Characterizing Beliefs About Breast Cancer and Comorbid Diabetes After Cancer Treatment
Purpose: To investigate how breast cancer survivors with comorbid diabetes mellitus (diabetes) conceptualize their illnesses.
Participants & Setting: 19 community-dwelling, English- or Spanish-speaking women with diabetes in New York, New York, who received chemotherapy or hormone therapy for stage I–IIIA breast cancer in the past five years.
Methodologic Approach: Semistructured interviews were administered by trained research staff, and were audio recorded and transcribed. Three coders reviewed transcripts through an iterative coding process. An interpretive descriptive approach was used to identify themes.
Findings: Major themes included an inverse relationship between illness control and concern, variation in perceived illness permanence, and differences in illness consequences. Women with a greater perceived control over breast cancer viewed their diabetes as a larger concern; others felt that their breast cancer could not be controlled but diabetes could.
Implications for Nursing: Understanding how breast cancer survivors view diabetes and cancer may explain the variation in survivors’ self-management behaviors, and how it may influence their attitudes and behaviors in the context of cancer treatment.
Jump to a section
With rates of survival for early-stage cancer diagnoses increase, a growing number of cancer survivors are living with chronic illnesses, such as diabetes mellitus (diabetes). This is particularly true among older adult cancer survivors, who are more likely to have at least one chronic illness. In 2015, an estimated 12.2 million U.S. adults aged 65 years or older had diabetes (Centers for Disease Control and Prevention, 2017). Although patients often perceive a cancer diagnosis as a higher threat, older adults with early-stage cancer may be at a greater risk of dying from a chronic illness instead. In a cohort of older adult patients with breast cancer, fewer than half (43%) died from cancer; and comorbidities, including heart failure and diabetes, significantly predicted shorter survival times (Siegelmann-Danieli et al., 2006). A review of 18 cohort and case-control studies of older patients with breast cancer and comorbidities similarly found that diabetes was associated with reduced odds of survival (Land et al., 2012; Lipscombe et al., 2007). Studies have found hazard ratios of 1.21:1.65 for all-cause mortality among patients with breast cancer and diabetes, compared to those with breast cancer alone (Cleveland et al., 2012; Jiralerspong et al., 2013; Zhou et al., 2014). As a result, comorbidity management requires more attention in cancer care, particularly among older adult survivors (Yancik et al., 2001).
One comorbid condition of particular concern is diabetes because women with preexisting diabetes appear to be at an increased risk for a breast cancer diagnosis. One meta-analysis found a summary risk ratio of 1.27 for breast cancer among women with diabetes (Boyle et al., 2012), and others found a hazard ratio of 1.17 for breast cancer as compared to women without diabetes after considering weight, age, and family history of cancer (Michels et al., 2003). Emerging literature focused on the effects of breast cancer on chronic health management in older adult women demonstrated that breast cancer survivors have decreased adherence to diabetes medication and poorer hemoglobin A1C control following cancer treatment (Calip et al., 2014; Santorelli et al., 2016). One explanation for this relationship between cancer and decreased medication adherence or worse diabetes outcomes may be that cancer survivors’ perceived level of control over their health affects their choice of coping strategies, and healthy versus unhealthy coping approaches may predict adherence to self-management behaviors (SMBs) (Park et al., 2008). In fact, one of the most important determinants of SMBs is patients’ beliefs about their illness. According to the Self-Regulation Model (Leventhal et al., 1984), illness perceptions influence expectations about the effectiveness and necessity of SMBs, which, in turn, affects patients’ level of engagement in SMBs, with potential for long-term health consequences.
For patients with diabetes, research has shown that stronger beliefs in one’s control over diabetes—in the effectiveness of diabetes treatments and in the probability of survival—predict closer adherence to diabetes SMBs recommendations (Harvey & Lawson, 2009; Mann et al., 2009; Vedhara et al., 2014). Other factors, such as culture, psychosocial factors, and comorbid illnesses, are also significant contributors to diabetes SMB adherence (Gonzalez et al., 2016; Nam et al., 2011). In the extensive literature regarding patients’ beliefs about diabetes, nearly all studies have relied on standardized survey questions to collect the data. These measures, although informative, limit the ability to capture a concept as subjective as illness perception, which may be better explored through an individual’s own responses.
A limited number of qualitative studies have examined patient concepts of diabetes and cultural factors that affect SMBs. For example, qualitative work conducted with Caribbean women with diabetes found themes surrounding the importance of a traditional diet; patients who believed in spiritual cures for diabetes showed lower diet and medication adherence (Magny-Normilus et al., 2019; Smith, 2011). This study stresses the need for culturally informed SMB recommendations for diabetes; however, many other important questions about perceptions of diabetes would benefit from qualitative investigations. A deeper understanding of diabetes beliefs in the context of other comorbid illnesses is of particular importance, given the high rates of comorbidity for diabetes with other chronic illnesses (Iglay et al., 2016) and cancers (Lo et al., 2012; Michels et al., 2003; Wolf et al., 2005).
The Self-Regulation Model has also been applied to elucidate patients’ perceptions of breast cancer and their effects on SMBs. A longitudinal study of women undergoing breast cancer treatment found that those who perceived more severe consequences and an ability to control breast cancer through health behaviors were more likely to increase efforts to follow SMBs for breast cancer post-treatment, including diet and physical activity (Costanzo et al., 2010). Other research has explored indications among women facing a new breast cancer diagnosis who are more likely to believe that health behaviors affect their breast cancer; early signs of this belief include an overall positive attitude and belief in one’s control over life (Henselmans et al., 2010).
As with diabetes, most of the research on breast cancer beliefs has been conducted using survey instruments, with a few notable exceptions. In the literature, qualitative work on breast cancer beliefs focused on the influence culture has on illness perceptions, particularly among Hispanic (Flórez et al., 2009) and Black (McQueen et al., 2011) women. Although these studies highlight the importance of qualitative exploration of breast cancer beliefs for developing culturally informed provider recommendations, addressing the unanswered question of how breast cancer beliefs occur in the context of other comorbid health conditions would arguably enrich the literature on breast cancer perceptions and associated SMBs.
The experience of receiving a breast cancer diagnosis and undergoing treatment is often a significant health event and may have a unique impact on beliefs about preexisting comorbid health conditions, such as diabetes. In support of this expectation, diabetes SMBs after a cancer diagnosis have been associated with a number of psychological and social changes, including higher rates of distress and lower rates of employment after treatment, particularly among women with comorbidities (Ahn et al., 2008; Syrowatka et al., 2017). To date, no qualitative investigations have focused on understanding the interrelationship between patients’ beliefs about cancer and chronic illness. This constitutes a gap in current knowledge of patients’ subjective understanding of comorbid health conditions, and exploring these beliefs may help to identify potential patterns of patient beliefs that could explain nonadherence to SMB recommendations among patients navigating multiple illnesses. The present study aimed to understand how older adult breast cancer survivors with comorbid diabetes characterize their experiences with both illnesses, using a qualitative data collection approach and interview questions based on the Self-Regulation Model.
Methodologic Approach
Participants were asked to share their experiences with breast cancer and diabetes through a semi-structured, in-person interview with a trained research coordinator who had prior experience conducting research interviews with cancer survivors with comorbid diabetes. The interview guide (see Figure 1) was developed to address the following a priori themes: the impact of breast cancer and diabetes on everyday life; concern about breast cancer and diabetes; experiences with treatment for both illnesses; engagement in SMBs for both illnesses (including medication adherence, diet, and exercise); beliefs about the importance of SMBs for each illness; and the cognitive effects, if any, of chemotherapy and/or hormone therapy. Questions regarding illness beliefs were modeled after the Brief Illness Perception Questionnaire (Broadbent et al., 2006), a validated quantitative measure of illness beliefs based on the Self-Regulation Model (Leventhal et al., 1984). The Brief Illness Perception Questionnaire covers eight key domains of illness beliefs on an 11-point scale. Researchers for the current study believed these eight questions would be relevant to patients with both breast cancer and diabetes, but they presented them to the patients as open-ended questions to elicit more meaningful information and responses. Other questions regarding diagnosis and treatment experiences, SMBs, and cognitive effects were developed through discussion and were later revised through pilot testing by the research team. 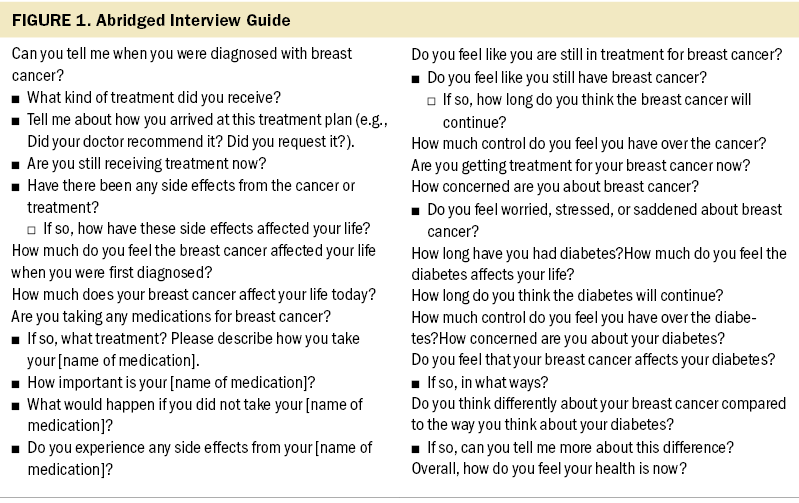
All interviews lasted for approximately 45–60 minutes and were audio recorded with participant consent. The recordings were transcribed by a professional transcription service, and the Spanish-language interview was translated and back-translated by research staff fluent in Spanish before coding. All transcripts were proofread, and random sections were verified through comparison to the audio recordings by a research coordinator. Interviews were coded through an iterative process, and the research team met regularly to discuss emergent themes and determine when saturation was reached, with the expectation that saturation would occur after 12–20 interviews (Guest et al., 2006).
A team of three independent coders reviewed all transcripts in full and then reread each interview line by line and recorded all instances of a preestablished set of initial codes grounded in the theoretical framework of the study. While applying the initial codebook, each coder also identified new in vivo codes, which the team reviewed and added to the evolving codebook. The coders met regularly throughout the coding process to discuss each transcript, revise the codebook based on the data thus far, and resolve coding discrepancies through in-person discussions to reach a consensus. A final codebook was developed through an iterative process, and final coding was entered in ATLAS.ti, version 8.2. The research team reviewed final code frequencies and intersections to identify codes or code groups with substantial content and then reread content coded in these groups to generate major themes. Analysis consisted of a combination of deductive review for themes surrounding the illness belief domains from the Self-Regulation Model and inductive development of themes based on in vivo codes and observed relationships between beliefs in the data.
Participants and Setting
The researchers identified breast cancer survivors with diabetes through the cancer registry of a large metropolitan hospital system in New York, New York. With the providers’ consent, the research team verified eligibility criteria through reviewing patients’ electronic health records and contacted individual breast cancer survivors via a mailed letter and follow-up telephone call. Patients were considered eligible if they were aged 55 years or older, were diagnosed with stage I–IIIA breast cancer, received chemotherapy or hormone therapy for breast cancer in the past five years, were diagnosed with type 2 diabetes more than one year ago and prior to the breast cancer diagnosis, and were community-dwelling English- or Spanish-speaking. Individuals were excluded if they had a major cognitive impairment or were unable to travel to the research offices for an in-person interview. Recruitment was conducted until thematic saturation was reached, which occurred after 19 interviews. Thematic saturation was considered to have been achieved when no codebook revisions or new patterns of response emerged from five consecutive interviews.
All interested participants provided in-person informed consent. The research procedures were approved by the institutional review board at the Icahn School of Medicine at Mount Sinai in New York, New York.
Participant age, race/ethnicity, breast cancer staging, diagnosis, and treatment history were obtained from medical records. Univariate statistics were run in IBM SPSS Statistics, version 26.0, to determine demographic characteristics, hemoglobin A1C levels, and breast cancer treatment history of the sample, including mean and standard deviation for age, as well as frequencies and percentages (see Table 1). 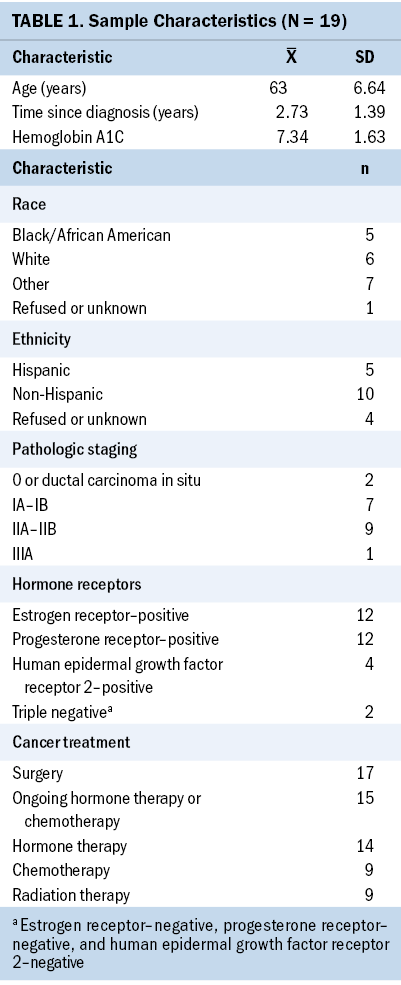
Findings
A total of 53 breast cancer survivors with diabetes were identified within the medical system and contacted with their provider’s permission. Of these, 19 participated in the qualitative interviews, with 18 conducted in English and 1 in Spanish. The participants’ average age was 63 years (standard deviation [SD] = 6.64), and five women self-identified as Black or African American, five as Hispanic or Latina, and six as White. Two participants identified as other or more than one race/ethnicity, and one declined to provide race and/or ethnic data.
Two participants were diagnosed with stage 0, or ductal carcinoma in situ, seven with stage IA–IB, nine with stage IIA–IIB, and one with stage IIIA breast cancer. Twelve of the participants had estrogen receptor–positive cancers, 12 had progesterone receptor–positive cancers, 4 were positive for human epidermal growth factor receptor 2, and 2 were triple-negative (estrogen receptor–negative, progesterone receptor–negative, and human epidermal growth factor receptor 2–negative). On average, participants were diagnosed with breast cancer 2.73 years (SD = 1.39) prior to the interviews. Seventeen had undergone surgical treatment for breast cancer, 9 received first-line and/or adjuvant chemotherapy, 9 received radiation therapy, and 14 received hormone therapy. At the time of the study, most of the women (n = 15) were still receiving either hormone therapy or chemotherapy. Their average hemoglobin A1C at the time of participation was 7.34 (SD = 1.63).
The authors identified three major themes related to the interrelationship of illness beliefs about breast cancer and diabetes: the inverse relationship between perceived control and concern, illness permanence, and types of long-term illness consequences.
Control Versus Concern
The majority (n = 17) of participants identified either breast cancer (n = 13) or diabetes (n = 4) as being under better control and, therefore, causing less concern, while expressing an inverse relationship for the other condition. Of the remaining two participants, one did not explicitly discuss control over diabetes, and the other did not discuss concern about diabetes. Some women (n = 3) felt that their breast cancer was well controlled through treatment, whereas diabetes was a larger concern for their present health. As one participant said:
I think that if you get the cancer, and you catch it, and you are cancer-free, I believe as long as you can stay cancer-free you’re fine; where I think the diabetes will continue to deteriorate different parts of my body.
Another woman explained her perception of the two illnesses as, “Diabetes is more different, more dangerous than cancer, for me. Diabetes has bothered my vision. . . . At least cancer is controllable, but diabetes is not because it goes in the blood.”
Among women who expressed that breast cancer was more controllable than diabetes, the most important SMB for breast cancer was usually identified as adherence to ongoing hormone therapy. As one participant stated, “I have complete control [over breast cancer]. [I] take the pill.” A participant who had completed her medication regimen for breast cancer commented on losing this aspect of control. When asked if she was taking medications for breast cancer, she responded, “No. I kind of wish I were. It would make me feel a little safer.”
Participants who were still receiving either hormone therapy or chemotherapy at the time of the interviews (n = 15) were generally less concerned with breast cancer (two expressed concern about breast cancer) than with diabetes (10 expressed concern about diabetes). Participants with earlier stages of breast cancer (stages o–I), nearly all of whom were still in treatment (n = 8), felt that their breast cancer was well controlled and not as concerning to them at the time as diabetes (n = 7). Participants with more advanced cancer felt that their breast cancer was not well controlled (n = 7). Among participants with both a greater time since their breast cancer diagnosis (two to five years) and those with a more recent diagnosis (less than two years), only a few women viewed their breast cancer as a current concern for their health (n = 4 and n = 0, respectively).
In contrast, a number of women (n = 7) felt diabetes could be controlled through self-management, but cancer was beyond their control and, therefore, a larger concern. One participant stated, “I don’t think the diabetes affects my life, I think I affect my life. I think I’m more in control of the diabetes than I am the cancer.” Another participant said, “Breast cancer, I can’t control that, because if it’s going to come, it’s going to come. But the diabetes, I know what not to do.”
Women who felt they had control over their diabetes frequently attributed this control to SMBs, and particularly to diet control. One participant explained that she felt she could control her diabetes through careful diet maintenance:
[I] try to eat the right foods. . . . I have to really put my foot down and not have . . . cheesecake, you want to take—“Oh, this tastes so good,”—and you just take one slice. And, I try to stay away from things like that, and I’ve been drinking plenty of water.
As another woman noted, having control does not necessarily mean perfect adherence: “My diabetes is in control . . . because I don’t eat very much, and I don’t [eat] much sweets and all that.” The four participants who had completed breast cancer treatment at the time of their interview expressed low concern about both breast cancer and diabetes and felt that diabetes was well controlled, which was supported by their hemoglobin A1C values.
Illness Permanence
Another major theme was the variability in the perceived permanence of breast cancer compared to diabetes. When asked, “Do you think you still have cancer?” responses varied widely. Most of the women (n = 13) responded that they did not (e.g., “I don’t think so. That’s weird, I haven’t thought about that. I guess I have no evidence of disease, I mean, they kind of took it.”). All nine women who were diagnosed with earlier stages of breast cancer, and most of those who were in the first two years since the diagnosis (n = 5) felt that cancer was a short-term illness. Others (n = 2) were unsure, stating, “I don’t know, because sometimes [my breasts] hurt, and I get cysts underneath.” For some women (n = 2), breast cancer remained a prominent threat that could affect the rest of their lives: “[I live with] that fear of, ‘Is it going to be breast [cancer] again? Am I going to have metastasis to the lung?’ that kind of thing. And so I live in fear.” On the other hand, participants were generally in agreement that diabetes is chronic and permanent. When asked, “How long do you think you’ll have diabetes?” nine women responded “forever” or “for the rest of my life.” As one participant explained, “I think the diabetes is permanently [sic], but the cancer can be treated.” Others (n = 2) were unsure of how long diabetes would continue to affect them, and several (n = 6) believed that their diabetes might be fully resolved in the short-term through medication, diet, and exercise. One woman expected that her diabetes would last “probably around a year . . . because I think I should be able to get my blood sugar numbers back to normal.”
In comparing their breast cancer and diabetes, eight women believed that one illness would affect their lives for much longer than the other and used this as a point of contact between the two health conditions.
Types of Illness Consequences
A third theme was the recognition of different consequences of breast cancer and diabetes. When asked to compare their breast cancer and diabetes, almost half of the women (n = 8) felt the two conditions were more different than alike. One participant responded, “Well, I think they’re two different diseases. Like, diabetes can’t metastasize.” Similarly, another participant explained the differences:
Well, breast cancer could kill me quickly. . . . Diabetes—that’s unlikely. But diabetes, there are other symptoms involved, other negative side effects. The breast cancer is either going to spread or not, or reoccur or not. It’s kind of apples and oranges.
Eleven of the participants identified the consequences of diabetes as being more severe than breast cancer, in many cases based on the experiences of loved ones with diabetes. As one participant said:
When I was diagnosed with diabetes, I was definitely much more upset than I was when I was diagnosed with cancer. . . . I mean, cancer is a big deal, don’t get me wrong, but I felt that I had done it to myself. And I had, because my father was a diabetic and my grandmother was a diabetic.
Regarding the long-term consequences, another said, “I see it in my brothers who had [diabetes]. One of my brothers had part of a foot and a toe off his other foot amputated, maybe like two months ago.” Even participants without a family history of diabetes were highly aware of the potential consequences, and the SMBs recommended to prevent complications. One participant said:
Well, you have to be careful because diabetes is a very serious disease. You can lose your limbs. And they say it affects other parts of the body, and they tell me, “Always check your feet—especially between the toes.”
By contrast, the remaining women (n = 7) felt breast cancer had more severe consequences, including the risk of metastasis and ongoing cognitive or emotional effects. One woman suspected she was experiencing long-term cognitive effects of breast cancer and said, “I didn’t know if the breast cancer affects your brain or anything. But I know that I’m not as quick, as OK to read something—I don’t remember it.” Others believed that although breast cancer had immediate consequences in their lives, the long-term consequences were limited. One participant said, “It’s really not in my hands, but I guess I’m lowering the chance of [metastases], because it can’t recur because I have a double mastectomy.”
Among women of various breast cancer stages, time since diagnosis, hemoglobin A1C levels, and perceptions of breast cancer or diabetes as having serious consequences did not appear to follow a clear pattern for which illness was considered more severe. However, most women’s responses reflected an inverse relationship, where one illness was viewed as having severe consequences and the other as less threatening to their current health.
Discussion
Overall, women generally perceived one illness to be more concerning and less controllable than the other, although opinions varied on which illness was most concerning. Women who were more recently diagnosed and still undergoing treatment and those who had less advanced stages of breast cancer generally considered their breast cancer under control and, therefore, less concerning than diabetes. Most patients saw diabetes as a lifelong illness, whereas women had differing views on the chronicity of breast cancer. Those with more recent breast cancer diagnoses or earlier breast cancer stages considered breast cancer as a short-term condition, while others viewed it as chronic. Some viewed breast cancer as a resolved illness, but others considered it an ongoing health risk. Women attributed different consequences to the two diagnoses: Breast cancer was associated with more psychological symptoms, whereas diabetes was associated with more severe physical consequences.
The findings of this qualitative study provide insight into how health concerns differ among cancer survivors with comorbid chronic illnesses. Older adult breast cancer survivors with diabetes have widely varied experiences with these two illnesses that inform their perceptions of each illness. These illness perceptions may then affect how cancer survivors view their current health, their long-term prognosis, and the effectiveness and importance of health management activities, which may then contribute to their health behaviors.
Although SMBs were not the central focus of these interviews, participant responses related to diabetes and breast cancer provided evidence of the ways in which comparative beliefs about comorbid illnesses can affect health management. In the current study, participants who viewed breast cancer as more controllable highlighted medication adherence as a method of control, whereas women who felt a greater ability to control their diabetes reported managing their health through diet. These findings align with existing quantitative evidence that illness perceptions, and particularly perceived control over illness, can be related to SMBs for both diabetes (Harvey & Lawson, 2009; Mann et al., 2009; Vedhara et al., 2014) and breast cancer (Henselmans et al., 2010). Therefore, it is important to recognize that cancer survivors with comorbidities have a range of illness beliefs, and it is also important to identify where survivors’ concerns are greatest. This can help providers to sufficiently understand their patients’ beliefs and how those beliefs may affect SMBs. Future research should explore how cancer and chronic illness beliefs correspond with SMBs for each illness among cancer survivors with comorbidities, and whether provider exploration and intervention on these beliefs could be an effective avenue for behavior change.
Although this qualitative approach provided new insights into the beliefs and valuations of cancer survivors with comorbid illness, the study was not without its limitations. Because of the selection of participants from a single urban setting, the results may not be generalizable to breast cancer survivors in other settings. In addition, the sample was limited to participants with breast cancer and diabetes, only one of a multitude of possible combinations of cancer and chronic illness diagnoses experienced by older adults. Although not a limitation, it is also important to note that the sample consisted only of women with a history of breast cancer, and, therefore, the findings of the study may be specific to the context of their gender and/or diagnosis. Despite these limitations, the study provided insight into patient conceptualizations of illness and developed a framework to compare cancer and a chronic illness.
Implications for Nursing
These findings can inform oncology nursing practice by illustrating how beliefs about other health conditions may influence patients’ attitudes and behaviors in the context of cancer treatment. Current efforts to improve diabetes SMBs by targeting health beliefs have had mixed success, with some programs effectively increasing SMBs (Jalilian et al., 2014) and others showing little to no improvement over usual diabetes care (Chatterjee et al., 2018; Khunti et al., 2012). The impact of contrasting illness beliefs about comorbid illnesses should be considered in breast cancer care because this may provide a route to improving SMBs for patients who have been unresponsive to interventions solely focused on one illness. 
Conclusion
These results provide a greater understanding of varied experiences of cancer survivors with comorbidities and provide potential implications for improving diabetes SMBs among older adult cancer survivors. Based on past evidence that a greater sense of control over cancer predicts more engagement in health habits, such as diet, exercise, and sleep (Park et al., 2008), breast cancer survivors who feel their cancer is under control may be more focused on managing their other health concerns, such as diabetes. Conversely, patients who see cancer as uncontrollable may be less consistent in maintaining SMBs. By contextualizing patients’ breast cancer beliefs and behaviors in their overall health management, practitioners may be able to more effectively identify and intervene on patient nonadherence or hesitancy in cancer treatment.
About the Author(s)
Kimberly A. Muellers, MPH, MS, is a clinical research coordinator in the Division of General Internal Medicine at the Icahn School of Medicine at Mount Sinai and a graduate student in the Department of Psychology at Pace University, both in New York, NY; Sarah Prieto, MA, is a graduate student in the Department of Psychology at the Ohio State University in Columbus, OH; and Jenny J. Lin, MD, MPH, is a professor in the Division of General Internal Medicine at the Icahn School of Medicine at Mount Sinai. This work was supported by the National Cancer Institute (R01CA214491 to JJL). Muellers and Lin contributed to the conceptualization and design. Prieto and Lin completed the data collection. Lin provided statistical support. All authors provided the analysis and contributed to the manuscript preparation. Muellers can be reached at kmuellers@pace.edu, with copy to ONFEditor@ons.org. (Submitted June 2021. Accepted September 9, 2021.)

