The Role of Oncology Nurses in Discussing Clinical Trials
Purpose/Objectives: To describe oncology nurses’ experiences discussing clinical trials with their patients, and to assess barriers to these discussions.
Research Approach: A qualitative study designed to elicit narratives from oncology nurses.
Setting: Community- and academic-based oncology clinics throughout the United States.
Participants: 33 oncology nurses involved in direct patient care in community-based and large hospital-based settings. The sample was drawn from members of the Oncology Nursing Society.
Methodologic Approach: In-depth interviews were conducted and analyzed using a immersion/crystallization approach to identify themes and patterns. The analyses highlight specific issues, examples, and contexts that present challenges to clinical trial discussions with patients.
Findings: Oncology nurses view their roles as patient educators and advocates to be inclusive of discussion of clinical trials. Barriers to such discussions include lack of knowledge and strategies for addressing patients’ common misconceptions and uncertainty about the timing of discussions.
Interpretation: These data indicate that enabling nurses to actively engage patients in discussions of clinical trials requires educational interventions to build self-efficacy and close knowledge gaps.
Implications for Nursing: Oncology nurses can play a critical role in advancing cancer care by supporting patients in decision making about clinical trial participation. This will require training and education to build their knowledge, reduce barriers, and increase their self-efficacy to fulfill this responsibility in various clinical settings.
Jump to a section
Cancer clinical trials (CTs) reveal new ways to prevent, diagnose, and treat patients with cancer, and provide effective supportive interventions for patients and their families. In addition, studies of new treatment regimens can provide participants with early access to promising interventions. Although CTs provide the evidence base for clinical practice, less than 10% of patients with cancer participate in them (Al-Refaie et al., 2011; Institute of Medicine, 2010; Murthy, Krumholz, & Gross, 2004; Unger et al., 2013). Various reasons explain why enrollment in trials is so low, but a common reason is because patients do not know the studies were an option for them (American Cancer Society, 2016). In addition, a variety of patient knowledge gaps and attitudes exist, including concerns about risks that may impede participation (Manne et al., 2015; Meropol et al., 2007, 2016).
A National Cancer Institute and American Society of Clinical Oncology symposium that focused on CT accrual revealed that improving provider communication with patients was an effective way of increasing patient participation. Oncology nurses are routinely involved in the care of patients who are eligible for enrollment in CTs. The Oncology Nursing Society’s ([ONS’s], 2016) Oncology Nurse Generalist Competencies begins with the statement, “Regardless of employment setting, comprehensive knowledge and skills regarding cancer pathophysiology, treatment options, and symptom management are required elements of practice” (p. 4). Specific competencies include providing education to address the needs of the patient and family caregivers, as well as identifying resources available to people with cancer and their caregivers. In Core Curriculum for Oncology Nursing, Klimaszewski (2016) confirmed the relevance of these competencies as they relate to CTs. Nursing interventions addressed in the book include providing information related to CT participation, reinforcing the voluntary nature of trial participation, and assisting and encouraging the patient and family to ask questions of the research team (Klimaszewski, 2016). As the highest rated professionals in honesty and ethics (Gallup, 2015), oncology nurses are in a key position to engage patients and increase awareness and accurate understanding of CTs through patient education, counseling, and support for informed decision making (Jenerette & Mayer, 2016).
Despite unanimity regarding the important role of oncology nurses in supporting patient awareness of and decisions about trial participation, little is known about the involvement of oncology nurses in CT decision making beyond those who work in specific CT support units. Although some investigation of the role of nurses as CT coordinators has taken place (Hastings, Fisher, & McCabe, 2012; Haugen et al., 2015; Ocker & Plank, 2000; Spilsbury et al., 2008; Sun & Borneman, 2007), much less is known about attitudes and behaviors of nurses who serve in traditional patient care roles. Arrigo, Gall, Delogne, and Molin’s (1994) study of European nurses revealed that the availability of information about trials varied among centers and that nurse respondents believed that their responsibilities related to CTs were primarily oriented toward direct care of the patients. Little is known about contemporary nursing practice and attitudes about CTs in the United States.
Burnett et al. (2001) interviewed 250 nurses working at a National Cancer Institute (NCI)-designated comprehensive cancer center. Most (96%) believed that patient participation in trials was important, although only 56% believed patients should be encouraged to participate. A survey of 173 primary care nurse practitioners revealed that only 48% felt comfortable discussing CTs with patients and that 73% reported three or more ethical concerns with research (Ulrich et al., 2012). However, the nurses also said that they were willing to recommend CTs but needed more education (Ulrich et al., 2012). Schutta and Burnett (2000) conducted a qualitative study with 22 patients who were enrolled in trials. These patients were unable to describe any influence of nurses on their decision to take part in the trials. These findings reveal that nurses may not routinely engage in discussions about this potential treatment option.
Oncology nurses can play a central role in informing patients about the option of participating in CTs, addressing questions and concerns, and supporting them in making informed decisions. However, evidence is lacking on the extent to which nurses see this as part of their role, their attitudes and beliefs, and what challenges exist in fulfilling these important responsibilities. To explore and evaluate the potential for engaging nurses to provide timely information to patients about CTs, a better understanding of current practice and an effective means to prepare nurses for this role are needed.
In a first step toward this aim, the current authors conducted a study of how nurses perceived their roles related to CTs. The purpose was to explore nurses’ attitudes and beliefs about CTs, their own role, and influential personal or environmental factors.
Research Approach
The current authors employed a qualitative design and analysis, using in-depth interview methods to generate new understanding about oncology nurses’ experiences and perceptions of their role in discussing CTs with patients. The development of the interview guide was based on a tradition of phenomenology (Giorgi, 1997; Holstein & Gubrium, 1998). The goal was to elicit lived experiences of discussing CTs with patients. The current authors also sought to elicit nurses’ perceptions and understandings of the contexts that promote or inhibit that activity, and perceptions of their role in and attitudes and beliefs of discussing CTs with patients with cancer.
Participants
Participants were drawn from a national sample of oncology nurses. The authors expected to have a 10% response rate of nurses after invitation, based on ONS’s experience with prior research studies. Therefore, 300 ONS oncology nurses, chosen randomly from the ONS membership, were invited by email to participate in an in-depth telephone interview regarding their experience with discussing CT therapies with patients. The authors used a purposive sample of 33 ONS members, stratified by practice setting, which maximized variation across a characteristic that was expected to affect nurses’ attitudes and subjective norms for discussing CTs with patients. Using this approach, the authors anticipated reaching saturation of new information related to initiating discussions with patients about CTs.
Methodologic Approach
The email invitation included the study information sheet for preview and an individualized link to a website with a prescreening survey. Inclusion criteria were nurses (a) currently practicing, (b) currently involved in direct patient care, (c) who were in a primary practice role, and (d) who had an email address. Nurses who were interested contacted the study staff, and if they met the inclusion criteria, a time to conduct the interview was scheduled. Informed consent was required of all participants. Study participation was incentivized with a $50 gift card. The study protocol was approved by the institutional review board of University Hospitals Cleveland Medical Center in Ohio.
Telephone interviews took place from October to December 2014, lasted 30–40 minutes, and were audio recorded. Verbal consent was obtained at the beginning of each interview. The semistructured interview guide featured open-ended questions regarding how nurses help patients with cancer learn about participating in CTs, as well as specific questions about the presence and extent of CTs at their primary work location. Interviews also explored nurses’ perceptions of barriers to discussing CTs with patients, their attitudes about having such discussions, and their perceptions of the subjective norms for nurses engaging in these discussions. Finally, demographic data were collected at the end of the interview, and opportunities were provided to address additional questions or thoughts.
Qualitative data were analyzed in several stages using an immersion/crystallization process (Crabtree & Miller, 1999), an iterative approach involving cycles of concentrated review of the data combined with reflection and intuitive insights. The first phase of analysis occurred during data collection. After half the interviews was completed, the initial set of interviews were analyzed for emerging themes and to identify areas where additional probing questions would facilitate understanding. Subsequently, the second round of interviews was conducted using a modified interview guide that incorporated probing questions about the emerging themes detected in the initial interviews. Saturation of concepts was reached at 24 interviews. The team continued to conduct interviews and analyses with the individuals who had already agreed to participate in the study, and did not accept any new participants, resulting in a sample size of 33.
On completion of the interviews, two of the authors read and discussed one-third of the interview transcripts and began to identify emergent themes and patterns. The same authors independently analyzed the remaining two-thirds of interviews and compiled detailed notes to build on identified themes and note patterns of variation. Finally, a third coauthor read and analyzed all 33 transcripts and recordings and provided additional insights and a synthesis of interpretations. The use of multiple perspectives to independently interpret data and compare similarities and differences is a strategy for corroborating and legitimating the analysis. The final synthesis and description of themes were developed and then reviewed for clarity and completeness by all authors.
Demographic information was entered and stored in a REDCap database (Harris et al., 2009). Descriptive statistics were used to summarize nurses’ demographic characteristics and primary work setting.
Findings
Thirty-five of the 302 nurses invited to participate responded and were eligible for the study. Thirty-four nurses successfully scheduled interviews, and 33 interviews were completed. Table 1 provides the demographic characteristics and primary work environments of participating nurses. The majority were female and White, with a mean age of 46 years. More than half worked in an outpatient setting, and 23 worked in a community setting. On average, respondents had 18 years of nursing experience and 13 years of oncology nursing experience. 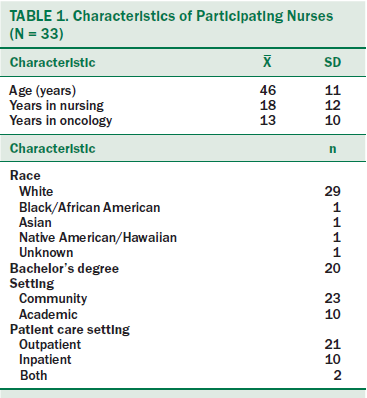
The Role of Oncology Nurses in Discussing Clinical Trials
Context of clinical trial team versus no team: Current practices for discussing CTs with patients varied with certain features of the practice setting. Designated clinical research nurses are often staffed in settings with on-site CTs. These nurses play a central role in initiating discussions with patients regarding their eligibility for specific CTs. Some locations have a CT team, including a research nurse and an oncologist who discuss the trials with the patient. Respondents said that, when present, CT nurses or teams initiated and discussed trials with patients. In locations with no dedicated CT nurse or team, oncologists usually raised the subject of participation in a CT. Only one participant noted that discussions of CTs systematically occurred with nearly all patients within her practice setting. Participants in this study also reported that supervisors and oncologists were generally supportive of the idea of oncology nurses discussing CTs. However, it was very uncommon for oncology nurses to initiate general discussions of CTs. In addition, most respondents were unsure whether doing so would be supported by supervisors and oncologists.
For most respondents working in an inpatient setting, the initial contact with a patient occurred after a CT had started; therefore, no perceived opportunity to initiate a discussion of a CT existed. Discussions about CTs in this context focused on treatment issues, such as side effects, rather than decision making.
Perceived primary role: Most of the respondents described the primary role of the oncology nurse as providing information, supporting, and assisting the patient after the initial discussion had taken place. Once patients process what they have been told by their oncologist or a research nurse, they often have additional questions and concerns. The nurses reported that they were often called upon to clarify or elaborate on CT information, helping patients and families understand the purpose of CTs and what might be involved.
Many oncology nurses also emphasized their role in providing emotional support to patients facing important decisions. Patients and their families experience a range of emotions, including hope, apprehension, and confusion. Nurses noted spending time listening to patients; offering compassion, empathy, and reassurance; and helping patients feel empowered about their decision. Respondents reported that patients, particularly when they have a preexisting relationship with nurses, feel comfortable asking them questions they may not feel comfortable asking CT nurses or may be embarrassed to ask their doctors.
Although it is most common for research staff or oncologists to initiate discussion of CTs, sometimes patients initiate discussions with their nurses, particularly if CTs are not offered on-site. The nurses generally felt comfortable discussing CTs in general terms in this context, but they often referred patients to other resources to determine eligibility for CTs at other sites. Some nurses also directed patients to online resources.
Overall, the roles described by oncology nurses regarding their involvement in CT discussions fit within their more general role as patient advocate. Nurses want to support patients to make informed decisions and appreciated that CTs could offer hope and empower patients to feel as if they are exploring every option available to them. CT discussions can build on and strengthen the nurse–patient relationship, based on trust, compassion, and advocacy. However, such discussions can also present challenges.
Barriers to Discussing Clinical Trials
Throughout the interviews with oncology nurses, several themes emerged regarding barriers to discussing CTs (see Figure 1). The most common challenge expressed by nurses was lack of information. Although most felt comfortable discussing CTs in general terms with their patients, patients often asked specific questions to which nurses did not know the answers. These questions often centered on the specifics of a CT, such as the study protocol and logistics, eligibility, financial burden, or on nuances of their specific cases. In such situations, the oncology nurse would contact the research nurse or oncologist for answers. However, this could prove frustrating if neither was available. For example, a nurse who worked on the night shift expressed that patients often felt relaxed and talked with the nurse during this time, but that others were not readily available to answer questions.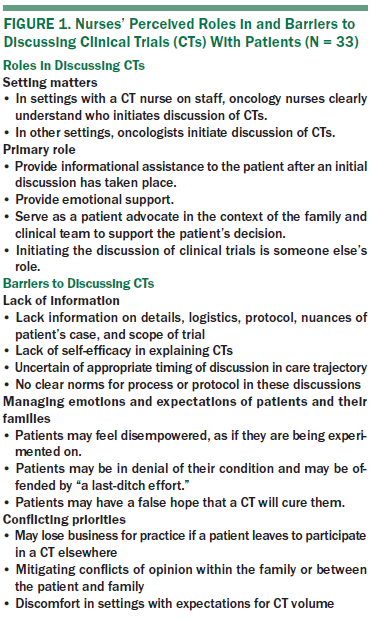
In other cases, respondents reported a lack of confidence in their ability to explain CTs correctly in general terms. This lack of self-efficacy was apparent, for example, when debunking common myths about CTs or explaining the benefits of CTs. Many patients and their families had conducted their own investigations of cancer treatments and asked challenging questions.
Another example of lacking necessary information is not knowing when to discuss CTs with patients within the care trajectory. When and with whom these discussions should occur are sometimes unclear. For example, a patient may be eligible for a specific trial only before starting treatment. If the nurse is responsible for administering the treatment, he or she may feel uncertain about how to proceed with such discussions. Many oncology nurses were unsure if oncologists would be supportive of them introducing CTs. Much of this uncertainty seems related to the lack of a clear process or protocol for having these discussions. In addition, very few respondents reported receiving any training about CTs.
Another area in which oncology nurses reported barriers to discussing CTs is in managing expectations, perceptions, and emotions of patients and their families. Several scenarios described by nurses required sensitivity, knowledge about CTs, and the ability to communicate effectively. In one situation, a patient felt that he or she was being experimented on, not necessarily for his or her own benefit but for the researchers’. Related to this is the expression of anger or frustration if a patient is assigned to the standard of care rather than the experimental group in a randomized CT. Another commonly reported assumption is that participating in a CT means that no hope exists for patients and that it is a last resort that is unlikely to provide any benefit. Concern was also expressed that participating in a CT may imply that current treatments are not working and that patients should not be satisfied with their current treatment plans and/or physicians. Alternatively, nurses indicated that participation may lead to an expectation of a cure. In such instances, oncology nurses may have to balance the patient’s hopes and expectations with the reality of the CT’s likely or potential benefit.
Finally, as advocates for their patients, nurses reported feeling a sense of conflicting priorities at times. For example, if an oncology nurse works in a practice that does not offer CTs, then referring a patient to another site that does offer CTs may conflict with his or her loyalty to the physician, who would be losing business if the patient left. This may lead to the interpretation that the current physician’s care is somehow less than optimal, requiring the move to another location where participation in CTs is offered. At the other extreme, a few nurses reported feeling some discomfort prioritizing patient advocacy in settings with CT volume expectations.
Discussion
In summary, the oncology nurses who participated in these interviews perceived that they played an important role in supporting patients who were considering participation in CTs. Although research nurses and oncologists most often introduced CTs to patients, nurses were actively engaged in answering questions or helping patients obtain answers. They also provided emotional support to patients and families, sometimes correcting misinterpretations or clarifying what the patient had been told by others.
Although they reported positive attitudes toward CTs and the nursing role, respondents described common challenges. Some of these were a knowledge deficit, uncertainties about the appropriateness of raising the topic before the patient asked, and the need for advanced skills in recognizing and responding to patients and families’ emotional concerns.
Limitations
The current authors engaged about 11% of eligible participants with a handwritten invitation letter, email reminder, and remuneration for completing the interview. The low response rate could be related to the method of invitation from an organization membership list, and whether emails were opened cannot be confirmed to calculate a participation rate among those who viewed the invitation. Nonetheless, collecting interviews and exploring new issues generated data in which patterns of responses were readily identified. Saturation of new information was reached after the first 24 interviews. These qualitative interview data were not intended to generate the frequency of responses. Additional data collection with larger samples and alternative data collection methods, such as a survey, could yield data to inform the frequency of behaviors and attitudes.
Implications for Nursing Practice and Research
These data confirm that oncology nurses recognize the central role they play in ensuring that patients have access to the newest therapies, as well as supporting the discovery of new and improved therapies for patients through CTs. Although many barriers reported by oncology nurses are unavoidable when discussing important topics in the context of a life-threatening disease, participants reported potential facilitators of discussion. Continuing education and/or guidelines for these discussions could prove helpful, as could resources, such as training videos. Like the findings by Ulrich et al. (2012), many respondents in the current study expressed an interest in training and education in this topic, and seemed driven to improve as patient advocates. However, the current study data suggest that interventions will require modifying the norms around nurse roles to effect change. This will entail not only delivering educational interventions to close gaps in knowledge but also building self-efficacy and positive attitudes among nurses, who understand that their role of engaging patients in discussions of CTs can advance cancer care through the discovery of improved therapies. Such training could provide specific suggestions for how to negotiate complex situations with patients and other healthcare providers. This may be particularly important in light of the current study findings that participants perceived that supervisors and oncologists were generally supportive of the idea of oncology nurses discussing CTs, but the nurses were less sure regarding whether supervisors and oncologists would support nurse initiation of these discussions.
Increased, targeted education and preparation for general discussions about CTs may increase nurses’ confidence. Increasing self-efficacy in nurses can contribute to more frequent discussion of CTs with patients or an ability to respond to unsolicited questions, assess patient understanding, and respond to misunderstandings or emotional concerns. Ultimately, increasing timely conversations about CTs with patients can contribute to quality decision making and access to CTs as a therapeutic opportunity.
Conclusion
Oncology nurses perceive that they play an important role in supporting patients who are considering participation in CTs but that they provide this support predominately after patients decide to participate in a trial. Enabling nurses to actively initiate general discussions with patients about CTs requires educational interventions to build self-efficacy and close gaps in knowledge.
The authors gratefully acknowledge Margaret M. Irwin, RN, MN, PhD, of the Oncology Nursing Society for her advice and support. The authors also acknowledge Dawn Miller, MA, Tyler Kinzy, MS, and Sue Krejci, MBA, for their input and work in the development of this project.
About the Author(s)
Flocke is a professor in the Department of Family Medicine and Community Health of the School of Medicine and the Case Comprehensive Cancer Center; Antognoli is a research associate in the Department of Family Medicine and Community Health of the School of Medicine; and Daly is a professor in the Frances Payne Bolton School of Nursing and the Case Comprehensive Cancer Center, all at Case Western Reserve University in Cleveland, OH; Jackson is an education coordinator at MetroHealth System in Cleveland; Fulton is a research operations manager, Liu is a research assistant III, and Surdam is a research assistant III, all in the School of Medicine and the Case Comprehensive Cancer Center at Case Western Reserve University; Manne is a professor at the Rutgers Cancer Institute of New Jersey in New Brunswick; and Meropol is vice president of Research Oncology at Flatiron Health in New York, NY, and an adjunct professor in the Case Comprehensive Cancer Center at Case Western Reserve University. This research was funded by a grant (R25CA177574; principal investigators: Barbara J. Daly and Neal J. Meropol) from the National Cancer Institute of the National Institutes of Health. Flocke, Daly, Manne, and Meropol contributed to the conceptualization and design. Jackson, Fulton, Liu, and Meropol completed the data collection. Flocke and Meropol provided statistical support. Flocke, Antognoli, Daly, Jackson, Fulton, Liu, Surdam, and Meropol provided the analysis. All authors contributed to the manuscript preparation. Flocke can be reached at susan.flocke@case.edu, with copy to editor at ONFEditor@ons.org. Submitted September 2016. Accepted for publication February 6, 2017.
References
Al-Refaie, W.B., Vickers, S.M., Zhong, W., Parsons, H., Rothenberger, D., & Habermann, E.B. (2011). Cancer trials versus the real world in the United States. Annals of Surgery, 254, 438–443. doi:10.1097/SLA.0b013e31822a7047
American Cancer Society. (2016). The basics of clinical trials. Retrieved from https://www.cancer.org/treatment/treatments-and-side-effects/clinical-t…
Arrigo, C., Gall, H., Delogne, A., & Molin, C. (1994). The involvement of nurses in clinical trials. Results of the EORTC Oncology Nurses Study Group survey. Cancer Nursing, 17, 429–433.
Burnett, C.B., Koczwara, B., Pixley, L., Blumenson, L.E., Hwang, Y.T., & Meropol, N.J. (2001). Nurses’ attitudes toward clinical trials at a comprehensive cancer center. Oncology Nursing Forum, 28, 1187–1192.
Crabtree, B.F., & Miller, W.L. (1999). Doing qualitative research (2nd. ed.). Thousand Oaks, CA: Sage Publications.
Gallup. (2015). Honesty/ethics in professions. Historical Trends. Retrieved from http://www.gallup.com/poll/187874/americans-faith-honesty-ethics-police…
Giorgi, A. (1997). The theory, practice, and evaluation of the phenomenological method as a qualitative research procedure. Journal of Phenomenological Psychology, 28, 235–260. doi:10.1163/156916297X00103
Harris, P.A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J.G. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42, 377–381. doi:10.1016/j.jbi.2008.08.010
Hastings, C.E., Fisher, C.A., & McCabe, M.A. (2012). Clinical research nursing: A critical resource in the national research enterprise. Nursing Outlook, 60, 149–156.e3. doi:10.1016/j.outlook.2011.10.003
Haugen, M., Kelly, K.P., Leonard, M., Mills, D., Sung, L., Mowbray, C., & Landier, W. (2015). Nurse-led programs to facilitate enrollment to children’s oncology group cancer control trials. Journal of Pediatric Oncology Nursing, 33, 387–391. doi:10.1177/1043454215617458
Holstein, J.A., & Gubrium, J.F. (1998). Phenomenology, ethnomethodology, and interpretive practice. In N.K. Denzin & Y.S. Lincoln (Eds.), Strategies of qualitative inquiry (pp. 137–157). Thousand Oaks, CA: Sage Publications.
Institute of Medicine. (2010). Transforming clinical research in the United States: Challenges and opportunities: Workshop summary. Washington, DC: National Academies Press.
Jenerette, C.M., & Mayer, D.K. (2016). Patient-provider communication: The rise of patient engagement. Seminars in Oncology Nursing, 32, 134–143. doi:10.1016/j.soncn.2016.02.007
Klimaszewski, A.D. (2016). Research protocols and clinical trials. In J.K. Itano (Ed.), Core curriculum for oncology nursing (5th ed., pp. 62–70). St. Louis, MO: Elsevier.
Manne, S., Kashy, D., Albrecht, T., Wong, Y.-N., Lederman Flamm, A., Benson, A.B., III, . . . Meropol, N.J. (2015). Attitudinal barriers to participation in oncology clinical trials: Factor analysis and correlates of barriers. European Journal of Cancer Care, 24, 28–38. doi:10.1111/ecc.12180
Meropol, N.J., Buzaglo, J.S., Millard, J., Damjanov, N., Miller, S.M., Ridgway, C., . . . Watts, P. (2007). Barriers to clinical trial participation as perceived by oncologists and patients. Journal of the National Comprehensive Cancer Network, 5, 655–664.
Meropol, N.J., Wong, Y.-N., Albrecht, T., Manne, S., Miller, S.M., Flamm, A.L., . . . Schluchter, M.D. (2016). Randomized trial of a web-based intervention to address barriers to clinical trials. Journal of Clinical Oncology, 34, 469–478. doi:10.1200/jco.2015.63.2257
Murthy, V.H., Krumholz, H.M., & Gross, C.P. (2004). Participation in cancer clinical trials: Race-, sex-, and age-based disparities. JAMA, 291, 2720–2726. doi:10.1001/jama.291.22.2720
Ocker, B.M., & Plank, D.M. (2000). The research nurse role in a clinic-based oncology research setting. Cancer Nursing, 23, 286–292.
Oncology Nursing Society. (2016). Oncology nurse generalist competencies. Retrieved from https://www.ons.org/sites/default/files/Oncology%20Nurse%20Generalist%2…
Schutta, K.M., & Burnett, C.B. (2000). Factors that influence a patient’s decision to participate in a phase I cancer clinical trial. Oncology Nursing Forum, 27, 1435–1438.
Spilsbury, K., Petherick, E., Cullum, N., Nelson, A., Nixon, J., & Mason, S. (2008). The role and potential contribution of clinical research nurses to clinical trials. Journal of Clinical Nursing, 17, 549–557. doi:10.1111/j.1365-2702.2006.01872.x
Sun, V.C., & Borneman, T. (2007). The oncology nurse’s role in the informed consent process. Oncology (Williston Park), 21(Suppl. 8), 11–14.
Ulrich, C.M., Zhou, Q., Ratcliffe, S.J., Ye, L., Grady, C., & Watkins-Bruner, D. (2012). Nurse practitioners’ attitudes about cancer clinical trials and willingness to recommend research participation. Contemporary Clinical Trials, 33, 76–84.
Unger, J.M., Hershman, D.L., Albain, K.S., Moinpour, C.M., Petersen, J.A., Burg, K., & Crowley, J.J. (2013). Patient income level and cancer clinical trial participation. Journal of Clinical Oncology, 31, 536–542. doi:10.1200/jco.2012.45.4553

