Oncology Nurses’ Attitudes and Engagement in Nursing Research
Objectives: To assess nurses’ attitudes and perceptions about research.
Sample & Setting: 623 RNs at a National Cancer Institute–designated comprehensive cancer center in the midwestern United States.
Methods & Variables: This study used a cross-sectional, descriptive survey to describe nurses’ attitudes toward nursing research, perceptions of the research environment, and research involvement.
Results: Nurses’ attitudes toward research were generally more positive than negative. Results suggested that the biggest obstacle to nurses participating in research is time.
Implications for Nursing: Understanding oncology nurses’ attitudes toward research and the research environment is vital for the future of patient outcomes research. Results from this study inform strategic goals for increasing nursing research capacity, including the use of research teams and access to research mentors and resources, as well as nursing research fellowship programs.
Jump to a section
Nursing research is important because it yields clinically relevant evidence to improve the health of individuals, families, and communities. This is particularly true in the field of oncology, where nursing research can affect patient outcomes, from prevention to survivorship to the end of life. However, barriers to nurses’ participation in research are found across all settings. To assess nurses’ attitudes about and engagement in research at the Ohio State University Comprehensive Cancer Center–Arthur G. James Cancer Hospital and Richard J. Solove Research Institute in Columbus, a freestanding academic National Cancer Institute (NCI)–designated comprehensive cancer center (CCC), the institution’s Nursing Innovation and Research Council chose to assess nurses’ attitudes and perceptions concerning research by replicating studies by Rizzuto, Bostrom, Suter, and Chenitz (1994) and Smirnoff, Ramirez, Kooplimae, Gibney, and McEvoy (2007).
Background
Nurses’ involvement in research is crucial, particularly as patient care transitions from interventions based on precedent to those based on the best evidence. Well-developed research and evidence-based practice (EBP) go hand in hand in improving patient outcomes and healthcare delivery. In the 21st century, regulating bodies require that EBP be integrated into nursing curricula (Melnyk & Fineout-Overholt, 2018). Although research creates evidence, EBP is the mechanism that puts evidence into practice. EBP is becoming the new standard of care, and more research is needed to create an ample supply of quality evidence to support this new culture (Melnyk & Fineout-Overholt, 2018).
Studies consistently show that nurses have positive attitudes toward research and agree that they should have the opportunity to be involved in such endeavors; however, clinical nurses face numerous barriers to research participation (Berthelsen & Hølge-Hazelton, 2015; Roxburgh, 2006). Examples of these barriers from the literature (Aljezawi et al., 2019; Berthelsen & Hølge-Hazelton, 2015; Silka, Stombaugh, Horton, & Daniels, 2012) include the following:
• Limited time away from direct patient care for research activities
• Minimal education in nursing programs concerning how nurses can be involved in research activities
• Little understanding of the importance of nurses’ roles in research activities and how to translate research findings to the bedside
A cross-sectional survey of 450 pediatric nurses by Hagan and Walden (2017) showed that availability of resources, personal relevance, and lack of time were dominant barriers to nursing research, as well as that the perceived severity of those varied by each participant’s educational and certification levels and his or her previous research experiences. The barriers that clinical nurses report are quite different than those reported by nurses in academic roles as a result of their job expectations and organizational structures (Segrott, McIvor, & Green, 2006).
Lacking time to formulate, carry out, and disseminate research are among the top barriers across multiple studies (Aljezawi et al., 2019; Berthelsen & Hølge-Hazelton, 2015; Silka et al., 2012). Nurses’ jobs often require that 100% of their time be spent performing direct patient care, with limited or no paid time away from clinical responsibilities. Nurses’ involvement in research may also be hindered by insufficient institutional support and lack of knowledge about the research process and its potential impact on patient outcomes. Institutional support for nursing research may vary widely by size, academic affiliation, and Magnet® status.
Common perceptions among nurses are that research can be done only by those with advanced degrees, that the research process is too complicated and cumbersome for nurses to be involved, and that applying new knowledge into clinical practice is outside their scope of practice or influence (Berthelsen & Hølge-Hazelton, 2015; Silka et al., 2012). In a cross-sectional, descriptive study of orthopedic hospital-based nurses, Berthelsen and Hølge-Hazelton (2015) found that although nurses’ interest in nursing research and their motivation to improve their research skills were high, they possessed low levels of perceived theoretical knowledge and practical research competence. McCleary and Brown (2003) determined, in a study of 175 nurses working in a pediatric hospital, that higher levels of education were associated with positive attitudes about research and research utilization. Completing courses on research design or research utilization was associated with positive attitudes toward research. Evidence suggests that increasing nurses’ knowledge about research may be one method to influence nurses’ attitudes about and participation in clinical research.
Two studies that explored nursing attitudes and perceptions of nursing research were used as templates for the current study: Rizzuto et al. (1994) and Smirnoff et al. (2007). Rizzuto et al. (1994) surveyed 1,217 nurses employed at nine healthcare agencies concerning their research attitudes, work environment, and research involvement. Their results indicated that nurses value nursing research and want more protected time that is dedicated to research-related activities. Prior research instruction, awareness of support for research, and positive attitudes toward research were predictive of participation in research activities (Rizzuto et al., 1994).
Smirnoff et al. (2007) replicated the study conducted by Rizzuto et al. (1994) in a large research-intensive academic medical center in New York City. Their results suggested that nurses’ (N = 470) positive attitudes toward research did not appear to translate into actual involvement in research activities. In addition, positive attitudes and perceived institutional support were not enough to increase involvement in nursing research (Smirnoff et al., 2007).
Critical analysis of the literature revealed that despite studies describing nurses’ attitudes in a variety of clinical settings, no study has examined nurses’ attitudes toward research, perception of the research environment, or research participation in a CCC. NCI-designated CCCs are recognized for their scientific leadership, resources, and research to ultimately improve patient outcomes. Results from this study can guide efforts to minimize barriers to nurses’ research participation and strengthen the nursing research culture and infrastructure at the NCI-designated CCC in the current study. Comparison of similar studies spanning two decades also informs nursing and healthcare leaders about progress made in nurses’ attitudes and involvement in clinical research.
The main study aims were to describe nurses’ attitudes toward nursing research, their perceptions of the research environment, and their research experience at a large academic NCI-designated CCC that focuses on education, research, and patient care. Results of this study inform efforts to provide a supportive infrastructure for hospital-based nursing research.
Methods
All RNs employed at the institution (N = 1,528) were invited to participate in the research study, including nurses in any role (e.g., oncology, surgical, critical care) and those with advanced degrees. Patient care associates, unit clerks, administrative assistants, and physician assistants were excluded from the study. Similar to the Rizzuto et al. (1994) and Smirnoff et al. (2007) studies, because the current authors wanted to fully understand responses from all RNs within the organization, all RNs were invited to participate. Therefore, a sample size estimation was not conducted prior to beginning the study.
Design and Data Collection Procedures
This study was a cross-sectional, descriptive, quantitative survey of nurses at a 316-bed cancer hospital and supportive ambulatory clinics. After receiving hospital administration and institutional review board (IRB) approval, all nurses at the study organization received an email with a link to participate in an online survey. The study was advertised using flyers posted in individual departments and via the hospital intranet, and potential participants received weekly email reminders. After gaining informed consent from interested participants, data were collected during a one-month period. The survey, which contained four online measures, took less than 10 minutes to complete. Participation was voluntary, and participant identifiers (email address) were stripped from the data set to deidentify survey respondents. Once the participants had completed the survey, they had the option to voluntarily include an email address; doing so would enter them into a drawing for a new or renewal membership to their professional organization. Data were collected using Qualtrics online software and analyzed using SAS, version 9.4.
Measures
Participants were asked to complete four online measures. The first measure was a demographics questionnaire created by the study team, which was followed by the 23-item Nursing Research Attitude Scale, which evaluates attitudes toward nursing research. Respondents indicated their agreement using a five-point Likert-type scale ranging from 1 (most negative attitude) to 5 (most positive attitude). Content validity was established by expert panel (Rizzuto et al., 1994). Construct validity of the Nursing Research Attitude Scale has been demonstrated (Cronbach alpha = 0.92) (Chenitz & Sater, 1987; Young, 1982); the Cronbach alpha of the sample in the current study was 0.92.
The third measure, the 15-item Research Environment Scale, evaluates perceptions about and awareness of existing support for research in the work environment using a four-point Likert-type scale ranging from 1 (most negative awareness) to 4 (most positive awareness) for the present as it is and the future as it should be; alternatively, participants could choose an “I do not know” response. Content validity was established by expert panel (Rizzuto et al., 1994). Construct validity of the Research Environment Scale has been established (Cronbach alpha = 0.88) (Chenitz & Sater, 1987; Young, 1982); the Cronbach alpha of the sample in the current study was 0.95.
The fourth measure was the 12-item Research Involvement Survey, which requires yes or no responses regarding past, present, and future research activities. Content validity of the Research Involvement Survey was demonstrated by expert panel, and construct validity was shown, with Cronbach alpha values for the past, present, and future scales being 0.89, 0.86, and 0.96, respectively (Bostrom & Suter, 1993; Rizzuto et al., 1994). Cronbach alpha values of the sample in the current study for the past, present, and future scales were 0.9, 0.83, and 0.93, respectively.
Data Analysis
Descriptive statistics were used to summarize the demographic data. For measures with Likert-type scales, responses were coded so that a larger score indicated more agreement. For each measure, overall scores were assigned to each respondent. To take advantage of as much collected data as possible, a measure score was assigned if a participant completed at least half of the measure’s items; the current authors assumed that answering at least half of a measure’s items provided an adequate estimate of the nurse’s level of agreement, knowledge, or activity level. In addition, using the responses from as many participants as possible lessened the potential for bias that may be introduced when participants are excluded from analyses because of incomplete data. Each member of the sample (N = 623) had at least one measure score but not necessarily scores on other measures. The number of missing measure scores varied by measure but ranged from 1% to 52%. The larger missing percent (52% comes from the Research Environment Scale Likert-type response options) is somewhat artificially high, because “I do not know” responses were coded as missing data for the analysis. Data were not missing at random. For example, about 6% of the respondents appear to have stopped participating in the study midway through completion of the online session, leaving all remaining items incomplete.
For the Nursing Research Attitude Scale, the overall score was the average of the 23 items. For the Research Environment Scale, each respondent was assigned four overall scores: two related to responses to the Likert-type scales (present and future) and two related to responses to the “I do not know” alternative response (present and future). For the Research Involvement Survey, each respondent was assigned three overall scores: the percent of yes responses to an activity (a) that occurred more than six months ago (past), (b) that occurred now or within the past six months (current), and (c) that is planned for the next year (future).
Relationships between demographic variables and overall scores on the Nursing Research Attitude Scale were assessed. Also examined were relationships between demographic variables and the “present as it is” perceptions of the Research Environment Scale. Independent sample t tests were used for education level (at most, bachelor’s degree; at least, master’s degree); completion of a research course (yes or no); and job title (nondirect patient care [nurse manager, clinical nurse specialist, nurse educator, administrator, leader, nursing informatics] versus direct patient care [staff nurse, nurse practitioner, care coordinator]). For years employed at the hospital, years as a nurse, and age, the sample was divided based on terciles, and analysis of variance (ANOVA) was used to assess whether there were mean survey score differences among the three groups. Statistical testing was limited to overall measure scores, and parametric tests (t tests and ANOVAs) were assumed to be adequate given the sample size and the characteristics of the overall score distributions.
Results
Of the 1,528 participants offered the survey, 623 nurses answered at least half of the items from at least one of the measures (41% response rate). Table 1 summarizes respondent characteristics. The participants’ (N = 580) mean age was 38.9 years, with a median of 37 years and a range of 21–66 years. About 93% of participants were women. In addition, about 90% of respondents identified as White, 4% as Black, 2% as Asian, 2% as Hispanic, and the remaining 3% as other. Most of the participants held a bachelor’s degree (70%), and 23% held a master’s degree; others held an associate degree (4%), a nursing diploma (1%), or a doctoral degree (1%). 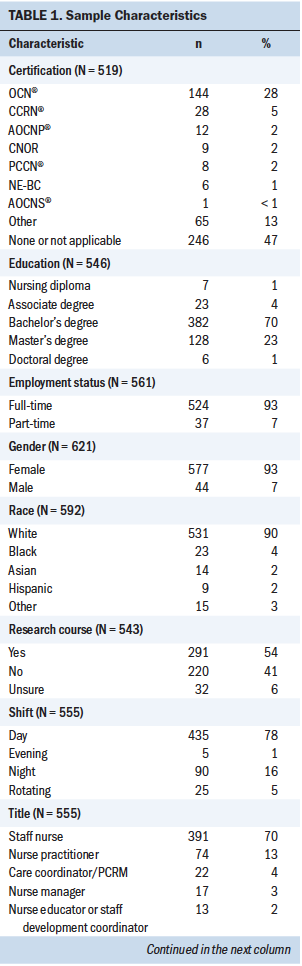
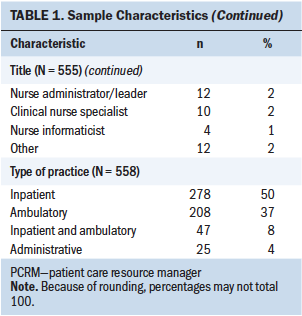
In regard to research education, 291 (54%) respondents reported having taken a research course at some point. Participants (N = 582) had worked as an RN for an average of 13 years, with a median of 9 years and a range of 0–45 years. In addition, participants (N = 566) were employed as a nurse at the hospital for an average of 7.4 years, with a median of 5 years and a range of 0–45 years. Most respondents worked full-time (93%) and on the day shift (78%). The participants acknowledged working in a wide variety of roles, including staff nurse (70%), nurse practitioner (13%), care coordinator/patient care resource manager (4%), nurse manager (3%), nurse educator or staff development coordinator (2%), nurse administrator/leader (2%), clinical nurse specialist (2%), and nurse informaticist (1%); the remaining 2% identified as other. Respondents worked in an inpatient setting (50%), an ambulatory setting (37%), an inpatient and ambulatory setting (8%), or an administrative setting (4%).
Attitudes Toward Nursing Research
Overall scores for the Nursing Research Attitude Scale (N = 296) ranged from 2.55 to 5 on a scale ranging from 1 to 5, with higher scores indicating more positive attitudes. The mean response of 3.8 (SD = 0.5) suggests that nurses’ attitudes toward research were generally more positive than negative. The four items with the highest average scores were as follows:
• “Nursing research findings should guide practice” (mean = 4.44).
• “Nurses should have the opportunity to be involved in nursing research” (mean = 4.35).
• “The use of clinical research findings will improve the quality of nursing care” (mean = 4.3).
• “Nursing interventions should be based on clinical nursing research findings” (mean = 4.29).
In contrast, the two items with the lowest average scores were as follows:
• “I have identified a clinical problem that should be researched” (mean = 2.94).
• “I seldom hear the result of nursing studies” (reverse-scored) (mean = 2.77).
When testing for relationships between attitudes about nursing research and demographic characteristics, evidence demonstrates a more positive attitude from those with at least a master’s degree compared to those with at most a bachelor’s degree (t[542] = 6.67, p < 0.0001). Those employed as nurses for 15 or more years reported a more positive attitude toward nursing research when compared to those employed for 1–14 years (F[2,575] = 5.03, p = 0.007). Similarly, nurses aged older than 44 years reported more positive attitudes about nursing research when compared to those aged younger than 32 years (F[2,573] = 3.87, p = 0.02). Nurses who completed a research course had more positive attitudes compared to those who had not (t[507] = 6.44, p < 0.0001). There was a statistically significant difference between direct care nurses and indirect care nurses (mean = 3.72 versus 4, p < 0.001), suggesting that indirect care nurses have a more positive attitude toward nursing research. There was no evidence of a relationship between attitude toward nursing research and years employed at the hospital.
Research Environment
The results from the Research Environment Scale (N = 296) (see Table 2) indicated that the most negative perceptions were as follows:
• “On-duty time is allowed for analysis of nursing research findings” (mean = 1.97).
• “On-duty time is permitted for proposal writing” (mean = 1.85).
• “Time is allowed during the work day for the writing and publishing of research” (mean = 1.69). 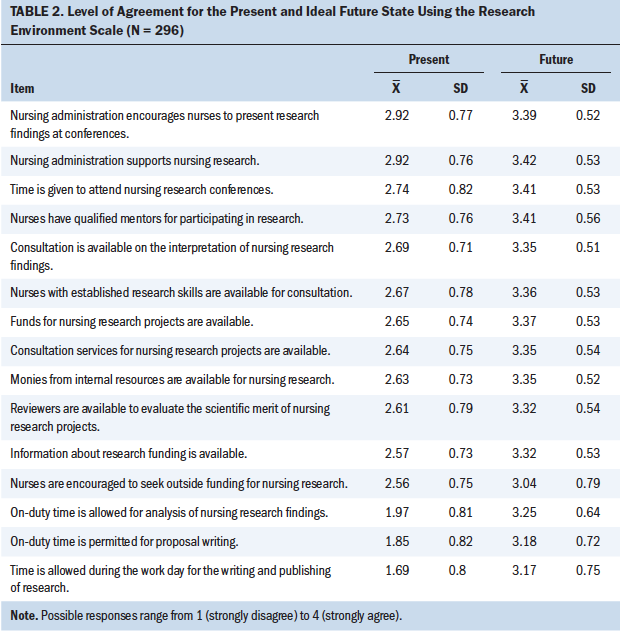
These results suggest that the biggest obstacle to nurses participating in research is time. The Research Environment Scale compared the perception of present organizational support to the ideal future state. The present environment was rated less positive, with a mean score of 2.5 (possible range of 1–4), and the ideal future state was more positive, with a mean score of 3.3, indicating that opportunities exist to improve the perception of the research environment.
A total of 43% of nurses responded “I do not know” when asked to describe the research environment as it currently exists, and 16% responded “I do not know” regarding what they think about the future. Respondents reported being much less aware (that is, more likely to answer “I do not know”) of the following items (see Table 3):
• “Monies from internal resources are available for nursing research.”
• “Consultation is available on the interpretation of nursing research findings.”
• “Reviewers are available to evaluate the scientific merit of nursing research projects.”
• “Consultation services for nursing research projects are available.” 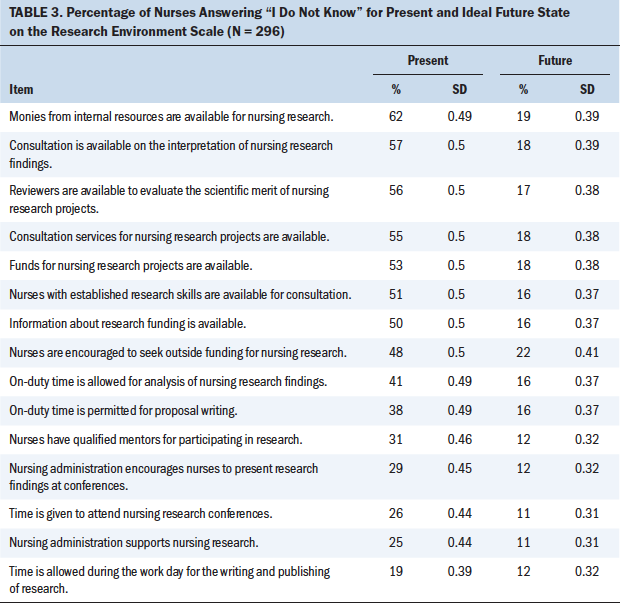
Evidence was found to support more positive attitudes about the research environment among nurses in administrative positions (e.g., leadership, education, informatics, case management) when compared to direct patient care nurses (t[263] = 3.05, p = 0.003). No evidence was found to indicate a relationship between perceptions of the present research environment and education level, years employed at the hospital, years employed as a nurse, age, or completion of a research course.
Research Involvement
The three most frequently reported past research activities on the Research Involvement Scale (N = 546) were as follows:
• “Collaborating with others in a nursing research study” (31%, n = 167)
• “Collecting data for research other than my own” (28%, n = 153)
• “Changing a nursing practice or protocol based on nursing research findings” (22%, n = 118)
Eighteen percent (n = 65) of respondents had participated in research in the past, whereas 8% (n = 41) are currently involved in research endeavors. Fourteen percent (n = 76) of respondents anticipated participation in research in the future. The three least frequently reported areas of current participation in research were as follows:
• “Submitting findings for publication or presentation” (6%, n = 31)
• “Seeking approval for nursing research study from an IRB (human subjects research review committee)” (3%, n = 15)
• “Applying for funding for a nursing research study” (3%, n = 15)
Scores on the Nursing Research Attitude Scale were positively correlated with scores on the Research Environment Scale (r = 0.167, p = 0.004) and the Research Involvement Scale (r = 0.296, p < 0.001). However, there was no relationship found between Research Environment Scale scores and Research Involvement Scale scores.
Discussion
Results from the current study indicate that oncology nurses at the study institution consider research to be important and believe that research should guide practice. These results also identify barriers to research participation related to time, knowledge, and availability of resources. Comparing results from the current study to prior studies and identifying strengths and opportunities to engage more nurses in research is valuable.
Comparison of Studies
Although this study replicates studies by Rizzuto et al. (1994) and Smirnoff et al. (2007), the current sample is unique in that nursing attitudes toward research at a large, freestanding, academic, NCI-designated CCC were explored. A study by Burnett et al. (2001) assessed nurses’ attitudes about clinical trials and factors influencing patient participation in clinical trials at a CCC, finding that nurses generally reported clinical trials as being important to improving standards of care; however, their attitudes about patient participation varied by work setting. Although this work is important for research-intensive CCCs, the current authors’ focus was specifically on nurses’ attitudes about their own participation in the research generation and implementation process.
The two prior studies that were replicated were conducted at nine California healthcare agencies (N = 1,217) (Rizzuto et al., 1994) and at a large metropolitan hospital in New York City (N = 470) (Smirnoff et al., 2007). The current sample has a higher proportion of nurses with bachelor’s (70%) and master’s degrees (23%), which is consistent with the institution’s nursing professional practice model and Magnet status. In the Rizzuto et al. (1994) study, 52% and 15% of participants had bachelor’s and master’s degrees, respectively, whereas in the Smirnoff et al. (2007) study, 60% and 22% of participants had bachelor’s and master’s degrees, respectively.
In addition, the current study sample has a smaller percentage of direct care staff nurses—71% in the current study, compared to 80% in the Rizzuto et al. (1994) study and 79% in the Smirnoff et al. (2007) study—and more advanced practice and administrative nurses. Participants in the current study had been a nurse for an average of 13 years, compared to 12.7 years in the Rizzuto et al. (1994) study and 15.5 years in the Smirnoff et al. (2007) study.
In the current study, 54% of participants had taken a course on research, as compared to 62% in the Rizzuto et al. (1994) study and 54% in the Smirnoff et al. (2007) study. The current sample of nurses also reported less participation in research (past or present) compared with those in the other two studies: 55% in the current study, compared to 62% in the Rizzuto et al. (1994) study and 62% in the Smirnoff et al. (2007) study.
Nurses in the current study reported their past involvement in research consisting of collaborating with others on nursing research, whereas participants in the other two studies reported that they had collected data for others’ research. Participants in all three studies noted that their current research activities entailed collecting data for others’ research; participants in the current study and in the Rizzuto et al. (1994) study reported that their future research activities would be intended to change a practice based on nursing research, whereas those in the Smirnoff et al. (2007) study said they would collaborate with others on a nursing research study.
With regard to nurses’ attitudes toward research, participants in the current study and those in the other two studies strongly agreed with the idea that nurses should have the opportunity to participate in research and that research should guide practice and interventions. It was also noted that engaging in research contributes to the nurse’s personal growth. Participants in all three studies stated that the greatest discrepancy between what is and what should be within the research environment related to having on-duty time to pursue research activities.
Barriers to Research Participation Across Studies
After nearly two decades, findings are similar across the three settings: The most common barrier cited by nurses to conducting research remains time. Staff nurses have the primary responsibility of direct patient care and usually do not have time available in their shifts for planning studies, writing protocols, or leading a research team. Other top barriers to research participation were lack of knowledge and availability of research-related resources. Results from the current study showed that nurses with more advanced degrees and/or promotion to administrative and other nondirect care roles had more positive attitudes about research. Additional education—in the form of either formal research training programs or frequent seminars and workshops—may encourage engagement. Partnering nurses who have research questions with doctorally prepared nurse scientists is another way to leverage team members’ strengths. Respondents in this study were largely unaware of the many resources available to them at the current institution, including internal grants, mentors, consultants, statisticians, graduate research assistants, publishing workshops, and the Center for Clinical and Translational Science, among others.
Similarly, a mixed-methods study of 146 clinical nurses in Singapore by Loke, Laurenson, and Lee (2014) showed that although nurses demonstrated strong enthusiasm for conducting research, this was not adequate for them to actively participate in research. Loke et al. (2014) highlighted the need for protected time, financial support, education, and collaboration for nurses to actively participate in research; they also noted that when institutional support was available, awareness of research opportunities for clinical nurses needed to be strengthened to enable more direct care nurses to conduct research within the context of competing nursing practice demands.
Nurses in all three studies (Rizzuto et al., 1994; Smirnoff et al., 2007; the current study) reported that research should guide nursing practice. In the past decade, there has been growth of EBP in nursing curricula and clinical practice through guidelines, policies, and quality improvement processes. There has also been an exponential increase in the number of Doctor of Nursing Practice–trained nurses, whose expertise involves examining the evidence for clinical problems, incorporating client preferences, and implementing best practices. Despite the need for high-level research evidence to inform EBP, nurses may have become more comfortable with EBP principles than research.
Limitations
Generalizability of the study results is limited because of the large proportion of the sample that is White (90%) and female (93%) with a bachelor’s degree or higher (94%). Study results are, therefore, not generalizable to men or to non-Caucasian participants. The potential of bias was present for participants who provided identifiable information (email address) along with study data; lack of anonymity may have resulted in participants feeling pressured to submit socially desirable answers to items. There may also be a response bias: Nurses with an interest in research may have been more likely to participate in the survey.
Participants noted research experience that involved collecting data for others and collaborating with others; however, based on wording of the measure, it is unclear whether these others are nurses or not. In addition, it is unclear how respondents conceptualized “participation in research”—this could range from taking care of a patient involved in a clinical trial to collecting data for a non-nurse researcher to being the principal investigator on a nursing research study. Respondents also may have varying definitions of nursing research and may conceptualize it as including any research led by nurses or research specific to nursing clinical care.
Implications for Nursing and Research
Care of patients with cancer is in a continual mode of change related to advances in science, technology, and treatment (Cox, Arber, Gallagher, Mackenzie, & Ream, 2017). Nursing practices should adapt in response to this rapidly changing environment of care and should be not only up to date but also rigorously evidence based. To keep pace with the changing landscape of cancer care, addressing barriers to nurses’ participation in research and EBP is paramount.
The Nursing Research and Innovation Shared Governance Council at the study institution has taken initiative and leadership in addressing these barriers in partnership with oncology nursing department leaders. Results of the current study have been used to inform strategic goals, with a focus on enhancing interested oncology nurses’ access to research mentors and resources. To address the barrier of time away from direct patient care to carry out research activities, an oncology nursing research fellowship program that offers protected time off the unit, mentorship from a nurse scientist, and didactic content for nurses who wish to engage in research was proposed. The challenge of time can also be addressed by creating research teams where oncology expertise and work are shared among a group. Nurses who perform research activities outside of working hours are also incentivized through a clinical ladder program. The purpose of the clinical ladder program is to promote professional nursing practice by recognizing and rewarding those experienced RNs who excel in clinical practice, education, and research.
Strategies to address knowledge and participation in research include educational offerings and direct mentorship by an oncology nurse scientist, which can be accomplished with clinical–academic partnerships. Attempts to engage nurses include marketing the institution’s oncology nursing research resources and successes and modeling successful nursing research projects for peers. The hospital and oncology nursing department benefit because nurses’ research activities are used as evidence of nursing excellence for maintaining Magnet status. 
Conclusion
Oncology nurses in the current study agreed that they should have the opportunity to engage in research and that research should guide practice. However, barriers still exist for oncology nurses, including lack of time, knowledge, and research resources. It is imperative for oncology nurse leaders and nurse scientists to develop a supportive infrastructure to allow nursing research to flourish. Institutions wishing to expand nursing research capacity are called to innovate novel approaches to address time away from direct patient care, leverage clinical–academic partnerships, and embed a nursing culture that values nurses’ participation and leadership in research.
About the Author(s)
Elizabeth K. Arthur, PhD, APRN-CNP, AOCNP®, is a nurse scientist at the Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (The James) at the Ohio State University Wexner Medical Center and a research assistant professor in the College of Nursing at the Ohio State University, both in Columbus; Carlton G. Brown, PhD, RN, AOCN®, NEA-BC, FAAN, is the president and nurse research consultant at Zenith Healthcare Solutions in Palm Springs, CA; Lindy Martz, RN, BSN, CCM, NE-BC, is operations manager at Geisinger Knapper Clinic in Danville, PA; Lynn Weatherby, RN, BSN, OCN®, is a clinic nurse, Theresa Purcell, RN, BSN, OCN®, is a staff nurse, Jessica Dove, RN, BSN, OCN®, is a staff nurse, Emily Ridgway, MPH, is a graduate assistant, and Mina Cheriki, BS, is a graduate assistant, all at The James; Loraine Sinnott, PhD, is a senior statistician in the Data Coordinating and Analysis Center in the College of Optometry at the Ohio State University; and Robin Rosselet, DNP, APRN-CNP, AOCN®, is administrative director of advanced practice providers, research, and evidence-based practice at The James and an assistant professor of clinical practice in the College of Nursing at the Ohio State University. Arthur has received dissertation grants from the Oncology Nursing Foundation through an unrestricted grant from Genentech and Sigma Theta Tau International. Sinnott has received research funding from Vistakon. Arthur, Martz, Weatherby, Purcell, and Rosselet contributed to the conceptualization and design. Arthur, Weatherby, Purcell, and Rosselet completed the data collection. Arthur and Sinnott provided statistical support. Arthur, Brown, Weatherby, Dove, Sinnott, and Rosselet provided the analysis. All authors contributed to the manuscript preparation. Arthur can be reached at liz.arthur@osumc.edu, with copy to ONFEditor@ons.org. (Submitted March 2019. Accepted May 15, 2019.)
References
Aljezawi, M., Al Qadire, M., Alhajjy, M.H., Tawalbeh, L.I., Alamery, A.H., Aloush, S., & Albashtawy, M. (2019). Barriers to integrating research into clinical nursing practice. Journal of Nursing Care Quality, 34, E7–E11. https://doi.org/10.1097/NCQ.0000000000000371
Berthelsen, C.B., & Hølge-Hazelton, B. (2015). Orthopaedic nurses’ attitudes towards clinical nursing research—A cross-sectional survey. International Journal of Orthopaedic and Trauma Nursing, 19, 74–84. https://doi.org/10.1016/j.ijotn.2014.10.004
Bostrom, J., & Suter, W.N. (1993). Research utilization: Making the link to practice. Journal of Nursing Staff Development, 9, 28–34.
Burnett, C.B., Koczwara, B., Pixley, L., Blumenson, L.E., Hwang, Y.T., & Meropol, N.J. (2001). Nurses’ attitudes toward clinical trials at a comprehensive cancer center. Oncology Nursing Forum, 28, 1187–1192.
Chenitz, W.C., & Sater, B. (1987). Nurse’s attitudes toward research and the clinical setting as a research environment. Unpublished manuscript.
Cox, A., Arber, A., Gallagher, A., MacKenzie, M., & Ream, E. (2017). Establishing priorities for oncology nursing research: Nurse and patient collaboration. Oncology Nursing Forum, 44, 192–203.
Hagan, J., & Walden, M. (2017). Development and evaluation of the barriers to nurses’ participation in research questionnaire at a large academic pediatric hospital. Clinical Nursing Research, 26, 157–175. https://doi.org/10.1177/1054773815609889
Loke, J.C.F., Laurenson, M.C., & Lee, K.W. (2014). Embracing a culture in conducting research requires more than nurses’ enthusiasm. Nurse Education Today, 34, 132–137. https://doi.org/10.1016/j.nedt.2012.09.006
McCleary, L., & Brown, G.T. (2003). Association between nurses’ education about research and their research use. Nurse Education Today, 23, 556–565.
Melnyk, B.M., & Fineout-Overholt, E. (2018). Evidence-based practice in nursing and healthcare: A guide to best practice (4th ed.). Philadelphia, PA: Wolters Kluwer Health.
Rizzuto, C., Bostrom, J., Suter, W.N., & Chenitz, W. C. (1994). Predictors of nurses’ involvement in research activities. Western Journal of Nursing Research, 16, 193–204. https://doi.org/10.1177/019394599401600206
Roxburgh, M. (2006). An exploration of factors which constrain nurses from research participation. Journal of Clinical Nursing, 15, 535–545. https://doi.org/10.1111/j.1365-2702.2006.01374.x
Segrott, J., McIvor, M., & Green, B. (2006). Challenges and strategies in developing nursing research capacity: A review of the literature. International Journal of Nursing Studies, 43, 637–651. https://doi.org/10.1016/j.ijnurstu.2005.07.011
Silka, C.R., Stombaugh, H.A., Horton, J., & Daniels, R. (2012). Nursing research in a nonacademic health system: Measuring knowledge, attitudes, and behaviors. Journal of Nursing Administration, 42, 386–392. https://doi.org/10.1097/NNA.0b013e318261935d
Smirnoff, M., Ramirez, M., Kooplimae, L., Gibney, M., & McEvoy, M.D. (2007). Nurses’ attitudes toward nursing research at a metropolitan medical center. Applied Nursing Research, 20, 24–31. https://doi.org/10.1016/j.apnr.2005.11.003
Young, K.J. (1982). Measurement of attitudes toward the nursing research environment in the university setting [Abstract]. Journal of Nursing Education, 21(8), 46–47.




