The Effects of Virtual Reality on Anxiety and Self-Efficacy Among Patients With Cancer: A Pilot Study
Objectives: To examine the impact of a nurse-led intervention on anxiety levels and perceived self-efficacy to cope in patients receiving first-time chemotherapy using a customized prechemotherapy educational virtual reality (VR) video.
Sample & Setting: 35 patients with cancer receiving first-time chemotherapy participated in this study at a large suburban cancer center in Newark, Delaware.
Methods & Variables: A single-group, quasi-experimental pilot study was conducted to examine the feasibility of a customized prechemotherapy educational VR video in patients receiving first-time chemotherapy. The State-Trait Anxiety Inventory, heart rate, and blood pressure were used to measure anxiety, and the Cancer Behavior Inventory–Brief Version measured perceived self-efficacy to cope with cancer. Measures were taken pre- and postintervention, and patient satisfaction was examined postintervention.
Results: Anxiety level, heart rate, and blood pressure significantly decreased from baseline to postintervention, and perceived self-efficacy to cope significantly increased from baseline to postintervention.
Implications for Nursing: Personalized prechemotherapy educational VR videos could be further examined as an innovative nursing intervention to meet the health, emotional, and educational needs of diverse patient populations.
Jump to a section
An estimated 1.9 million people in the United States will be diagnosed with cancer in 2021, and for those diagnosed, chemotherapy will be a common oncologic treatment administered to cure or control cancer and to provide palliative therapy (American Cancer Society [ACS], 2021). Chemotherapy treatment consists of highly customized medications requiring an interprofessional team to deliver individualized treatment plans for each patient (ACS, 2020). Educating patients about their treatment plans is critically important because each patient will experience chemotherapy differently (Lambourne et al., 2019).
Anxiety is common among individuals who receive a cancer diagnosis and is a natural response to stressful situations (OncoLink, 2020a). Preparing for chemotherapy can be a particularly anxiety-provoking experience because of not knowing what to expect (Lambourne et al., 2019). Anxiety, in turn, may affect patients’ learning capacity (Dunn et al., 2012) and their perceived self-efficacy or confidence to cope with their cancer treatment (OncoLink, 2020b). To help alleviate anxiety and support patients coping with cancer, the National Cancer Institute (NCI, 2019) recommends cancer education sessions, relaxation training, and counseling. Although patient education is considered a cornerstone of cancer treatment preparation, patients learn in vastly different ways, and traditional written and verbal information may not be sufficient to meet their learning needs during an anxious time (Lambourne et al., 2019).
Virtual reality (VR) modalities could be a promising educational tool to deliver and reinforce pretreatment information through a visually appealing mechanism. Although VR has mostly been used as a consumer gaming device (Lessick & Kraft, 2017), researchers in health care are increasingly studying its effects and meaningful use during certain procedures. For example, VR use in both the pediatric and adult patient populations has demonstrated to be a promising tool in distracting patients from painful procedures (Glennon et al., 2018; Ng et al., 2018; Piskorz & Czub, 2017). Piskorz and Czub (2017) found that perceived pain intensity decreased among patients in the intervention group who used VR as a distraction mechanism. Because of VR’s immersive nature and required active participation, patients can focus on their simulated environment instead of their pain (Giglioli et al., 2017).
VR creates an immersive, 3D simulation, in which users have the sensation of experiencing real-life situations (Giglioli et al., 2017; Lessick & Kraft, 2017). VR can provide a safe environment for patients to explore before they start treatment (Jimenez et al., 2017). Studies have emerged in the adult oncology population examining the use of VR as a pretreatment educational tool, specifically pertaining to radiation therapy, to decrease anxiety and increase comprehension about this particular oncologic treatment (Jimenez et al., 2018; Marquess et al., 2017). A study by Marquess et al. (2017) found that providing a VR educational experience explaining radiation therapy decreased patients’ anxiety (p < 0.05) and increased their understanding of their treatment (p < 0.001). No studies were found in the literature examining the use of VR as an educational reinforcement tool aimed at decreasing anxiety and improving feelings of self-efficacy to cope with cancer before IV chemotherapy treatments commence. This is not unusual as traditional chemotherapy pretreatment education normally consists of verbal and written material (Jimenez et al., 2017).
Introducing VR as a reinforcement educational tool prior to IV chemotherapy is an innovative and novel nurse-led approach. In most of the literature examining the use of VR in patients receiving chemotherapy, VR has been used as a distraction tool to lower anxiety while patients actively receive infusions (Chirico et al., 2016), not as a pretreatment educational tool. Given the dearth of research in this area, the purpose of this pilot study was to examine the effects of a prechemotherapy educational VR video on anxiety levels and perceived self-efficacy to cope with cancer for patients receiving first-time chemotherapy treatment.
Methods
Design and Theoretical Framework
Guided by the cognitive-motivational-relational theory (Lazarus & Smith, 1988), this study employed a single-group, quasi-experimental design using a customized prechemotherapy educational VR video to measure anxiety and perceived self-efficacy to cope with cancer immediately before and after watching the VR video. Patient experience and satisfaction were also evaluated after watching the VR video. The cognitive construct, which consists of knowledge and appraisals, was the focus for this study because cognitive appraisals of information influence individuals’ emotions when exposed to different situations or experiences (Lazarus, 1991; Lazarus & Smith, 1988). Knowledge comprises situational and generalized beliefs about how things work, and appraisal is an evaluation of personal significance of encounters with the environment (Lazarus, 1991; Lazarus & Smith, 1988). Using the cognitive construct as a guide, real-life situational, environmental, and educational information delivered in the customized VR video may positively influence emotions.
Study Population and Setting
A convenience sample of patients with cancer who were scheduled to start chemotherapy for the first time at Helen F. Graham Cancer Center in Newark, Delaware, were recruited from April 2019 to March 2020. Because of the COVID-19 pandemic, enrollment stopped in March 2020. Enrollment was open to adult patients who were (a) diagnosed with cancer and scheduled to start IV chemotherapy for the first time and (b) able to read, write, and speak English. Patients were excluded if they (a) had a prior history of IV chemotherapy treatment; (b) were receiving immunotherapy only; (c) had a history of seizures; (d) had visual, auditory, and/or cognitive impairments; (e) were currently complaining of headaches; (f) had a history of motion sickness; and (g) had a history of methicillin-resistant Staphylococcus aureus related to sharing of VR equipment.
Customized Prechemotherapy Virtual Reality Video
Standard prechemotherapy education consists of personalized verbal and written explanations of patients’ chemotherapeutic treatment and a tour of the infusion suite environment prior to starting treatment. This single educational session, which takes place days to weeks before the patient’s first treatment, typically lasts for 45 minutes, with ample time to answer questions. Despite having this educational session, many clinical nurses noticed that numerous patients arrived at their first treatment feeling very anxious. These patients expressed having anxiety over not knowing what to expect, which can be a common reaction among patients preparing for cancer treatment (NCI, 2018). In addition, memory and recall of medical information is often poor and inaccurate for many patients in general, particularly when feeling anxious (Kessels, 2003).
To supplement the verbal and written prechemotherapy education patients received and to provide an innovative nurse-led educational reinforcement experience, a customized prechemotherapy VR video was developed. Clinical nurses caring for this patient population were consulted to contribute their ideas and perspectives to alleviate patients’ anxiety about what to expect on their first day of IV chemotherapy treatment. These clinical nurses were specifically asked about the common concerns they often address with patients on their first day and the educational information in need of reinforcement. Clinical nurses also informally asked various patients what they wished they knew more about before starting treatment. After receiving feedback from the clinical nurses, the study team members created a video script for nursing clinicians to use that incorporated the same terminology and nuanced language patients would hear while receiving their IV treatment. The central patients portrayed in the VR videos were real patients undergoing chemotherapy treatment who volunteered their time to film the video. None of the patients had scripted dialogue, and their suggestions were incorporated into final filming to promote the authenticity of patient and nursing clinician interactions.
Five brief video chapters were created that portrayed a typical first day of IV chemotherapy infusion, totaling 16 minutes of content. Each chapter covered different aspects of a patient’s first day from beginning to end, including initial check-in and measurement of vital signs, preparation of IV chemotherapy in the pharmacy, RN safety checks, administration of chemotherapy, discharge instructions, and nurse navigator support and resources. Video chapter locations included the waiting room, infusion suite, pharmacy, medication room, and nurse navigator’s consultation space. A unique aspect of VR was the ability to film each chapter from the patient’s point of view through an immersive 3D experience. To ensure the accuracy and authenticity of the final VR content, an interprofessional team that consisted of clinical nurses, nursing leadership, advanced practice nurses, pharmacists, and technologists reviewed and approved the final product.
Creating the VR video encompassed recruiting diverse clinicians, patients, and volunteers to portray themselves in their normal roles during their typical interactions with one another. For example, a video clip showed clinical nurses conducting two RN safety checks in the medication room after the chemotherapy medication arrived from the pharmacy. Patients waiting for their infusion cannot witness these first two RN safety checks in the secured medication room; therefore, this content was designed to reinforce the numerous safety checks involved before chemotherapy administration. Another unique aspect of the VR content was consultation with the pharmacy regarding preparation of individualized chemotherapy infusions. Patients do not have pharmacy access to visualize this process, and through the VR video, they watched an authentic portrayal of how IV chemotherapy medication is prepared in a safe and sterile environment. The “actors” in the video consisted of oncology nurses, medical assistants, pharmacists, dedicated oncology staff volunteers, and patient volunteers. The VR video content included voiceover and pop-up text to reinforce and emphasize certain educational content, such as the rationale for different safety checks, the importance of calling the office with a concern, and why preparing chemotherapy medication takes additional time.
Procedures
Prior to participant recruitment, the institutional review board at ChristianaCare in Newark, Delaware, approved the study. Potential participants were screened for eligibility and recruited into the study after receiving their in-person chemotherapy education. Patients who were interested in participating in the study were instructed to arrive one hour before their first IV chemotherapy treatment appointment. On arrival, patients were shown the VR equipment, and their questions were answered. Patients were consented while sitting in a comfortable chair. After the consenting process, the study team members showed participants the VR equipment and explained how the headset would work. Heart rate and blood pressure were measured, then participants completed the survey questionnaires. The clean and sanitized VR headset was placed on participants’ heads while they watched the 16-minute video. Immediately after the VR video concluded, participants’ heart and blood pressure were measured again, then the postintervention survey questionnaires were completed. All participants received a $5 gift card to a local cafe as a token of appreciation for their participation.
Data Collection and Measurement
Objective measurements of anxiety were assessed through heart rate and blood pressure recordings. Anxiety levels were also measured using the State-Trait Anxiety Inventory (STAI). The STAI is a widely used self-reported inventory designed to assess two dimensions of anxiety: current state and trait anxiety (Spielberger et al., 1968, 1983). The STAI has well-established criterion and construct validity, as well as internal consistency reliability coefficients ranging from 0.86 to 0.95 (Vodermaier et al., 2009). Because the current state of anxiety was of interest to the researchers, only the 20-item state survey of the STAI was used as this survey is a sensitive indicator of present anxiety (Spielberger et al., 1968, 1983). Each STAI item is given a weighted score ranging from 1 (not at all) to 4 (very much so), in which higher scores indicate greater feelings of anxiety (Spielberger et al., 1968, 1983).
The Cancer Behavior Inventory–Brief Version (CBI-B) is a 12-item measure of perceived self-efficacy to cope with cancer. The CBI-B is a shorter form of the reliable and validated CBI-Long Version (CBI-L) (Heitzmann et al., 2011). Using three different samples, the internal consistency reliability coefficients of the CBI-B were 0.84, 0.84, and 0.88, and the correlation between the CBI-B and the CBI-L was 0.95 (Heitzmann et al., 2011). Participants rate their level of confidence to perform the 12 different coping behaviors, such as sharing feelings of concern or remaining relaxed throughout treatment, using a nine-point Likert-type scale ranging from 1 (not at all confident) to 9 (totally confident), with higher scores indicating higher levels of confidence.
Prior to the VR intervention, sociodemographic data were collected through chart review and included gender, marital status, race, cancer diagnosis, cancer stage, and treatment type (chemotherapy, radiation therapy, surgery). Education level and prior use of VR were also examined. After watching the VR video, participant satisfaction with using VR was rated using a five-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). Participants were also asked a single open-ended, qualitative question about their VR experience to capture their personal feelings in their own words.
Data Analysis
Quantitative data consisted of sociodemographic characteristics, pre-/postintervention vital signs (heart rate and blood pressure), pre-/postintervention anxiety and self-efficacy scores, and satisfaction rating. Qualitative data comprised an open-ended experience question. Descriptive (means, standard deviations, frequencies, and percentages) and inferential (Wilcox matched-pairs signed ranks test) statistics were calculated using R, version 3.4. Qualitative experience responses were manually analyzed to develop a general sense of the information and to reflect on the overall meaning of responses. Through content analysis, responses were categorized and then clustered to identify themes (Creswell & Creswell, 2018). Emerging themes were discussed with study team members to ensure agreement and trustworthiness of results. 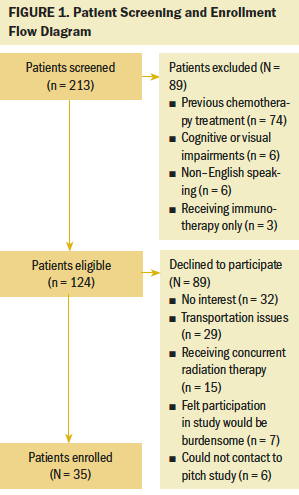
Results
Two-hundred and thirteen patients were screened for eligibility to participate in the study, and 35 patients were enrolled in the study (see Figure 1). The sociodemographic characteristics of participants are summarized in Table 1. The mean age of study participants was 61.8 years, with a range of 37–83 years. Participants had various educational backgrounds and cancer diagnoses. More women (n = 27) participated in the study; of these, 11 had a diagnosis of breast cancer. Most participants had not used VR prior to study enrollment (n = 29). 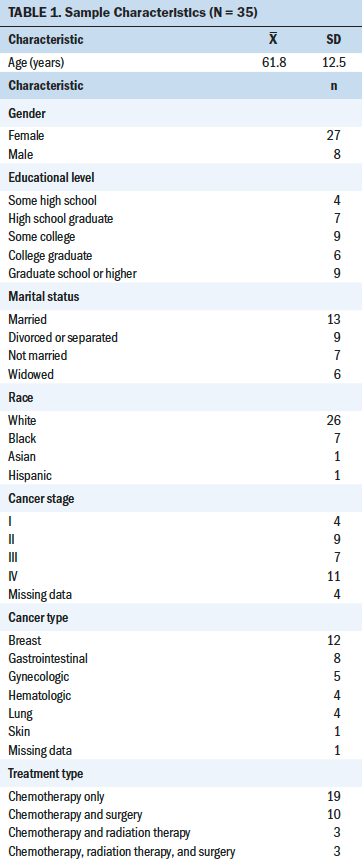
Study participants’ heart rate, blood pressure, and STAI scores significantly decreased from baseline after watching the VR video (p < 0.001) (see Table 2). Both heart rate and blood pressure measurements were positively correlated with the STAI scores (r = 0.1). Study participants’ CBI-B scores significantly increased from baseline after watching the VR video (p < 0.001). Almost all participants reported being satisfied using VR (n = 34), and all participants (N = 35) reported that the VR video enhanced the written and verbal chemotherapy education they had already received. 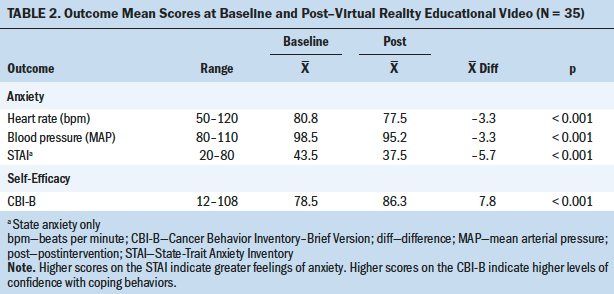
After viewing the VR video, participants answered an open-ended question regarding their experience using VR technology. Most participants reported positive feedback about their VR experience. For example, one participant stated, “It was good to see what I’m going to experience before going through it.” Another participant stated, “I think that this will help newly diagnosed patients feel more at ease.” Key themes that emerged after performing a manual content analysis included the following: enjoyable, helpful, informative, relaxing, and just OK.
Discussion
Guided by the cognitive-motivational-relational theory, this study provided preliminary evidence supporting the use of a customized prechemotherapy educational VR video to reduce anxiety and improve perceived self-efficacy to cope with initial chemotherapy treatment. Cognitively appraising the VR content appeared to influence participants’ emotions when exposed to the 3D-simulated environment. Patients had knowledge about their first day of treatment from previous written and verbal education they had received, yet they had no way of appraising the environment until after their first treatment commenced. Because of this nurse-led, innovative VR intervention, participants could be immersed in their first day of treatment before starting IV chemotherapy, enabling them to cognitively appraise the infusion suite environment and reinforce prior education.
Immersing participants in a simulated VR environment exposed and connected them to their treatment experience before starting therapy. Taking this opportunity to reinforce previous chemotherapy education provided another chance to address misconceptions or misunderstandings about treatment, as well as lessened participants’ anxious feelings of not knowing what to expect (Lambourne et al., 2019). After watching the VR video, participants’ anxiety levels, which were determined based on their heart rate, blood pressure, and STAI scores, significantly decreased from their baseline levels that had been measured immediately before watching the VR video. Feeling less anxious was a common theme found in the qualitative results. This finding is consistent with other studies measuring anxiety levels with the use of VR in radiation–oncology populations (Jimenez et al., 2017; Marquess et al., 2017). A mixed-methods study by Jimenez et al. (2017) evaluated the most and least useful aspects of Virtual Environment for Radiotherapy Training (VERT) in a sample of patients with breast cancer. Their findings revealed that most participants believed VERT helped them to visualize their radiation therapy treatment and understand their treatment (Jimenez et al., 2017). However, the educational VR video used in the current study differed from the interventions used in other studies because a customized 3D experience was created for participants receiving first-time IV chemotherapy. Participants were immersed in their infusion suite and experienced the personalized care they would receive from various staff members. Watching the video allowed for a safe space for participants to explore and visualize a full conceptualization of how their first day of treatment would be.
Understanding perceived self-efficacy to cope with cancer is important in the oncology population because patients are dealing with a wide range of emotions that can change often (NCI, 2018). Participants’ perceptions of self-efficacy to cope with cancer increased from baseline after watching the customized educational VR video. In an immersive environment, participants could observe the caring process from when they checked in through the receipt of discharge instructions at the end of treatment. In addition, participants could listen to dialogue between patients and the nurse navigator, explaining the many resources in place to support them throughout treatment. Observing these real clinical interactions in a safe VR environment prepared participants for what to expect when they started treatment, such as sources of comfort, which nurtured feelings of self-efficacy to cope with cancer.
The study sample consisted of mostly older adults who had not used VR in the past. This is consistent with the emerging literature that VR has mostly been used as a gaming device among younger individuals (Lessick & Kraft, 2017). More women than men participated in the study, which may have been related to the cancer treatment center treating a large population of patients with breast cancer who are typically female. Participants with at least some college education opted to participate in the study, which may be related to college-educated individuals having the additional resources needed to participate in studies (U.S. Food & Drug Administration, 2018). Marital status may have influenced study participation, as 63% of the participants were single, divorced/separated, or widowed. The use of VR may have provided another form of support to them.
All participants reported that the customized educational VR video enhanced the chemotherapy education they had previously received in verbal and written formats. Feeling more informed about the chemotherapy treatment process was a common theme found in the qualitative results. When patients feel better informed, they tend to have less anxiety, uncertainty, and fear associated with treatment (Saeed, 2018). Evidence supports using procedural and environmental information to facilitate patient preparation for a medical encounter (Schofield et al., 2012). Consistent with the results of previous studies, VR provided an alternative method of learning from typical prechemotherapy education (Jimenez et al., 2017). Patients may also be able to retain and understand only a certain amount of information when it is presented in a verbal format (Laws et al., 2018). According to Kessels (2003), 40%–80% of medical information is forgotten almost immediately. Providing an opportunity to immerse patients in their first-day experience with treatment while reinforcing education may help with retaining information.
Based on the qualitative experience feedback, participants found the VR video relaxing, informative, and helpful. This feedback aligns with 97% of participants reporting being satisfied with using VR. The primary reasons for creating the customized video were to reinforce the prior chemotherapy education participants had already received and to reduce their anxiety about not knowing what to expect on their first day of treatment. By watching the educational VR video, participants were able to observe a typical day of treatment while receiving a credible and factual visualization of the chemotherapeutic process.
Limitations
Several limitations were present in this study. Because of the COVID-19 pandemic and the increased risk of transmission, the study had to be stopped early, as enrollment involved direct patient contact and sharing of VR hardware. In addition, study team members were attending to other COVID-19–related issues that limited the time they had to conduct the study. The VR video used in this study was a highly customized video tailored to specific outpatient infusion sites; therefore, generalizability to other oncology and general patient populations is limited. This pilot study was meant to build preliminary evidence about using VR to improve anxiety and perceived self-efficacy to cope with cancer among patients receiving first-time chemotherapy treatment. To determine causality, future studies would need a control group with multiple arms to evaluate whether the immersive quality of VR, the VR educational content itself, or prior in-person chemotherapy education had the greatest impact on anxiety levels and perceived self-efficacy. The sample size was small, and a convenience sampling technique was employed, which may have contributed to selection bias. To lessen potential biases, study team members attempted to recruit a diverse patient population scheduled to begin receiving IV chemotherapy treatment.
Implications for Nursing
Patients with cancer diagnoses typically receive interventions aimed at decreasing their anxiety while actively undergoing treatment, such as music therapy, mindfulness meditation, and coaching (Smith et al., 2014). However, few interventions directly target reducing anxiety in preparation for patients’ initial chemotherapy treatment. To reduce this gap in available anxiety-reducing interventions before treatment, nurses can seek new ways to reach patients, possibly with the aid of technology. VR, which has the capability of immersing patients in different aspects of their treatment course, could be one of those aids.
Applications for VR are virtually limitless (Chirico et al., 2016). VR could be used in many different patient populations and settings, such as presurgical and preprocedural education. In addition, VR could be used for many different aspects of nursing care, such as relaxation during procedures to reduce the need for medications (Glennon et al., 2018; Mohammad & Ahmad, 2018). Even with these potential uses, financial and personnel resources should be considered prior to implementation. Because many devices cost hundreds of dollars, VR hardware could be cost prohibitive (Robertson, n.d.). A less expensive alternative could be asking patients to use their personal smartphone within a VR cardboard box, such as Google Cardboard (https://arvr.google.com/cardboard), to simulate a closed environment. Dedicated staffing resources are also needed to set up the hardware and videos for patients’ use. Hospital volunteers may be able to help in this regard, enabling nurses and aides to continue participating in their typical patient care duties. 
Conclusion
This study contributed to the limited knowledge about using educational VR videos as a nursing intervention to aid in patients’ preparation for first-time chemotherapy treatment. Patients who participated in the study enjoyed the experience and felt less anxious and more confident in their ability to cope with their cancer treatment after watching the customized VR video. In addition to patients receiving first-time treatment, personalized educational VR videos could be created to meet the diverse health and educational needs of various patient populations through an immersive 3D experience.
The authors gratefully acknowledge the patients who participated in this study. They also extend their gratitude to the Health and Technology Innovation Center at ChristianaCare for sharing their virtual reality (VR) technology expertise and guidance and NAPCO Media for filming and producing the customized VR video.
About the Author(s)
Susan D. Birkhoff, PhD, RN, is a nurse scientist in the Department of Nursing Research and Evidence Based Practice; Cynthia Waddington, MSN, RN, AOCN®, NE-BC, is the clinical director of the cancer program, Jordan Williams, BSN, RN, OCN®, is a clinical practice coordinator, and Leslie Verucci, MSN, CNS, APN-BC, is a nurse practitioner and Maureen Dominelli, RN, BSN, is an RN, both on the Oncology Express Unit, all at the Helen F. Graham Cancer Center; and Richard Caplan, PhD, is a senior biostatistician in the Value Institute, all at ChristianaCare in Newark, DE. This study was funded by the 2018 American Nurses Credentialing Center Magnet® Prize, sponsored by Cerner. Birkhoff, Waddington, Williams, Verucci, and Caplan contributed to the conceptualization and design. Birkhoff, Waddington, Williams, Verucci, and Dominelli completed the data collection. Birkhoff and Caplan provided statistical support. All authors provided analysis and contributed to the manuscript preparation. Birkhoff can be reached at susan.birkhoff@christianacare.org, with copy to ONFEditor@ons.org. (Submitted December 2020. Accepted January 28, 2021.)




