althouse, Huff, Tomatis, & Wilbourn 1979; Skov et al., 1990). Therefore, measures should be taken to prevent occupational exposure to these drugs.
The people at risk for exposure to hazardous drugs are not only the healthcare workers who directly handle them, but also those who come in contact with the contaminated body excreta of patients with cancer. Those who do not directly handle drugs, such as volunteers, dietitians, and oncologists, also are at risk for exposure to drugs in the healthcare environment (Hon, Teschke, Demers, & Venners, 2014). Variable amounts of antineoplastic agents and their metabolites are excreted in the urine, stool, sweat, and other body excreta of patients receiving these drugs (American Society of Hospital Pharmacists [ASHP], 1990; Polovich, 2011).
Caregivers are at a higher risk for indirect drug exposure because they generally do not wear personal protective equipment (Nygren & Lundgren, 1997). Exposure to antineoplastic drugs can occur during routine nursing tasks; levels of drugs have been detected in patients’ bedding and sweat (Fransman, Vermeulen, & Kromhout, 2005). A study comparing different sources of exposure in nonhospital environments demonstrated that workers dealing with contaminated hospital laundry were exposed to antineoplastic drugs through inhalation. In addition, they were exposed through their skin while cleaning toilets and washing patients in patients’ homes and nursing homes (Meijster, Fransman, Veldhof, & Kromhout, 2006). These findings suggest that family members living with patients with cancer also are potentially at risk for exposure to antineoplastic drugs.
Anticancer chemotherapy is shifting from inpatient to outpatient settings, and the proportion of patients treated as outpatients is increasing. During outpatient chemotherapy, patients spend most of their time at home. Therefore, the risk of exposure for family members living with patients treated with antineoplastic agents is a concern. According to the current safety guidelines for hazardous drug handling, care should be taken when handling body fluids during the first 48 hours post-treatment because the majority of drugs are excreted during this period (ASHP, 1990; Occupational Safety and Health Administration [OSHA], 1995).
Studies on drug exposure have been limited to this time frame only. For instance, one study reported that family members of three patients who were administrated cyclophosphamide (CPA) (Cytoxan®) or 5-fluorouracil (Adrucil®) were exposed to these drugs during the first 48 hours after outpatient chemotherapy (Yuki, Sekine, Takase, Ishida, & Sessink, 2013). However, no published report has evaluated the exposure risks of family members living with patients treated with CPA more than 48 hours post-treatment. Because excretion time varies between different drugs, the period during which hazardous drug-handling precautions should be followed needs to be defined for each antineoplastic agent.
This study targeted women with breast cancer treated with CPA, a commonly used antineoplastic drug. CPA is classified as a human genotoxic carcinogen by the International Agency for Research on Cancer ([IARC], 2013). During chemotherapy, patients received bolus IV doses of CPA regularly through an outpatient service. The current study was conducted with primary objectives of (a) measuring the total amount of CPA excreted in the urine of patients with cancer during the first seven days after CPA administration and (b) evaluating the risk of exposure to family members by measuring the urine CPA levels of cohabitants during the same period.
Methods
Eight female patients with breast cancer who periodically received CPA in the outpatient chemotherapy center at a university hospital in Japan and 10 family members living with these patients participated in this study. Ten healthy volunteers who matched with the family members for gender, age, and smoking status were enrolled as a control group. None of the participants had comprehension issues, and they collected their urine samples at home. The Eastern Cooperative Oncology Group performance status for each patient was grade 0 (Oken et al., 1982).
Ethical Considerations
This study was conducted with the approval of the ethics committee of Fukushima Medical University in Japan. A researcher interviewed patients with breast cancer who had been referred by their physicians in outpatient service. The researcher explained the objectives and methods of the study to potential participants through written and oral descriptions. After treatment, the researcher visited patients’ homes to explain the same information to family members. It was explained that nonparticipation would not cause any disadvantages, and that they were allowed to withdraw at any time even after they had consented to participate. Potential participants were assured that privacy would be strictly observed. Participants gave written consent if they agreed to take part in the study.
Urine Sampling
Once patients completed chemotherapy infusion at the outpatient center, a researcher visited them in their homes and repeated the explanation of the tests and procedures for urine sample collection. Patients and their family members recorded the time and volume of each urination for seven consecutive days at home after chemotherapy was administered. They collected 10 ml samples of each urination using a sampling kit, and the samples were immediately stored in a compact freezer used solely for the purpose of storing the samples at −20°C. Patients also collected a test sample when they urinated at the hospital after receiving chemotherapy. Participants in the control group also collected urine for seven consecutive days at home; however, collection was terminated by some patients after four days because of personal circumstances.
Urine Sample Analyses
All samples were shipped on dry ice to a laboratory for analysis. To determine CPA levels, the unchanged form of CPA was detected and measured in the urine samples of patients, their family members, and the control subjects. The sample volume used for CPA de-termination in urine was 5 ml. The detection limit of CPA was 0.01 ng/ml for family members and control subjects and 100 ng/ml for patients (samples were diluted 5,000-fold prior to clean-up and analysis). Urine samples were prepared according to standard procedures (Sessink, Anzion, Van den Broek, & Bos, 1992; Sessink, Boer, Scheefhals, Anzion, & Bos, 1992; Sessink, Scholtes, Anzion, & Bos, 1993). CPA was analyzed using gas chromatography (GC) in tandem with a mass spectroscopy (MS) system.
GC-MS is a technique used for the qualitative and quantitative analysis of organic compounds in which a vaporized mixture is chromatographically separated into its components. GC refers to a type of chromatography that uses a gaseous mobile phase. A qualitative analysis of GC-separated components is accomplished by individually subjecting them to MS as they are eluted from the chromatography column. Quantitative analysis of the individual components is determined by their peak intensities in the chromatogram.
Findings
During the first seven days after chemotherapy, 276 and 243 urine samples were collected from eight patients and their 10 family members, respectively (see Tables 1 and 2). During this period, 40% of the urine samples collected from the patients contained detectable levels of CPA. The total amount of CPA excreted by patients during the seven days was 108.3–181.5 ng, representing 13%–24% of the dose administered during chemotherapy. The collection times for the last samples containing CPA were 38–114 hours after chemotherapy, and they were greater than 48 hours for 63% of patients. None of the patients vomited during the study period.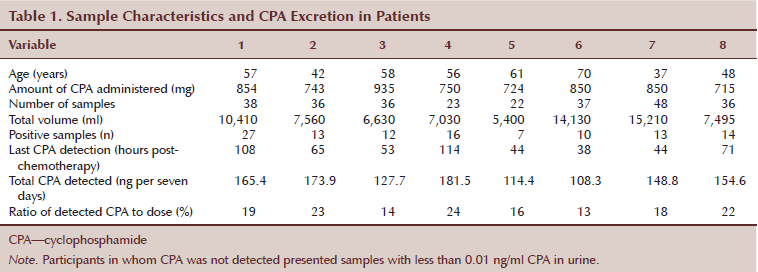
Family members frequently were found to be contaminated with CPA, which was detected in 21% of the 243 urine samples, representing six of the 10 family members. The total amount of CPA detected in family members’ urine was highly variable, ranging from 17–252 ng per member. The collection times for the last samples containing detectable CPA levels ranged from 42–154 hours after chemotherapy. The amount of CPA excreted by most family members (four out of six) was comparable to the amount excreted by the patients (≥ 101.5 ng). None of the 204 urine samples collected from the 10 control subjects contained detectable levels of CPA. Therefore, family members living with patients receiving chemotherapy are at a high risk for drug exposure if they do not take appropriate personal protective measures.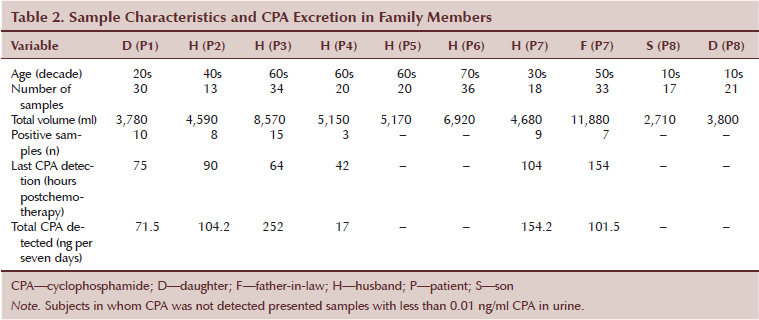
The time-course profiles of CPA excretion in the urine samples of patients and their family members during the first seven days after chemotherapy were compared. The family members of patients 1, 2, 3, 4, and 7 showed detectable CPA levels. In patients, CPA excretion gradually declined during the first four days. In contrast, the profiles of family members exhibited no clear peaks. In most cases, CPA concentration peaks were higher in family members than in patients 48 hours post-treatment (see Figures 1 and 2). The exposure variability among family members could be explained by the duration of close contact with patients in common spaces. In the case of patient 7, both family members were exposed to the drug but with different lag times for the first detection of CPA in their urine (see Figure 3). CPA was continuously excreted in the urine of patient 7’s husband 54–104 hours post-treatment, whereas the father-in-law intermittently excreted CPA. In contrast, the two family members of patient 8 were not exposed to the drug, which may be partially explained by the fact that they used separate bathrooms. The family member of patient 5 showed no sign of CPA exposure, perhaps because they did not use the same bathroom and their work shifts did not overlap. These data suggest that the main factors responsible for family members’ secondary CPA exposure from autonomous patients with cancer at home are shared bathrooms and amount of time spent in common space.
[[{"type":"media","view_mode":"media_original","fid":"20186","attributes":{"alt":"","class":"media-image","height":"370","typeof":"foaf:Image","width":"502"}}]]
Discussion
This study compared the amount of CPA excreted in the urine of patients with cancer and their cohabiting family members during the first seven days after chemotherapy. The total amount of CPA excreted by the patients during this period was 108.3–181.5 ng, representing 13%–24% of the total administered dose. These data are consistent with the findings of a previous study, which showed that 3%–36% of CPA is excreted in the urine of patients after chemotherapy (Hedmer, Tinnerberg, Axmon, & Jonsson, 2008). In addition, as much as 30% of an IV dose of CPA is excreted in the urine of patients with cancer within two days after drug administration (OSHA, 1995). This large variability is explained by individual differences in drug metabolism. To minimize exposure to hazardous drugs, safety guidelines recommend that healthcare workers handling body fluids or beddings use personal protective equipment during the 48 hours after chemotherapy (ASHP, 1990; OSHA, 1995; Polovich, 2011). However, the results of this study showed that 63% of patients still excreted significant amounts of CPA three days after chemotherapy. Therefore, the recommended use of personal protective equipment should be extended to five days for all hospital personnel in close contact with patients receiving chemotherapy.
[[{"type":"media","view_mode":"media_original","fid":"20191","attributes":{"alt":"","class":"media-image","height":"370","typeof":"foaf:Image","width":"542"}}]]
The home environment is more problematic than hospitals regarding secondary drug exposure because family members do not wear protective equipment and common spaces are not sterilized on a daily basis. Large concentrations of CPA were detected in samples collected from the family members of most (five out of eight) patients. Most family members (four out of six) exposed to CPA excreted total drug amounts comparable to those excreted by the patients (≥ 101.5 ng), which is comparable to the exposure level of healthcare workers in hospital settings (Sessink et al., 1992; Sessink, Kroese, van Kranen, & Bos, 1995).
[[{"type":"media","view_mode":"media_original","fid":"20196","attributes":{"alt":"","class":"media-image","height":"466","typeof":"foaf:Image","width":"761"}}]]
Several studies at medical facilities reported the presence of antineoplastic drugs in the urine of healthcare workers who had not directly handled antineoplastic agents, indicating secondary exposure from environmental contamination (Pethran et al., 2003; Wick, Slawson, Jorgenson, & Tyler, 2003). Nurses are exposed to antineoplastic drugs through their skin while removing contaminated bed sheets belonging to patients receiving chemotherapy (Fransman et al., 2005). In the current study, although family members did not directly handle patients’ body fluids, six family members of five patients were exposed to the drug. This highlights the existence of residual body fluids containing CPA in the home environment. An environmental monitoring study conducted in the home bathrooms of two patients detected drug contamination on the toilet seat, bathroom floor, and door knobs 48 hours after CPA administration. The levels of contamination were much higher than those in hospital areas (e.g., pharmacy) (Yuki et al., 2013). These data are consistent with the persistently high levels of CPA detected in this study in family members even after CPA levels decreased to less than 80% in patients. These findings indicate that the safety guidelines designed to prevent drug exposure during the first 48 hours post-treatment are not appropriate for family members of patients postchemotherapy, particularly when dealing with the residual body fluids that accumulate in the home environment.
Implications for Nursing
Patients in this study excreted large amounts of CPA because of their chemotherapy, and the administered drugs were detected in urine samples collected from cohabiting family members. Although these family members did not receive chemotherapy, CPA was detected in their urine samples during the postadministration period, indicating secondary exposure from environmental surface contamination at home.
The prevention of contamination with antineoplastic agents at home should be stressed to avoid the exposure of family members to these toxic drugs. Yuki et al. (2013) demonstrated the contamination of the home setting and exposure of family members to CPA via the drug residue (such as excreta) of patients receiving chemotherapy.
Guidelines recommend procedures to prevent drug exposure for healthcare workers in hospitals and institutions (ASHP, 1990; OSHA, 1995; Polovich, 2011). The instructions given to patients and their families to prevent exposure to antineoplastic drugs at home are based on these procedures. However, patients and family members rarely use disposable gloves and gowns when handling potentially contaminated blood, urine, feces, or vomit. These guidelines also state that caution should be exercised when flushing the toilet (performed twice after appropriately lowering the toilet seat lid) following the disposal of excreta of patients administered cytotoxic drugs within the previous 48 hours. Applying measures to prevent drug contamination of the toilet environment, including the toilet seat, floor around the toilet, door knob, and washbasin, and taking precautions when handling clothing and linens that have been in contact with the patient’s urine and other body fluids, is necessary.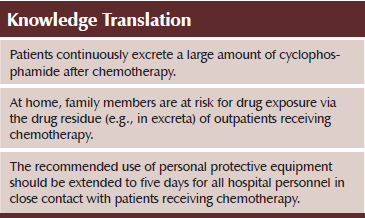
Conclusion
The findings of this study raise an important public health issue. As anticancer chemotherapy in outpatient settings is more commonly practiced, family members may be exposed to high doses of antineoplastic drugs for as many as five days post-treatment. Therefore, an urgent need exists for the development of safety guidelines adapted to the home environment to prevent the secondary exposure of cohabiting family members.
References
Althouse, R., Huff, J., Tomatis, L., & Wilbourn, J. (1979). Chemicals and industrial processes associated with cancer in humans (IARC Monographs, Vol. 1–20). IARC Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans. Supplement, 1, 1–71.
American Society of Hospital Pharmacists. (1990). ASHP technical assistance bulletin on handling cytotoxic and hazardous drugs. American Journal of Hospital Pharmacy, 47, 1033–1049.
Burgaz, S., Karahalil, B., Canli, Z., Terzioglu, F., Ancel, G., & Anzion, R.B. (2002). Assessment of genotoxic damage in nurses occupationally exposed to antineoplastics by the analysis of chromosomal aberrations. Human and Experimental Toxicology, 21, 129–135. doi:10.1191/0960327102ht230oa
Cardonick, E., & Iacobucci, A. (2004). Use of chemotherapy during human pregnancy. Lancet Oncology, 5, 283–291. doi:10.1016/S1470-2045(04)01466-4
Fransman, W., Roeleveld, N., Peelen, S., de Kort, W., Kromhout, H., & Heederik, D. (2007). Nurses with dermal exposure to antineoplastic drugs: Reproductive outcomes. Epidemiology, 18, 112–119. doi:10.1097/01.ede.0000246827.44093.c1
Fransman, W., Vermeulen, R., & Kromhout, H. (2005). Dermal exposure to cyclophosphamide in hospitals during preparation, nursing and cleaning activities. International Archives of Occupational and Environmental Health, 78, 403–412. doi:10.1007/s00420-004-0595-1
Hedmer, M., Tinnerberg, H., Axmon, A., & Jonsson, B.A. (2008). Environmental and biological monitoring of antineoplastic drugs in four workplaces in a Swedish hospital. International Archives of Occupational and Environmental Health, 81, 899–911. doi:10.1007/s00420-007-0284-y
Hemminki, K., Kyyronen, P., & Lindbohm, M.L. (1985). Spontaneous abortions and malformations in the offspring of nurses exposed to anesthetic gases, cytostatic drugs, and other potential hazards in hospitals, based on registered information of outcome. Journal of Epidemiology and Community Health, 39, 141–147. doi:10.1136/jech.39.2.141
Hon, C.Y., Teschke, K., Demers, P.A., & Venners, S. (2014). Antineoplastic drug contamination on the hands of employees working throughout the hospital medication system. Annals Occupational Hygiene, 58, 761–770. doi:10.1093/annhyg/meu019
International Agency for Research on Cancer. (2013). IARC monographic on the evaluation of the carcinogenic risk: The IARC monographs, volumes 1-109. Retrieved from http://monographs.iarc.fr/ENG/Classification/
Kusnetz, E., & Condon, M. (2003). Acute effects from occupational exposure to antineoplastic drugs in a para-professional health care worker. American Journal of Industrial Medicine, 44, 107–109. doi:10.1002/ajim.10230
Mader, R.M., Rizovski, B., Steger, G.G., Wachter, A., Kotz, R., & Rainer, H. (1996). Exposure of oncologic nurses to methotrexate in the treatment of osteosarcoma. Archives of Environmental Health, 51, 310–314. doi:10.1080/00039896.1996.9936030
McDiarmid, M.A., Oliver, M.S., Roth, T.S., Rogers B., & Escalante, C. (2010). Chromosome 5 and 7 abnormalities in oncology personnel handling anticancer drugs. Journal of Occupational and Environmental Medicine, 52, 1028–1034. doi:10.1097/JOM.0b013e3181f73ae6
Meijster, T., Fransman, W., Veldhof, R., & Kromhout, H. (2006). Exposure to antineoplastic drugs outside the hospital environment. Annals of Occupational Hygiene, 50, 657–664. doi:10.1093/annhyg/mel023
Meirow, D., & Schiff, E. (2005). Appraisal of chemotherapy effects on reproductive outcome according to animal studies and clinical data. Journal of the National Cancer Institute. Monographs, 34, 21–25. doi:10.1093/jncimonographs/lgi025
Nygren, O., & Lundgren, C. (1997). Determination of platinum in workroom air and in blood and urine from nursing staff attending patients receiving cisplatin chemotherapy. International Archives of Occupational and Environmental Health, 70, 209–214. doi:10.1007/s004200050209
Occupational Safety and Health Administration. (1995). OSHA technical manual: Controlling occupational exposure to hazardous drugs (Occupational Safety and Health Administration, Section 6, Ch. 2). Retrieved from www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
Oken, M.M., Creech, R.H., Tormey, D.C., Horton, J., Davis, T.E., McFadden, E.T., & Carbone, P.P. (1982). Toxicity and response criteria of the Eastern Cooperative Oncology Group. American Journal of Clinical Oncology, 5, 649–655. doi:10.1097/00000421-198 212000-00014
Pethran, A., Schierl, R., Hauff, K., Grimm, C.H., Boos, K.S., & Nowak, D. (2003). Uptake of antineoplastic agents in pharmacy and hospital personnel. Part I: Monitoring of urinary concentrations. International Archives of Occupational and Environmental Health, 76, 5–10.
Polovich, M. (2011). Safe handling of hazardous drugs (2nd ed.). Pittsburgh, PA: Oncology Nursing Society.
Sessink, P.J., Anzion, R.B., Van den Broek, P.H., & Bos, R.P. (1992). Detection of contamination with antineoplastic agents in a hospital pharmacy department. Pharmaceutisch Weekblad Scientific Edition, 14, 16–22. doi:10.1007/BF01989220
Sessink, P.J., Boer, K.A., Scheefhals, A.P., Anzion, R.B., & Bos, R.P. (1992). Occupational exposure to antineoplastic agents at several departments in a hospital. Environmental contamination and excretion of cyclophosphamide and ifosfamide in urine of exposed workers. International Archives of Occupational and Environmental Health, 64, 105–112. doi:10.1007/bf00381477
Sessink, P.J., Kroese, E.D., van Kranen, H.J., & Bos, R.P. (1995). Cancer risk assessment for health care workers occupationally exposed to cyclophosphamide. International Archives of Occupational and Environmental Health, 67, 317–323. doi:10.1007/BF00385647
Sessink, P.J., Scholtes, M.M., Anzion, R.B., & Bos, R.P. (1993). Determination of cyclophosphamide in urine by gas chromatography-mass spectrometry. Journal of Chromatography, 616, 333–337. doi:10.1016/0378-4347(93)80404-R
Skov, T., Lynge, E., Maarup, B., Olsen, J., Rorth, M., & Winthereik, H. (1990). Risks for physicians handling antineoplastic drugs. Lancet, 336, 1446. doi:10.1016/0140-6736(90)93148-i
Walusiak, J., Wittczak, T., Ruta, U., & Palczynski, C. (2002). Occupational asthma due to mitoxantrone. Allergy, 57, 461.
Wick, C., Slawson, M.H., Jorgenson, J.A., & Tyler, L.S. (2003). Using a closed-system protective device to reduce personnel exposure to antineoplastic agents. American Journal of Health-System Pharmacy, 60, 2314–2320.
Yuki, M., Sekine, S., Takase, K., Ishida, T., & Sessink, P.J. (2013). Exposure of family members to antineoplastic drugs via excreta of treated cancer patients. Journal of Oncology Pharmacy Practice, 19, 208–217. doi:10.1177/1078155212459667
About the Author(s)
Michiko Yuki, RN, PhD, is a professor in Health Sciences at Hokkaido University in Sapporo, Japan, and the Department of Public Health Nursing at Fukushima Medical University in Japan; Takashi Ishida, MD, is director of the Clinical Oncology Center and an associate professor in the Department of Pulmonary Medicine at Fukushima Medical University; and Satoko Sekine, MD, is a doctor of pulmonary medicine at Fukushima Medical University. The study was funded by a grant from the Secom Science and Technology Foundation. Mention of specific products and opinions related to those products do not indicate or imply endorsement by the Oncology Nursing Forum or the Oncology Nursing Society. Yuki can be reached at yukimck@hs.hokudai.ac.ip, with copy to editor at ONFEditor@ons.org. (Submitted March 2014. Accepted for publication May 8, 2015.)

