Patients With Advanced Cancer and Minor Children: An Exploratory Study of Health-Related Quality of Life and Satisfaction With Care
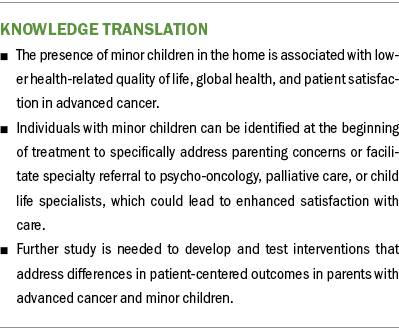
Objectives: Patients with advanced cancer and minor children experience high rates of depression and anxiety. However, associations between parental status and other aspects of the patient experience are not well understood. This study compared patient-reported outcomes of patients with and without minor children.
Sample & Setting: This was a retrospective analysis of 448 adults with stage III or IV solid tumors from a public research registry.
Methods & Variables: Multiple linear regression models or modified Poisson regression models were fitted to evaluate differences in health-related quality of life, global health, and patient satisfaction scores between patients living with and without minors.
Results: One in five patients lived with minor children. They reported significantly worse health-related quality of life, global physical health, and global mental health. They also expressed lower satisfaction with time spent with their provider, communication, and financial aspects.
Implications for Nursing: Patients with minor children may benefit from earlier identification and support for their psychosocial needs and concerns.
Jump to a section
For most individuals, an advanced cancer diagnosis profoundly affects their physical, emotional, spiritual, and family well-being. Disruptions in family responsibilities, increased reliance on caregivers, financial concerns, and alterations in household routines are common (Moore et al., 2015; Schmitt et al., 2008). Patients with advanced cancer experience these changes within the context of their family unit, and those with minor children (aged younger than 18 years) report distinct challenges to parenting. Healthcare systems frequently under-recognize these challenges, despite the central importance of parenting for nearly all adults with minor children (Oláh, 2015; Taylor et al., 2011). This gap underscores the need to better understand the cancer experience for these individuals.
Parenting with advanced cancer frequently leads to serious psychological distress (Park et al., 2016). About 60% of individuals surveyed in cross-sectional studies of parents with advanced cancer reported clinically significant depression and anxiety symptoms. Individuals with advanced cancer and minor children are five times more likely to develop anxiety disorders than individuals without children (Nilsson et al., 2009; Park et al., 2016). Several experiences unique to parents may contribute to this phenomenon, such as the practical challenges of raising dependents while severely ill, the need to articulate and discuss illness in developmentally appropriate ways, and concerns about the emotional impact of their illness on their children (Muriel et al., 2012; Sinclair et al., 2019). Parents with advanced cancer must cope with heightened grief and worry about dying before their children reach adulthood (Park et al., 2017). Those who lack a coparent face the additional psychological and practical challenges of addressing guardianship needs (Nelson et al., 2020). Taken together, these studies suggest that having minor children affects psychological health in patients with advanced cancer. Expanding the understanding of the cancer experience for these individuals could provide important insights on how to improve patient-centered care.
Modern cancer care increasingly strives to be responsive to patients’ values, needs, and preferences (Warsame & D’Souza, 2019). Several patient-reported outcomes (PROs), such as health-related quality of life (HRQOL), reflect this patient-centered goal. Individual and family factors beyond the healthcare setting can also shape patients’ experience of cancer and HRQOL. For example, increased age, positive religious coping, and better performance status are associated with higher HRQOL in patients with advanced cancer (Jordhøy et al., 2001; Tarakeshwar et al., 2006) Further characterizing these factors can help contextualize the impact of cancer and potentially make HRQOL assessments more useful. However, current research is limited because most oncology studies evaluating HRQOL lack data on parental status (Ernst et al., 2012; Kypriotakis et al., 2016; van Roij et al., 2018).
Most studies that address parents with advanced cancer focus on the effects of cancer itself on the patient or their family. Outside of the pediatric setting, few studies have examined parents’ satisfaction with cancer care and the extent to which their expectations as parents were met (Wolf et al., 2008). As with HRQOL, characteristics intrinsic to patients themselves can also influence assessments of patient satisfaction. For example, young adults and women are more likely to report greater dissatisfaction with their cancer care, as are patients with higher symptom burden (Lis et al., 2009; Walker et al., 2003). In addition, clinical characteristics like cancer type and severity can influence patient satisfaction with care (Bitar et al., 2004; Kleeberg et al., 2005). Clinician behaviors, such as clear communication and attentiveness to how the patient is coping with illness, also affect patient satisfaction (Lis et al., 2009). These factors may be particularly relevant for patients with minor children and advanced cancer. To date, no prior study has evaluated the role of parental status and patient satisfaction with cancer care.
Patients’ perceived HRQOL and satisfaction with care are important components of patient-centered care. Nearly all adults with minor children consider their parental role central to their personal identity, yet this characteristic is rarely addressed in routine cancer care. Although prior studies of parents with advanced cancer include assessments of PROs, they typically rely on participant samples without a clear comparison group (Nilsson et al., 2009; Park et al., 2018; Schmitt et al., 2008), which limits the ability to contextualize study findings. By using a large retrospective cohort, this study sought to generate new insights into the patient experience of parents with advanced cancer. The purpose of this study was to describe and compare HRQOL, global health, and patient satisfaction among patients with advanced cancer with and without minor children.
Methods
Design and Sample
This is a secondary analysis of data collected through the University of North Carolina at Chapel Hill’s Health Registry/Cancer Survivorship Cohort (HR/CSC). This is an institutional review board–approved registry of 5,624 patients that combines patient interview data with clinical, epidemiologic, and biologic specimens. Eligible patients were recruited from outpatient oncology clinics between 2010 and 2016 if they were 18 years or older, had a cancer diagnosis, had a North Carolina mailing address, and were proficient in English or Spanish. Fifty-two percent of approached individuals enrolled in the HR/CSC. Details about the HR/CSC cohort have been previously reported and are publicly available (Pergolotti et al., 2017; Smitherman et al., 2018). This project was reviewed and approved by the Human Research Protections Program (Institutional Review Board Number: 09-0605) at the University of North Carolina at Chapel Hill.
Of the 5,624 patients in the HR/CSC, 470 individuals were diagnosed with advanced cancer, defined here as a pathologically confirmed solid tumor with regional or distant metastases. Of these individuals, 22 were excluded because of uncertainty with respect to their cancer stage or type. The remaining 448 patients were divided into two groups: patients living with minors if they had at least one minor child and patients living without minors if they reported no minor children in the home. Patients with hematologic malignancies were excluded because of the small number participating in the cohort (2.2%) and the added complexity of assessing disease severity in these individuals.
Measures and Data Collection
Within two weeks of participant enrollment in the HR/CSC, trained interviewers conducted a cross-sectional, structured interview using computer-assisted telephone software (University of North Carolina, 2014). Data from the HR/CSC were linked to patient electronic health records to ascertain cancer diagnosis and stage. Demographic questions gathered data on age, gender, employment status, race, and ethnicity (University of North Carolina, 2014). Participants did not provide their income or insurance status. The interviews addressed lifestyle and health history, as well as several standardized measures of PROs (University of North Carolina, 2014). This study evaluated the following PROs identified as highly relevant to the population of parents with advanced cancer: functional status, HRQOL, global health, and patient satisfaction. Only participants with complete data (72%) were included in this study.
HRQOL: The Functional Assessment of Cancer Therapy–General Population (FACT-GP) assesses four dimensions of HRQOL: physical, functional, emotional, and social/family well-being. The 21-item scale uses a five-point ordinal scale ranging from 0 (not at all) to 4 (very much) with total scores ranging from 0 to 84 (Janda et al., 2009; Webster et al., 2003). Higher scores indicate better HRQOL, and the minimal clinically significant difference (MCID) is estimated to be five points (Doll et al., 2015). Prior studies have confirmed the FACT-GP’s population norms, factor structure, internal consistency, and validity, as well as its ability to identify patient needs and assist in directing care (Adonizio et al., 2019; Janda et al., 2009).
Global health: The National Institutes of Health’s Patient-Reported Outcomes Measurement Information System (PROMIS) Global-10 is a widely used, highly reliable, well-validated 10-item scale assessing fatigue, physical function, pain, emotional distress, and social health (Hays et al., 2009). The PROMIS Global-10 has two components: physical health and mental health. For all PROMIS measures, raw scores are converted into a T score, whose distributions are standardized to the U.S. population (population mean = 50, SD = 10). Higher scores reflect better overall function, and the MCID ranges from two to six points (Yost et al., 2011).
Patient satisfaction: The 18-item Patient Satisfaction Questionnaire Short Form (PSQ-18) is an internally reliable, well-validated self-report measure assessing general patient satisfaction in six dimensions: technical quality (proficiency), interpersonal manner, communication, financial aspects, time spent with doctor, and accessibility and convenience (Thayaparan & Mahdi, 2013). Each item is scored on a five-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). The subscale scores represent the mean score for questions within that specific domain; higher scores indicate higher patient satisfaction (Marshall & Hays, 1994).
Theoretical Framework
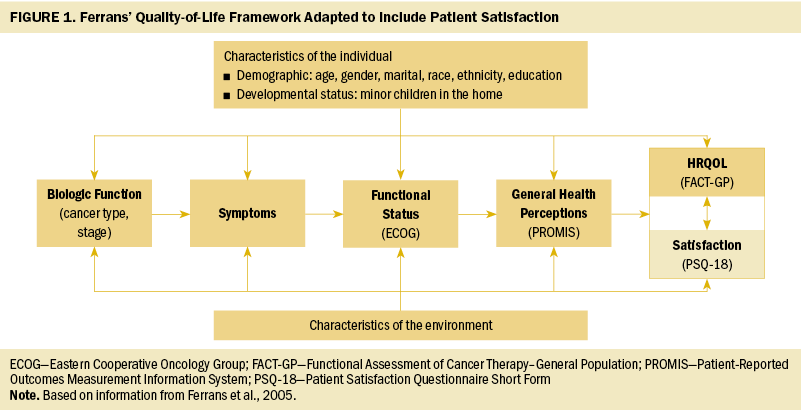
Among published HRQOL models, Ferrans’ conceptual model is one of the most robust (Bakas et al., 2012). This model posits that biologic function, symptoms, functional status, and general health perceptions are key factors influencing HRQOL. Individual and environmental characteristics are overarching themes that affect each factor as well as HRQOL (Ferrans et al., 2005). The current study included patient satisfaction as an outcome variable because of its bidirectional relationship with HRQOL and shared antecedent factors (Brédart et al., 2013). A reduced, modified version of Ferrans’ model using the data from the HR/CSC registry (see Figure 1) was used to examine the role of having minor children on the studied outcomes in patients with cancer.
Statistical Analyses
Descriptive statistics were used to characterize PRO measurements among the study sample. Scores for the FACT-GP, PROMIS Global-10, and PSQ-18 were calculated using standard algorithms. Differences in participant demographic and illness characteristics according to parental status were explored using Fisher’s exact tests for categorical variables and Wilcoxon rank sum tests for continuous variables. For continuous outcome measures, Wilcoxon rank sum tests were used to compare scores between groups. Linear regression models were fit for the outcomes FACT-GP, PROMIS Global-10 Physical Health, and PROMIS Global-10 Mental Health, with p values reported for differences in unadjusted and adjusted models. Because of a skewed distribution in the FACT-GP measure, various transformations were explored; the best transformation was the square transformation, which was used in the linear model analysis. For each PSQ-18 domain, satisfaction was categorized as scoring 3 or higher, indicating agreement with the questionnaire statement. Modified Poisson regression modeling with risk ratio (RR) and 95% confidence interval (CI) was performed to evaluate differences in the likelihood of parents to report satisfaction compared to nonparents. Because of the exploratory nature of this study, adjustments for multiple testing were not included. Analyses were not stratified by age because all models were controlled for age. Analyses were performed using SAS, version 9.3.
Results
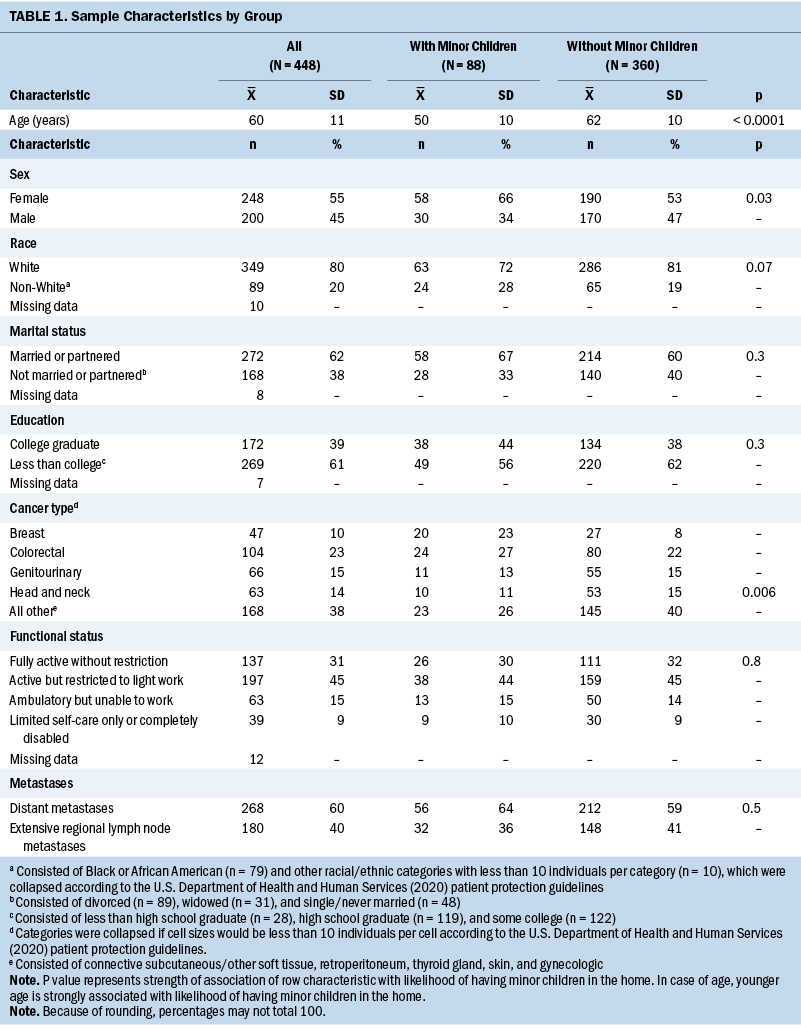
Among the 448 individuals within the HR/CSC with an advanced cancer diagnosis, 19.6% (N = 88) were patients living with minor children. Demographic and disease characteristics of the two groups are presented in Table 1. Patients living with minors were younger (mean = 50 years) than the patients living without minors (mean = 62 years, p < 0.0001). Patients living with minors were also more likely to be female (66%) and identify as White (81%) than patients living without minors (53%, p < 0.02, and 72%, p < 0.003, respectively). There were no significant between-group differences with respect to performance status or proportion of individuals with distant versus regional metastases. Across the entire sample, there was substantial diversity with respect to educational attainment, cancer type, race, and ethnicity. Demographic and clinical characteristics were included in multivariable modeling.
Health-Related Quality of Life and Global Health
Median HRQOL and global health scores for patients with and without minor children are presented in Table 2. Median FACT-GP scores were nearly 10 points lower among patients with minor children (median = 71.7) compared to patients without minor children (median = 81.7, p = 0.0004). Lower FACT-GP scores were reported in patients with minor children in every HRQOL domain. Controlling for age, race, ethnicity, gender, education, marital status, functional status, and extent of metastatic disease, median FACT-GP scores among patients living with minors remained lower compared to patients living without minors (R2 = 37%, p = 0.005). Because of skewed data, adjusted models for FACT-GP subscales were not fit.
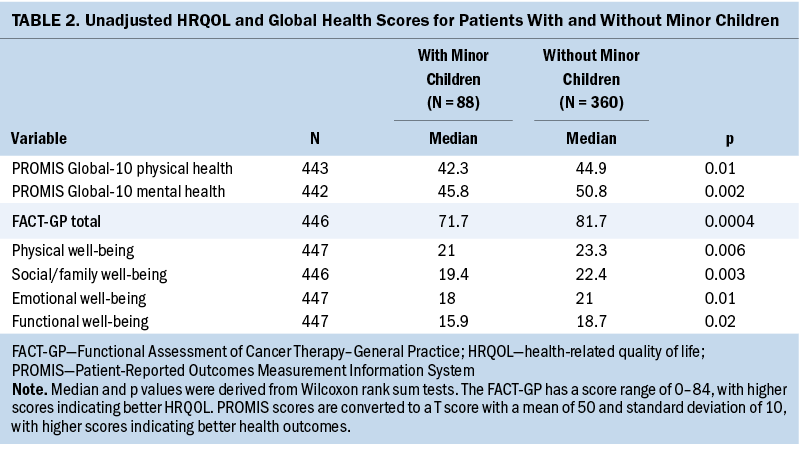
Living with a minor child was also significantly associated with poorer assessment of overall general health. In both adjusted and unadjusted analyses, patients living with minors scored worse on PROMIS Global-10 physical health (adjusted p = 0.01) and mental health (adjusted p = 0.004). These models fit reasonably well with R2 values of 25% and 39%, respectively.
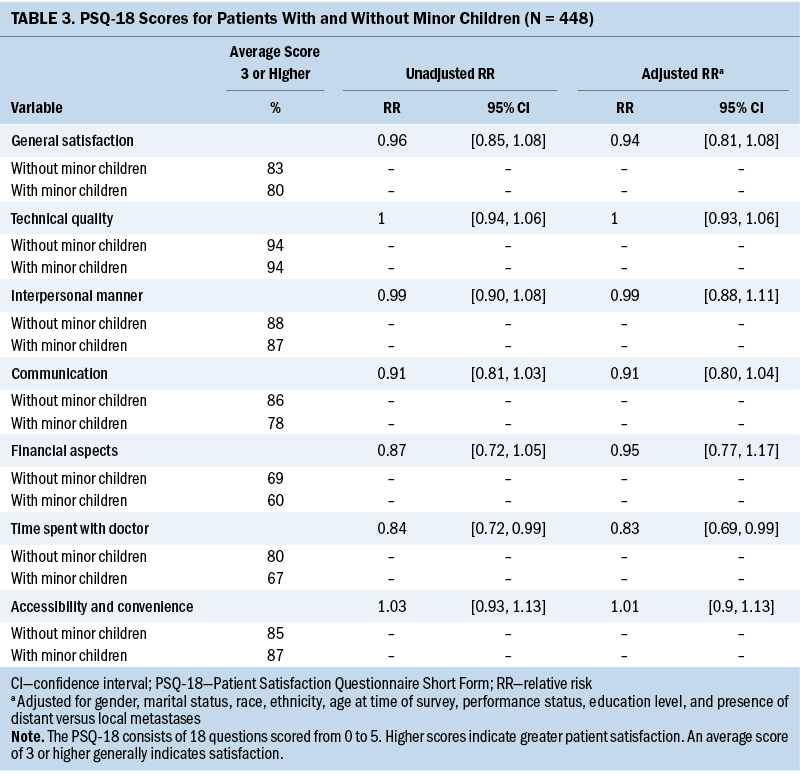
Patient Satisfaction
Patient satisfaction scores are summarized in Table 3. In unadjusted analyses, patients living with minor children were generally less likely to report satisfaction, or scores of higher than 3, in the domains of the PSQ-18. They reported significantly lower satisfaction with time spent with their doctor in both unadjusted (RR = 0.84, 95% CI [0.72, 0.99]) and adjusted analyses. Patients with minor children also reported lower satisfaction with physician communication (RR = 0.91, 95% CI [0.81, 1.03]) and financial aspects (RR = 0.87, 95% CI [0.77, 1.05]) in unadjusted analyses, although these results did not reach statistical significance.
Discussion
PROs offer an opportunity to understand patients’ experiences without requiring providers to interpret their responses. This study sought to use a large, preexisting cohort of individuals to explore the relationships between parental status and several PROs important to patient-centered care in advanced cancer. The results of this study build on existing research and improve understanding of the differences in the cancer experience in patients with minor children.
The results of this study indicated that living with a minor child was associated with clinically important differences in HRQOL and global health, even after adjustment for demographic and illness characteristics. This is consistent with results from a smaller study of patients with cancer, which found that individuals with minor children had worse cognitive and emotional functioning (Ernst et al., 2012). It also corroborates findings from a large cohort study of patients with advanced cancer that revealed worse quality of death or worse final week of life (as reported by their caregivers) among patients with dependent children (Nilsson et al., 2009). The results of the present study suggest these differences occur throughout the disease course, not only before the very end of life. They also affirm the need for earlier identification and support for the psychosocial needs of patients with minor children.
Overall, patients in this study reported high satisfaction with their providers. However, lower satisfaction was reported by patients with minor children, particularly on the subscale of time spent with a doctor. In this study, patients presumably received care by the same providers and had equal access to cancer support resources. Although a direct relationship between patient satisfaction and having minor children cannot be inferred from this study, there may be several possible reasons for this association. It is possible that the presence of minors in the home furthers the complexity of treatment planning for patients with advanced cancer and creates a need for greater communication support within families (Dalton et al., 2019). It is also possible that patients with minors need more time in their clinical encounters to acknowledge and receive support for the profound psychological suffering associated with the risk of early mortality and its impact on young children. In an observational study of 384 women with breast cancer, those with children had greater unmet psychological needs regarding uncertainty about the future, fear of cancer spreading, ability to take care of oneself, and lack of control over treatment outcomes (Brédart et al., 2013). The lower PROMIS mental health scores reported among patients with minors is consistent with prior studies of this population and further underscores the need for greater psychosocial support (Ellis et al., 2009; Park et al., 2018).
There are limitations with cross-sectional study and secondary analyses. Selection of study variables were limited to measures in the HR/CSC database, and data about parenting concerns or ages of minor children were not available. In addition, the patients in this registry reflect the demographics of only one state within the United States. There is also the potential for unmeasured confounding. Controlling for age in all statistical analyses may not fully account for the life disruptions that serious illness causes in younger adults with cancer (Kazak et al., 2010; Smith et al., 2013). Other unmeasured factors, such as health insurance status or household income, may also confound results. Analyses by specific cancer types or subcategories of education could provide more nuanced understanding of these results.
Notable strengths of this study are a large sample size and a diverse population of patients across multiple socioeconomic domains. Data from the HR/CSC were derived from the only public comprehensive cancer center in North Carolina, which provides care for all patients regardless of their ability to pay. Data from many patients with a broad range of cancer types were included in the initial query. Although the dataset did not include household income, it was able to control for educational level, which is frequently used as a stable indicator of lifetime socioeconomic status and is highly correlated with income in most populations of patients with cancer (Cella et al., 1991; Krieger et al., 1997). In addition, the difference in overall HRQOL scores exceeded the MCID for the FACT-GP scale and remained clinically significant in adjusted analyses. Measures of illness severity, such as functional status, FACT-GP physical well-being scores, and extent of metastases, were similar between groups, suggesting that HRQOL differences are unlikely to be attributable to differences in physical symptom burden.
These results support recommendations in the United States and globally that psychosocial care should be a standard component of treatment for oncology patients (Coleman et al., 2008). These recommendations may be particularly salient for patients with advanced cancer and minor children. Parents with advanced cancer commonly report concerns about the impact of their illness and potential death on their children, the availability and capacity of other adult caregivers, and whether and how to share prognostic information with their children (Park et al., 2017, 2021; Turner et al., 2007). These concerns can require nuanced and emotionally charged conversations with skilled clinicians and may indicate a gap in clinical oncology and psycho-oncology services. Communication workshops for healthcare professionals and other members of the community on how to communicate with children about a life-threatening illness could increase parent satisfaction with their care and self-efficacy in navigating these conversations (Dalton et al., 2019). Interventions to promote these communication skills may be particularly relevant for nurses because of the field’s emphasis on patient-centered care. For example, in Sweden, where law mandates that clinicians consider the needs of children of seriously ill parents, the Swedish Society of Nursing recommends that nurses initiate such discussions with patients and their families (Eklund et al., 2020). Although these guidelines do not reflect standardized practice across most Western countries, institutions can implement strategies to proactively engage seriously ill parents with comprehensive psychosocial services. Individuals with minor children can be identified at the beginning of their cancer treatment to facilitate specialty referral to psycho-oncology, palliative care, or child life specialists. Interventions addressing parenting concerns could potentially reduce parents’ anxiety, improve family communication, and lead to enhanced satisfaction with care and well-being. Given the link between parental coping in cancer and their children’s emotional adjustment, improving parental well-being could lead to improved outcomes for their children as well (Visser et al., 2004).
As an exploratory, hypothesis-generating study, adjustments for multiple tests were not reported. However, the parameter estimates of the linear regression models can facilitate future research on this topic. Studies that assess parents’ expectations of how their providers address parenting concerns could help explain the differences identified in this study. Another potential area of interest would be to examine whether the number and age of minor children affect patients’ concerns and outcomes. Future interventions aimed at addressing parenting needs for patients with cancer could include patient satisfaction as a potential outcome of interest.
Implications for Nurses
Achieving patient-centered cancer care for patients with minors heavily relies on nursing support. Oncology nurses’ multiple roles in cancer care delivery can facilitate interprofessional strategies for treatment needed to support parenting concerns (Ferrell et al., 2013). Nursing assessments offer unique opportunities to recognize and validate patients’ parenting concerns, and nursing care plans could integrate parent- or child-specific interventions to improve family coping and support (McFarlane & Bennett, 2006). Enhancing nurses’ awareness of the psychosocial needs of patients with minors may help mitigate the negative impact on their HRQOL and satisfaction with care.
Conclusion
Understanding the patient experience is an essential component of patient-centered care. This study suggests that patients with advanced cancer and minor children have unique needs that may not be fully addressed by the current cancer care system.
The authors gratefully acknowledge the University of North Carolina Health Registry/Cancer Survivorship Cohort participants for their important contributions.
About the Authors
Stephanie A. Chien, BS, is a medical student in the Department of Psychiatry in the School of Medicine, Allison M. Deal, MS, is a biostatistician and Hillary M. Heiling, MS, is a graduate research assistant, both in the Lineberger Comprehensive Cancer Center, and Justin L. Gettings, MD, is a psychiatrist in the Department of Psychiatry in the School of Medicine, all at the University of North Carolina at Chapel Hill; Yue Wang, PhD, is an assistant professor of statistics in the School of Mathematical and Natural Sciences at Arizona State University in Phoenix; Laura Farnan, MD, PhD, is a biostatistician in the Lineberger Comprehensive Cancer Center at the University of North Carolina at Chapel Hill; Jeannette T. Bensen, MS, PhD, is an associate professor in the Department of Epidemiology in the Gillings School of Global Public Health, director of the University of North Carolina Health Registry/ Cancer Survivorship Cohort, and co-director of the Prostate Cancer Consortium at the Lineberger Comprehensive Cancer Center, all at the University of North Carolina at Chapel Hill; Adrian Gerstel, BA, is a project manager in the Lineberger Comprehensive Cancer Center at the University of North Carolina at Chapel Hill; Deborah K. Mayer, PhD, RN, AOCN®, FAAN, is the Francis Hill Fox Distinguished Professor in the School of Nursing and director of Cancer Survivorship in the Lineberger Comprehensive Cancer Center, both at the University of North Carolina at Chapel Hill; Kate E. Stanton, MPH, is a study coordinator and Courtney A. Nelson, MS, BS, is a research assistant, both in the Department of Psychiatry at the University of North Carolina at Chapel Hill; Laura J. Quillen, BS, is a medical student in the Health Science Center at the University of Tennessee in Memphis; and Eliza M. Park, MD, MSc, is an assistant professor in the Department of Psychiatry, the Lineberger Comprehensive Cancer Center, and the Department of Medicine, all at the University of North Carolina at Chapel Hill. The project was supported by the National Institutes of Health through Grant Award Number 5K07CA218167 (Park), the Doris Duke Charitable Foundation through Grant Award Number 2015213 (Park), and the University of North Carolina Lineberger Comprehensive Cancer Center’s University Cancer Research Fund. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Mayer holds stock in Carevive. Park has received honoraria from UpToDate. Deal, Gettings, Mayer, Stanton, Quillen, and Park contributed to the conceptualization and design. Farnan, Bensen, and Quillen completed the data collection. Deal, Heiling, Wang, Farnan, and Bensen provided statistical support. Chien, Deal, Heiling, Gettings, Wang, Farnan, Mayer, and Park provided the analysis. Chien, Deal, Heiling, Gettings, Farnan, Bensen, Gerstel, Mayer, Nelson, and Park contributed to the manuscript preparation. Park can be reached at leeza_park@med.unc.edu, with copy to ONFEditor@ons .org. (Submitted June 2021. Accepted February 13, 2022.)
References
Adonizio, C.S., Weeder, J., Benner, E., Manikowski, J., Hergenrather, J., Wojtowicz, M., & Woods, J.I. (2019). QOL assessment integrated into the clinical care of cancer survivors to identify needs and direct care. Journal of Clinical Oncology, 37(15, Suppl.), 6611–6611. https://doi.org/10.1200/JCO.2019.37.15_suppl.6611
Bakas, T., McLennon, S.M., Carpenter, J.S., Buelow, J.M., Otte, J.L., Hanna, K.M., . . . Welch, J.L. (2012). Systematic review of health-related quality of life models. Health and Quality of Life Outcomes, 10, 134. https://doi.org/10.1186/1477-7525-10-134
Bitar, R., Bezjak, A., Mah, K., Loblaw, D.A., Gotowiec, A.P., & Devins, G.M. (2004). Does tumor status influence cancer patients’ satisfaction with the doctor-patient interaction? Supportive Care in Cancer, 12(1), 34–40. https://doi.org/10.1007/s00520-003-0534-9
Brédart, A., Kop, J.-L., Griesser, A.-C., Fiszer, C., Zaman, K., Panes-Ruedin, B., . . . Dolbeault, S. (2013). Assessment of needs, health-related quality of life, and satisfaction with care in breast cancer patients to better target supportive care. Annals of Oncology, 24(8), 2151–2158. https://doi.org/10.1093/annonc/mdt128
Cella, D.F., Orav, E.J., Kornblith, A.B., Holland, J.C., Silberfarb, P.M., Lee, K.W., . . . Maurer, L.H. (1991). Socioeconomic status and cancer survival. Journal of Clinical Oncology, 9(8), 1500–1509. https://doi.org/10.1200/jco.1991.9.8.1500
Coleman, M.P., Alexe, D.M., Albreht, T., & McKee, M. (Eds.) (2008). Responding to the challenge of cancer in Europe. Institute of Public Health of the Republic of Slovenia.
Dalton, L., Rapa, E., Ziebland, S., Rochat, T., Kelly, B., Hanington, L., . . . Stein, A. (2019). Communication with children and adolescents about the diagnosis of a life-threatening condition in their parent. Lancet, 393(10176), 1164–1176. https://doi.org/10.1016/S0140-6736(18)33202-1
Doll, K.M., Kalinowski, A.K., Snavely, A.C., Irwin, D.E., Bensen, J.T., Bae-Jump, V.L., . . . Gehrig, P.A. (2015). Obesity is associated with worse quality of life in women with gynecologic malignancies: An opportunity to improve patient-centered outcomes. Cancer, 121(3), 395–402. https://doi.org/10.1002/cncr.29061
Eklund, R., Kreicbergs, U., Alvariza, A., & Lövgren, M. (2020). Children’s self-reports about illness-related information and family communication when a parent has a life-threatening illness. Journal of Family Nursing, 26(2), 102–110. https://doi.org/10.1177/1074840719898192
Ellis, J., Lin, J., Walsh, A., Lo, C., Shepherd, F.A., Moore, M., . . . Rodin, G. (2009). Predictors of referral for specialized psychosocial oncology care in patients with metastatic cancer: The contributions of age, distress, and marital status. Journal of Clinical Oncology, 27(5), 699–705. https://doi.org/10.1200/jco.2007.15.4864
Ernst, J., Götze, H., Brähler, E., Körner, A., & Hinz, A. (2012). Quality of life of parents diagnosed with cancer: Change over time and influencing factors. European Journal of Cancer Care, 21(4), 535–541. https://doi.org/10.1111/j.1365-2354.2012.01330.x
Ferrans, C.E., Zerwic, J.J., Wilbur, J.E., & Larson, J.L. (2005). Conceptual model of health-related quality of life. Journal of Nursing Scholarship, 37(4), 336–342. https://doi.org/10.1111/j.1547-5069.2005.00058.x
Ferrell, B., McCabe, M.S., & Levit, L. (2013). The Institute of Medicine report on high-quality cancer care: Implications for oncology nursing. Oncology Nursing Forum, 40(6), 603–609. https://doi.org/10.1188/13.onf.603-609
Hays, R.D., Bjorner, J.B., Revicki, D.A., Spritzer, K.L., & Cella, D. (2009). Development of physical and mental health summary scores from the Patient-Reported Outcomes Measurement Information System (PROMIS) global items. Quality of Life Research, 18(7), 873–880. https://doi.org/10.1007/s11136-009-9496-9
Janda, M., DiSipio, T., Hurst, C., Cella, D., & Newman, B. (2009). The Queensland Cancer Risk Study: General population norms for the Functional Assessment of Cancer Therapy–General (FACT-G). Psycho-Oncology, 18(6), 606–614. https://doi.org/10.1002/pon.1428
Jordhøy, M.S., Fayers, P., Loge, J.H., Saltnes, T., Ahlner-Elmqvist, M., & Kaasa, S. (2001). Quality of life in advanced cancer patients: The impact of sociodemographic and medical characteristics. British Journal of Cancer, 85(10), 1478–1485. https://doi.org/10.1054/bjoc.2001.2116
Kazak, A.E., DeRosa, B.W., Schwartz, L.A., Hobbie, W., Carlson, C., Ittenbach, R.F., . . . Ginsberg, J.P. (2010). Psychological outcomes and health beliefs in adolescent and young adult survivors of childhood cancer and controls. Journal of Clinical Oncology, 28(12), 2002–2007. https://doi.org/10.1200/jco.2009.25.9564
Kleeberg, U.R., Tews, J.-T., Ruprecht, T., Höing, M., Kuhlmann, A., & Runge, C. (2005). Patient satisfaction and quality of life in cancer outpatients: Results of the PASQOC* study. Supportive Care in Cancer, 13(5), 303–310. https://doi.org/10.1007/s00520-004-0727-x
Krieger, N., Williams, D.R., & Moss, N.E. (1997). Measuring social class in US public health research: Concepts, methodologies, and guidelines. Annual Review of Public Health, 18, 341–378. https://doi.org/10.1146/annurev.publhealth.18.1.341
Kypriotakis, G., Vidrine, D.J., Francis, L.E., & Rose, J.H. (2016). The longitudinal relationship between quality of life and survival in advanced stage cancer. Psycho-Oncology, 25(2), 225–231. https://doi.org/10.1002/pon.3846
Lis, C.G., Rodeghier, M., & Gupta, D. (2009). Distribution and determinants of patient satisfaction in oncology: A review of the literature. Patient Preference and Adherence, 3, 287. https://doi.org/10.2147/ppa.s6351
Marshall, G.N., & Hays, R.D. (1994). The patient satisfaction questionnaire short form (PSQ-18). RAND Corporation. https://www.rand.org/pubs/papers/P7865.html
McFarlane, S., & Bennett, C. (2006). Redefining the primary nurse role in oncology care: A 21st century perspective. Canadian Oncology Nursing Journal, 16(2), 99–103. https://doi.org/10.5737/1181912x16299103
Moore, C.W., Rauch, P.K., Baer, L., Pirl, W.F., & Muriel, A.C. (2015). Parenting changes in adults with cancer. Cancer, 121(19), 3551–3557. https://doi.org/10.1002/cncr.29525
Muriel, A.C., Moore, C.W., Baer, L., Park, E.R., Kornblith, A.B., Pirl, W., . . . Rauch, P.K. (2012). Measuring psychosocial distress and parenting concerns among adults with cancer: The Parenting Concerns Questionnaire. Cancer, 118(22), 5671–5678. https://doi.org/10.1002/cncr.27572
Nelson, C.A., Stanton, K.E., Bowers, S.M., & Park, E.M. (2020). Addressing child custody concerns of parents with life-limiting illness. Journal of Palliative Medicine, 23(8), 1134–1138. https://doi.org/10.1089/jpm.2019.0293
Nilsson, M.E., Maciejewski, P.K., Zhang, B., Wright, A.A., Trice, E.D., Muriel, A.C., . . . Prigerson, H.G. (2009). Mental health, treatment preferences, advance care planning, location, and quality of death in advanced cancer patients with dependent children. Cancer, 115(2), 399–409. https://doi.org/10.1002/cncr.24002
Oláh, L.S. (2015). Changing families in the European Union: Trends and policy implication. United Nations Expert Group Meeting, NY, United States.
Park, E.M., Check, D.K., Song, M.-K., Reeder-Hayes, K.E., Hanson, L.C., Yopp, J.M., . . . Mayer, D.K. (2017). Parenting while living with advanced cancer: A qualitative study. Palliative Medicine, 31(3), 231–238. https://doi.org/10.1177/0269216316661686
Park, E.M., Deal, A.M., Check, D.K., Hanson, L.C., Reeder-Hayes, K.E., Mayer, D.K., . . . Rosenstein, D.L. (2016). Parenting concerns, quality of life, and psychological distress in patients with advanced cancer. Psycho-Oncology, 25(8), 942–948. https://doi.org/10.1002/pon.3935
Park, E.M., Deal, A.M., Yopp, J.M., Edwards, T., Resnick, S.J., Song, M.-K., . . . Rosenstein, D.L. (2018). Understanding health-related quality of life in adult women with metastatic cancer who have dependent children. Cancer, 124(12), 2629–2636. https://doi.org/10.1002/cncr.31330
Park, E.M., Wang, M., Bowers, S.M., Muriel, A.C., Rauch, P.K., Edwards, T., . . . Song, M.-K. (2021). Adaptation and psychometric evaluation of the parenting concerns questionnaire—Advanced disease. American Journal of Hospice and Palliative Medicine, 39(8), 918–925. https://doi.org/10.1177/10499091211049801
Pergolotti, M., Deal, A.M., Williams, G.R., Bryant, A.L., Bensen, J.T., Muss, H.B., & Reeve, B.B. (2017). Activities, function, and health-related quality of life (HRQOL) of older adults with cancer. Journal of Geriatric Oncology, 8(4), 249–254. https://doi.org/10.1016/j.jgo.2017.02.009
Schmitt, F., Piha, J., Helenius, H., Baldus, C., Kienbacher, C., Steck, B., . . . Romer, G. (2008). Multinational study of cancer patients and their children: Factors associated with family functioning. Journal of Clinical Oncology, 26(36), 5877–5883. https://doi.org/10.1200/jco.2007.12.8132
Sinclair, M., Schofield, P., Turner, J., Rauch, P., Wakefield, C., Mann, G.B., . . . Stafford, L. (2019). Maternal breast cancer and communicating with children: A qualitative exploration of what resources mothers want and what health professionals provide. European Journal of Cancer Care, 28(6), e13153. https://doi.org/10.1111/ecc.13153
Smith, A.W., Bellizzi, K.M., Keegan, T.H., Zebrack, B., Chen, V.W., Neale, A.V., . . . Lynch, C.F. (2013). Health-related quality of life of adolescent and young adult patients with cancer in the United States: The Adolescent and Young Adult Health Outcomes and Patient Experience study. Journal of Clinical Oncology, 31(17), 2136–2145. https://doi.org/10.1200/jco.2012.47.3173
Smitherman, A.B., Anderson, C., Lund, J.L., Bensen, J.T., Rosenstein, D.L., & Nichols, H.B. (2018). Frailty and comorbidities among survivors of adolescent and young adult cancer: A cross-sectional examination of a hospital-based survivorship cohort. Journal of Adolescent and Young Adult Oncology, 7(3), 374–383. https://doi.org/10.1089/jayao.2017.0103
Tarakeshwar, N., Vanderwerker, L.C., Paulk, E., Pearce, M.J., Kasl, S.V., & Prigerson, H.G. (2006). Religious coping is associated with the quality of life of patients with advanced cancer. Journal of Palliative Medicine, 9(3), 646–657. https://doi.org/10.1089/jpm.2006.9.646
Taylor, P., Passel, J., Wang, W., & Velasco, G. (2011). For millennials, parenthood trumps marriage. Pew Research Center. https://www.pewresearch.org/wp-content/uploads/sites/3/2011/03/millenni…
Thayaparan, A.J., & Mahdi, E. (2013). The Patient Satisfaction Questionnaire Short Form (PSQ-18) as an adaptable, reliable, and validated tool for use in various settings. Medical Education Online, 18(1), 21747. https://doi.org/10.3402/meo.v18i0.21747
Turner, J., Clavarino, A., Yates, P., Hargraves, M., Connors, V., & Hausmann, S. (2007). Development of a resource for parents with advanced cancer: What do parents want?. Palliative and Supportive Care, 5(2), 135–145. https://doi.org/10.1017/s1478951507070204
University of North Carolina. (2014). For researchers—Interviews and questionnaires. https://unchealthregistry.com/ForResearchersInterview.php
U.S. Department of Health and Human Services. (2020). CMS cell suppression policy. https://www.hhs.gov/guidance/document/cms-cell-suppression-policy
van Roij, J., Fransen, H., van de Poll-Franse, L., Zijlstra, M., & Raijmakers, N. (2018). Measuring health-related quality of life in patients with advanced cancer: A systematic review of self-administered measurement instruments. Quality of Life Research, 27(8), 1937–1955. https://doi.org/10.1007/s11136-018-1809-4
Visser, A., Huizinga, G.A., van der Graaf, W.T.A., Hoekstra, H.J., & Hoekstra-Weebers, J.E.H.M. (2004). The impact of parental cancer on children and the family: A review of the literature. Cancer Treatment Reviews, 30(8), 683–694. https://doi.org/10.1016/j.ctrv.2004.06.001
Walker, M.S., Ristvedt, S.L., & Haughey, B.H. (2003). Patient care in multidisciplinary cancer clinics: Does attention to psychosocial needs predict patient satisfaction? Psycho-Oncology, 12(3), 291–300. https://doi.org/10.1002/pon.651
Warsame, R., & D’Souza, A. (2019). Patient reported outcomes have arrived: A practical overview for clinicians in using patient reported outcomes in oncology. Mayo Clinic Proceedings, 94(11), 2291–2301. https://doi.org/10.1016/j.mayocp.2019.04.005
Webster, K., Cella, D., & Yost, K. (2003). The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: Properties, applications, and interpretation. Health and Quality of Life Outcomes, 1, 79. https://doi.org/10.1186/1477-7525-1-79
Wolf, D.M., Lehman, L., Quinlin, R., Zullo, T., & Hoffman, L. (2008). Effect of patient-centered care on patient satisfaction and quality of care. Journal of Nursing Care Quality, 23(4), 316–321. https://doi.org/10.1097/01.ncq.0000336672.02725.a5
Yost, K.J., Eton, D.T., Garcia, S.F., & Cella, D. (2011). Minimally important differences were estimated for six Patient-Reported Outcomes Measurement Information System-Cancer scales in advanced-stage cancer patients. Journal of Clinical Epidemiology, 64(5), 507–516. https://doi.org/10.1016/j.jclinepi.2010.11.018


