Interventions to Improve Quality of Life, Well-Being, and Care in Latino Cancer Survivors: A Systematic Literature Review
Problem Identification: Hispanic/Latino cancer survivors are at risk for increased psychosocial burden, in part, because of lower survival rates and lower quality of life (QOL) when compared with other populations. Despite this, very few interventional studies have been conducted in this population. This review synthesizes research on supportive care interventions to improve QOL, well-being, and cancer care in Hispanic/Latino cancer survivors.
Literature Search: Data sources included MEDLINE®, CINAHL®, and PsycINFO®. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guideline was employed.
Data Evaluation: This review includes studies conducted with cancer survivors from diagnosis to survivorship and addresses any type of intervention for Hispanic/Latino survivors of all cancer types and sites. Studies were written in English and had a sample of at least 25% Hispanics/Latinos. Key study attributes were extracted and tabled.
Synthesis: Of the 15 studies reviewed, types of interventions included were psychosocial (n = 6), educational (n = 4), exercise/diet (n = 4), and navigational (n = 1). Most studies were pilot and feasibility studies, and nine were randomized, controlled trials (RCTs).
Conclusions: Interventional studies for Hispanic/Latino cancer survivors are at the very early stages of scientific development and are feasible and accepted by the Hispanic/Latino population. Culturally relevant psychosocial support and educational, exercise, and navigational interventions are beneficial for this population.
Implications for Research: To advance the science, as the Hispanic/Latino population rapidly increases, a great need exists for additional research in this area. A theoretical basis for interventions is needed for development of additional research. Efficacy of culturally relevant supportive care interventions needs to be tested through RCTs, replication, and multisite studies. A need exists for these developing interventions to be translated into practice to improve QOL and well-being for Hispanic/Latino cancer survivors.
Jump to a section
Cancer survivors are at risk for diminished health and well-being from cancer and cancer treatment. Effects of treatment may endure many years after diagnosis, and new treatment-related problems can present years after treatment is completed (Yabroff, Lawrence, Clauser, Davis, & Brown, 2004). Demands that confront cancer survivors are not simply a continuation of experiences that occur during the cancer treatment phase; they are unique problems along the cancer continuum, as the person treated for cancer progresses into survivorship (Feuerstein, 2007). Persistent effects include physical and psychological symptoms and social and spiritual impact. Cancer survivors are at risk for comorbid illness, functional limitations, difficulties with returning to work and other role transitions, uncertainty, fear of recurrence, and barriers to quality health care, all of which complicate their lives (American Cancer Society, 2012; Ganz, 2006; Haylock, 2006; Hewitt, Greenfield, & Stovall, 2005; McNulty & Nail, 2015). Growing attention is being paid to the needs of post-treatment cancer survivors and the vital role of supportive care interventions, as well as interventions to promote health and wellness (Wolin & Colditz, 2011). When patients receive psychosocial support, they are better able to manage the challenges of everyday life after cancer and cancer treatment (Schmid-Büchi, Halfens, Müller, Dassen, & van den Borne, 2013). Despite this, the literature is replete with accounts of significant unmet needs with regards to supportive care for cancer survivors (Beesley, Price, Webb, O’Rourke, & Marquart, 2013; Carey et al., 2012; Sanson-Fisher et al., 2000).
Insufficient attention has been given to the supportive care needs of ethnic minority and underserved patients with cancer, who are at risk for psychosocial morbidity (Eversley et al., 2005; Moadel, Morgan, & Dutcher, 2007; Nápoles, Ortíz, O’Brien, Sereno, & Kaplan, 2011). Hispanics/Latinas are dis-proportionally affected by cancer and are more likely to be diagnosed with breast cancer at later stages and to experience lower five-year survival rates (Kingsley & Bandolin, 2010). Hispanic/Latina breast cancer survivors are diagnosed at younger ages, have higher rates of advanced breast cancer, have lower survival rates than their Caucasian counterparts (Wu et al., 2012), and have demonstrated lower qualiy of life (QOL) (Yanez, Thompson, & Stanton, 2011).
Underserved populations, particularly Hispanics/Latinos, experience an increased burden with regard to the biopsychosocial impact of cancer (Ashing-Giwa, Rosales, Lai, & Weitzel, 2013; Moadel, Morgan, et al., 2007). One study found that Hispanics/Latinos were more likely to report poor mental, physical, and social QOL when compared with Caucasians and African Americans (Yanez et al., 2011), as well as lower perceived social support, high levels of uncertainty (Sammarco & Konecny, 2010), and higher levels of depression (Ashing-Giwa et al., 2013). Hispanic/Latino cancer survivors had the highest level of unmet supportive care needs (informational, practical, supportive, and spiritual) when compared with African Americans and Caucasians (Moadel, Morgan, et al., 2007).
Several studies have focused on the determinants of QOL in Hispanic/Latino cancer survivors, but evidence is developing for which concepts, including cultural ones, are most influential (Lopez-Class et al., 2011). Variations in ethnic groups with regard to QOL may have numerous explanations, including differences in access to and quality of cancer care (Rodríquez, Bustamante, & Ang, 2009; Perez, Ang, & Vega, 2009), cultural beliefs, and the influence of immigration (Ashing-Giwa, Padilla, Bohórquez, Tejero, & Garcia, 2006; Buki et al., 2008; Eversley et al., 2005; Nápoles-Springer, Ortíz, O’Brien, Díaz-Méndez, & Pérez-Stable, 2007). Despite these differences, minimal interventional studies have been conducted to improve QOL in Hispanic/Latino cancer survivors (Wolin & Colditz, 2011). Culturally relevant interventions are revised and tailored to a cultural group’s traditional views, values, and lifestyles (Castro, Barrera, & Martinez, 2004). Such interventions are needed to reduce the psychosocial burden in this population. The purpose of this systematic review is to examine interventional studies that have been conducted to improve the QOL in adult Hispanic/Latino cancer survivors, to evaluate the body of evidence for feasibility and efficacy of existing studies, and to suggest next steps.
Methods
This article uses the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) format (Moher, Liberati, Tetzlaff, & Altman, 2009) guideline. A search was conducted for publications in English from 1994–2014 that focused on interventions for Hispanic/Latino survivors. The researchers selected studies addressing any interventions for cancer survivors of all cancer types and sites and having a sample in which at least 25% of participants were identified as Hispanic/Latino. All types of interventions were included. The researchers excluded studies that focused on prevention and surveillance. Other reasons for exclusion were not addressing postdiagnosis cancer survivors and Hispanics/Latinos not being separated out as a group in the results.
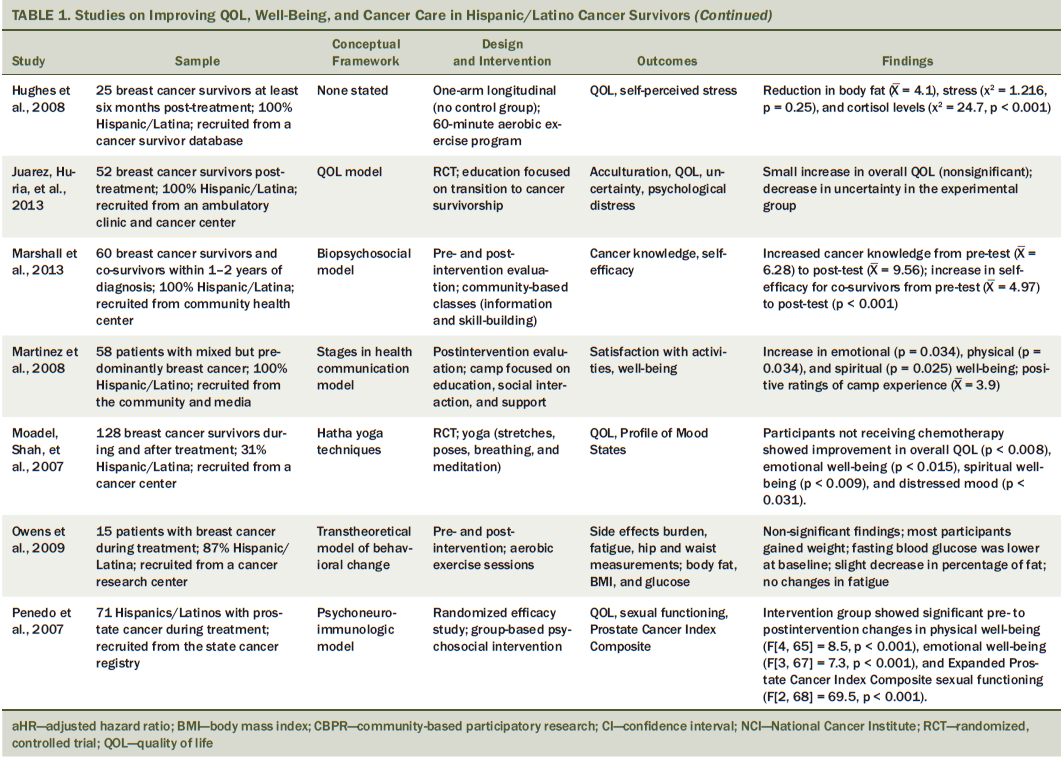
The studies were categorized by sample description, study design, theory or model used (if any), cancer type and site, type of intervention, major findings, and implications. If participants received evaluation of the intervention before and after, it was considered a pre-/post-test design. Studies were considered to be randomized control if participants were assigned randomly to either an intervention or control group. If studies used any theoretical framework or model, then it was further described. The researchers identified cancer types and sites, as well as where participants were along the cancer continuum (see Table 1). This review focused on studies conducted in cancer survivors from diagnosis to survivorship.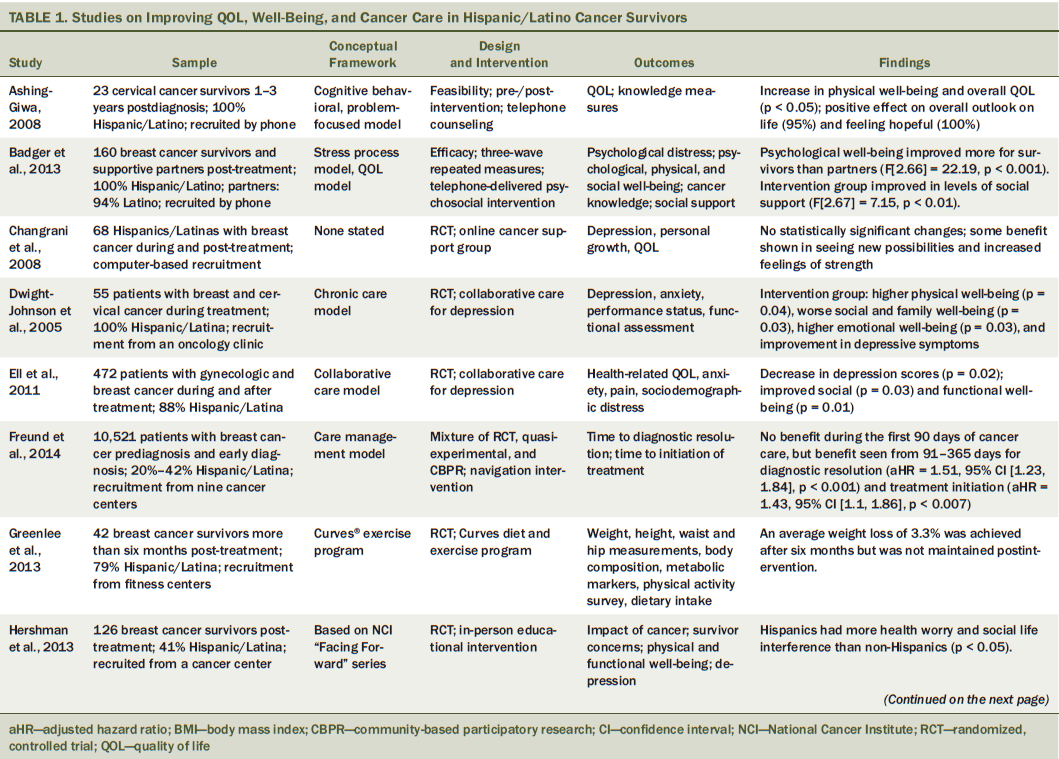
Results
Database searches yielded 468 articles. Two researchers independently screened the titles and abstracts of the studies brought up by the keyword searches. The majority of the studies focused on prevention and surveillance, did not focus on Hispanics/Latinos, and were descriptive studies and, therefore, did not meet inclusion criteria. A total of 15 studies remained after the deletion of duplicates between the searches and the application of the inclusion criteria (see Figure 1). Of the 15 articles included in this review, six were studies testing psychosocial support, four addressed educational programs, four were exercise interventions, and one focused on navigation. 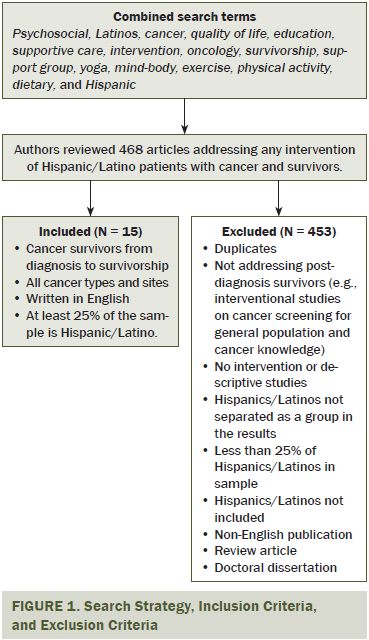
Psychosocial Support Interventions
Six studies met the sample criteria that are classified as psychosocial support interventions. One study focused on men with prostate cancer (Penedo et al., 2007), and the rest included women diagnosed with gynecologic or breast cancer. Of these, one study included partners, but the person diagnosed was female (Badger et al., 2013). Several studies used at-home interventions including telephone and computer, two were conducted in oncology clinics, and one was conducted at a university. All but one study (Ell et al., 2011) had 100% Hispanic/Latino participants. The study samples were a mixture of cancer survivors currently receiving treatment and those who were post-treatment. All studies in this group used bilingual or monolingual Spanish interventions. QOL was the overarching theme and, generally, the primary outcome measure.
Ashing-Giwa (2008) conducted a small feasibility study implementing culturally sensitive interventions in a telephonic format for patients with cervical cancer considered to be disease-free. Participants were offered either a six-session telephone counseling session with a survivorship kit or a survivorship kit alone. Badger et al. (2013) studied the efficacy of two telephone interventions for psychosocial support of Hispanic/Latina breast cancer survivors in the acute phase of care and their supportive partners, to study decreased distress and improvement in QOL. Dyads were randomly assigned to one of two interventions for eight weeks—telephone interpersonal counseling (TIP-C) or telephone health education (THE). TIP-C addressed mood and affect management, emotional expression, interpersonal communication and relationships, social support, and cancer information, and THE focused on normal breast health and routine tests for the diagnosis and prevention of breast cancer, treatment, side effects of treatment, and interventions to combat these side effects.
Another study (Changrani et al., 2008) examined the viability of online support groups (OSGs) with Spanish-language intervention. Those in the intervention group received 90-minute OSG sessions for 30 weeks through the Virtual Community for Immigrants With Cancer. Issues of interest to the group were discussed, including symptom management, side effects, family concerns, and alienation. Penedo et al. (2007) explored the efficacy of a 10-week group-based cognitive-behavioral stress management intervention. Patients were randomly assigned to this intervention or a half-day stress management seminar (control group). Dwight-Johnson, Ell, and Lee (2005) sought to determine whether collaborative depression care programs could be adapted in public sector oncology clinics that service low-income Hispanic/Latino patients with breast and cervical cancer. In this study, patients were randomly assigned to the collaborative care intervention or usual care for depression. In the collaborative care group, patients were educated about antidepressants and problem-solving therapy and allowed to choose either as their first-line depression treatment. During problem-solving therapy, patients met with a social worker weekly for eight weeks, and for the medication intervention, patients received follow-up from the oncologist.
Ell et al. (2011) assessed long-term outcomes of low-income patients after treatment in the collaborative care model for depression. Patients were randomly assigned to enhanced usual care or the intervention using the collaborative model. For those in a 12-month intervention group receiving acute treatment, social workers provided problem-solving therapy and healthcare system navigation, a psychiatrist prescribed antidepressants based on preference and need, and side-effect monitoring was done by telephone. Telephone calls were made once per month and included monitoring symptoms and one or more problem-solving therapy “booster” sessions delivered in person or via phone, and motivational support. Outcomes for patients were measured at 12 months, 18 months, and 24 months.
All but one study (Changrani et al., 2008) showed statistically significant improvements based on the interventions. Measures included physical well-being, QOL measures, psychological well-being, depressive symptoms, social well-being, functional well-being, emotional well-being, and sexual functioning. The study by Changrani et al. (2008), despite not having statistically significant findings, did show some statistical trends for seeing new possibilities and increased feelings of strength. Participants in this online intervention expressed gratitude for the ability to have someone to talk to about their situation.
Educational Interventions
Four studies were identified as educational interventions for Hispanic/Latino cancer survivors. Of those four studies, two were randomized, controlled trials (RCTs) and two were non-randomized trials with pre- and postintervention evaluation. Three of the studies targeted breast cancer survivors only (Hershman et al., 2013; Juarez, Mayorga, Hurria, & Ferrell, 2013; Marshall et al., 2013), and one study targeted various cancer types (Martinez, Aguado Loi, Martinez, Flores, & Meade, 2008). All study samples were post-treatment cancer survivors.
All educational intervention studies were bilingual (English and Spanish), and three studies used culturally relevant educational materials by using a theoretical conceptual framework. For example, Marshall et al. (2013) used the family systems and sociocultural theory as a conceptual framework to examine the need for consideration of social class and culture for Hispanic/Latino cancer survivors. Most educational intervention studies addressed multiple content areas and used more than one teaching method. For example, Juarez, Hurria, Uman, and Ferrell (2013) examined the effects of an English/Spanish educational intervention to provide Hispanic/Latina breast cancer survivors and their co-survivors with structured information about high incidence of QOL concerns and strategies to assist them. The education included physical, psychological, social, and spiritual components specific to breast cancer. Individually tailored follow-up counseling support via telephone was integrated upon completion of the four sessions.
Martinez et al. (2008) developed a three-day cancer camp for adult Spanish-speaking Hispanic/Latino cancer survivors. This intervention included three key components: (a) education on nutrition, stress management, relaxation, and cancer resources; (b) social interaction with morning walks and exercise; and (c) group discussion and counseling to increase the support network. Marshall et al. (2013) conducted a pre- and postintervention, offered as a free community health service with classes delivered by a trained counselor and a promotora (a community health worker employed by the partner community health center), for either low-income Hispanic/Latina breast cancer survivors or co-survivors. The intervention, named “Un Abrazo Para La Familia” (A Hug for the Family), provided evidence-based cancer information about coping with cancer and caregiving, an explanation of depression as a treatable illness, and information about the risks of breast cancer. Hershman et al. (2013) used a single-blinded randomized trial to examine the effect of an in-person survivorship intervention following adjuvant breast cancer therapy on health worry, treatment satisfaction, and the impact of cancer when comparing Hispanic and non-Hispanic ethnic groups at baseline, three months, and six months. Participants receiving the survivorship intervention met with a nurse practitioner and nutritionist for about one hour and received a personalized treatment summary, surveillance recommendations, discussion of risk for late effects and toxicities, and screening and lifestyle recommendations (in English or Spanish).
Two studies (Marshall et al., 2013; Martinez et al., 2008) found statistically significant positive effects of their intervention on at least one of the expected outcomes (e.g., physical, psychological, social, spiritual well-being, self-efficacy, cancer knowledge). For example, results from Martinez et al. (2008) revealed an increase in emotional, physical, and spiritual well-being scores after a cancer camp. Juarez, Huria, et al. (2013) did not find a statistically significant effect of the intervention on QOL between the experimental and control groups, but the four domains of QOL increased slightly in both groups or remained unchanged.
Exercise Interventions
Four studies that met the sample criteria used exercise interventions. Of these four studies, two used randomized designs (Greenlee et al., 2013; Moadel, Shah, et al., 2007), and two were pre-/post-test one-arm longitudinal studies (Hughes, Leung, & Naus, 2008; Owens, Jackson, & Berndt, 2009). All four studies were conducted in breast cancer survivors. These studies spanned the postdiagnosis continuum, with one being conducted during treatment (Owens et al., 2009), one with a mixed-treatment and after-treatment sample (Moadel, Shah, et al., 2007), and two focused on cancer survivors greater than six months after treatment (Greenlee et al., 2013; Hughes et al., 2008). None of the articles described any sort of cultural tailoring with regard to the interventions. Two studies included samples that were predominantly Spanish-speaking (Hughes et al., 2008; Moadel, Shah, et al. 2007), one study was mixed (Greenlee et al., 2013), and one study did not describe the preferred language of the sample (Owens et al., 2009). One study provided materials in English and Spanish (Greenlee et al., 2013). Two studies used an exclusively fitness-focused intervention (Hughes et al., 2008; Owens et al., 2009), one study was a combination of an exercise and diet regimen (Greenlee et al., 2013), and one study included fitness with mind and body components (Moadel, Shah, et al., 2007).
Owens et al. (2009) conducted a small feasibility study of a structured exercise intervention in a sample of early-stage breast cancer survivors during treatment. This study used a mixed-method, longitudinal, and pre-/post-test quasi-experimental design. The intervention, informed by the Transtheoretical Model of behavioral change, consisted of exercising three times a week for one hour during a period of six months. Exercises were designed to increase the heart rate to a calorie-burning range. Barriers to adhering to the program were identified, revealing that some participants had difficulty setting aside time to exercise. Reasons for participation included appearance, social support, feeling better as soon as possible, and learning to focus on themselves.
Moadel, Shah, et al. (2007) conducted an RCT of yoga in a multiethnic sample of patients with breast cancer within five years of diagnosis. Using a randomized, wait-list control design, the intervention consisted of 12 sessions, lasting 90 minutes each week. The intervention was based on Hatha yoga techniques, was co-developed by an oncologist and a yoga instructor, and consisted of three major yoga components: physical stretches and poses, breathing exercises, and meditation. Favorable outcomes for the intervention group included an improvement in overall QOL; an improvement in emotional, social, and spiritual well-being; and a decrease in distressed mood. One cited limitation was that only 69% of the participants attended the classes.
Hughes et al. (2008) conducted a pilot study to determine the effectiveness of an individualized and home-based exercise intervention in post-treatment breast cancer survivors. The study had a one-arm, longitudinal design with a single-system analysis (no control group). The intervention included aerobics, flexibility, and muscle conditioning, but the frequency of the exercise program was not described. The outcomes included measures of physical fitness, QOL, self-reported stress, and salivary cortisol levels. The duration was 60 minutes per week during a 10-week period.
Greenlee et al. (2013) tested the feasibility of the commercial Curves® program on breast cancer survivors who were at least six months post-treatment. The study design was a crossover with wait-list control. In the immediate intervention arm, participants engaged in the Curves program for six months, followed by six months of the diet and exercise program of their choice. In the wait-list control group, the participants were encouraged to not participate in any particular weight loss or exercise program for the first six months, followed by participating in the Curves program for six months. The Curves program nutrition course consists of promoting a high-vegetable and low-fat, low-calorie diet. The exercise program consisted of 30 minutes of strength training and low-impact aerobic exercise 3–5 days per week. This pilot study found that recruiting and retaining breast cancer survivors to a randomized weight loss trial is feasible.
Statistical significance of study outcomes varied across these studies considerably. One study (Greenlee et al., 2013) had no significant findings, but the majority of the studies showed some significant changes in biologic study variables, such as salivary cortisol levels (Hughes et al., 2008) and well-being measures (Moadel, Shah, et al., 2007). None of the studies showed a statistically significant or maintained weight loss in the participants, an outcome that often is measured in exercise intervention studies (Hughes et al., 2008; Owens et al., 2009). Several studies did show trends in a positive direction (i.e., moderate weight loss), which provided evidence to support conducting the studies in larger samples (Greenlee et al., 2013; Hughes et al., 2008; Moadel, Shah, et al., 2007; Owens et al., 2009), with an additional focus on adherence to the intervention (Greenlee et al., 2013; Moadel et al., 2007; Owens et al., 2009).
Navigation Intervention
Using a mixture of a randomized and a quasi-experimental design, Freund et al. (2014) investigated the efficacy of a patient navigation intervention that focused on preventing delays in care in a mixed sample of participants who were newly diagnosed. This was a large study across nine cancer centers. No benefit was found during the first 90 days of cancer care, but a benefit was seen from 91–365 days for time from initial screening test to diagnostic confirmation, and time from screening to treatment initiation.
Discussion
In this review, the researchers searched a large body of literature on interventional studies for Hispanic/Latino cancer survivors from three major databases, finding 15 studies meeting the study inclusion criteria. Studies meeting inclusion criteria were limited because many studies had no intervention component or focused on preventive behaviors. This article synthesizes the existing literature on a variety of interventions that focused on psychosocial support, education, exercise, and patient navigation in Hispanic/Latino cancer survivors. The researchers found that, although this is a new and developing area of research, most of the interventions were feasible, effective, and showed promise for additional studies. This review provides evidence to support the effectiveness of several types of interventions with this population.
The most effective types of interventions found in the psychosocial support studies were largely RCTs or had a pre-/post-test design. Most were short-term interventions, with only one looking at the long-range effects of supportive interventions (Ell et al., 2011). These studies had a strong theoretical basis, such as the collaborative care model, and they employed well-founded techniques to adapt the intervention to Hispanics/Latinos. They provided evidence that phone and online psychosocial support interventions are feasible in this population.
The educational interventions deployed bilingual and culturally relevant interventions. They also showed that Hispanic/Latina breast cancer survivors may experience a greater amount of uncertainty related to their lack of understanding about breast cancer, side effects of cancer, financial concerns, and fear of recurrence. Additional interventions should address these concerns and decrease uncertainty in Hispanic/Latina breast cancer survivors.
In the exercise intervention studies, a lack of cultural tailoring of the interventions was most notable. This could be due, in part, to the fact that most of the samples included a variety of ethnic and cultural groups. These studies also suffered from lack of adherence to the intervention and difficulties in retaining participants in control groups. Designing culturally relevant attention control groups, such as educational support interventions geared toward the population, may assist with study retention and help with increasing sample sizes.
Eight of the 15 studies described a conceptual model or framework that guided the study. The most common model used was a QOL model, which identifies areas of focus for outcomes but does not affect how or why an intervention may be effective. The collaborative care model guided the studies that focused on reducing depression in survivors and resulted in well-designed studies. Other models were very specific, such as the Hatha yoga techniques and the psychoneuroimmunologic model, which informed a stress reduction technique for prostate cancer survivors. Using well-developed and tested models that guide intervention design and targeted outcomes could strengthen this body of work.
Across all studies, intervention fidelity rarely was described. Several studies described lack of adherence to the intervention, which could have contributed to nonsignificant findings. In the exercise studies, not addressing cultural relevance also could have contributed to nonsignificant findings. Across all types of studies, various combinations of interventions were frequent (i.e., education/support and diet/exercise). This makes sorting out which component of the intervention is contributing to which outcomes challenging. Another issue was the heterogeneity of outcome measures, which makes comparing across studies a challenge.
Limitations
Half of the studies included mixed ethnicity samples, not allowing for the full cultural adaptation to the Hispanic/Latino population to occur. For the studies that included 100% Hispanic/Latino participants, which were mostly the psychosocial support and educational interventions, cultural adaptation techniques were more fully developed. On the contrary, in the exercise studies, none of the articles described any efforts at cultural tailoring of the interventions. In the navigation study, the focus was to obtain a multiethnic sample, not necessarily targeted to the Hispanic/Latino culture. Because many of the studies were not specific to Hispanics/Latinos, drawing conclusions specific to this population is challenging. The interventions described are applicable to broader populations.
The findings showed that two-thirds of the interventional studies focused on breast cancer. Although breast cancer is one of the most common forms of cancer diagnosed in Hispanics/Latinas (Wu et al., 2012), because of the synthesis of this literature with unbalanced gender and cancer types, the researchers could not generalize the findings to other types of cancer survivors. Additional studies need to examine different types of interventions for other cancer survivors and increase the representation of males.
Very few of the studies engaged in community-based participatory research strategies, which potentially could be more favorable in designing effective and sustainable interventions. Very few studies measured the level of acculturation of the sample, and not all provided the primary language of the participants. Overall, the studies were pilots with small sample sizes and lacked control groups and randomized designs. Although they were able to demonstrate that, for the most part, the interventions were feasible, these design issues show that larger and more robust studies are needed in this population, with stronger cultural tailoring strategies.
In the psychosocial support studies, no studies tested interventions that included in-person group support with family engagement for Hispanic/Latino cancer survivors. This is in contrary to the Hispanic/Latino value of familismo, or familism, and the importance of maintaining a connection with close and extended family. Two educational interventions did include family members in the intervention (Juarez, Hurria, et al., 2013; Marshall et al., 2013). Additional Hispanic/Latino values, such as personalismo (valuing personal relationships more than institutional), confianza (establishing trusting relationships), simpatia (pleasant, polite, and nonconfrontational social interactions), and respeto (demonstrating respect to others) need to be considered when designing survivorship interventions for Hispanics/Latinos (Juarez, Mayorga, et al., 2013).
Issues with intervention adherence, fidelity, and cultural tailoring have been previously discussed and create limitations for this body of work. Very few of the studies were focused exclusively on patients during treatment, and most samples were a mixture of cancer survivors receiving treatment and post-treatment cancer survivors, or exclusively post-treatment cancer survivors. An opportunity exists for Hispanics/Latinos undergoing treatment to have a stronger voice in this body of research and proactively address QOL concerns.
The researchers searched the published literature through October 2014, so published literature after this date was not included in the review. Although the researchers implemented rigorous searching techniques and a wide variety of search terms, all pertinent studies may not have been found. In addition, the risk of publication bias always exists because of the fact that many studies with nonsignificant findings are not published. Because of the variation and heterogeneity of intervention type and outcomes measured, the researchers were unable to conduct a meta-analysis across studies.
Implications for Practice
Hispanic/Latino cancer survivors can benefit from referrals to interventions that are brief and accessible, and based on an individualized needs assessment. Ongoing psychosocial and functional assessments across the cancer continuum can help identify who may be at risk and what type of interventions would be most appropriate for that individual. For example, if a cancer survivor is screened positively for depression, he or she may be referred to a collaborative care model if available. With regard to depression and other psychosocial concerns, collaboration between the oncologist and primary care provider is needed. Phone and Internet support interventions could be cost-effective options for clinical agencies.
Long-term follow-up of cancer survivors in practice and research is important. Most patients with cancer are transferred to primary care, which may not be as familiar with the needs of the population (Ganz, 2009). More work is needed to translate these findings into practice and reach clinicians to help improve culturally relevant supportive care. A paucity of interventions are available for this population, and limited referral opportunities may be accessible because these studies are, for the most part, preliminary and have not yet resulted in long-term program development available to patients. As this work develops, creating a local or national list of referral resources for oncology, survivorship, and primary care providers who care for the Hispanic/Latino population would be invaluable. Patient engagement in the design of the interventions is also paramount. Patient and community engagement in the design of the intervention is also paramount for the Hispanic/Latino population because of the importance of cultural and linguistic relevance.
Conclusion
This systematic review of the published literature clearly has shown that interventional studies for Hispanic/Latino cancer survivors are at the very early stage of scientific development. This is the first article, to the researchers’ knowledge, that focuses on this segment of the cancer trajectory from diagnosis forward. The researchers have provided evidence that most of the interventions that have been tested are feasible and accepted by the Hispanic/Latino population and warrant additional study through replication and larger multisite studies. The evidence provides support of the notion that culturally relevant psychosocial support, educational, exercise, and navigational interventions have benefits for this population. Hispanic/Latino cancer survivors are at risk for negative outcomes and may not have access to these types of support services. A sense of urgency exists to move the science forward in this area, translate the findings into practice, and develop sustainable programs to effectively serve the Hispanic/Latino population.
The authors dedicate this article to the memory of Julie McNulty, RN, PhD, CPHQ, who died shortly prior to publication. The authors gratefully acknowledge her contribution in developing this article as first author. Her passion for and dedication to improving health and wellness for patients with cancer and survivors will be remembered.
References
American Cancer Society. (2012). Cancer treatment and survivorship facts and figures 2012–2013. Retrieved from http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/docum…
Ashing-Giwa, K., Rosales, M., Lai, L., & Weitzel, J. (2013). Depressive symptomatology among Latino breast cancer survivors. Psycho-Oncology, 22, 845–853. doi:10.1002/pon.3084
Ashing-Giwa, K.T. (2008). Enhancing physical well-being and overall quality of life among underserved Latina-American cervical cancer survivors: Feasibility study. Journal of Cancer Survivorship, 2, 215–223. doi:10.1007/s11764-008-0061-2
Ashing-Giwa, K.T., Padilla, G.V., Bohórquez, D.E., Tejero, J.S., & Garcia, M. (2006). Understanding the breast cancer experience of Latina women. Journal of Psychosocial Oncology, 24(3), 19–52. doi:10.1300/J077v24n03_02
Badger, T.A., Segrin, C., Hepworth, J.T., Pasvogel, A., Weihs, K., & Lopez, A.M. (2013). Telephone-delivered health education and interpersonal counseling improve quality of life for Latinas with breast cancer and their supportive partners, Psycho-Oncology, 22, 1035–1042. doi:10.1002/pon.3101
Beesley, V.L., Price, M.A., Webb, P.M., O’Rourke, P. & Marquart, L. (2013). Changes in supportive care needs after first-line treatment for ovarian cancer: Identifying care priorities and risk factors for future unmet needs. Psycho-Oncology, 22, 1565–1571. doi:10.1002/pon.3169
Buki, L.P., Garcés, D.M., Hinestrosa, M.C., Kogan, L., Carrillo, I.Y., & French, B. (2008). Latina breast cancer survivors’ lived experiences: Diagnosis, treatment, and beyond. Cultural Diversity and Ethnic Minority Psychology, 14, 163–167. doi:10.1037/1099-9809.14.2.163
Carey, M., Lambert, S., Smits, R., Paul, C., Sanson-Fisher, R., & Clinton-McHarg, T. (2012). The unfulfilled promise: A systematic review of interventions to reduce the unmet supportive care needs of cancer patients. Supportive Care in Cancer, 20, 207–219. doi:10.1007/s00520-011-1327-1
Castro, F.G., Barrera, M., Jr., & Martinez, C.R., Jr. (2004). The cultural adaptation of prevention interventions: Resolving tensions between fidelity and fit. Prevention Science, 5, 41–45. doi:10.1023/B:PREV.0000013980.12412.cd
Changrani, J., Leiberman, M., Golant, M., Rios, P., Damman, J., & Gany, F. (2008). Online cancer support groups: Experiences with underserved immigrant Latinas. Primary Psychiatry, 15(10), 55–62.
Dwight-Johnson, M., Ell, K., & Lee, P.J. (2005). Can collaborative care address the needs of low-income Latinas with comorbid depression and cancer? Results from a randomized pilot study. Psychosomatics, 46, 224–232. doi:10.1176/appi.psy.46.3.224
Ell, K., Xie, B., Kapetanovic, S., Quinn, D.I., Lee, P.J., Wells, A., & Chou, C.P. (2011). One-year follow-up of collaborative depression care for low-income, predominantly Hispanic patients with cancer. Psychiatric Services, 62, 162–170. doi:10.1176/ps.62.2.pss6202_0162
Eversley, R., Estrin, D., Dibble, S., Wardlaw, L., Pedrosa, M., & Favila-Penny, W. (2005). Post-treatment symptoms among ethnic minority breast cancer survivors. Oncology Nursing Forum, 32, 250–256. doi:10.1188/05.ONF.250-256
Feuerstein, M. (2007). Defining cancer survivorship. Journal of Cancer Survivorship, 1, 5–7. doi:10.1007/s11764-006-0002-x
Freund, K.M., Battaglia, T.A., Calhoun, E., Darnell, J.S., Dudley, D.J., Fiscella, K., . . . Pasket, E.D. (2014). Impact of patient navigation on timely cancer care: The Patient Navigation Research Program. Journal of the National Cancer Institute, 106(6), 1–9. doi:10.1093/jnci/dju115
Ganz, P.A. (2006). Monitoring the physical health of cancer survivors: A survivorship-focused medical history. Journal of Clinical Oncology, 24, 5105–5111. doi:10.1200/JCO.2006.06.0541
Ganz, P.A. (2009). Survivorship: Adult cancer survivors. Primary Care, 36, 721–741. doi:10.1016/j.pop.2009.08.001
Greenlee, H.A., Crew, K.D., Mata, J.M. McKinley, P.S., Rundle, A.G., Zhang, W., . . . Hershman, D.L. (2013). A pilot randomized controlled trial of a commercial diet and exercise weight loss program in minority breast cancer survivors. Obesity, 21, 65–76. doi:10.1002/oby.20245
Haylock, P.J. (2006). The shifting paradigm of cancer care. Cancer Nursing, 29(2 Suppl.), 16S–19S. doi:10.1097/00002820-200603002-00007
Hershman, D.L., Greenlee, H., Awad, D., Kalinsky, K., Maurer, M., Kranwinkel, G., . . . Crew, K.D. (2013). Randomized controlled trial of a clinic-based survivorship intervention following adjuvant therapy in breast cancer survivors. Breast Cancer Research and Treatment, 138, 795–806. doi:10.1007/s10549-013-2486-1
Hewitt, M., Greenfield, S., & Stovall, E. (2005). From cancer patient to cancer survivor: Lost in transition. Washington, DC: National Academies Press.
Hughes, D.C., Leung, P., & Naus, M.J. (2008). Using single-system analyses to assess the effectiveness of an exercise intervention on quality of life for Hispanic breast cancer survivors: A pilot study. Social Work in Health Care, 47, 73–91.
Juarez, G., Hurria, A., Uman, G., & Ferrell, B. (2013). Nueva Luz: Impact of a bilingual education intervention on the quality of life of Latina breast cancer survivors. Oncology Nursing Forum, 40, E50–E60. doi:10.1188/13.ONF.E50-E60
Juarez, G., Mayorga, L., Hurria, A., & Ferrell, B. (2013). Survivorship education for Latina breast cancer survivors: Empowering survivors through education. Psicooncologia, 10, 57–68.
Kingsley, C., & Bandolin, S. (2010). Cultural and socioeconomic factors affecting cancer screening, early detection and care in the Latino population. Retrieved from http://ethnomed.org/clinical/cancer/cultural-and-socioeconomic-factors-…
Lopez-Class, M., Perret-Gentil, M., Kreling, B., Caicedo, L., Mandelblatt, J., & Graves, K.D. (2011). Quality of life among immigrant Latina breast cancer survivors: Realities of culture and enhancing cancer care. Journal of Cancer Education, 26, 724–733.
Marshall, C.A., Badger, T.A., Curran, M.A., Koerner, S.S., Larkey, L.K., Weihs, K.L., . . . García, F.A. (2013). Un Abrazo Para La Familia: Providing low-income Hispanics with education and skills in coping with breast cancer and caregiving. Psycho-Oncology, 22, 470–474.
Martinez, D., Aguado Loi, C.X., Martinez, M.M., Flores, A.E., & Meade, C.D. (2008). Development of a cancer camp for adult Spanish-speaking survivors: Lessons learned from Camp Alegria. Journal of Cancer Education, 23, 4–9. doi:10.1080/08858190701818234
McNulty, J.A., & Nail, L. (2015). Cancer survivorship in rural and urban adults: A descriptive and mixed methods study. Journal of Rural Health, 31, 282–291. doi:10.1111/jrh.12106
Moadel, A.B., Morgan, C., & Dutcher, J. (2007). Psychosocial needs assessment among an underserved, ethnically diverse cancer patient population. Cancer, 109(2 Suppl.), 446–454. doi:10.1002/cncr.22357
Moadel, A.B., Shah, C., Wylie-Rosett, J., Harris, M.S., Patel, S.R., Hall, C.B., & Sparano, J.A. (2007). Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: Effects on quality of life. Journal of Clinical Oncology, 25, 4387–4395. doi:10.1200/JCO.2006.06.6027
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D.G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151, 264–269. doi:10.7326/0003-4819-151-4-200908180-00135
Nápoles, A.M., Ortíz, C., O’Brien, H., Sereno, A.B., & Kaplan, C.P. (2011). Coping resources and self-rated health among Latina breast cancer survivors. Oncology Nursing Forum, 38, 523–531. doi:10.1188/11.ONF.523-531
Nápoles-Springer, A.M., Ortíz, C., O’Brien, H., Díaz-Méndez, M., & Pérez-Stable, E.J. (2007). Use of cancer support groups among Latina breast cancer survivors. Journal of Cancer Survivorship, 1, 193–204. doi:10.1007/s11764-007-0029-7
Owens, B., Jackson, M., & Berndt, A. (2009). Pilot study of a structured aerobic exercise program for Hispanic women during treatment for early-stage breast cancer. Medsurg Nursing, 18, 23–29.
Penedo, F.J., Traeger, L, Dahn, J., Molton, I., Gonzalez, J.S., Schneiderman, N., & Antoni, M.H. (2007). Cognitive behavioral stress management intervention improves quality of life in Spanish monolingual Hispanic men treated for localized prostate cancer: Results of randomized controlled trial. International Journal of Behavioral Medicine, 14, 164–172. doi:10.1007/BF03000188
Perez, D., Ang, A., & Vega, W.A. (2009). Effects of health insurance on perceived quality of care among Latinos in the United States. Journal of General Internal Medicine, 24(Suppl. 3), 555–560.
Rodríquez, M.A., Bustamante, A.V., & Ang, A. (2009). Perceived quality of care, receipt of preventive care, and usual source of health care among undocumented and other Latinos. Journal of General Internal Medicine, 24(Suppl. 3), 508–513.
Sammarco, A., & Konecny, L.M. (2010). Quality of life, social support, and uncertainty among Latina and Caucasian breast cancer survivors: A comparative study. Oncology Nursing Forum, 37, 93–99. doi:10.1188/10.ONF.93-99
Sanson-Fisher, R., Girgis, A., Boyes, A., Bonevski, B., Burton, L., & Cook, P. (2000). The unmet supportive care needs of patients with cancer. Supportive Care Review Group. Cancer, 88, 226–237. doi:10.1002/(SICI)1097-0142(20000101)88:1<226::AID-CNCR30>3.0.CO;2-P
Schmid-Büchi, S., Halfens, R.J., Müller, M., Dassen, T., & van den Borne, B. (2013). Factors associated with supportive care needs of patients under treatment for breast cancer. European Journal of Oncology Nursing, 17, 22–29. doi:10.1016/j.ejon.2012.02.003
Wolin, K.Y., & Colditz, G. (2011). Design and conduct of intervention-based research among cancer survivors. Cancer Epidemiology, Biomarkers and Prevention, 20, 2078–2084. doi:10.1158/1055-9965.EPI-11-0605
Wu, X.C., Lund, M.J., Kimmick, G.G., Richardson, L.C., Sabatino, S.A., Chen, V.W., . . . Lipscomb, J. (2012). Influence of race, insurance, socioeconomic status, and hospital type on receipt of guideline concordant adjuvant systemic therapy for locoregional breast cancers. Journal of Clinical Oncology, 30, 142–150. doi:10.1200/JCO.2011.36.8399
Yabroff, K.R., Lawrence, W.F., Clauser, S., Davis, W.W., & Brown, M.L. (2004). Burden of illness in cancer survivors: Findings from a population-based national sample. Journal of the National Cancer Institute, 96, 1322–1330. doi:10.1093/jnci/djh255
Yanez, B., Thompson, E.H., & Stanton, A.L. (2011). Quality of life among Latina breast cancer patients: A systematic review of the literature. Journal of Cancer Survivorship, 5, 191–207.
About the Author(s)
At the time of writing McNulty and W. Kim were both assistant professors in the College of Nursing and Health Innovation at Arizona State University; Thurston is a program director at Cancer Support Community Arizona; and J. Kim is a research assistant and Larkey is a professor, both in the College of Nursing and Health Innovation at Arizona State University, all in Phoenix. This research was funded by a 2015 ONS Foundation Research Career Development award (McNulty) supported by Genentech, and the Arizona State University Francis Fellowship in Biobehavioral Oncology. McNulty, W. Kim, Thurston, J. Kim, and Larkey contributed to the conceptualization and design. McNulty, W. Kim, and J. Kim completed the data collection. McNulty and W. Kim contributed to the analysis. McNulty, W. Kim, Thurston, and Larkey contributed to the manuscript preparation. W. Kim can be reached at sunny.kim@asu.edu, with copy to editor at ONFEditor@ons.org. Submitted October 2015. Accepted for publication December 16, 2015.

