A Survey of Information Needs and Preferences of Patients With Head and Neck Cancer
Objectives: To determine the information needs and preferences of patients who had human papillomavirus–associated head and neck cancer (HNC) and who were aged 18–65 years in the post-treatment phase of recovery.
Sample & Setting: 205 patients who completed treatment for HNC at two large cancer centers in Western Canada.
Methods & Variables: A self-administered survey was completed in paper or online format. Participants were asked about information considered most important, sources of information used during recovery, and sources considered most helpful.
Results: Participants wanted information on signs and symptoms of recurrence, cure rates, post-treatment rehabilitation, treatment and recovery time frames, and financial assistance. They identified healthcare providers as the most frequently used and helpful source of information, but also reported that the Internet was useful and that an online information resource would be helpful during recovery.
Implications for Nursing: Nurses can provide more personalized information for survivors of HNC by contributing to the development of reliable Internet-based resources. The developers of these resources could also consider creating ways to directly link healthcare providers and survivors of HNC who are experiencing problems stemming from diagnosis and treatment.
Jump to a section
In 2016, an estimated 5,660 people had been diagnosed with head and neck cancer (HNC) in Canada (Canadian Cancer Society, 2016). Of these 1,335 tumors originated in the oropharynx and were consistently associated with human papillomavirus (HPV) infection (Canadian Cancer Society, 2016). Although the incidence rates of HNCs have decreased, HPV-associated oropharyngeal squamous cell carcinomas have dramatically risen since the late 1990s (Canadian Cancer Society, 2016; Forte, Niu, Lockwood, & Bryant, 2012; Pytynia, Dahlstrom, & Sturgis, 2014). This shift in HNC etiology has the potential to impose a substantial economic burden on health systems and has changed the population characteristics of survivors of HNC (Coughlan & Frick, 2012; Pytynia et al., 2014; Reich et al., 2016).
The largest increase in HPV-associated HNC in Canada and the United States has been observed in men aged 40–59 years (Chaturvedi, Engels, Anderson, & Gillison, 2008; Forte et al., 2012). Although HPV-associated HNCs tend to be diagnosed at more advanced stages, individuals with HPV-associated HNC are younger than those with non-HPV HNC, respond better to treatment, have a decreased risk of recurrence, and have better survival rates than individuals with non-HPV HNCs (Heath et al., 2012; Marur, D’Souza, Westra, & Forastiere, 2010; Pytynia et al., 2014). Younger age at diagnosis leads to prolonged survivorship but also contributes to shorter productive work years, increased distress after treatment, and a diminished cancer-specific quality of life (QOL) (Johnson-Obaseki, McDonald, Corsten, & Rourke, 2012; Wells et al., 2015, 2016). Given the shifting demographic and clinical profile of those with HPV-associated HNC, this emerging population may experience a unique set of post-treatment needs when compared to survivors of non-HPV HNC (Powell & Evans, 2015).
• What types of information are most important?
• What modes of delivery are most frequently used?
• What modes of delivery are considered most helpful?
The secondary research question was as follows:
• Do age, gender, education, and time since treatment completion predict information preferences?
Based on the limited literature available and the authors’ clinical experience, it was hypothesized that age, gender, education, and time since treatment completion would be significant predictors of information preferences.
Methods
Sample and Setting
The study population included individuals who met the following criteria: aged 18–65 years at the time of diagnosis with squamous cell carcinomas of the oral cavity or oropharynx, no history of recurrent or metastatic disease, completed treatment in the past one month to five years (2009–2014) in either one of the two large cancer centers in Alberta, resided in the province of Alberta, Canada (all cancer care in Alberta is provided at these two cancer centers), and able to read and write in English. The specified age range was selected based on the available literature on HPV-associated HNC. HPV status was not included as a criteria because HPV status tumor testing protocols were not in place until partway through this study. Staff at the Alberta Cancer Registry (ACR) identified individuals who met the inclusion criteria. Individuals with HNC diagnosed in 2013 were not yet included in the ACR database, so identification of these participants was done by a research assistant who manually reviewed the charts of individuals diagnosed with HNC in 2013 and identified those who met eligibility criteria. Using these two approaches, the total population size of 545 individuals who met study criteria were identified, and all were invited to participate in the study.
Design and Data Collection
A mixed-methods survey design was used. Data were collected using a self-administered mail-in survey or an Internet-based survey containing the same questions. The survey consisted of the Head and Neck Information Needs Questionnaire (HaNiQ), two sections on modes of information delivery (tested by Dall’Armi, Forstner, Simpson, and Simpson, 2009), four open-ended information provision preference questions, and four demographic items. The HaNiQ was developed by Dall’Armi et al. (2009), has good internal consistency and reliability (Cronbach alpha = 0.95), and has previously been tested with HNC populations (Dall’Armi et al., 2013). The open-ended questions were developed specifically for this study by the research team and included the following:
• Is there any other information that is not included in these questions that you think is important during your current stage of recovery?
• What sources of information would you like to use in the future, in addition to those you already use?
• Would you find an Internet-based information resource useful during recovery?
• Please comment on why you would find this useful/not useful?
The complete questionnaire was pretested with five colleagues with clinical experience in HNC. The goals of the pretest were to identify questions that might be unclear or difficult to understand and to establish the face validity of the open-ended questions developed for the study. No changes to the HaNiQ were suggested, but several suggestions regarding the open-ended questions were made, and the questions were revised based on this feedback.
The Health Research Ethics Board at the University of Alberta granted ethical approval for this project, and Alberta Health Services granted operational approval. Following ethics approval, the principal investigator prepared study packages containing an information letter that discussed consent, a copy of the survey (with directions on how to access an electronic version if participants wished to complete the survey online), and a pre-stamped, pre-addressed return envelope. Each return envelope was marked with a unique identifier number so that ACR staff could track returned surveys and identify those requiring a postcard reminding them to complete and return the survey. The ACR staff then addressed all packages and mailed them to all eligible individuals. The principal investigator had no access to names of study participants. Mailing occurred from March 29 to April 8, 2014; one reminder postcard was sent on May 23, 2014. Age and gender data were provided by the ACR staff for those who returned the questionnaire and those who did not.
Data Analysis
After data entry and cleaning, age and gender of responders and nonresponders were compared. Responses to open-ended questions were inductively categorized using thematic analysis, and the frequency of each coded category was recorded. Cronbach alpha for the HaNiQ was calculated. The primary research questions were addressed by calculating descriptive statistics for all study variables. Using multiple regression and logistic regression (IBM SPSS Statistics, version 15.0), with the significance level set at p < 0.05 for all analyses, the authors were able to answer the secondary research question.
Rigor
Rigor was addressed by using a validated and reliable survey instrument and by using identical forms of the survey for the paper-based and electronic data collection. All written material was prepared at an eighth-grade reading level to reduce nonresponse bias related to lower educational achievement.
Results
Of the 545 surveys sent, 29 did not reach the potential participant because of wrong addresses, 2 potential participants were deceased, and 3 were ineligible. This resulted in 511 potential participants. Of these, 16 (3%) declined to participate and 290 (57%) did not respond. Of those who did respond, 178 (87%) mailed their survey responses in and 27 (13%) responded online. A total of 205 surveys (response rate of 40%) were analyzed for this study.
The sample was predominantly male (n = 174, 85%), with an average age of 58 years (SD = 6.5, range = 35–71). Participants had an average education of 14 years (SD = 2.6) and completed treatment an average of 28 months prior to the study (SD = 17.9, range = 2–61). To determine whether participants differed from nonparticipants, the authors compared these two groups based on gender and age. Time following treatment completion was not compared for the participant and nonparticipant groups because the authors did not have any information regarding time following treatment completion for the nonparticipant group. The proportion of men and women in the participant and nonparticipant groups were not significantly different. There was a moderate (eta-squared = 0.1) difference (mean difference = 5.01, 95% confidence interval [CI] [1.8, 8.2]) in age between female participants (mean = 57, SD = 6.5) and female nonparticipants (mean = 52, SD = 8.74; t(75.7) = –3.05, p = 0.0032, two-tailed). Similarly there was a moderate (eta-squared = 0.12) difference (mean difference = 5.4, 95% CI [4, 6.8]) in age between male participants (mean = 58.6, SD = 6.5) and male nonparticipants (mean = 53.2, SD = 7.8; t(399.4) = -7.6, p = 0.00, two-tailed). Nonparticipants were, on average, five years younger than participants. Although the genders of participants and nonparticipants were not significantly different, the nonparticipants were significantly younger and, therefore, the results should be generalized with caution.
The Cronbach alpha for the HaNiQ was 0.92. The Cronbach alpha results for the subscales were disease profile = 0.88, treatment = 0.95, side effects = 0.9, psychosocial = 0.93, and survivorship = 0.68. 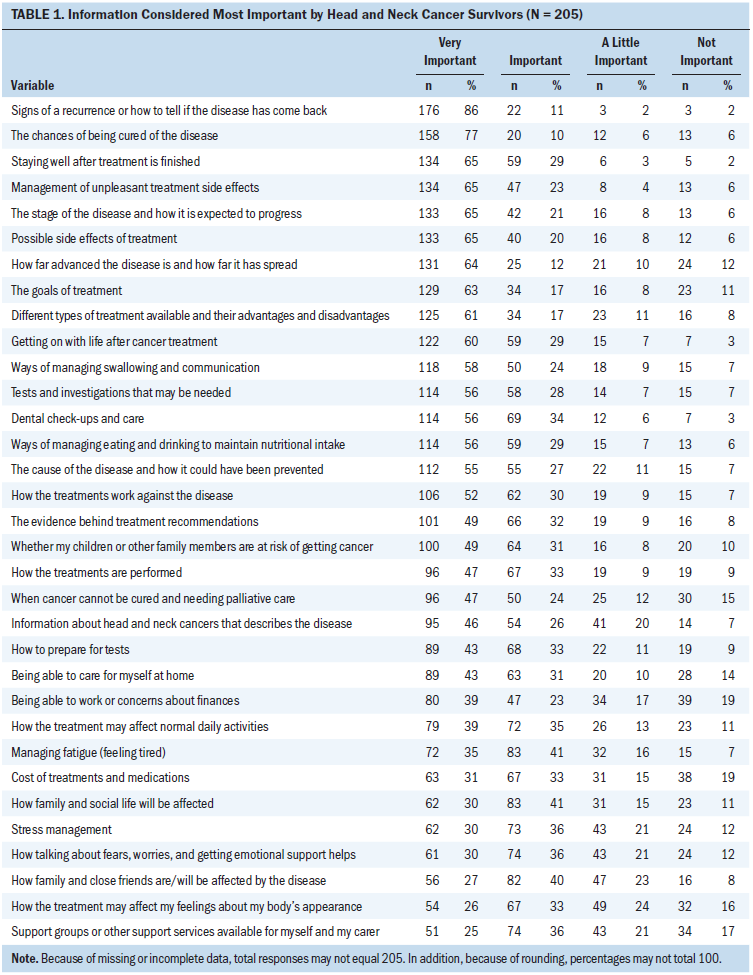
Primary Research Questions
Information considered most important: Predictably, the survivorship items of the HaNiQ were considered most important (65%), but the disease profile (58%), treatment (57%), and side effect (53%) domains were also important to participants (see Table 1). Table 2 displays additional information that participants thought was important. 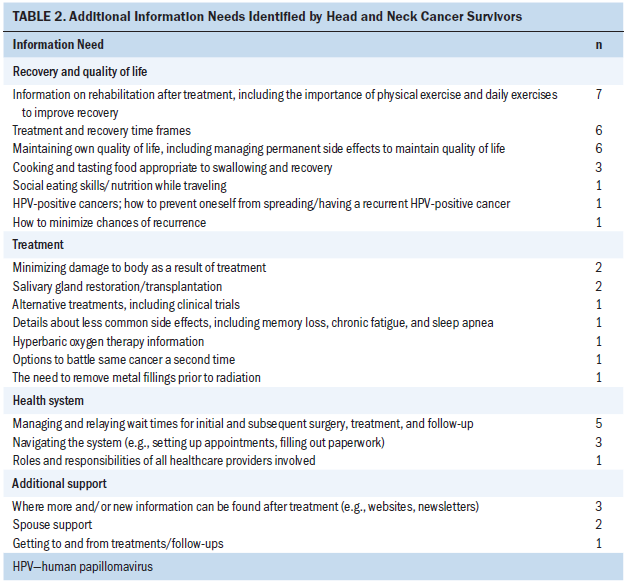
Modes of information delivery used: Source of information use items in the survey are displayed in Table 3. The source of information used most frequently are healthcare providers, followed by family and friends, the Internet, and written materials. An additional question asked participants to indicate what kind of information resources they would like to use in the future. Seventy-seven participants answered this additional question, with the Internet identified as the preferred source for future use (n = 31, 40%). Participants also wanted to use healthcare providers (n = 14, 18%), support groups (n = 12, 16%), and other individuals with cancer (n = 8, 10%). 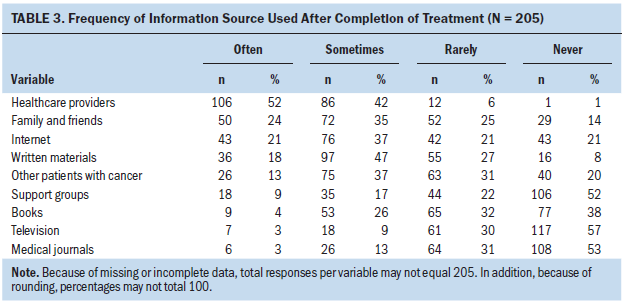
Modes of information delivery considered most helpful: Table 4 displays the reported helpfulness of various information sources. Survey participants considered healthcare providers and family and friends as the most helpful sources of information. The Internet, other individuals with cancer, and support groups were less often used by participants. 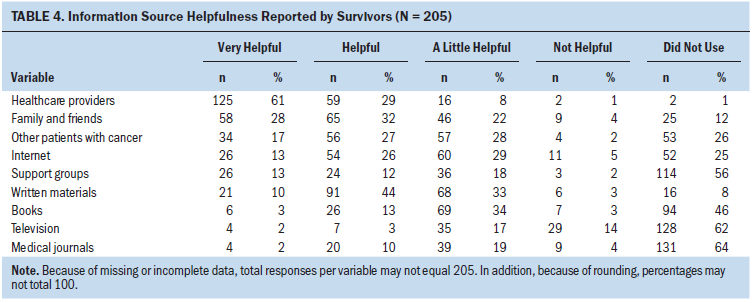
The question “Would you find an Internet-based information resource useful during recovery?” was included in the survey, and 81% (n = 157) answered “yes.” Logistic regressions were conducted to assess the ability of four factors (age, gender, education, and time since treatment completion) to predict the likelihood of finding an Internet-based information resource useful (yes or no). The full model was not statistically significant (chi-square [5, n = 191] = 7.615, p = 0.179), but those who had a high school education or less found an Internet-based information resource less useful than those with more education. Reasons given for why an Internet-based information resource was considered useful or not useful are provided in Table 5. 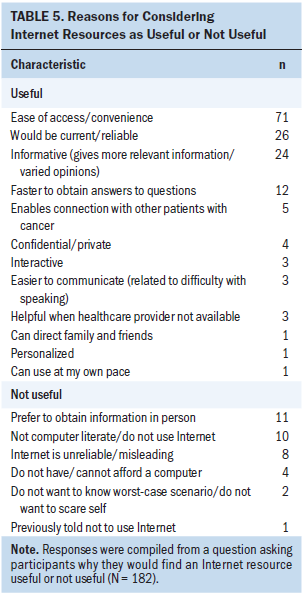
Secondary Research Questions
Power calculations were conducted as part of this phase of the study. The authors had 205 evaluable cases. For the linear regression, a sample of 205 observations provides 90% power with four predictor variables at a significance level of 5%. For the logistic regression, a sample size of 205 provides 85% power at a significance level of 5% to detect a medium effect size (odds ratio [OR] = 2). 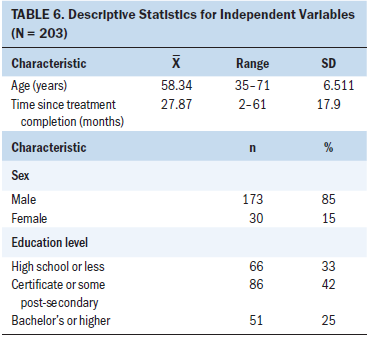
Multiple regression was used to determine whether age, gender, time since completion of treatment, and education level predicted the importance scores for the five HaNiQ information subscales (disease profile, treatment, side effects, psychosocial, and survivorship). Descriptive statistics for the independent variables are summarized in Table 6. Results of the multiple regression models are displayed in Table 7. Only statistically significant models are shown. 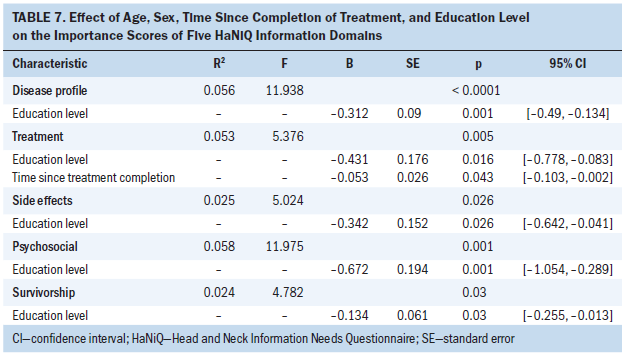
The models for the disease profile, treatment, side effect, psychosocial, and survivorship domain analyses explained 5.6%, 5.3%, 2.5%, 5.8%, and 2.4% of the variance in each model, respectively. All models were significant. Overall, level of education was the only predictor that consistently explained a significant portion of the variance in the dependent variables. Of note, the importance of information in all domains decreased as level of education increased. Time since treatment completion was only a significant independent predictor in the treatment domain, with longer times since treatment predicting lower treatment information importance scores.
Logistic regression was used to determine if age, gender, time since completion of treatment, and education level could explain the frequency of use (never, rarely, sometimes, and often) of nine sources of information (healthcare providers, written materials, the Internet, television, medical journals, books, support groups, other individuals with cancer, and family and friends). None of the nine models were statistically significant as a whole. Table 8 displays a summary of all statistically significant independent variables for each source of information. 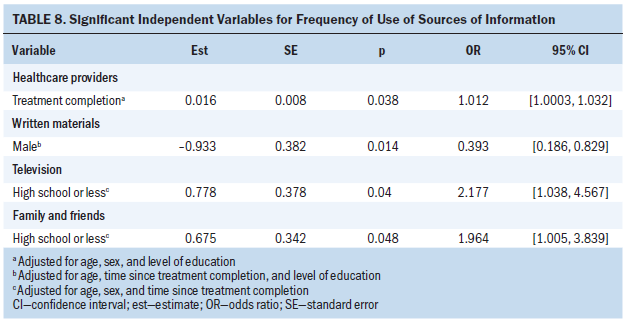
Holding all other sources of information constant, the authors noted the following:
• The use of healthcare providers as an information source increased 1.012 times for every month since treatment was completed (95% CI [1.0003, 1.0322]).
• The use of written materials as an information source was 61% less common in men than women (OR = 0.39; 95% CI [0.187, 0.829]).
• The use of television as an information source increased 2.2 times with education level (OR = 2.18; 95% CI [1.038, 4.567]).
• The use of family and friends as an information source increased 1.96 times with each level of education (OR = 1.96; 95% CI [1.005, 3.839]).
Logistic regression was used to determine if age, gender, time since completion of treatment, and education level could explain the modes of information delivery considered most helpful (healthcare providers, written materials, the Internet, television, medical journals, books, support groups, other individuals with cancer, and family and friends). None of the nine models were statistically significant, and none of the variables were significantly correlated with information source helpfulness for any of the information sources.
Discussion
Importance of Information Content
Participants identified information about survivorship as most important. In their smaller survey, Dall’Armi et al. (2009) used the same instrument to determine information needs of HNC survivors of all ages. The ratings in their study were comparable; however, more participants in the Dall’Armi et al. (2009) study rated more items as very important. It is unclear how soon after completion of treatment their study was conducted, but a shorter time frame between survey and treatment completion may explain the differences, because survivors in a more acute stage of recovery may need more information to facilitate coping (Matsuyama, Kuhn, Molisani, & Wilson-Genderson, 2013).
The findings of the current study were similar to those of several others. Chen, Lai, Liao, Chang, and Lin (2009) found that 37% of surgically treated individuals with HNC had high or moderate unmet needs regarding cancer remission, and 31% wanted to know more about “things you can do to help yourself get well.” Shea-Budgell, Kostaras, Myhill, and Hagen (2014) and Mistry, Wilson, Priestman, Damery, and Haque (2010) similarly found that survivors of cancer wanted more information on prognosis or recovery, prevention of cancer, and chances of cancer spreading or returning. Participants with HNC in a more recent study (Jabbour et al., 2017) reported that they received minimal information on effects of treatment on ability to work (45%), support groups (56%), and psychosexual health (56%) during recovery, all of which are important aspects of survivorship.
Ghazali et al. (2013) discussed fear of recurrence as a major concern for people with HNC during recovery, which could have a negative effect on survivors’ psychological well-being. They found that 35% of HNC survivors attending clinic visits consistently experienced fear of recurrence throughout the first nine months of recovery (Ghazali et al., 2013). The findings from the current study also suggest that information on signs and chances of recurrence must be discussed with HNC survivors throughout recovery to facilitate psychological coping and adjustment.
Another finding of the current study was that information about the disease, treatment, and side effects of treatment were still considered important by people with HNC in the post-treatment phase. Dall’Armi et al. (2009) and Bozec et al. (2016) found that individuals with HNC still wanted more information about disease, treatment, and side effects after treatment completion. Mistry et al. (2010) also found that individuals with cancer in the post-treatment stage still wanted to know more information about the type, cause, and symptoms of the cancer. These findings suggest that most items on the HaNiQ survey are key pieces of information that should be included in educational resources at all stages of recovery for HNC survivors at the cancer centers in Alberta.
Participants in the current study thought that, in addition to all the items included in the HaNiQ, information about financial assistance, rehabilitation, treatment/recovery time frames, maintenance of QOL, and managing wait times were also important. This is consistent with survivors of HNC in other studies who said they were not given enough information on financial support, effects of treatment on QOL, length of recovery, staying healthy after treatment, and what to expect after treatment (Dall’Armi et al., 2009; Jabbour et al., 2017; Llewellyn et al., 2006). Topics on financial assistance are clearly an important gap in current information provision in Alberta because survivors who are of working age are sometimes forced to delay return to work, or choose to reduce work hours due to physical side effects and altered functioning, leading to a loss of normality and control, reduced income, and becoming more dependent on family members (Semple et al., 2008). A unique finding of the current study was related to the importance of managing wait times for initial treatment and follow-up appointments. This may be related to the specific structure of the healthcare system in Alberta.
The scope of information needs of this patient population points to the need to equip training and practicing nurses with resources to help individuals with HNC as they move through their cancer journey. Providers of educational programs for nursing students could consider discussing these findings in educational programs to help learners better understand the broad challenges faced by individuals with HNC post-treatment. Practicing nurses value speaking directly with researchers and clinical specialists and rank in-service education and training opportunities as their primary sources of information for clinical decision making (Mills, Field, & Cant, 2009). Therefore, in-services hosted by researchers and clinical specialists could focus on anticipating the information needs of individuals treated for tumors of the head and neck associated with HPV infection and could focus on ways this information could be used to cope with the challenges during the active treatment and survivorship periods. Simple information that survivors may not feel is important at the beginning of the treatment trajectory, such as treatment and recovery time frames, navigating the health system, and referrals to social work to plan finances, may help alleviate stress if anticipated by nurses and addressed early in the cancer trajectory.
Sources of Information
Participants used healthcare providers (n = 106, 52%) most frequently to obtain information about recovery. Family and friends (n = 50, 24%), the Internet (n = 43, 21%), and written materials (n = 36, 18%) were the other primary sources of information. In multiple studies, the use of healthcare providers as the primary mode of information delivery was reported (Papadakos et al., 2017; Rogers et al., 2012; Walsh et al., 2010); however, both Rogers et al. (2012) and Papadakos et al. (2017) reported that the second most common source was leaflets (40%) and pamphlets (23%), respectively. This differs from the results of the current study; the authors found that only 18% used written materials. The authors used the term written materials in the current study, and participants may not have considered leaflets to be part of this category of information, despite getting them frequently at their follow-up appointments.
The Internet was used often by 21% (n = 43) and sometimes by 37% (n = 76) of participants in this study. Rogers et al. (2012) found that 25% of their HNC participants used the Internet often, and 15% used it occasionally. The time frame between the two data collection times in Rogers et al. (2012) and the current study—2010 and 2014—could explain the difference in occasional use. The growing popularity of the Internet as well as an influx of health-related information onto the Internet has opened this medium to a larger proportion of survivors of cancer (Crutzen et al., 2014). Shea-Budgell et al. (2014) found that the Internet was the most popular source of information, used by 57% of survivors of cancer in their survey.
Information Source Helpfulness
Survey participants considered healthcare providers as well as family and friends as the most helpful resources. Other individuals with cancer and the Internet were used less; however, they were still considered helpful or very helpful by 44% (n = 90) and 39% (n = 80) of participants, respectively, who used these resources. Overall, Dall’Armi et al. (2009) also found that their participants with HNC rated healthcare providers as most helpful, followed by the Internet and family and friends.
Eighty-one percent (n = 157) of participants thought that an Internet-based information resource would be useful during recovery. Of those who considered that it would be useful, 48% (n = 71) attributed usefulness to ease of access and convenience. Of those who felt it would not be useful, 32% (n = 11) preferred to obtain information in person, 29% (n = 10) were not computer literate, 24% (n = 8) thought the Internet was unreliable/misleading, and 12% (n = 4) did not have access to a computer/Internet. These results are similar to those of Rogers et al. (2012) who found that 35% were not familiar with computers or lacked the skill to use them. An important difference between the findings of the current study and those of Rogers et al. (2012) is that they found 37% of HNC survivors had no access to a computer, and only 7% distrusted information on the Internet. Access to computers and Internet at home and in places of employment has likely improved for society, in general, since Rogers et al.’s study was conducted (from 2007–2010). The popularity of the Internet and an influx of online health information has also sparked a new movement focused on the importance of identifying and using reliable sources on the Internet (Kowalczyk & Draper, 2012). This new development may help individuals find information online that they trust.
Factors Explaining Information Importance
The results of the current study indicated that higher education resulted in a decrease in importance of receiving information in all domains. The current results are comparable to Chen et al. (2009). Studies conducted with a variety of cancer populations had similar results (Matsuyama et al., 2011, 2013; Mistry et al., 2010). This may be because individuals with higher levels of education have the skills to find the information they require independently. The authors of the current study also found less need for treatment information as time following treatment increased, which is consistent with other studies (Mistry et al., 2010; Papadakos et al., 2017). Matsuyama et al. (2013) studied other cancer populations and demonstrated that, although information needs tend to decrease with time, total information needs remain high in the recovery period. This suggests that information provision resources of individuals with HNC in the current authors’ cancer program may be more used in the first several years post-treatment, but access to these resources should remain open for all survivors of HNC.
Factors Explaining Information Source Use
Healthcare providers were used more frequently for information as the time following treatment completion increased. Rutten, Arora, Bakos, Aziz, and Rowland (2005) obtained similar results, reporting that the use of healthcare providers increased from 27% during diagnosis and treatment to 41% post-treatment. This finding supports the importance of including healthcare providers in HNC survivorship programs in Alberta.
Areas for Future Research
The authors initially set out to complete this research as a needs assessment to inform the development of an online information resource for survivors of HNC. Because little was known about the unique needs of individuals diagnosed with tumors associated with HPV infection at the time, the needs assessment was completed to have a more comprehensive understanding of what information was considered important and of the best way to deliver this information to individuals within the target group. The natural next step would be to develop and pilot an online resource in partnership with nurses, individuals with HNC, and other stakeholders.
Of note, age was not a significant predictor in any of the models tested in this study. Future researchers could address this topic by exploring whether generation or developmental maturity, or age-related variables such as employment status, would more accurately explain outcomes. Another potentially important demographic variable to explore in further studies is marital status. On the open-ended question, several participants indicated that they wanted more information on spousal support.
Written information was used less commonly by men than women. The higher the education level of participants, the more frequently they used family and friends as a source of information. These two findings are new and warrant further investigation.
In the current study, the authors focused on information needs of individuals diagnosed with tumors associated with HPV infection in Alberta. It would be valuable to know whether similar findings could be documented in other provinces and countries. If so, healthcare providers from Alberta and these other regions could collaborate on the development of Internet-based resources for individuals who are survivors of tumors of the head and neck associated with HPV infection.
Limitations
This study has several limitations. First, although the responders and nonresponders to the survey comprise the total population of individuals who met inclusion criteria, the response rate was 40%, and responders and nonresponders differed moderately on age (nonresponders were, on average, five years younger), and, therefore, the findings should be cautiously generalized to the population. Second, the authors merged the paper-based and online-based data (87% returned the paper survey and 13% responded online), and this may have affected the findings. Third, because HPV tumor sample testing only became routine partway through the study, the proportion of people with HPV-positive HNCs in the study population is unknown. The authors chose demographic and clinical inclusion criteria for this study based on literature to maximize recruitment of individuals with HPV-associated HNC.
Implications for Nursing
Healthcare providers were the most frequently used resource by HNC survivors in the current study and, therefore, these individuals must ensure that they have comprehensive information available for HNC survivors. In addition to being considered the most trustworthy resource, healthcare providers also significantly influence cancer survivors’ health-related decisions (Shea-Budgell et al., 2014; Walsh et al., 2010). Nurse-led educational interventions have been shown to improve outcomes in individuals with cancer well into survivorship (de Leeuw et al., 2013). Consequently, nurses in Alberta could use the results of this study to ensure that educational material is congruent with needs of individuals with HNC. Advanced practice nurses (APNs), such as clinical nurse specialists and nurse practitioners, are particularly well equipped to guide the development of information resources because of their coordinating role on the interprofessional team. In addition to being clinicians and educators, APNs understand administrative and organizational functions, which can enable them to identify resources and key stakeholders necessary for appropriate information source development (Scarpa, 2004). Individuals undergoing treatment for cancer have previously reported that APNs specializing in oncology offer comprehensive and holistic care throughout the cancer trajectory (Stahlke, Rawson, & Pituskin, 2017). They are particularly skilled at anticipating physical needs, as well as providing person-centered psychosocial support (Stahlke et al., 2017). For these reasons, survivors of HNC may benefit from more APN-led oncology clinics where APNs could assist survivors of HNC with the challenges they face.
Providers of educational programs for nursing students and professional development programs for RNs could consider discussing the findings of this study in educational programs to help learners better understand the post-treatment challenges faced by individuals with HNC. The scope of information resources used by survivors of cancer in this study could also be used to teach nurses how to help survivors access trustworthy and accurate information from many difference sources.
Testing of tumor samples postoperatively to establish HPV status has only recently become routine in Alberta. More than half of the participants in the current study thought it was very important to get information about the cause of their cancer and ways it could have been prevented. Therefore, in addition to testing tumor samples, discussions about the cause of their HNC should be held with each individual with HNC and his or her family. Nurses are well positioned to help individuals with HPV-associated HNC understand the impact of HPV-positive tumors on treatment, recovery, and survivorship. Such discussions could normalize the topic of HPV and potentially prompt further dialogue about safer sexual practices, risks of HPV transmission, and HPV prevention in younger family members.
The authors found that information from healthcare providers is often being supplemented with Internet-based resources. Fifty-eight percent (n = 119) of the participants in the current study sometimes or often used the Internet, 40% (n = 31 of 77 participants who answered the question) wanted to use the Internet more in the future, and 81% (n = 148 of 182 who answered the question) agreed that an Internet-based resource would be useful during recovery. These findings demonstrate the increasing popularity of the Internet as an important source of cancer information in Alberta. A current review of Internet resources was not available; however, Dall’Armi et al. published such a review in 2009. After examining 32 HNC information resources, Dall’Armi et al. (2009) concluded that HNC information available on the Internet, at that time, was mediocre at best. Some topics that were considered important, such as being able to work and concerns about finances, how family and close friends will be affected by the disease, and how family life or social life will be affected by the disease, were barely mentioned in several of the reputable websites studied at that time. In addition, several of the most important topics, such as stress management, whether children or other family members are at risk of getting cancer, and perhaps, most alarmingly, signs of recurrence, were not included in any of the 32 Internet resources studied by Dall’Armi et al. (2009). For these reasons, nurses must be aware of the quality of Internet and paper-based resources so they can guide individuals with HPV-associated HNC to access accurate and relevant information throughout the survivorship journey. In addition, nurses in Alberta must join efforts with cancer organizations to develop more comprehensive and trustworthy Internet-based resources for people with HNC. Examples of content, which should be included in such resources, are well outlined in this study. Such an endeavor would certainly benefit the QOL of HNC survivors in Alberta. Similar studies could be replicated throughout Canada to build a better understanding of online resources that would benefit wider audiences. [[{"fid":"47391","view_mode":"default","fields":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false},"link_text":null,"type":"media","field_deltas":{"1":{"format":"default","alignment":"","field_file_image_alt_text[und][0][value]":false,"field_file_image_title_text[und][0][value]":false}},"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
Conclusion
The purpose of this study was to better understand the information needs of individuals diagnosed with tumors of the head and neck most consistently associated with HPV infection. Some themes not reported in studies with other survivors with this type of cancer, such as the need for detailed information on signs and symptoms of recurrence and cure, rehabilitation after treatment, treatment and recovery time frames, and financial assistance, were very important to the individuals who responded to the survey. In addition, the Internet as a mode of information was identified as useful from the standpoint of study participants. Finally, a reliable Internet-based information resource was regarded as very important by the majority of participants. These results suggest the need for further study of the unique information needs of individuals with HPV-associated HNC so that appropriate resources can be developed.
About the Author(s)
Oksana Saroa, RN, MN, is a site RN at Revera’s McKenzie Towne Retirement Residence in Calgary, Alberta; Anita E. Molzahn, CM, PhD, RN, FCAHS, is a professor in the Faculty of Nursing and Herbert C. Northcott, PhD, is a professor in the Department of Sociology, both at the University of Alberta in Edmonton; Karmen Schmidt, BScN, MN, NP, is a nurse practitioner at the University of Alberta Cross Cancer Institute in Edmonton; Sunita Ghosh, PhD, is a research scientist for CancerControl Alberta in Edmonton; and Karin Olson, RN, PhD, is a professor in the Faculty of Nursing at the University of Alberta in Edmonton, all in Canada. This research was funded by the Maurice and Edna Marie Minton Endowment Fund for Cancer Nursing Research (principal investigator: Oksana Saroa) from the University of Alberta. Saroa, Molzahn, Schmidt, and Olson contributed to the conceptualization and design. Saroa completed the data collection. Saroa, Northcott, and Ghosh provided statistical support. Saroa, Molzahn, Schmidt, Ghosh, and Olson provided the analysis. Saroa, Northcott, Schmidt, Ghosh, and Olson contributed to the manuscript preparation. Saroa can be reached at zimka@ualberta.ca, with copy to ONFEditor@ons.org. (Submitted February 2018. Accepted May 7, 2018.)
References
Bozec, A., Schultz, P., Gal, J., Chamorey, E., Chateau, Y., Dassonville, O., . . . Fakhry, N. (2016). Evaluation of the information given to patients undergoing head and neck cancer surgery using the EORTC QLQ-INFO25 questionnaire: A prospective multicentric study. European Journal of Cancer, 67, 73–82. https://doi.org/10.1016/j.ejca.2016.08.005
Canadian Cancer Society. (2016). Canadian cancer statistics, 2016. Retrieved from http://www.cancer.ca/~/media/cancer.ca/CW/cancer%20information/cancer%2…
Chaturvedi, A.K., Engels, E.A., Anderson, W.F., & Gillison, M.L. (2008). Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. Journal of Clinical Oncology, 26, 612–619. https://doi.org/10.1200/JCO.2007.14.1713
Chen, S.C., Lai, Y.H., Liao, C.T., Chang, J.T., & Lin, C.C. (2009). Unmet information needs and preferences in newly diagnosed and surgically treated oral cavity cancer patients. Oral Oncology, 45, 946–952. https://doi.org/10.1016/j.oraloncology.2009.06.002
Coughlan, D., & Frick, K.D. (2012). Economic impact of human papillomavirus-associated head and neck cancers in the United States. Otolaryngologic Clinics of North America, 45, 899–917. https://doi.org/10.1016/j.otc.2012.05.002
Crutzen, R., Beekers, N., van Eenbergen, M., Becker, M., Jongen, L., & van Osch, L. (2014). E-loyalty towards a cancer information website: Applying a theoretical framework. Psycho-Oncology, 23, 685–691. https://doi.org/10.1002/pon.3471
Dall’Armi, L., Forstner, D., Simpson, G., & Simpson, T. (2009). Developing information resources for people with head and neck cancer. Sydney, Australia: New South Wales Oncology Group and Cancer Institute NSW.
Dall’Armi, L., Simpson, G.K., Forstner, D., Simpson, T., Roydhouse, J.K., & White, K.J. (2013). The information needs of patients with head and neck cancer and their caregivers: A short report of instrument development and testing. Applied Nursing Research, 26, 40–44. https://doi.org/10.1016/j.apnr.2012.08.001
de Leeuw, J., Prins, J.B., Teerenstra, S., Merkx, M.A., Marres, H.A., & van Achterberg, T. (2013). Nurse-led follow-up care for head and neck cancer patients: A quasi-experimental prospective trial. Supportive Care in Cancer, 21, 537–547. https://doi.org/10.1007/s00520-012-1553-1
Forte, T., Niu, J., Lockwood, G.A., & Bryant, H.E. (2012). Incidence trends in head and neck cancers and human papillomavirus (HPV)-associated oropharyngeal cancer in Canada, 1992–2009. Cancer Causes and Control, 23, 1343–1348. https://doi.org/10.1007/s10552-012-0013-z
Ghazali, N., Cadwallader, E., Lowe, D., Humphris, G., Ozakinci, G., & Rogers, S.N. (2013). Fear of recurrence among head and neck cancer survivors: Longitudinal trends. Psycho-Oncology, 22, 807–813. https://doi.org/10.1002/pon.3069
Gold, D. (2012). The psychosocial care needs of patients with HPV-related head and neck cancer. Otolaryngologic Clinics of North America, 45, 879–897.
Heath, S., Willis, V., Allan, K., Purdie, K., Harwood, C., Shields, P., . . . Gilbert, D.C. (2012). Clinically significant human papilloma virus in squamous cell carcinoma of the head and neck in UK practice. Clinical Oncology, 24, e18–e23. https://doi.org/10.1016/j.clon.2011.05.007
Husson, O., Mols, F., & van de Poll-Franse, L.V. (2011). The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: A systematic review. Annals of Oncology, 22, 761–772. doi: https://doi.org/10.1093/annonc/mdq413
Jabbour, J., Milross, C., Sundaresan, P., Ebrahimi, A., Shepherd, H.L., Dhillon, H.M., . . . Clark, J.R. (2017). Education and support needs in patients with head and neck cancer: A multi-institutional survey. Cancer, 123, 1949–1957. https://doi.org/10.1002/cncr.30535
Johnson-Obaseki, S., McDonald, J.T., Corsten, M., & Rourke, R. (2012). Head and neck cancer in Canada: Trends 1992 to 2007. Otolaryngology—Head and Neck Surgery, 147, 74-78. https://doi.org/10.1177/0194599812437332
Kowalczyk, N., & Draper, L.J. (2012). Trends in patient information preferences and acquisition. Radiologic Technology, 83, 316–324.
Llewellyn, C.D., McGurk, M., & Weinman, J. (2006). How satisfied are head and neck cancer (HNC) patients with the information they receive pre-treatment? Results from the satisfaction with cancer information profile (SCIP). Oral Oncology, 42, 726–734. https://doi.org/10.1016/j.oraloncology.2005.11.013
Marur, S., D’Souza, G., Westra, W.H., & Forastiere, A.A. (2010). HPV-associated head and neck cancer: A virus-related cancer epidemic. Lancet Oncology, 11, 781–789. https://doi.org/10.1016/S1470-2045(10)70017-6
Matsuyama, R.K., Kuhn, L.A., Molisani, A., & Wilson-Genderson, M.C. (2013). Cancer patients’ information needs the first nine months after diagnosis. Patient Education and Counseling, 90, 96–102. https://doi.org/10.1016/j.pec.2012.09.009
Matsuyama, R.K., Wilson-Genderson, M., Kuhn, L., Moghanaki, D., Vachhani, H., & Paasche-Orlow, M. (2011). Education level, not health literacy, associated with information needs for patients with cancer. Patient Education and Counseling, 85, e229–e236. https://doi.org/10.1016/j.pec.2011.03.022
Mesters, I., van den Borne, B., De Boer, M., & Pruyn, J. (2001). Measuring information needs among cancer patients. Patient Education and Counseling, 43, 253–262.
Mills, J., Field, J., & Cant, R. (2009). The place of knowledge and evidence in the context of Australian general practice nursing. Worldviews on Evidence-Based Nursing, 6, 219–228. https://doi.org/10.1111/j.1741-6787.2009.00163.x
Mistry, A., Wilson, S., Priestman, T., Damery, S., & Haque, M.S. (2010). How do the information needs of cancer patients differ at different stages of the cancer journey? A cross-sectional survey. JRSM Short Reports, 1(4), 30. https://doi.org/10.1258/shorts.2010.010032
Papadakos, J., McQuestion, M., Gokhale, A., Damji, A., Trang, A., Abdelmutti, N., & Ringash, J. (2017). Informational needs of head and neck cancer patients. Journal of Cancer Education, 33, 847–856. https://doi.org/10.1007/s13187-017-1176-9
Powell, N.G., & Evans, M. (2015). Human papillomavirus-associated head and neck cancer: Oncogenic mechanisms, epidemiology and clinical behaviour. Diagnostic Histopathology, 21(2), 49–64. https://doi.org/10.1016/j.mpdhp.2015.02.003
Pytynia, K.B., Dahlstrom, K.R., & Sturgis, E.M. (2014). Epidemiology of HPV-associated oropharyngeal cancer. Oral Oncology, 50, 380–386. https://doi.org/10.1016/j.oraloncology.2013.12.019
Reich, M., Licitra, L., Vermorken, J.B., Bernier, J., Parmar, S., Golusinski, W., . . . Leemans, C.R. (2016). Best practice guidelines in the psychosocial management of HPV-related head and neck cancer: Recommendations from the European Head and Neck Cancer Society’s Make Sense campaign. Annals of Oncology, 27, 1848–1854. https://doi.org/10.1093/annonc/mdw272
Rogers, S.N., Rozek, A., Aleyaasin, N., Promod, P., & Lowe, D. (2012). Internet use among head and neck cancer survivors in the North West of England. British Journal of Oral and Maxillofacial Surgery, 50, 208–214. https://doi.org/10.1016/j.bjoms.2011.03.264
Rutten, L.J., Arora, N.K., Bakos, A.D., Aziz, N., & Rowland, J. (2005). Information needs and sources of information among cancer patients: A systematic review of research (1980–2003). Patient Education and Counseling, 57, 250–261. https://doi.org/10.1016/j.pec.2004.06.006
Scarpa, R. (2004). Advanced practice nursing in head and neck cancer: Implementation of five roles. Oncology Nursing Forum, 31, 579–583. https://doi.org/10.1188/04.ONF.579-583
Semple, C.J., Dunwoody, L., Kernohan, W., McCaughan, E., & Sullivan, K. (2008). Changes and challenges to patients’ lifestyle patterns following treatment for head and neck cancer. Journal of Advanced Nursing, 63, 85–93.
Shea-Budgell, M.A., Kostaras, X., Myhill, K.P., & Hagen, N.A. (2014). Information needs and sources of information for patients during cancer follow-up. Current Oncology, 21, 165–173.
Slev, V.N., Mistiaen, P., Pasman, H.R., Verdonck-de Leeuw, I.M., van Uden-Kraan, C.F., & Francke, A.L. (2016). Effects of eHealth for patients and informal caregivers confronted with cancer: A meta-review. International Journal of Medical Informatics, 87, 54–67. https://doi.org/10.1016/j.ijmedinf.2015.12.013
Stahlke, S., Rawson, K., & Pituskin, E. (2017). Patient perspectives on nurse practitioner care in oncology in Canada. Journal of Nursing Scholarship, 49, 487–494. https://doi.org/10.1111/jnu.12313
Walsh, M.C., Trentham-Dietz, A., Schroepfer, T.A., Reding, D.J., Campbell, B., Foote, M.L., . . . Cleary, J.F. (2010). Cancer information sources used by patients to inform and influence treatment decisions. Journal of Health Communication, 15, 445–463. https://doi.org/10.1080/10810731003753109
Wells, M., Cunningham, M., Lang, H., Swartzman, S., Philp, J., Taylor, L., & Thomson, J. (2015). Distress, concerns and unmet needs in survivors of head and neck cancer: A cross-sectional survey. European Journal of Cancer Care, 24, 748–760.
Wells, M., Swartzman, S., Lang, H., Cunningham, M., Taylor, L., Thomson, J., . . . McCowan, C. (2016). Predictors of quality of life in head and neck cancer survivors up to 5 years after end of treatment: A cross-sectional survey. Supportive Care in Cancer, 24, 2463–2472. https://doi.org/10.1007/s00520-015-3045-6




