Patient-Perceived Access to Care When Actively Seeking Treatment
Purpose/Objectives: To examine predictors of perceived access to care and reported barriers to care of patients with cancer actively seeking treatment.
Design: Retrospective secondary data analysis.
Setting: U.S. Medical Expenditure Panel Survey, a national survey with questions about healthcare coverage and access.
Sample: 1,170 adults with cancer actively seeking treatment.
Methods: A retrospective analysis of data. Bivariate tests for significant association between individual characteristics and low perceived access to care were conducted using a chi-square test.
Main Research Variables: The dependent variable was perceived access to care. The independent variables included sex, age, race, poverty status, education level, marital status, cancer site, comorbidities, and insurance status.
Findings: Those with Medicaid insurance or no health insurance had significantly lower perceived access to care compared to those with Medicare. Institutional barriers to treatment, such as financial or insurance, were the most common reported barriers.
Conclusions: Most adults with cancer reported adequate access to medical care and medications, but a small yet vulnerable population expressed difficulties in accessing treatment.
Implications for Nursing: To effectively advocate for vulnerable populations with Medicaid or no insurance, nurses may require specialized knowledge beyond the scope of general oncology nursing.
Jump to a section
Almost 30 years of progress in cancer survival rates have not been equally distributed throughout the U.S. population (Byers, 2010). Risk for cancer mortality differs by health insurance status in the United States (Han et al., 2014; Shi et al., 2013), and these disparities persist when controlling for cancer stage at diagnosis (Bradley, Given, & Roberts, 2002; Halpern et al., 2008; Koroukian, Bakaki, & Raghavan, 2011). Therefore, the National Cancer Institute ([NCI], 2015) recommends prioritizing access to cancer care in research. Few studies have examined delays and barriers to care among patients with cancer during treatment by various insurance types (Fedewa, Ward, Stewart, & Edge, 2010; Massarweh et al., 2014; Scoggins et al., 2011). To identify disparities in treatment access among people diagnosed with cancer, the current authors used a national survey dataset. They explored the factors associated with the perceptions of access to care of patients diagnosed with cancer who were currently undergoing specialist care treatment and also examined reported barriers to timely treatment or pharmaceuticals.
Barriers to health service use, influencing health behaviors and interacting at multiple levels, may be conceptualized using an ecological perspective to health promotion (McLeroy, Bibeau, Steckler, & Glanz, 1988; NCI, 2005; Scheppers,van Dongen, Dekker, Geertzen, & Dekker, 2006). The current authors applied an ecological model to barriers experienced during the treatment phase and categorized reported barriers into three levels: intrapersonal, interpersonal, and institutional. Intrapersonal barriers are individual characteristics that affect health behaviors, including transportation, attitudes, and comorbidities. Interpersonal barriers involve relations to other people, such as employment issues, child care, communication with providers, and marital status. Institutional barriers are rules, regulations, and policies of organizations, including cost of care, insurance limitations, and provider access problems (e.g., long waits for appointments).
Because access to cancer treatment affects cancer survival, oncology nurse navigation (ONN) was developed to remove barriers for individual patients, their families, and caregivers (Oncology Nursing Society, Association of Oncology Social Work, & National Association of Social Workers, 2010). The aims of ONNs are to help patients achieve timely access to high-quality medical and psychosocial care throughout all phases of cancer care (Freeman & Rodriguez, 2011). ONN interventions are most commonly provided during one or more phases of the care continuum, including screening, diagnosis follow-up, treatment, and survivorship (Wells et al., 2008). The period after diagnosis follow-up and before cancer survival is known as the treatment phase, where about 25% of ONN efforts are focused (Brown et al., 2012).
Although ONN intervention during the screening and diagnosis follow-up phases is mostly successful, the evidence for treatment phase ONN interventions remains inconclusive (Paskett, Harrop, & Wells, 2011; Wells et al., 2008). Only a small number of studies have concentrated on the treatment phase; most focus mainly on screening and diagnosis follow-up. In addition, the few studies that have addressed the treatment phase contain methodological issues that limit the results. For example, Ell et al. (2009) applied financial and insurance assistance interventions, previously identified as effective, to control and intervention groups, which rendered differences between groups undetectable. This suggests that financial and insurance-related barriers during the treatment phase of cancer care may exist for certain patients, but the few studies that have analyzed this relationship either had a restricted sample of only patients with breast cancer (Fedewa et al., 2010) or solely addressed travel barriers among those insured with Medicaid (Massarweh et al., 2014; Scoggins et al., 2011).
Addressing the gap in evidence regarding access to care during the treatment phase is necessary. Therefore, the current authors narrowed the study population to adult patients in the United States who were actively seeking care. The association between independent variables and perceived access to care was tested, and the authors hypothesized that insurance status had the strongest association with patient-perceived access to care during the treatment phase, adjusting for demographic, socioeconomic, and health status factors. The barriers to care reported by respondents with the lowest perceived access to care within the ecological model of health promotion were also summarized.
Methods
The current authors conducted a retrospective analysis of data from the 2012 Medical Expenditure Panel Survey (MEPS) Health Component. MEPS was produced by the Agency for Healthcare Research and Quality and includes questions on healthcare coverage, costs, use, and access. MEPS is a nationally representative survey of noninstitutionalized civilian families and individuals in the United States. The survey employs stratified random sampling, which oversamples certain underrepresented groups, such as those diagnosed with cancer, to ensure representativeness. This study was determined exempt by the institutional review board of the University of South Florida because the database employed can be accessed by the public and is deidentified.
The dataset included adults aged 18 years or older and surveyed via the 2012 MEPS, the last year in which the survey results used in this analysis were available. Only individuals with cancer who were eligible to complete the supplemental questionnaire regarding access to care were included in the study. Finally, to identify individuals seeking active treatment, only those naming a usual source of care (i.e., a person or facility) whose providers believed they needed treatment, who had visited a provider at least once in the past year, and who had ongoing specialist treatment as their usual source of care were included.
Perceived care is a meaningful outcome, because the perception of lack of access to care can influence health-seeking behaviors and objective access to care (Scheppers et al., 2006). In the current study, a new perceived access to care score (PACS) was created by combining the responses of four MEPS items, including ease of access to needed care, timeliness of healthcare appointments, delay in obtaining needed treatment, and delay in obtaining needed medications. The dependent variable of this study was the PACS group, defined dichotomously. PACSs for individuals were tallied and divided into quartiles, which were categorized into two groups—a group with the lowest scores and a group with all higher scores. Therefore, the authors created a binary dependent variable that included individuals in the lowest quartile group who were compared to everyone else.
More specifically, each participant’s response was assigned a point value of 1 (lowest perceived access to care) to 4 (highest perceived access to care). If the individual answered “always” to “How often was it easy to get the care, tests, or treatment you or a doctor believed was necessary?” he or she would gain four points. If the individual answered “never” to that question, he or she would gain one point. The sum of points for the four questions equaled each participant’s PACS. The discrete PACS for each person ranged from 4, indicating the lowest perceived access to care, to 16, indicating the highest perceived access to care. Table 1 shows the MEPS questions, response options, and point values for calculating the PACS. 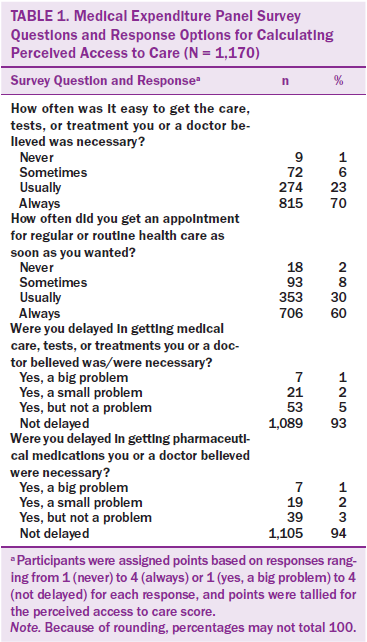
To identify the factors associated with the lowest perceived access to care group dependent variable, the current authors used multiple independent variables that represented key demographic, socioeconomic, and health status factors. Bivariate tests for significant association between individual characteristics and low perceived access to care were conducted using a chi-square test for independence.
The key independent variable of interest was the presence and type of U.S. health insurance, categorized as commercial, Medicare, or Medicaid/other government. Commercial insurance is private insurance commonly obtained through employers. Medicare is the federal government–sponsored insurance available to qualified individuals older than age 65 years and some disabled adults. Medicaid is state government insurance for individuals with low incomes. The Medicaid/other government category included state and local government–run insurance programs provided to otherwise uninsured individuals. The authors categorized the small group of individuals (n =70) who were dually eligible for Medicare and Medicaid in the Medicaid/other government category, because some of them may not have been able to afford out-of-pocket Medicare expenses (e.g., premiums, deductibles). Some beneficiaries qualify for support from Medicaid programs to cover these costs, but not all dually eligible individuals qualify (Gold, Jacobson, & Garfield, 2012). Therefore, assigning dually eligible individuals to the Medicaid/other government insurance group recognized the potential access barriers similar to those of the patients who were eligible only for Medicaid (Rowland, 2015). Finally, TRICARE, the U.S. Department of Defense’s healthcare program, was categorized as commercial insurance.
Additional independent variables included sex, age, race, poverty level, education level, and marital status. The authors’ model included the reported cancer sites—breast, colon, cervix, melanoma, prostate, nonmelanoma of the skin, and other cancers, which included bladder, brain, leukemia, lung, lymphoma, prostate, throat, and thyroid (cancers listed in MEPS). Individuals with more than one cancer were categorized as multisite. Model references used nonmelanoma of the skin as the reference category, because this cancer is quickly and easily treated and, logically, has the least treatment access challenges (American Society of Clinical Oncology, 2015).
Comorbidities may affect patient-reported health outcomes (Smith et al., 2008), so the model also adjusted for noncancer diagnoses (e.g., myocardial infarction, congestive heart failure) by using a modificationof a widely employed severity adjustment methodology, the Charlson Comorbidity Index (CCI) (Charlson, Pompei, Ales, & MacKenzie, 1987; Deyo, Cherkin, & Ciol, 1992). To create the severity adjustment groups, a weight was assigned for each relevant diagnosis code (ICD-9-CM), and the weights were totaled for each person to provide a total comorbidity score. The authors modified the CCI by not scoring a diagnosis of cancer unless it was a metastatic solid tumor (Deyo et al., 1992). Adjusting for comorbidities was consistent with comparable studies that examined the association of patients’ insurance status with access to cancer treatments (Fedewa et al., 2010; Massarweh et al., 2014).
For the main analysis, a multivariable logistic regression model that examined factors associated with the lowest perceived access group, compared to higher quartiles, was developed. The non-normal and negatively skewed PACS distribution made multiple linear regression infeasible. Instead, the model predicted membership in the lowest perceived access to care quartile compared to all higher quartiles. By using a binary dependent variable, logistic regression predicts the likelihood that an individual would be present in the lowest perceived access quartile group after considering the values of the independent variables (Hosmer, Lemeshow, & Sturdivant, 2000). All statistical tests were two-sided, and a 0.05 probability of a Type I error was used.
In addition, the authors explored commonly identified barriers to care among individuals in the lowest quartile group. MEPS data provide additional information on the barriers related to survey questions 3 and 4. For example, question 3 includes a follow-up question regarding the reason for unattained treatment: “What reason were you unable to get necessary medical care, tests, or treatments you or a doctor believed was/were necessary?” Responses were limited to one option, which was assumed by the authors to be the most important reason. The authors analyzed the responses and categorized them into three levels of the ecological model: intrapersonal, interpersonal, and institutional.
Results
The dataset included 28,090 adults aged 18 years or older. Among those individuals, 2,284 had been diagnosed with cancer and 2,157 were eligible to take the supplemental questionnaire regarding access to care. The final study sample included 1,170 participants who met inclusion criteria.
Analysis of the national survey dataset revealed that few patients with cancer reported access to care difficulties. For example, the majority of respondents reported that it was “always” (n = 815, 70%) or “usually” (n = 274, 23%) “easy to get the care, tests, or treatment you or a doctor believed was/were necessary.” However, perceived access challenges existed in the results, with a small proportion reporting that it was “sometimes” (n = 72, 6%) or “never” (n = 9, 1%) easy to get necessary care. These results were consistent with those of the other three survey questions comprising the PACS.
Prior to analysis, the authors defined the PACS dependent variable measure as binary, with the lowest PACS quartile group and the higher quartile group. Patients in the lowest perceived access group had a PACS of 13 or less. One hundred eighty-four individuals were categorized below this point, identified as the lowest perceived access group. Although the proportion of individuals in the lowest PACS quartile was less than 25%, if the cutoff PACS was adjusted to 14 or higher, the proportion of people in the lowest perceived group would have exceeded 25%. All remaining higher quartiles of PACS included 986 individuals. The non-normal PACS distribution was negatively skewed with a mean of 14.8, median of 16, standard deviation of 1.7, minimum of 6, and maximum of 16. 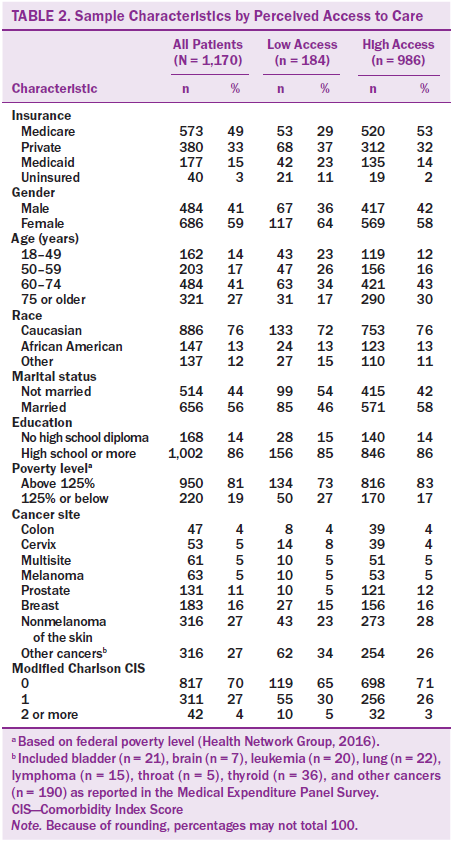
Table 2 shows the characteristics of adults diagnosed with cancer, including the total sample, the lowest perceived access group, and all higher perceived access groups, as well as the chi-square tests of independence results, which revealed significant association (p < 0.05) between multiple characteristics, including insurance status (chi-square = 68.85, p < 0.001), age (chi-square = 34.35, p < 0.001), marital status (chi-square = 8.64, p <0.01), family income (chi-square = 8.89, p < 0.01), and cancer site (chi-square = 15.94, p < 0.05), and low perceived access to care.
The authors’ multivariate logistic regression model depicted a significant association between low perceived access to care and insurance status (p < 0.05). Adults with cancer with Medicaid had a 2.71 increased odd (95% confidence interval [CI] [1.04, 3.27]) of being in the low perceived access to care quartile compared to those with Medicare (p = 0.04). In addition, uninsured respondents had a 1.85 increased odd (95% CI [2.92, 14.99]) of being categorized in the low perceived access to care group compared to those with Medicare (p < 0.001).
The adjusted odds ratios and 95% CIs for the study variables are summarized in Table 3. The multivariate logistic model results were abbreviated, leaving out the insignificant independent variables, such as family income level and the modified CCI groups, which were retained in the model but did not affect the results. All interaction terms were statistically insignificant and were excluded from the model.
Compared to intrapersonal and interpersonal barriers, institutional barriers were most commonly reported by those with low perceived access to care. Could not afford care was the most frequently reported reason for delayed medical care, tests, treatments (n = 24, 30%), delayed medications (n = 31, 48%), or either (a) delayed medical care, tests, or treatment or (b) delayed medications (n = 45, 34%). Challenges with health insurance were the second most common institutional barrier. Few individuals reported intrapersonal barriers (n = 13, 10%), such as problems getting to doctor’s office, which was the most important intrapersonal barrier, and even fewer identified interpersonal barriers (n = 9, 7%), such as communication with providers, the most important interpersonal barrier. Barriers classified as other were also common, totaling 27 (33%) for delayed medical care, tests, or treatments; 17 (26%) for delayed medications; and 42 (32%) for either type of delay. MEPS did not specify “other” barriers in the dataset. Table 4 summarizes barriers to care reported by respondents in the lowest quartile group. Frequency of responses is organized into three ecological model categories (rows) and three access-related issues (columns).
Respondents in the low perceived access to care group frequently reported delays in care because of institutional barriers. Uninsured patients were significantly more likely to report institutional barriers compared to those with all other types of insurance (chi-square = 51.7, p < 0.001).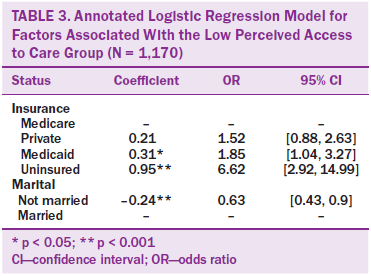
Discussion
Based on a national survey of adults with cancer currently receiving care, the current study revealed that those with Medicaid or no health insurance were more likely to report low perceived access to care compared to those with Medicare. The results were consistent with existing evidence in which insurance status is associated with access to care challenges during the treatment phase for patients diagnosed with cancer (Fedewa et al., 2010; Gwyn et al., 2004). In addition, the institutional barriers, particularly cost of care, were most common among those reporting the lowest perceived access to care.
Consistent with other research, the findings revealed that the majority of patients diagnosed with cancer reported few delays, but the vulnerable few with access challenges could be identified by their insurance type. A study by Yabroff et al. (2013) revealed that about 9 of 10 cancer survivors and noncancer respondents obtained adequate access to care. However, the uninsured and publicly insured were more likely to report challenges. Together, these findings provide an important reference point for additional research of the effects of insurance coverage on patient-perceived access to cancer care.
The current findings should be evaluated in the context of the changes to insurance coverage in the United States. The landmark Patient Protection and Affordable Care Act (ACA) of 2010 extended health insurance coverage to millions more people in the United States through two main policies (Kaiser Commission on Medicaid and the Uninsured, 2016; Moy et al., 2011). The ACA has extended health insurance coverage to millions more people in the United States through two main policies (Kaiser Commission on Medicaid and the Uninsured, 2016). First, individuals may buy private insurance through a new health insurance exchange, a collection of private health plans offered through a web-based marketplace, and federal subsidies make the insurance policies on the exchange more affordable for those who qualify (Kaiser Commission on Medicaid and the Uninsured, 2016). Also, the ACA expanded Medicaid insurance to millions of low-income people by raising the income limit in states that choose to implement the policy option (Crowley & Golden, 2014). The increased insurance coverage heightens the demand for health services, including cancer treatment (Martin, Hartman, Benson, & Catlin, 2015). However, potential repeal and replacement of the ACA may lead to a disruption to gains made in the number of insured individuals and breadth of their health insurance coverage (Eltorai & Eltorai, 2017). 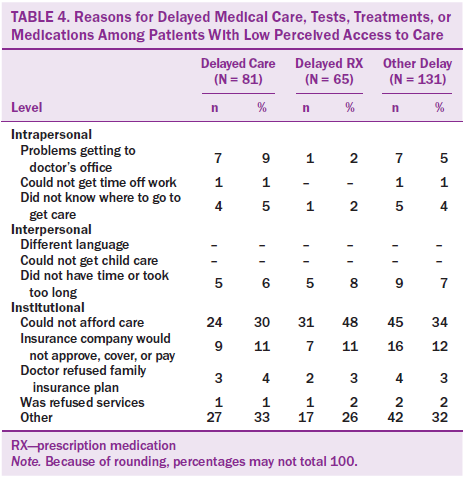
Even if ACA laws remain in place, more than 32 million people in the United States remained uninsured in 2015 (Kaiser Commission on Medicaid and the Uninsured, 2016). Among them are about 3 million people with low incomes living in the states that chose not to expand Medicaid (Kaiser Commission on Medicaid and the Uninsured, 2016). As reflected in the current results, lack of insurance puts treatment for cancer, which can be very expensive, out of reach for many (Dusetzina, Basch, & Keating, 2015). Therefore, uninsured patients diagnosed with cancer reporting institutional access barriers was not surprising.
However, financial and insurance-related challenges were commonly reported even by patients with Medicaid, confirming past findings regarding an underinsurance problem among patients with cancer (Tejeda et al., 2013). Research on access to cancer should consider multiple dimensions of underinsurance as it relates to Medicaid insurance (Lavarreda, Brown, & Bolduc, 2011). For example, the ACA has covered millions more in the state government–based Medicaid insurance system, but whether the providers can accommodate the additional volume of patients diagnosed with cancer is unknown (Sommers & Kronick, 2016). Early research on noncancer services has not revealed an association between access to care problems and Medicaid expansion policies (Ndumele, Mor, Allen, Burgess, & Trivedi, 2014; Tipirneni et al., 2015). Also, Medicaid insurance payment rates to providers often are significantly lower than those of privately financed insurance and Medicare, leading providers to reject patients insured by Medicaid (Zuckerman & Goin, 2012). Future research should evaluate whether payment rates or the level of provider participation affects Medicaid patients’ access to cancer care.
Limitations
This study has four main limitations. First, although MEPS is appropriate and a widely cited data source for the assessment of barriers to cancer treatment (Fiscella et al., 2011), the selected survey questions and PACS composite have not been validated for measuring patient-perceived access to care. The MEPS tool was not specifically designed for adult cancer-related access to treatment but rather for all types of care. When evaluating the reported barriers for perceived access, only one reason for limited access to care was recorded in the survey. Other unreported contributing barriers that significantly delay the receipt of treatment or prescription medications may exist. Also, insurance coverage was identified for each person at a single point in time during the survey, and the authors assumed continuous enrollment in the indicated insurance status for the analysis. Whether intermittent or continuous enrollment in a specific type of insurance would affect the results is unknown. Finally, this study measured patient-perceived access to treatment instead of the more precise access to care outcomes, such as treatment completion duration, commonly measured for ONN programs.
Implications for Nursing
Access to care is an important challenge for a small but vulnerable group of patients without insurance or with Medicaid. With the implementation of the ACA, increased insurance coverage (Kaiser Commission on Medicaid and the Uninsured, 2016) is expected to enable earlier cancer detection, more timely treatment, and improved outcomes for vulnerable populations in the United States (Moy et al., 2011). However, potential legislative actions by the 115th Congress (2017–2018) and/or regulatory actions by the Trump administration may increase the number of patients with cancer without insurance. Depending on the success of repealing and replacing the ACA, the number of people covered by Medicaid could decrease dramatically, and the consumer protections for individuals with preexisting coverage, including cancer, could be weakened (Eltorai & Eltorai, 2017). Although nurses welcome the opportunity to connect individuals with resources they need to get healthy (Daley, 2013), additional administrative complexities present a challenge to nurses, who should become more knowledgeable about the various financial and insurance-related barriers that impede patient access to cancer care (Spetz, 2014).
As ONN programs continue to expand beyond their currently limited implementation (Pruitt & Sportsman, 2013), ONN likely will be increasingly responsible for removing prevalent institutional barriers. Specialized knowledge beyond the scope of general oncology nursing, including the intricacies of the healthcare system, may be required to effectively advocate for patients (Brown et al., 2012; McMullen, 2013). However, this knowledge may not be emphasized in nursing education, particularly at the prelicensure level. For ONN programs to succeed, sponsoring organizations must provide training regarding the financial resources available from the healthcare organization and community at large.
The 2016 ONN role delineation study identified practical jobs tasks of the oncology nurse navigator, such as coordinating financial resources and collaborating with multidisciplinary colleagues to learn best practices (Lubejko et al., 2017). Job-function activities include coordinating charity care (McMullen, 2013), obtaining Medicaid treatment funding (Ell, Vourlekis, Lee, & Xie, 2007), coordinating with internal patient financial services departments (Horner et al., 2013), facilitating financial assistance applications (Braun et al., 2012), and handling insurance issues (Carroll et al., 2010). Such tasks can significantly improve treatment (Ell et al., 2007), despite being very time consuming, according to nurse navigators (Lin et al., 2008). Formal interprofessional collaborations among nurse navigators and patient financial service representatives, social workers, and other professionals focused on institutional barriers can support vulnerable patient populations’ access to treatment.
Conclusion
This study determined the risk factors associated with low perceived access to care and described the barriers that cause delays during the treatment phase of cancer care. Most adults with cancer report adequate access to medical care and medications. However, the current results showed that the Medicaid-insured and uninsured adult patients diagnosed with cancer are more likely to report low perceived access to care during the treatment phase, adjusting for demographic, socioeconomic, and health status factors. Institutional policies, such as cost and insurance factors, were the most commonly reported barriers. Future examination of survey data for periods after 2012 should be conducted to determine the impact of insurance coverage on perceived access to cancer care. This analysis is critically important, particularly in light of later legislative efforts that may significantly increase uninsured rates among vulnerable populations in the United States.
About the Author(s)
Pruitt is a visiting assistant professor in the Department of Health Policy and Management in the College of Public Health at the University of South Florida in Tampa, and Sportsman is the director of consultation and services at Elsevier Education in Maryland Heights, MO. No financial relationships to disclose. Pruitt and Sportsman contributed to the conceptualization and design, analysis, and manuscript preparation. Pruitt completed the data collection and provided statistical support. Pruitt can be reached at zpruitt1@health.usf.edu, with copy to editor at ONFEditor@ons.org. Submitted March 2016. Accepted for publication August 25, 2016.
References
American Society of Clinical Oncology. (2015). Skin cancer (non-melanoma): Treatment options. Retrieved from http://www.cancer.net/cancer-types/skin-cancer-non-melanoma/treatment-o…
Bradley, C.J., Given, C.W., & Roberts, C. (2002). Race, socioeconomic status, and breast cancer treatment and survival. Journal of the National Cancer Institute, 94, 490–496. doi:10.1093/jnci/94.7.490
Braun, K.L., Kagawa-Singer, M., Holden, A.E., Burhansstipanov, L., Tran, J.H., Seals, B.F., . . . Ramirez, A.G. (2012). Cancer patient navigator tasks across the cancer care continuum. Journal of Health Care for the Poor and Underserved, 23, 398–413. doi:10.1353/hpu.2012.0029
Brown, C.G., Cantril, C., McMullen, L., Barkley, D.L., Dietz, M., Murphy, C.M., & Fabrey, L.J. (2012). Oncology nurse navigator role delineation study: An Oncology Nursing Society report. Clinical Journal of Oncology Nursing, 16, 581–585. doi:10.1188/12.CJON.581-585
Byers, T. (2010). Two decades of declining cancer mortality: Progress with disparity. Annual Review of Public Health, 31, 121–132. doi:10.1146/annurev.publhealth.121208.131047
Carroll, J.K., Humiston, S.G., Meldrum, S.C., Salamone, C.M., Jean-Pierre, P., Epstein, R.M., & Fiscella, K. (2010). Patients’ experiences with navigation for cancer care. Patient Education and Counseling, 80, 241–247. doi:10.1016/j.pec.2009.10.024
Charlson, M.E., Pompei, P., Ales, K.L., & MacKenzie, C.R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40, 373–383.
Crowley, R.A., & Golden, W. (2014). Health policy basics: Medicaid expansion. Annals of Internal Medicine, 160, 423–425. doi:10.7326/M13-2626
Daley, K.A. (2013). Greater access to health care is here: Let’s do our part to get America covered. Retrieved from http://www.theamericannurse.org/index.php/2013/10/15/greater-access-to-…
Deyo, R.A., Cherkin, D.C., & Ciol, M.A. (1992). Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology, 45, 613–619.
Dusetzina, S.B., Basch, E., & Keating, N.L. (2015). For uninsured cancer patients, outpatient charges can be costly, putting treatments out of reach. Health Affairs, 34, 584–591. doi:10.1377/hlthaff.2014.0801
Ell, K., Vourlekis, B., Lee, P.-J., & Xie, B. (2007). Patient navigation and case management following an abnormal mammogram: A randomized clinical trial. Preventive Medicine, 44, 26–33. doi:10.1016/j.ypmed.2006.08.001
Ell, K., Vourlekis, B., Xie, B., Nedjat-Haiem, F.R., Lee, P.-J., Muderspach, L., . . . Palinkas, L.A. (2009). Cancer treatment adherence among low-income women with breast or gynecologic cancer: A randomized controlled trial of patient navigation. Cancer, 115, 4606–4615. doi:10.1002/cncr.24500
Eltorai, A.E., & Eltorai, M.I. (2017). The risk of expanding the uninsured population by repealing the Affordable Care Act. Retrieved from http://jamanetwork.com/journals/jama/fullarticle/2607483
Fedewa, S.A., Ward, E.M., Stewart, A.K., & Edge, S.B. (2010). Delays in adjuvant chemotherapy treatment among patients with breast cancer are more likely in African American and Hispanic populations: A national cohort study 2004–2006. Journal of Clinical Oncology, 28, 4135–4141. doi:10.1200/JCO.2009.27.2427
Fiscella, K., Ransom, S., Jean-Pierre, P., Cella, D., Stein, K., Bauer, J.E., . . . Walsh, K. (2011). Patient-reported outcome measures suitable to assessment of patient navigation. Cancer, 117, 3601–3615. doi:10.1002/cncr.26260
Freeman, H.P., & Rodriguez, R.L. (2011). History and principles of patient navigation. Cancer, 117, 3537–3540. doi:10.1002/cncr.26262
Gold, M.R., Jacobson, G.A., & Garfield, R.L. (2012). There is little experience and limited data to support policy making on integrated care for dual eligibles. Health Affairs, 31, 1176–1185. doi:10.1377/hlthaff.2012.0162
Gwyn, K., Bondy, M.L., Cohen, D.S., Lund, M.J., Liff, J.M., Flagg, E.W., . . . Coates, R.J. (2004). Racial differences in diagnosis, treatment, and clinical delays in a population-based study of patients with newly diagnosed breast carcinoma. Cancer, 100, 1595–1604. doi:10.1002/cncr.20169
Halpern, M.T., Ward, E.M., Pavluck, A.L., Schrag, N.M., Bian, J., & Chen, A.Y. (2008). Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: A retrospective analysis. Lancet Oncology, 9, 222–231. doi:10.1016/S1470-2045(08)70032-9
Han, X., Jemal, A., Flowers, C.R., Sineshaw, H., Nastoupil, L.J., & Ward, E. (2014). Insurance status is related to diffuse large B-cell lymphoma survival. Cancer, 120, 1220–1227. doi:10.1002/cncr.28549
Health Network Group. (2016). 2016 federal poverty level. Retrieved from https://obamacare.net/2016-federal-poverty-level
Horner, K., Ludman, E.J., McCorkle, R., Canfield, E., Flaherty, L., Min, J., . . . Wagner, E.H. (2013). An oncology nurse navigator program designed to eliminate gaps in early cancer care. Clinical Journal of Oncology Nursing, 17, 43–48. doi:10.1188/13.CJON.43-48
Hosmer, D.W., Lemeshow, S., & Sturdivant, R.X. (2000). Applied logistic regression (2nd ed.). New York, NY: John Wiley & Sons.
Kaiser Commission on Medicaid and the Uninsured. (2016). Key facts about the uninsured population. Retrieved from http://kaiserf.am/19BJGeq
Koroukian, S.M., Bakaki, P.M., & Raghavan, D. (2011). Survival disparities by Medicaid status: An analysis of 8 cancers. Cancer, 118, 4271–4279. doi:10.1002/cncr.27380
Lavarreda, S.A., Brown, E.R., & Bolduc, C.D. (2011). Underinsurance in the United States: An interaction of costs to consumers, benefit design, and access to care. Annual Review of Public Health, 32, 471–482. doi:10.1146/annurev.publhealth.012809.103655
Lin, C.J., Schwaderer, K.A., Morgenlander, K.H., Ricci, E.M., Hoffman, L., Martz, E., . . . Heron, D.E. (2008). Factors associated with patient navigators’ time spent on reducing barriers to cancer treatment. Journal of the National Medical Association, 100, 1290–1297.
Lubejko, B.G., Bellfield, S., Kahn, E., Lee, C., Peterson, N., Rose, T., . . . McCorkle, M. (2017). Oncology nurse navigation: Results of the 2016 role delineation study. Clinical Journal of Oncology Nursing, 21, 43–50. doi:10.1188/17.CJON.43-50
Martin, A.B., Hartman, M., Benson, J., & Catlin, A. (2015). National health spending in 2014: Faster growth driven by coverage expansion and prescription drug spending. Health Affairs, 35, 150–160. doi:10.1377/hlthaff.2015.1194
Massarweh, N.N., Chiang, Y.-J., Xing, Y., Chang, G.J., Haynes, A.B., You, Y.N., . . . Cormier, J.N. (2014). Association between travel distance and metastatic disease at diagnosis among patients with colon cancer. Journal of Clinical Oncology, 32, 942–948. doi:10.1200/JCO.2013.52.3845
McLeroy, K.R., Bibeau, D., Steckler, A., & Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15, 351–377.
McMullen, L. (2013). Oncology nurse navigators and the continuum of cancer care. Seminars in Oncology Nursing, 29, 105–117. doi:10.1016/j.soncn.2013.02.005
Moy, B., Polite, B.N., Halpern, M.T., Stranne, S.K., Winer, E.P., Wollins, D.S., & Newman, L.A. (2011). American Society of Clinical Oncology policy statement: Opportunities in the patient protection and Affordable Care Act to reduce cancer care disparities. Journal of Clinical Oncology, 29, 3816–3824. doi:10.1200/JCO.2011.35.8903
National Cancer Institute. (2005). Theory at a glance: A guide for health promotion practice (2nd ed.). Washington, D.C.: Author.
National Cancer Institute. (2015). Cancer and public health. Retrieved from http://www.cancer.gov/research/areas/public-health
Ndumele, C.D., Mor, V., Allen, S., Burgess, J.F., & Trivedi, A.N. (2014). Effect of expansions in state Medicaid eligibility on access to care and the use of emergency department services for adult Medicaid enrollees. JAMA Internal Medicine, 174, 920–926. doi:10.1001/jamainternmed.2014.588
Oncology Nursing Society, Association of Oncology Social Work, & National Association of Social Workers. (2010). Oncology Nursing Society, the Association of Oncology Social Work, and the National Association of Social Workers joint position on the role of oncology nursing and oncology social work in patient navigation. Retrieved from http://bit.ly/2nfhsRj
Paskett, E.D., Harrop, J.P., & Wells, K.J. (2011). Patient navigation: An update on the state of the science. CA: A Cancer Journal for Clinicians, 61, 237–249. doi:10.3322/caac.20111
Pruitt, Z., & Sportsman, S. (2013). The presence and roles of nurse navigators in acute care hospitals. Journal of Nursing Administration, 43, 592–596. doi:10.1097/01.NNA.0000434510.74373.40
Rowland, D. (2015). The Medicare and Medicaid partnership at age 50. Generations, Summer 2015, 35–42.
Scheppers, E., van Dongen, E., Dekker, J., Geertzen, J., & Dekker, J. (2006). Potential barriers to the use of health services among ethnic minorities: A review. Family Practice, 23, 325–348. doi:10.1093/fampra/cmi113
Scoggins, J.F., Fedorenko, C.R., Donahue, S.M., Buchwald, D., Blough, D.K., & Ramsey, S.D. (2011). Is distance to provider a barrier to care for Medicaid patients with breast, colorectal, or lung cancer? Journal of Rural Health, 28, 54–62. doi:10.1111/j.1748-0361.2011.00371.x
Shi, R., Mills, G., McLarty, J., Burton, G., Shi, Z., & Glass, J. (2013). Commercial insurance triples chances of breast cancer survival in a public hospital. Breast Journal, 19, 664–667. doi:10.1111/tbj.12185
Smith, A.W., Reeve, B.B., Bellizzi, K.M., Harlan, L.C., Klabunde, C.N., Amsellem, M., . . . Hays, R.D. (2008). Cancer, comorbidities, and health-related quality of life of older adults. Health Care Financing Review, 29(4), 41–56.
Sommers, B.D., & Kronick, R. (2016). Measuring Medicaid physician participation rates and implications for policy. Journal of Health Politics, Policy and Law, 41, 211–224. doi:10.1215/03616878-3476117
Spetz, J. (2014). How will health reform affect demand for RNs? Nursing Economics, 32, 42–43.
Tejeda, S., Darnell, J.S., Cho, Y.I., Stolley, M.R., Markossian, T.W., & Calhoun, E.A. (2013). Patient barriers to follow-up care for breast and cervical cancer abnormalities. Journal of Women’s Health, 22, 507–517. doi:10.1089/jwh.2012.3590
Tipirneni, R., Rhodes, K.V., Hayward, R.A., Lichtenstein, R.L., Reamer, E.N., & Davis, M.M. (2015). Primary care appointment availability for new Medicaid patients increased after Medicaid expansion in Michigan. Health Affairs, 34, 1399–1406. doi:10.1377/hlthaff.2014.1425
Wells, K.J., Battaglia, T.A., Dudley, D.J., Garcia, R., Greene, A., Calhoun, E., . . . Raich, P.C. (2008). Patient navigation: State of the art or is it science? Cancer, 113, 1999–2010. doi:10.1002/cncr.23815
Yabroff, K.R., Short, P.F., Machlin, S., Dowling, E., Rozjabek, H., Li, C., . . . Virgo, K.S. (2013). Access to preventive health care for cancer survivors. American Journal of Preventive Medicine, 45, 304–312. doi:10.1016/j.amepre.2013.04.021
Zuckerman, S., & Goin, D. (2012). How much will Medicaid physician fees for primary care rise in 2013? Evidence from a 2012 survey of Medicaid physician fees. Retrieved from https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8398.pdf

