Mammography Screening of Chinese Immigrant Women: Ever Screened Versus Never Screened
Purpose/Objectives: To compare the differences in mammogram completion rates over time between Chinese American women with and without a history of mammogram screening.
Design: Secondary analysis of a randomized, controlled intervention study.
Setting: Metropolitan areas of Portland, Oregon.
Sample: 300 foreign-born Chinese immigrant women aged 40 years or older. Of these, 83 women (28%) had never had a mammogram.
Methods: Participants who had not been screened with a mammogram within the past 12 months were randomized into either an education group or a control (brochure) group. All participants completed a baseline survey, which was administered again at 3, 6, and 12 months.
Main Research Variables: Mammography history, breast cancer knowledge, perceived risks, susceptibility, benefits, and common and cultural barriers.
Findings: Women who had never been screened were less likely to have insurance, a regular healthcare provider, or to have been instructed to have a mammogram. Postintervention in the education group, mammogram completion was not significantly different between those with or without a history of screening (p = 0.52). In the control brochure group, significantly more women with a history of screening had a mammogram (p = 0.03).
Conclusions: Practitioners must be aware of differential effects of education on mammography cancer screening based on women’s history of screening.
Implications for Nursing: Print material may not be as effective with women who have never been screened with a mammogram. Targeted approaches based on such understanding has the potential to decrease the breast cancer screening disparity among Chinese immigrant women.
Jump to a section
Early breast cancer detection through regular mammography screening reduces morbidity and mortality (American Cancer Society [ACS], 2013). In the United States, Asian Americans (AAs) are the fastest-growing ethnic group, and breast cancer is the most commonly diagnosed cancer for women in this population. However, AA women’s mammography rates are well below the national Healthy People project goal of 81% and consistently lower than rates for all other U.S. ethnic groups (ACS, 2013; Gomez et al., 2013; HealthyPeople.gov, 2015; Partnership for Prevention, 2007).
The target population for this study, Chinese Americans (CAs), is the largest of the AA subgroups (Humes, Jones, & Ramirez, 2011). Similar to other AA women, CA women have much lower rates of mammography screening than the general population. Several studies in the past 30 years have reported on breast cancer screening among CA women (Lee-Lin & Menon, 2005). The mammogram use and adherence rates have been reported in three different ways in the literature: at least once in a lifetime, mammogram in the past year, and mammogram in the past two years. For CA women, 12%–86% of women reported having had a mammogram at least once in their lifetimes (Lee, Lee, & Stewart, 1996; Lee-Lin et al., 2007; Tang, Solomon, & McCracken, 2000; Tu et al., 2003; Yu, Kim, Chen, & Brintnall, 2001), and 49%–61% reported having had one mammogram within the past one to two years (Lee et al., 1996; Lee-Lin et al., 2007; Tang et al., 2000; Tu et al., 2003; Yu, Seetoo, Tsai, & Sun, 1998; Yu & Wu, 2005). These rates are much below the national targeted goal of 81%.
CA immigrant women have higher breast cancer incidence than their counterparts living in Asian countries, and data from 1990–2008 indicate that CA women experienced a statistically significant 1.2% annual increase in breast cancer (Gomez et al., 2013). Cultural beliefs may influence screening behaviors among CA immigrant women. In a focus group study assessing perceptions of health, illness, and cancer screening knowledge and beliefs of 54 CA women aged 50 years or older, zero women mentioned the importance of having regular health checkups or cancer screening (Liang, Yuan, Mandelblatt, & Pasick, 2004). In addition, CA women have misconceptions and inaccurate knowledge about breast cancer and screening, and many view themselves as having a much lower susceptibility to developing breast cancer than European American women (Lee-Lin et al., 2007; Lee-Lin, Menon, Leo, & Pedhiwala, 2013). As a result, many of these women may never seek mammography screening.
Very few researchers have explored reasons why CA women rarely participate in mammography screening (Lee-Lin & Menon, 2005), and even fewer have assessed any interventions that could improve mammography screening among CA women who have never obtained a mammogram. To the authors’ knowledge, only one research group has compared CA women’s status of ever versus never screened in mammography screening. In the single study, women without a history of screening were more likely to be recent immigrants, to have lower income and limited English proficiency, and to lack regular sources of care (Wang et al., 2009). Never screened women had lower knowledge about breast cancer, had more Eastern cultural views, perceived higher barriers to screening, and reported lower intention to obtain mammograms than those with a screening history (Wang et al., 2009). However, the current authors do not know if past screening history influences how women might respond to an educational intervention designed to increase mammogram use.
To address this gap in the literature, the authors conducted a secondary analysis of a previous randomized, controlled educational intervention study to increase mammogram screening among CA immigrant women (Lee-Lin, Nguyen, Pedhiwala, Dieckmann, & Menon, 2015). In the current article, the authors report the results of the secondary analysis on the differences between CA women (N = 300; aged 40 years or older) who had never been screened versus those who had been screened, with respect to demographic characteristics, breast cancer knowledge, cultural and health beliefs, and mammography uptake in response to the educational intervention over time (at 3, 6, and 12 months). The primary study results are reported in Lee-Lin et al. (2015).
Methods
Participants
The authors recruited a convenience sample of CA immigrant women from Asian community organizations in the Portland metropolitan area in Oregon. Criteria for inclusion were (a) foreign-born Chinese woman, (b) aged 40 years or older, (c) no history of breast cancer, (d) understands and reads English or Chinese, (e) no mammogram within the past 12 months, (f) willing to provide telephone and mailing address, and (g) willing to be randomized into one of two study groups.
For this study, foreign-born Chinese women was defined as those who had immigrated to the United States and self-identified as Chinese or Chinese American. Immigrants are more likely to have diverse cultural beliefs about health and health behavior (ACS, 2009; Lee & Pacheco, 2004), and about 70% of CAs are foreign-born immigrants (Reeves & Bennett, 2004).
Design
In the parent study, the authors used a randomized, controlled trial design to test the efficacy of the intervention, a targeted breast health educational program (TBHEP), to increase mammography screening compared to a brochure control group. In this article, the authors focus on the differential effect of the intervention on women in both study groups, with respect to their history of ever having been screened with a mammogram. The intervention was divided into two parts: a one-hour group TBHEP education session preceded by individual counseling sessions with each participant within 10 days of the group class, and it was targeted to the participants’ stage of readiness to change behavior (e.g., precontemplation, contemplation) and commonly held cultural and health beliefs about breast cancer and mammography screening. The entire intervention is reported in detail elsewhere (Lee-Lin et al., 2015).
Women in the control group received a brochure that was developed by the National Cancer Institute. The brochure emphasized the woman taking care of herself now, so she can be there to care for her family later.
Procedures
Chinese community partner agencies and trained staff recruited participants and obtained their informed consent, following approval from the institutional review board at Oregon Health and Science University in Portland. For 17 months from April 2010 to September 2011, CA women were recruited and enrolled into the study. Eligibility, screening history, and stage of readiness were assessed with the following questions.
• Have you had a mammogram in the past 12 months?
• Have you had a mammogram any time before the past 12 months?
• Do you plan to have a mammogram in the next 6 months?
According to the transtheoretical model (Prochaska & Velicer, 1997), these questions are sufficient to assess stage of readiness (precontemplation and relapse precontemplation versus contemplation and relapse contemplation), and have been successfully used in previous studies with a similar target sample (Lee-Lin et al., 2013). Each participant was randomly assigned to the control or intervention group using a prepared randomization list after determining her stage of readiness to change (precontemplation and relapse precontemplation versus contemplation and relapse contemplation). At the completion of the baseline and each follow-up survey (TBHEP questionnaire), an incentive of a local supermarket gift certificate (valued at $10) was provided to each intervention and brochure group participant.
Women in the brochure group completed a 20-minute self-administered baseline survey that measured breast cancer screening knowledge, practices, perceived susceptibility, benefits, barriers, and cultural beliefs. They were also given a mammogram informational brochure and a telephone call reminder about the follow-up survey after three months.
Overall, the TBHEP intervention had a large effect (71%) on mammogram completion at 12 months postintervention. Detailed intervention effect is reported elsewhere (Lee-Lin et al., 2015).
Measures
The TBHEP Foreign-Born Chinese Women’s Questionnaire, developed and tested in previous studies (Lee-Lin et al., 2007, 2008), was used in this study. The 93-item questionnaire has four subscales: perceived susceptibility, perceived benefits, perceived barrier, and perceived cultural barriers. The Cronbach alphas of each subscale used in this survey ranged from 0.71–0.89 in previous tests for reliability (Lee-Lin et al., 2008). The Cronbach alphas of each subscale ranged from 0.64–0.9 for the current study. The detailed development and validity of the original questionnaire was reported elsewhere (Lee-Lin et al., 2008).
Statistical Analysis
The authors needed 270 women to complete the study, so 300 participants were enrolled to account for a 10% attrition rate based on prior studies with AAs for a minimum of 135 per group for 80% statistical power (Lee-Lin et al., 2007, 2015; Lee-Lin, Menon, Nail, & Lutz, 2012).
Descriptive data for all demographic and background variables were computed using SAS®, version 9.2.2. The authors compared the never screened and ever screened groups on demographic and background characteristics at baseline using chi-square and Fisher’s exact test for categorical data (Freeman & Halton, 1951) and Wilcoxon rank sum tests for continuous data. The never and ever screened groups were compared for the intervention and control brochure groups, with respect to breast cancer knowledge and cultural and health beliefs measured at baseline and 3, 6, and 12 months using the Wilcoxon rank sum tests. The authors also compared mammogram completion rates between the never and ever screened groups for the TBHEP intervention and brochure control groups at 3, 6, and 12 months using chi-square and Fisher’s exact test.
Results
Sample Demographics
From April 2010 to September 2011, the authors enrolled 300 women with a response rate of 58%. Eighty-three women (28%) had never had a mammogram in their lives (never screened), and 217 women (72%) reported being screened at least once in their lives but not in the past 12 months (ever screened). The attrition rate at 12 months for the never screened was 7.2% and 6.5% for the ever screened.
As summarized in Table 1, the majority of women were married (77%), had emigrated from mainland China (84%), and reported having received some high school education (72%). At the time of the study, the median age of the ever screened group was significantly older than the never screened group (59 years versus 53 years, p = 0.04). The ever screened group had lived longer in the United States (12 years versus 5 years, p < 0.001). Within the control group (n = 153), 24% had never been screened, and, in the intervention group (n = 147), 31% had never been screened. Women who had never been screened were less likely to have a regular healthcare provider (p < 0.001), not been told to have a mammogram by a healthcare provider (p < 0.001), and reported no insurance coverage for having a mammogram (p < 0.001).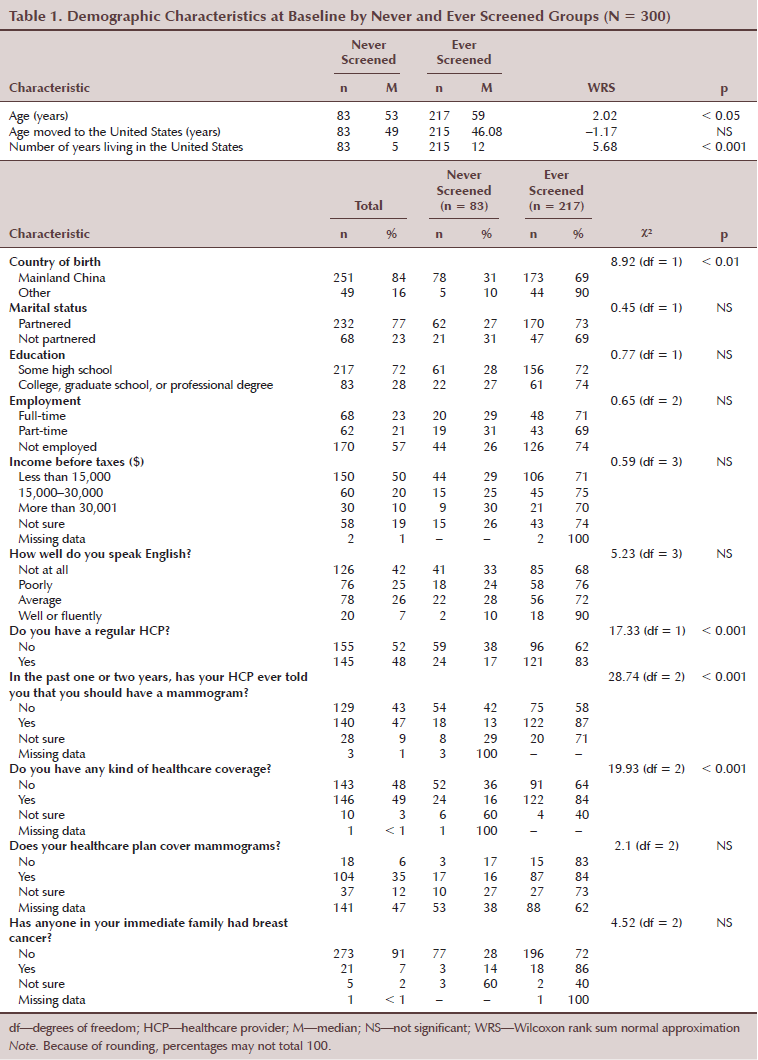
Breast Cancer and Mammography Knowledge and Cultural Beliefs
Women who had never been screened (compared to ever screened), reported higher median scores on perceived barriers (2.81 versus 2.48, p = 0.001), use of Eastern medicine (3.33 versus 3, p = 0.01) and reliance on others (3.33 versus 3, p < 0.01) at baseline (see Table 2).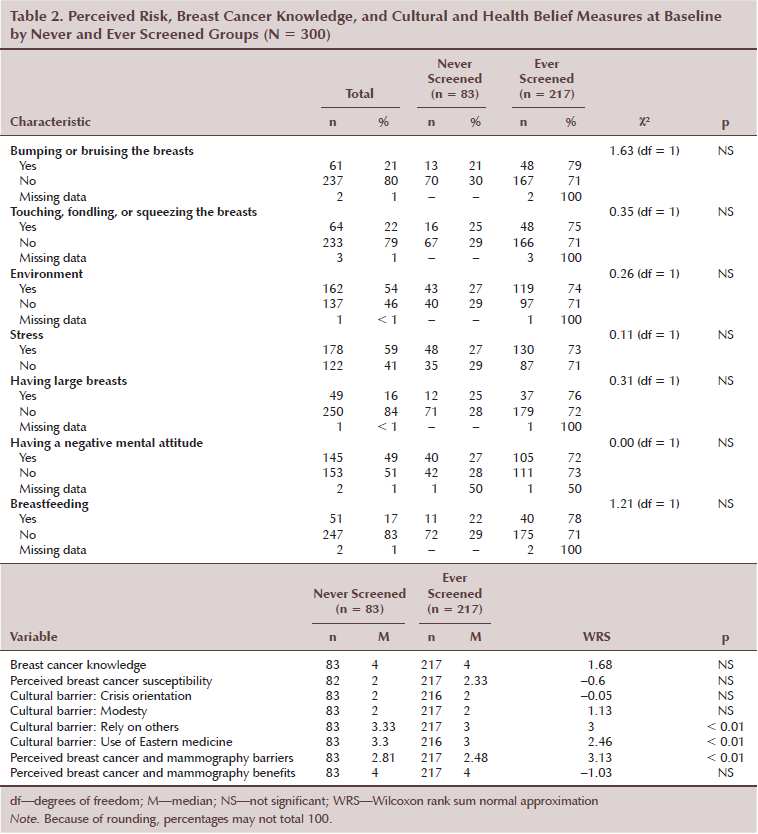
Substratification analysis on each treatment group at baseline and 3, 6, and 12 months (see Table 3) indicated that never screened women (compared to ever screened) in the control group reported significantly higher scores on the following barrier ratings: modesty concerns at 12 months, use of Eastern medicine at baseline and 6 and 12 months, reliance on others at all four time points, and breast cancer and mammography barriers at all four time points.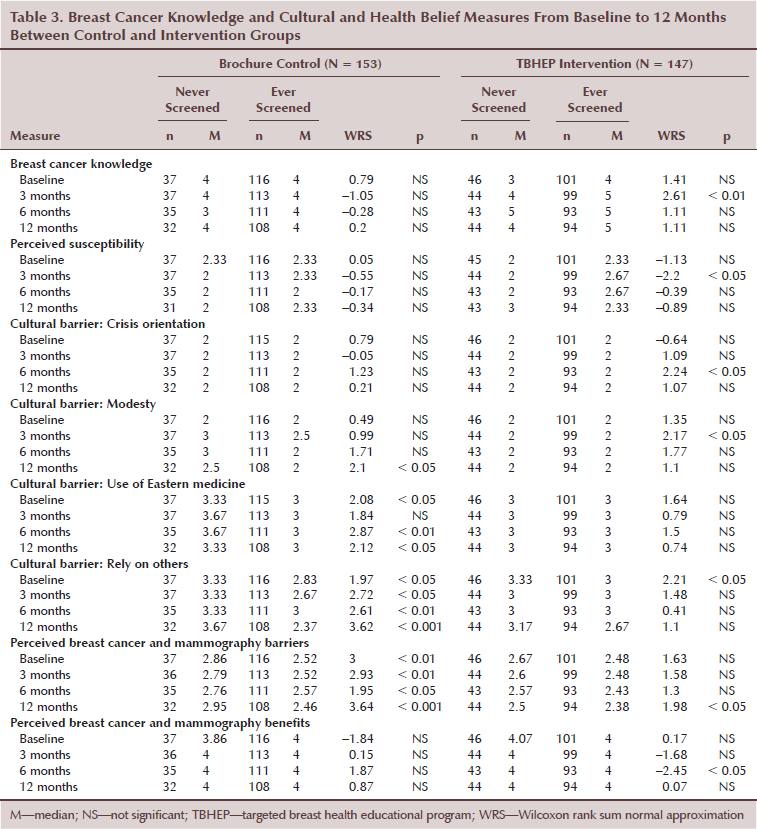
Intervention group: Never screened women reported significantly lower breast cancer knowledge and perceived susceptibility at 3 months and fewer breast cancer and mammography benefits at 6 months. They reported significantly higher scores on the following barriers: modesty concerns at 3 months, crisis orientation at 6 months, and breast cancer and mammography barriers at 12 months.
Postintervention, women with a screening history had significantly higher knowledge at 3 months when compared to the never screened group (p < 0.01). Similar patterns were noted at 3 months postintervention in susceptibility (p < 0.05) and the modesty concerns barrier (p < 0.05). Significant differences of the crisis orientation barrier (p < 0.05) and breast cancer and mammography benefits (p < 0.05) occurred at 6 months. At 12 months, significantly lower breast cancer and mammography barriers were noted in the screened group when compared to the never screened group (p < 0.05). At 12 months postintervention, mammogram completion was not significantly different among women who had never been screened when compared with those who had been screened in the past (75% versus 66%; p = 0.3).
Brochure control group: Use of Eastern medicine (p < 0.05), breast cancer and mammography barriers (p < 0.01), and reliance on others (p < 0.05) were significantly different at all three time points postintervention. At 12 months, the modesty concerns barrier score decreased significantly in the screened group when compared with the never screened group (p < 0.05).
The authors compared never and ever screened women within each treatment group, control or intervention, on mammogram completion. Mammogram completion was significantly different in the control group never and ever screened categories of women at all three time points postintervention (3 months: chi-square [1, n = 28] = 5.69, p = 0.02; 6 months: chi-square [1, n = 41] = 8.68, p = 0.003; 12 months: chi-square [1, n = 63] = 4.77, p = 0.03). In the TBHEP intervention group, the comparisons in completing their mammograms were not significantly different at all three time points postintervention (3 months: chi-square [1, n = 86] = 0.04, p = 1; 6 months: chi-square [1, n = 97] = 0.46, p = 0.5; 12 months: chi-square [1, n = 99] = 1.08, p = 0.3) (see Table 4). Women with no screening history were significantly less likely to have a mammogram (50% versus 28%; p = 0.03). History of mammography screening mattered in the brochure control group but not in the TBHEP intervention group.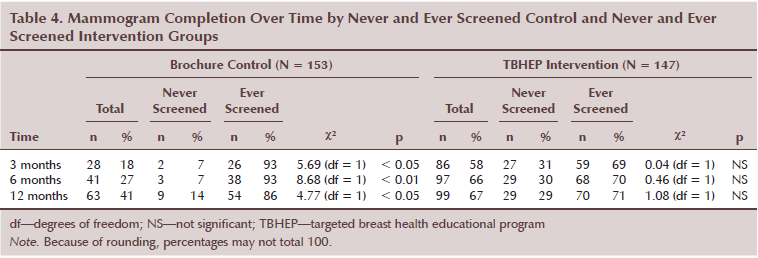
Discussion
At 12 months postintervention, mammogram completion was not significantly different among women who had never been screened when compared with those who had been screened in the TBHEP group. When women received an intensive in-person intervention, screening history was not a factor in post-intervention mammogram completion. However, in the control group, women with no screening history were significantly less likely to undergo screening. In the current study, the in-person intervention appears to have washed out the influence of past screening behavior; however, past screening was a factor in moving women to mammogram completion in the group that only received printed educational material. Given that many public programs use educational materials, such as print media, practitioners must differentiate the effects of that material based on women’s historic experiences with mammography. Print material may not be as effective with women who have never been screened before. Targeted approaches based on such understanding will go a long way toward decreasing the breast cancer screening disparity among CA women. Clinicians may want to assess past mammogram completion (even if women are not current with screening) because it may take more intensive counseling or education to encourage women who have never had a mammogram in the past.
Consistent with previous results (Wang et al., 2009), women who had never been screened with a mammogram were more likely to be recent immigrants, have Eastern views, use Eastern medicine, and perceive more barriers to getting a mammogram. They were also less likely to have a regular healthcare provider or regular sources of care and to be told to have a mammogram by a provider. However, unlike Wang et al.’s (2009) findings, knowledge and susceptibility scores at baseline in the current study were not different between the two groups with and without screening history in the sample of Chinese immigrant women. The TBHEP intervention differentially influenced knowledge postintervention between women who had ever been screened versus never been screened. Women who had ever been screened and received TBHEP improved in knowledge significantly at 3 months. Women who had never been screened improved their knowledge scores at 6 and 12 months. At 6 and 12 months, there were no longer any significant differences in knowledge scores between the two groups. A similar pattern was noted with susceptibility scores. Consistent with the authors’ past study (Lee-Lin et al., 2013), perceived breast cancer susceptibility scores increased significantly postintervention. Women in the ever screened group increased their breast cancer perceived susceptibility immediately after the TBHEP. However, the score dropped by the 12-month time point. Booster education may be needed to sustain the intervention effect.
In general and cultural barriers, women who had never been screened had higher barriers scores and relied more on others at baseline. It seemed to take longer for the intervention to take effect on barriers except for the modesty barrier (significant change at 3 months) in the TBHEP group. The crisis orientation barrier was significantly different between the two groups at 6 months, and the breast cancer and mammography barriers were significantly different between the two groups at 12 months. In the brochure control group, women had significantly lower modesty barrier scores when compared with women who had never been screened at 12 months.
In a previous study (Lee-Lin et al., 2007), perceived breast and mammography benefits did not predict mammography completion. Although CA women have a tendency to respond positively to benefit items, this did not necessarily mean they took action to have a mammogram (Lee-Lin et al., 2008). However, in this study, among those who received the TBHEP education, women who had been screened in the past had significantly higher benefit scores when compared to women who had never been screened.
Limitations
There were several limitations to this study. First, the authors used self-report to assess mammogram uptake, which may have led to under- or overreporting. Self-report of beliefs and screening behavior may be influenced by social desirability. Second, because the authors enrolled a convenience sample, participants in the study may have been more motivated to get mammograms. CA women who have low income or financial challenges may enroll in such a study because of the prospect of free mammography screening. Third, study participants were randomized to one of two groups. However, because all study participants were members of the Chinese community, there may have been contamination between groups, minimizing true between-group differences in study outcomes. Fourth, because the participants were a convenience sample recruited exclusively from the Chinese community in a single northwestern city in the United States, the results cannot be generalized to immigrant CA women living in other areas. Finally, the authors conducted multiple statistical tests given the number of study outcomes and the three time points, which increases the chances of finding differences because of chance alone. These findings should be replicated in future studies.
Implications for Nursing Practice and Research
Practitioners and policy makers must be aware of how a woman’s cultural background and past screening history affects her decision to have a mammogram. For CA women, assessment of what they have been told about mammography, both by healthcare providers and by their support systems, is important. Assisting them to find a regular healthcare provider and supporting them through a first mammogram may be crucial to their future screening behavior. In addition, differentiating the effects of printed media material based on women’s historic experiences with mammography could be helpful. Women who had never been screened reported higher barriers, lower breast cancer knowledge, and more reliance on others for assistance in obtaining health and screening care. Therefore, print educational materials may not be as effective with women who have never been screened. Assessing women’s mammography history at the initial encounter is vital.
In addition, the authors have found a consistent pattern in that many CA women view themselves as having low susceptibility to developing breast cancer (Lee-Lin et al., 2007, 2013). Simply giving printed screening material to CA women with no mammography history may not be helpful to facilitate understanding of breast cancer risk. They may need face-to-face interaction with practitioners who can explain the importance of having a mammogram, who will listen to their concerns and barriers, and provide assistance or needed navigation in obtaining screening. Growing evidence indicates that patient navigation significantly increases screening among low-income minorities (Christie et al., 2008; Freeman & Rodriguez, 2011). Navigators could be available at the community level and the hospital or clinic level to promote easy access to mammography screening (Paskett, 2012). Navigators can provide emotional support, necessary resources and guidelines, or logistic assistance on women’s journeys through health promotion or the cancer trajectory if it is found. Future research may need to focus on such targeted approaches to help decrease the breast cancer screening disparity among CA women.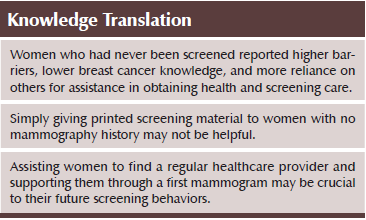
Conclusions
Women with no mammography screening history may have distinctive needs and barriers to obtaining a mammogram, and breast cancer educational programs may influence them differently. Practitioners must distinguish the effects of such programs based on women’s mammography screening history. Targeted approaches based on such understanding may help to decrease breast cancer screening disparity among CA women.
The authors gratefully acknowledge the Chinese community and the Asian Health Service Center for their support and participation in this project, as well as Judith Baggs, PhD, RN, FAAN, for her editorial assistance.
References
American Cancer Society. (2009). Breast cancer facts and figures 2009-2010. Retrieved from http://www.cancer.org/acs/groups/content/@nho/documents/document/f86100…
American Cancer Society. (2013). Breast cancer facts and figures 2013–2014. Retrieved from http://www.cancer.org/acs/groups/content/@research/documents/document/a…
Christie, J., Itzkowitz, S., Lihau-Nkanza, I., Castillo, A., Redd, W., & Jandorf, L. (2008). A randomized controlled trial using patient navigation to increase colonoscopy screening among low-income minorities. Journal of the National Medical Association, 100, 278–284.
Freeman, G.H., & Halton, J.H. (1951). Note on exact treatment of contingency, goodness of fit and other problems of significance. Biometrika, 38, 141–149. doi:10.1093/biomet/38.1-2.141
Freeman, H.P., & Rodriguez, R.L. (2011). History and principles of patient navigation. Cancer, 117(Suppl.), 3539–3542. doi:10.1002/cncr.26262
Gomez, S.L., Noone, A.M., Lichtensztajn, D.Y., Scoppa, S., Gibson, J.T., Liu, L., . . . Miller, B.A. (2013). Cancer incidence trends among Asian American populations in the United States, 1990–2008. Journal of National Cancer Institute, 105, 1096–1110. doi:10.1093/jnci/djt157
HealthyPeople.gov. (2015). 2020 topics and objectives—Objectives A–Z. Retrieved from http://www.healthypeople.gov/2020/topicsobjectives2020/default
Humes, K.R., Jones, N.A., & Ramirez, R.R. (2011). Overview of race and Hispanic origin: 2010: 2010 Census brief. Retrieved from http://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf
Lee, M., Lee, F., & Stewart S. (1996). Pathways to early breast and cervical detection for Chinese American women. Health Education Quarterly, 23(Suppl.), S76–S88.
Lee, S.M., & Pacheco, G. (2004). Cultural and language barriers to health and healthcare among Asian immigrant women. Washington, DC: U.S. Department of Health and Human Services.
Lee-Lin, F., & Menon, U. (2005). Breast and cervical cancer screening practices and inventions among Chinese, Japanese, and Vietnamese Americans. Oncology Nursing Forum, 32, 995–1003. doi:10.1188/05.ONF.995-1003
Lee-Lin, F., Menon, U., Leo, M.C., & Pedhiwala, N. (2013). Feasibility of a targeted breast health education intervention for Chinese American immigrant women. Oncology Nursing Forum, 40, 361–372. doi:10.1188/13.ONF.361-372
Lee-Lin, F., Menon, U., Nail, L., & Lutz, K.F. (2012). Findings from focus groups indicating what Chinese American immigrant women think about breast cancer and breast cancer screening. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 41, 627–637. doi:10.1111/j.1552-6909.2012.01348.x
Lee-Lin, F., Menon, U., Pett, M., Nail, L., Lee, S., & Mooney, K. (2007). Breast cancer beliefs and mammography screening practices among Chinese American immigrants. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 36, 212–221. doi:10.1111/j.1552-6909.2007.00141.x
Lee-Lin, F., Menon, U., Pett, M., Nail, L., Lee, S., & Mooney, K. (2008). Measuring breast cancer and mammography screening beliefs among Chinese American immigrants. Western Journal of Nursing Research, 30, 852–868. doi:10.1177/0193945908319247
Lee-Lin, F., Nguyen, T., Pedhiwala, N., Dieckmann, N., & Menon, U. (2015). A breast health educational program for Chinese American women: 3- to 12-month postintervention effect. American Journal of Health Promotion, 29, 173–181. doi:10.4278/ajhp.130228-QUAN-91
Liang, W., Yuan, E., Mandelblatt, J.S., & Pasick, R.J. (2004). How do older Chinese women view health and cancer screening? Results from focus groups and implications for interventions. Ethnicity and Health, 9, 283–304. doi:10.1080/1355785042000250111
Partnership for Prevention. (2007). Preventive care: A national profile on use, disparities, and health benefits. Retrieved from http://www.rwjf.org/content/dam/farm/reports/reports/2007/rwjf13325
Paskett, E.D. (2012). Cancer health disparities: Moving from why they occur to how they can be prevented. Journal of Clinical Oncology, 30, 354–356. doi:10.1200/JCO.2011.39.5947
Prochaska, J.O., & Velicer, W.F. (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12, 38–48. doi:10.4278/0890-1171-12.1.38
Reeves, T.J., & Bennett, C.E. (2004). We the people: Asians in the United States: Census 2000 special reports. Retrieved from http://www.census.gov/prod/2004pubs/censr-17.pdf
Tang, T.S., Solomon, L.J., & McCracken, L.M. (2000). Cultural barriers to mammography, clinical breast exam, and breast self-exam among Chinese-American women 60 and older. Preventive Medicine, 31, 575–583. doi:10.1006/pmed.2000.0753
Tu, S.P., Yasui, Y., Kuniyuki, A.A., Schwartz, S.M., Jackson, J.C., Hislop, T.G., & Taylor, V. (2003). Mammography screening among Chinese-American women. Cancer, 97, 1293–1302. doi:10.1002/cncr.11169
Wang, J.H., Mandelblatt, J.S., Liang, W., Yi, B., Ma, I.J., & Schwartz, M.D. (2009). Knowledge, cultural, and attitudinal barriers to mammography screening among nonadherent immigrant Chinese women. Cancer, 115, 4828–4838. doi:10.1002/cncr.24517
Yu, E.S., Kim, K.K., Chen, E.H., & Brintnall, R.A. (2001). Breast and cervical cancer screening among Chinese American women. Cancer Practice, 9, 81–91. doi:10.1046/j.1523-5394.2001.009002081.x
Yu, M.Y., Seetoo, A.D., Tsai, C.K., & Sun, C. (1998). Sociodemographic predictors of Papanicolaou smear test and mammography use among women of Chinese descent in southeastern Michigan. Women’s Health Issues, 8, 372–381. doi:10.1016/S1049-3867(98)00020-6
Yu, M.Y., & Wu, T.Y. (2005). Factors influencing mammography screening of Chinese American women. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 34, 386–394. doi:10.1177/0884217505276256
About the Author(s)
Frances Lee-Lin, RN, PhD, OCN®, CNS, is an associate professor in the School of Nursing, Thuan Nguyen, PhD, is an assistant professor in the School of Public Health, and Nisreen Pedhiwala, MS, is a research associate and Nathan Dieckmann, PhD, is an assistant professor, both in the School of Nursing, all at Oregon Health and Science University in Portland; and Usha Menon, PhD, RN, FAAN, is a professor in the College of Nursing at Ohio State University in Columbus. The study was funded by a grant (MRSGT-09-090-01-CPPB) from the American Cancer Society. Lee-Lin can be reached at leelinf@ohsu.edu, with copy to editor at ONFEditor@ons.org. (Submitted September 2014. Accepted for publication February 26, 2015.)

