Addressing Childhood Cancer in Low-Resource Countries: Current Challenges, Strategies, and Recommendations
Children and adolescents represent a small, but critically important, number of patients with cancer worldwide (14.1 million newly diagnosed adults versus 160,000 children annually). The life years saved when a child is cured of cancer are about 71 compared to 15 years for an adult in most high-income countries (HICs). In HICs, about 80% of children survive cancer. Unfortunately, in low- and middle-income countries (LMICs), the survival rates are generally 50% or less. In these resource-limited settings, only 15%–37% of children and adolescents have access to cancer treatment, and most are diagnosed with advanced-stage disease, making cure impossible.
Jump to a section
Children and adolescents represent a small, but critically important, number of patients with cancer worldwide (14.1 million newly diagnosed adults versus 160,000 children annually) (Ferlay et al., 2012; Rodriguez-Galindo et al., 2015). The life years saved when a child is cured of cancer are about 71 compared to 15 years for an adult in most high-income countries (HICs) (St. Baldrick’s Foundation, 2016). In HICs, about 80% of children survive cancer. Unfortunately, in low- and middle-income countries (LMICs), the survival rates are generally 50% or less (Erdmann et al., 2014; Israels, Challinor, Howard, & Arora, 2015). In these resource-limited settings, only 15%–37% of children and adolescents have access to cancer treatment (Ribeiro et al., 2008), and most are diagnosed with advanced-stage disease, making cure impossible (Awadelkarim, Mariani-Costantini, & Elwali, 2012; Sullivan et al., 2014). The World Health Organization, the United Nations, and other international groups have called for cancer treatment as a human right and have begun to direct attention to cancer as a growing noncommunicable disease that threatens public health across LMICs (NCD Alliance, 2016). This article outlines challenges and offers strategies and solutions related to childhood cancers in LMICs. Examples of relevant global initiatives are summarized in Figure 1.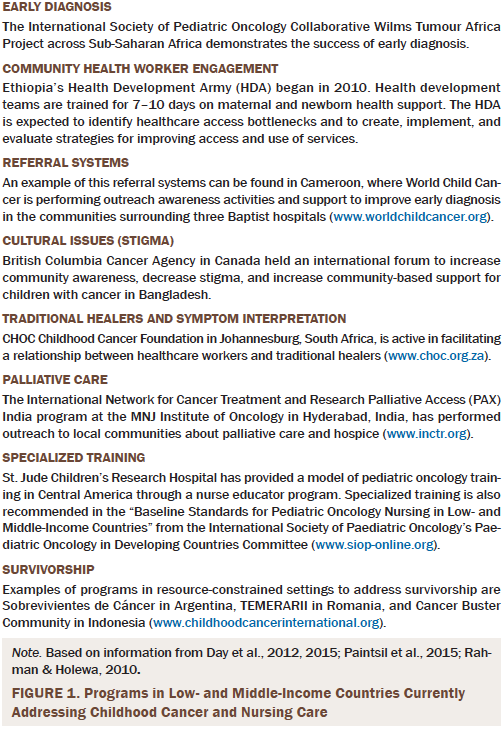
Strengthen Community Health Worker Engagement and Increase Early Diagnosis
Early diagnosis is critical to ensure that children and adolescents with cancer have the chance to be cured; in fact, successful treatment of several childhood cancers in LMICs has demonstrated this to be true (Howard et al., 2004; Pan American Health Organization, 2014). Two examples include Burkitt’s lymphoma and Wilms tumor, which can be cured when diagnosed early and treated with adapted treatment protocols that consider local comorbidities and resource realities of LMICs (Israels, Ribeiro, & Molyneux, 2010).
Community health workers (CHWs) in most LMICs represent the frontlines of the health delivery system, and their connections to the community can be leveraged to improve prompt diagnosis and referral. However, CHWs often receive short-term (a few days, weeks, or months) training that does not include childhood cancer signs and symptoms (Maternal and Child Health Integrated Program, 2013). A child with an enlarged belly in LMICs is more likely to have parasites than a Wilms tumor. As frontline care providers, CHWs must be given the tools to identify children and adolescents with possible cancer. One barrier is that many CHWs practice in rural areas and, therefore, are hard to bring together for training. Given the large number of adults with advanced cancer in LMICs, CHW training for early signs and symptoms of cancer could combine adult and childhood cancer awareness to ensure that CHWs are vigilant and knowledgeable across the lifespan.
Creating a strong CHW national network for childhood cancer in LMICs will ensure that children with cancer are recognized early, receive appropriate referrals and treatment, and are supported during home-based care or following completion of treatment to monitor for long-term side effects. Improved referral systems and financial support for families during a child’s treatment are essential to avoid abandonment of care and loss to follow-up once a child is diagnosed. Once a CHW suspects that a child or adolescent has cancer, they need a protocol for how to proceed. CHW must know who to call and where treatment is available, and they must have clear instruction on how to refer patients with suspected cancer for further diagnostic evaluation. A robust, efficient, and effective referral system is essential because some childhood cancers, such as Burkitt’s lymphoma, grow so fast that a child can die within several days (Texas Children’s Hospital, 2016). Poor transportation systems and long distances, as well as poverty, can lead to delayed arrival in a local clinic, district hospital, or tertiary care facility; these realities must also be addressed in referral protocols. Governmental and nongovernmental organization support for transportation fees and food for families traveling to more advanced care facilities will be essential to ensure that children and adolescents arrive in time for appropriate follow-up diagnostics and further care.
Address Cultural Considerations
In many LMICs, cancer can be a highly stigmatizing condition (Denburg, Wilson, Gupta, Kutluk, & Torode, 2015), causing parents and the child or adolescent to ignore or hide symptoms if they suspect cancer. The issue of prognosis disclosure can become further complicated if families do not want their child to know the details of their disease, and nurses may feel caught in the middle. Educating CHWs and raising local community awareness about cancer can contribute to decreasing stigma and improving early diagnosis. In addition, this will lead to improved support for families of children and adolescents who return to their communities on outpatient therapy or after completing treatment. Decreasing the stigma of cancer is also important for families whose child or adolescent has returned home to die or who has died; these families need enhanced community support during times of grief and bereavement.
In LMICs, the cultural norm is for families to first seek traditional medicine as treatment for symptoms of cancer (Magrath et al., 2013). Unfortunately, this action can delay a child or adolescent’s treatment for cancer and decrease the chance of survival. Fear of losing clientele and their reputation may cause traditional healers to hesitate in referring patients before trying to cure (B. Ramaru, personal communication, February 22, 2016; CHOC Childhood Cancer Foundation South Africa, 2014).
Improved communication and collaboration between tertiary healthcare providers and traditional healers will help to ensure that children with cancer in LMICs are diagnosed quickly and referred promptly for treatment. Therefore, physicians, nurses, and other members of LMIC cancer treatment facilities need to work closely with CHWs to collaborate with traditional healers and foster open lines of communication. Although many traditional healers do not claim to heal patients with cancer, they may not be familiar with childhood cancer signs and symptoms and may initiate treatments that delay arrival at specialized cancer centers. Open communication allows traditional healers to complement their practice with referrals of children and adolescents suspected of having cancer to biomedical personnel for additional evaluation.
Expand Oncology Training
CHWs, local healthcare professionals in district hospitals, and nurses in all LMIC settings who care for children and adolescents with cancer must receive specialized training to provide comprehensive care during the entire cancer continuum. The cancer continuum for childhood cancer begins with early diagnosis, is followed by appropriate referral and treatment, and ends with either death and bereavement or cure and survivorship.
National government officials in the ministries of health and education have been called upon to dedicate funding for nursing specialization in oncology and to build locally sustainable programs in advanced oncology nursing education to ensure that the increasing cancer burden in LMICs can be addressed (Challinor et al., 2016; Galassi & Challinor, 2015). In many countries, even many upper middle–income countries, nurse oncology training remains focused on adults; however, nurse specialization training must include pediatric oncology content. Pediatric oncology nurse training in LMICs must include content in palliative care and survivorship monitoring and will require support from local ministries of health and education, as well as external support from international partners, until local capacity building and sustainability is achieved.
Palliative care is a critical component of cancer care in LMICs. Children and adolescents who are diagnosed with cancer deserve to have appropriate supportive care, which includes adequate pain control, the cornerstone of palliative care. This can be challenging in LMICs where opioids may not be legal or available (International Network for Cancer Treatment and Research, 2016a) or where healthcare providers have little experience prescribing and administering opioids, which can lead to undertreatment of pain. Programs, such as the International Network for Cancer Treatment and Research’s (2016b) Palliative Access (PAX) Program, have made great strides in improving and extending palliative care in LMICs. However, much work still needs to be done, including training nurses to provide palliative nursing care. Nurses working with CHWs to provide home-based palliative care significantly improve the quality of life for children and adolescents with terminal cancer (Tamannai et al., 2015); this type of collaborative care model can also help prepare and support a family and community during the grieving and bereavement process after the patient has died.
Survivors of childhood cancer in LMICs often have little follow-up care. This is problematic because patients can have lifelong sequelae from cancer treatment, including cardiac, neurocognitive, endocrine, and pulmonary issues. Therefore, childhood cancer survivors must be monitored regularly to avoid serious health problems in adulthood. One example of exemplary follow-up is in South Africa, where childhood cancer survivors are followed until they are aged 21 years or until they stop coming to the clinic (J. Geel, personal communication, March 22, 2016).
Conclusion
The growing burden of childhood cancer is a global noncommunicable disease problem that cannot be ignored. Early diagnosis of childhood cancers is key to survival. In LMICs where healthcare systems are fragile or difficult to access because of limited facilities, geography, and a lack of health professionals and material resources, early diagnosis is even more critical for successful childhood cancer care. Key strategies that can help improve care for children with cancer in LMICs include strengthening the role of the CHW, addressing cultural considerations (e.g., working collaboratively with traditional healers), and expanding pediatric oncology training, particularly in the areas of palliative care and survivorship.
Nurses must be an integral component of all cancer control plans, and their scope of practice must include comprehensive specialized oncology nursing care. Children and adolescents with cancer in LMICs deserve access to appropriate care, and the inclusion of childhood cancer in national cancer control plans is essential. Children are the future of LMICs; those who survive cancer and receive sufficient support can go on to make valuable contributions to the development of their society.
References
Awadelkarim, K.D., Mariani-Costantini, R., & Elwali, N.E. (2012). Cancer in the Sudan: An overview of the current status of knowledge on tumor patterns and risk factors. Science of the Total Environment, 423, 214–228. doi:10.1016/j.scitotenv.2010.09.010
Challinor, J.M., Galassi, A.L., Al-Ruzzieh, M.A., Bigirimana, J.B., Buswell, L., So, W.K., . . . Williams, M. (2016). Nursing’s potential to address the growing cancer burden in low- and middle-income countries. Journal of Global Oncology. Advance online publication. doi:10.1200/jgo.2015.001974
CHOC Childhood Cancer Foundation South Africa. (2014). CHOC Annual Review 2013–2014. Johannesburg, South Africa: Author.
Day, S., Challinor, J., Hollis, R., Abramovitz, L., & Hanaratri, Y. (2015). Paediatric oncology nursing care in low- and middle-income countries: A need for baseline standards. Cancer Control, 2015, 111–116.
Day, S., Garcia, J., Antillon, F., Wilimas, J.A., McKeon, L.M., Carty, R.M., . . . Howard, S.C. (2012). A sustainable model for pediatric oncology nursing education in low‐income countries. Pediatric Blood and Cancer, 58, 163–166. doi:10.1002/pbc.24007
Denburg, A., Wilson, M.G., Gupta, S., Kutluk, T., & Torode, J. (2015). Evidence brief: Advancing the development of national childhood cancer-care strategies in Latin America. Retrieved from https://www.mcmasterhealthforum.org/docs/default-source/Product-Documen…
Erdmann, F., Kielkowski, D., Schonfeld, S.J., Kellett, P., Stanulla, M., Dickens, C., . . . Schüz, J. (2014). Childhood cancer incidence patterns by race, sex and age for 2000–2006: A report from the South African National Cancer Registry. International Journal of Cancer, 136, 2628–2639. doi:10.1002/ijc.29308
Ferlay, J., Soerjomataram, I., Ervik, M., Dikshit, R., Eser, S., Mathers, C., . . . Bray, F. (2012). GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. Lyon, France: International Agency for Research on Cancer.
Galassi, A., & Challinor, J. (2015). Strengthening the oncology nurse workforce in low-income and middle-income countries. Lancet. Oncology, 16, 887–888. doi:10.1016/S1470-2045(15)00144-8
Howard, S.C., Pedrosa, M., Lins, M., Pedrosa, A., Pui, C.H., Ribeiro, R.C., & Pedrosa, F. (2004). Establishment of a pediatric oncology program and outcomes of childhood acute lymphoblastic leukemia in a resource-poor area. JAMA, 291, 2471–2475. doi:10.1001/jama.291.20.2471
International Network for Cancer Treatment and Research. (2016a). Cancer in developing countries. Retrieved from http://www.inctr.org/about-inctr/cancer-in-developing-countries
International Network for Cancer Treatment and Research. (2016b). Palliative access. Retrieved from http://www.inctr.org/programs/palliative-care-pax
Israels, T., Challinor, J., Howard, S., & Arora, R.H. (2015). Treating children with cancer worldwide—Challenges and interventions. Pediatrics, 136, 607–610. doi:10.1542/peds.2015-0300
Israels, T., Ribeiro, R.C., & Molyneux, E.M. (2010). Strategies to improve care for children with cancer in sub-Saharan Africa. European Journal of Cancer, 46, 1960–1966. doi:10.1016/j.ejca.2010.03.027
Magrath, I., Steliarova-Foucher, E., Epelman, S., Ribeiro, R.C., Harif, M., Li, C.-K., . . . Howard, S.C. (2013). Pediatric cancer in low-income and middle-income countries. Lancet Oncology, 14, E104–E116. doi:10.1016/S1470-2045(13)70008-1
Maternal and Child Health Integrated Program. (2013). Developing and strengthening community health worker programs at scale: A reference guide for program managers and policy makers. Retrieved from http://www.mchip.net/sites/default/files/mchipfiles/CHW_ReferenceGuide_…
NCD Alliance. (2016). Cancer. Retrieved from http://www.ncdalliance.org/node/40
Paintsil, V., David, H., Kambugu, J., Renner, L., Kouya, F., Eden, T., . . . Israels, T. (2015). The Collaborative Wilms Tumour Africa Project: Baseline evaluation of Wilms tumour treatment and outcome in eight institutes in Sub-Saharan Africa. European Journal of Cancer, 51, 84–91. doi:10.1016/j.ejca.2014.10.030
Pan American Health Organization. (2014). Early diagnosis of childhood cancer. Washington, DC: Author.
Rahman, S., & Holewa, H. (2010). Addressing childhood cancer in resource limited countries: The need for an international collaborative effort. Austral-Asian Journal of Cancer, 9. Retrieved from http://www.australasiancancer.org/journal-article-view/addressing-child…
Ribeiro, R.C., Steliarova-Foucher, E., Magrath, I., Lemerle, J., Eden, T., Forget, C., Mortara, I., . . . Miklavec, T. (2008). Baseline status of paediatric oncology care in ten low-income or mid-income countries receiving My Child Matters support: A descriptive study. Lancet. Oncology, 9, 721–729. doi:10.1016/S1470-2045(08)70194-3
Rodriguez-Galindo, C., Friedrich, P., Alcasabas, P., Antillon, F., Banavali, S., Castillo, L., . . . Gross, T. (2015). Toward the cure of all children with cancer through collaborative efforts: Pediatric oncology as a global challenge. Journal of Clinical Oncology, 33, 3065–3073. doi:10.1200/JCO.2014.60.6376
St. Baldrick’s Foundation. (2016). Filling the funding gap. Retrieved from http://www.stbaldricks.org/filling-the-funding-gap
Sullivan, R., Badwe, R.A., Rath, G.K., Pramesh, C.S., Shanta, V., Digumarti, R., . . . Purushotham, A.D. (2014). Cancer research in India: National priorities, global results. Lancet. Oncology, 15, e213–e222. doi:10.1016/S1470-2045(14)70109-3
Tamannai, M., Kaah, J., Mbah, G., Ndimba, J., D’Souza, C., Wharin, P., & Hesseling, P.B. (2015). An evaluation of a palliative care outreach programme for children with Burkitt lymphoma in rural Cameroon. International Journal of Palliative Nursing, 21, 331–337. doi:10.12968/ijpn.2015.21.7.331
Texas Children’s Hospital. (2016). Health conditions: Burkitt’s lymphoma. Retrieved from http://www.texaschildrens.org/health/burkitts-lymphoma
About the Author(s)
Afungchwi is a pediatric oncology nurse at Banso Baptist Hospital in Kumbo, Cameroon; Ramaru is an operational case manager specialist at AfroCentric Health in Roodepoort, South Africa; and Challinor is an associate adjunct professor in the School of Nursing at the University of California, San Francisco. No financial relationships to disclose. Challinor can be reached at jmchallinor@gmail.com, with copy to editor at ONFEditor@ons.org.

