A Brief Screening Tool for Assessment of Financial Toxicity
Objectives: To explore the utility of brief financial screening items to facilitate the implementation of routine financial toxicity screening.
Sample & Setting: 50 women with breast cancer completed a one-time survey that included the Comprehensive Score for Financial Toxicity (COST): A FACIT Measure of Financial Toxicity, a visual analog scale, and a brief sociodemographic questionnaire.
Methods & Variables: Survey responses were examined to assess the psychometric properties of individual COST items and the visual analog scale by calculating Cronbach’s alpha and Pearson’s correlation coefficients.
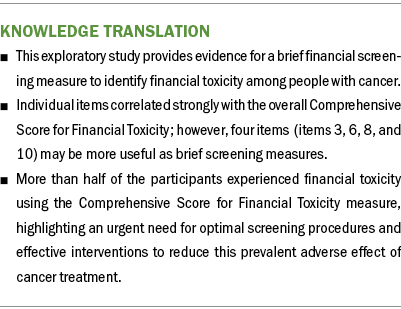
Results: The mean COST was 21.4, and 27 respondents met criteria for financial toxicity (a COST lower than 22). As expected, all items correlated strongly to the overall COST, but four items (items 3, 6, 8, and 10) performed strongest (r > 0.8).
Implications for Nursing: This study provides evidence for individual COST items to be used as brief screening items. Future research should test the utility of these items in larger sample sizes with a more diverse representation of patients by age, race, ethnicity, and tumor type and stage.
Jump to a section
Financial toxicity (Zafar et al., 2013) is the negative personal financial impact of cancer care and involves concrete or material burden, psychological impact, and coping behaviors in response to the impact of these costs (Tucker-Seeley & Thorpe, 2019). It is a prevalent and devastating adverse effect of cancer care and is associated with earlier mortality and poor quality of life (Ramsey et al., 2016). Interventions such as financial navigation and financial education may reduce or mitigate financial toxicity (Watabayashi et al., 2020). As interventions are being developed, accurate measurement and identification of financial toxicity is imperative to effectively evaluate the impact of such interventions. To date, most patients with cancer are at risk for financial toxicity during treatment and into survivorship (Banegas et al., 2016; Smith et al., 2019). Therefore, intermittent and standardized screenings, paired with appropriate follow-up and interventions, are critical to financial toxicity mitigation.
The Comprehensive Score for Financial Toxicity (COST): A FACIT Measure of Financial Toxicity is a reliable and valid patient-reported outcome measure of financial toxicity for adult patients with cancer (de Souza et al., 2014, 2017). Since its inception, it has been used as an outcome measure in research studies (de Souza et al., 2016; Pangestu & Rencz, 2023), but there are limited data to support thresholds for financial interventions or to establish an abbreviated version that clinicians perceive as feasible to implement in a clinical setting (Beauchemin et al., 2023). Routine screening for financial toxicity is recommended in pediatric and adult oncology settings (Meropol et al., 2009; Pelletier & Bona, 2015) because it may help to identify patients at risk for a financial crisis, such as bankruptcy or an inability to afford food or medication. Similar to other guideline-recommended screening measures that have been implemented into oncology clinical settings (Donovan et al., 2019), a brief measure of financial toxicity is needed. This article explores the utility of abbreviated financial screening items to facilitate the implementation of routine financial toxicity screening.
Methods
The current authors conducted a larger study that implemented systematic financial screening across a breast cancer outpatient setting at a large urban academic cancer center in New York, New York, and that was guided by the Consolidated Framework for Implementation Research (Damschroder et al., 2022). The study assessed stakeholder preferences for a comprehensive process to identify financial toxicity in a busy outpatient oncology clinic (Beauchemin et al., 2023). A key element of the stakeholder input was that the screening instrument should be brief (no more than two items). The current authors then recruited a subset of English-speaking patients aged 18 years or older who were undergoing treatment in the breast cancer outpatient setting. Patients actively receiving treatment were approached for participation in this cross-sectional survey study. The study protocol was approved by the Columbia University Institutional Review Board (AAAT2937), and all patients gave verbal consent. Because of the minimal-risk nature of this cross-sectional survey study, a waiver of consent was approved by the institutional review board. Consenting participants were asked to complete a brief survey in the clinic on paper or on a tablet that submitted results directly to the REDCap database. All paper responses were entered into the REDCap database by the study coordinator.
Survey Measures
The following patient-reported sociodemographic data were collected: age, sex, race, ethnicity, education, health literacy (Morris et al., 2006), work status, household income, number of household residents, and marital status. Financial toxicity was measured by COST (de Souza et al., 2017). COST is an established 11-item measure of financial toxicity among adults with robust psychometric properties (de Souza et al., 2014, 2017). The items are scored on a five-point Likert-type scale ranging from 0 (not at all) to 4 (very much), with negatively worded items reverse scored. The scores are then summed to create a total score ranging from 0 to 44, with lower scores indicating greater financial toxicity. The measure underwent rigorous psychometric testing during initial development among adults with cancer, and internal consistency was excellent, with a Cronbach’s alpha of 0.92. Reliability was also strong, with an intraclass correlation coefficient of 0.8 (95% confidence interval [0.57, 0.92]) using test–retest reliability. Construct validity was confirmed by a Pearson’s correlation between financial toxicity and higher psychological distress (p < 0.001) and between financial toxicity and household income (p < 0.001) (de Souza et al., 2014). Factor analysis identified a single factor accounting for 89% of the variance (de Souza et al., 2017). Participants in the current study also completed a single-item financial distress visual analog scale (VAS) adapted from distress screening tools (Donovan et al., 2019); scores range from 0 to 10, with higher scores indicating a higher level of financial stress within the past seven days. Participants were instructed to consider their level of distress related to finances or money.
Analysis
Descriptive statistics were used to characterize the participants and their financial toxicity scores as a binary outcome. A score of 22 or less indicates high financial toxicity; a score of greater than 22 indicates low financial toxicity (Wheeler et al., 2022). The current study used chi-square tests to examine the association between patient sociodemographic factors and the binary financial toxicity outcome. Because of the limited sample size, multivariable logistic regression models were not conducted.
To explore instrument and item performance for a brief screening tool, the authors conducted two psychometric assessments (Laganà & Prilutsky, 2016). Pearson’s correlation coefficients were calculated between each individual COST item, the VAS, and the total COST. A single item from the COST measure or VAS was expected to be a reliable instrument with moderate to high internal consistency because of prior psychometric assessment of the COST measure and its unidimensionality (de Souza et al., 2017). Validity was assessed by calculating Cronbach’s alpha. The authors expected to demonstrate strong internal consistency between individual items because of their conceptual overlap.
Results
Of the 54 patients who were approached, 50 women with breast cancer consented to participate in the survey between August and November 2021. Half of the surveys (n = 25) were completed in the clinic by respondents using pen and paper, and the other half were completed in the clinic via tablet. Table 1 describes the cohort.
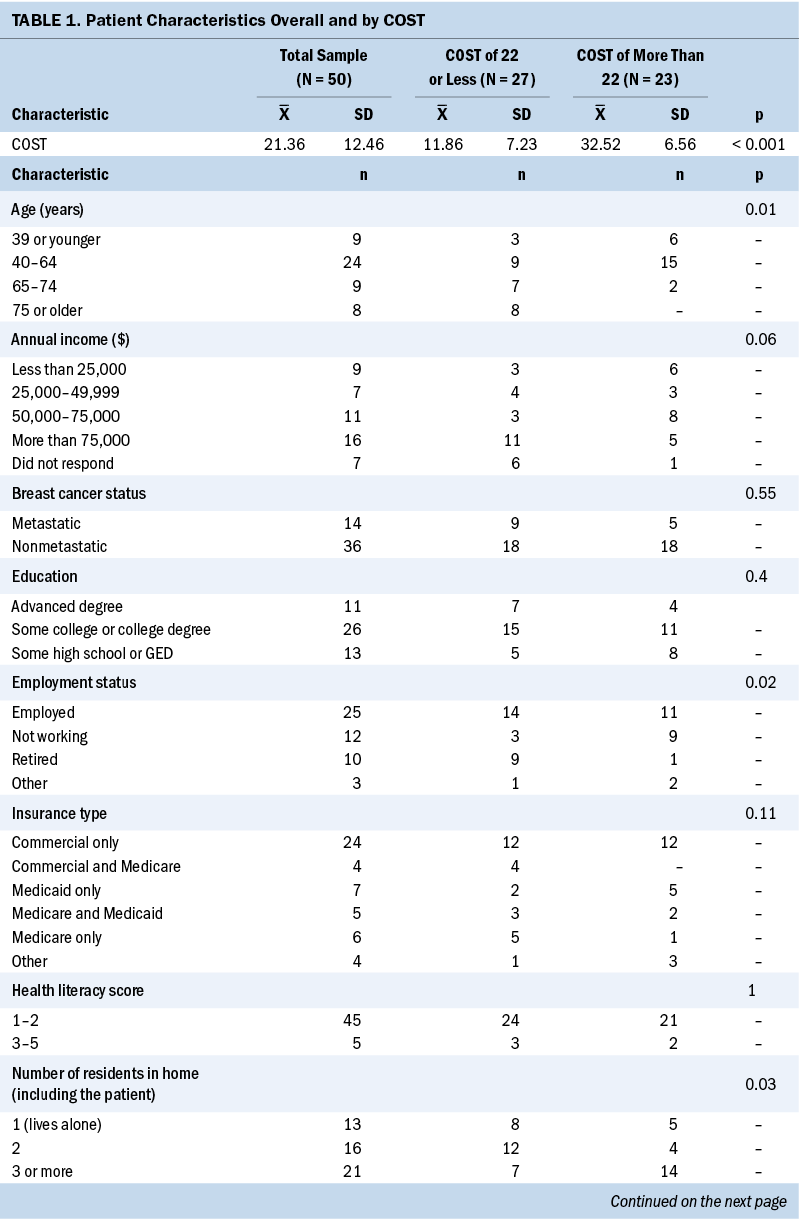
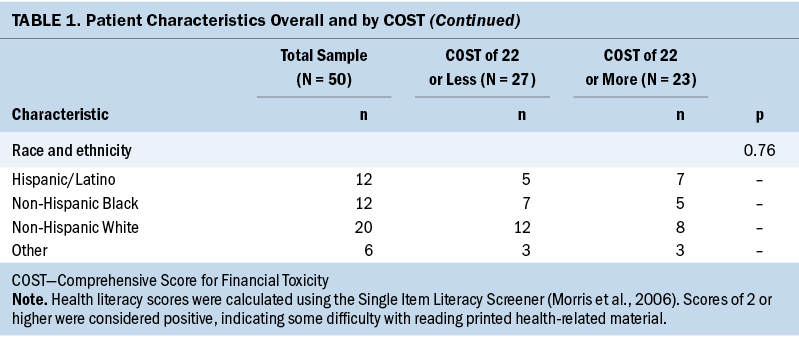
The mean COST for the sample was 21.36 (SD = 12.46); 27 participants met criteria for high financial toxicity (a COST of 22 or less). In univariate analysis, factors associated with high financial toxicity included living alone or with one other person, employment status, and age.
Psychometric Evaluation of Item to Total Scale Correlations
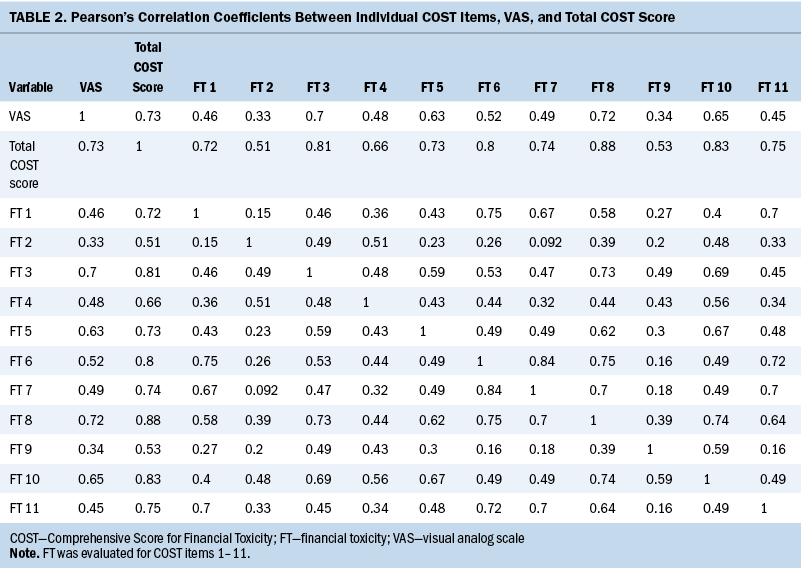
The measure was reliable, with strong internal consistency (Cronbach’s alpha = 0.922), and, expectedly, each COST item was positively correlated with the total COST (see Table 2). Correlation coefficients for individual items ranged from 0.51 (item 2) to 0.88 (item 8). The VAS was strongly correlated to the COST (r = 0.72) but did not perform as well as other COST items. Items 3 (“I worry about the financial problems I will have in the future as a result of my illness or treatment”), 6 (“I am satisfied with my current financial situation”), 8 (“I feel financially stressed”), and 10 (“My cancer or treatment has reduced my satisfaction with my present financial situation”) performed the strongest (r > 0.8).
Discussion
This study explored the utility of brief financial toxicity screening items to facilitate implementation in a busy clinical setting. As expected, the previously validated COST measure of financial toxicity had strong internal consistency and unidimensional factor structure (de Souza et al., 2017). Importantly, four individual screening items from COST may singularly identify financial toxicity.
The financial costs of cancer care affect most patients actively undergoing cancer treatment and those in survivorship (Han et al., 2020; Yabroff et al., 2019). The devastating effects of financial toxicity on health, social, and financial outcomes are well described. As interventions are developed and tested to mitigate this adverse effect of cancer treatment, it is critical that sensitive and specific screening measures are available and implemented. For example, psychosocial distress screening, a process that has been implemented more broadly across cancer clinical settings, is not sensitive or specific enough to accurately identify financial distress (Maldonado et al., 2021). In the current study, a VAS for distress, even when specified to finances, was not as specific as other COST items. This study provides new knowledge that can undergo additional testing in larger studies to discern the optimal brief screening items among a larger sample size using robust psychometric evaluation methods. In addition, more research is needed to understand the optimal screening items among the types of cancer, phases in the cancer continuum, demographic data (e.g., age, sex, gender, zip code), and cultural identities to ensure that screening items are translated, culturally acceptable, and valid for individuals with a primary language other than English (Bradley et al., 2021; Yabroff et al., 2021).
The mode of screening is an important contextual factor. In the current study, half of the respondents preferred to complete the survey using an electronic platform, suggesting a willingness toward digital screening for financial hardship. Electronic data capture can also improve integration with the electronic health record and facilitate linking patients who screen positive for financial toxicity with an intervention (Lambert et al., 2019; Yabroff et al., 2021). However, offering multiple modes of screening is important to promote inclusion and representation among individuals who may not feel comfortable with technology; therefore, additional paper or navigator-supported options are warranted (Beauchemin et al., 2023).
Limitations
The current study provides an important step toward identifying brief screening items for financial toxicity; however, there are limitations. First, this is a small cohort of women with breast cancer, which limits the generalizability. In addition, the authors were underpowered to conduct robust psychometric evaluation. Additional research should include larger sample sizes with adequate representation across patient and clinical characteristics to better discern an optimal screening measure. In addition, the cohort consisted of a majority of non-Hispanic White participants who spoke only English. Patients from underrepresented racial and ethnic groups are more likely to have undermeasured financial hardship because of structural and systemic inequality (Shah et al., 2022). Therefore, the importance of developing and testing brief financial screening tools in racially, ethnically, and clinically diverse populations is paramount because this gap in knowledge exacerbates the knowledge of financial hardship and effective measurement among vulnerable populations. From this study, the authors will take the next step toward testing this brief measure using robust psychometrics and, subsequently, will focus on establishing brief screening tools for individuals with primary languages other than English.
Implications for Nursing
More than half of the participants scored positive for financial toxicity using published cut points (Wheeler et al., 2022). Most participants had completed some college education and nearly half had commercial insurance coverage, highlighting the immense prevalence of financial burden and the lack of understanding for how these scores increase the risk of negative outcomes. Patients have a higher likelihood of experiencing financial toxicity as treatment continues and the time from the initial diagnosis increases (Rotter et al., 2019; Smith et al., 2022), partly because factors such as insurance coverage, as well as income- and health-related social needs, may fluctuate throughout the course of cancer treatment. Therefore, interventions must be tailored to a patient’s clinical and social needs. Nursing research is well positioned to lead this area of inquiry to improve understanding of financial toxicity trajectories and to test and implement patient-informed interventions.
As clinicians on the front line of patient care, nurses are often privy to distressing experiences from the patient perspective, including financial concerns. Awareness of financial toxicity, its prevalence and implications, and potential strategies to mitigate this problem are important to providing high-quality cancer care. However, screening for and addressing financial toxicity requires an interprofessional approach (Smith et al., 2022). Real action will require multilevel modifications involving not only the patient, family, and clinicians, but also the institutional and policy levels to address the upstream causes of financial toxicity, including adverse social determinants of health and structural inequities (Marmot & Allen, 2014).
Conclusion
This study is an important step toward understanding the utility of brief financial screening tools to facilitate the implementation of routine financial toxicity screening. Although all items may identify financial toxicity, specific questions may be more appropriate for certain populations and are important to consider when studying or tailoring a financial screening method for implementation. Additional research is needed to discern an optimal brief screening tool for financial toxicity.
About the Authors
Melissa Beauchemin, PhD, RN, CPNP-PC, CPON®, is the scientific co-lead of cancer care delivery research for the Minority/Underserved National Cancer Institute Community Oncology Research Program in the Herbert Irving Comprehensive Cancer Center and an assistant professor of nursing in the School of Nursing; Rohit Ranjit Raghunathan, MS, is a biostatistician and Alessandra Taboada, BS, is a clinical research coordinator, both in the Herbert Irving Comprehensive Cancer Center; Erik Harden, MA, is the program administrator for the National Cancer Institute Community Oncology Research Program in the Herbert Irving Comprehensive Cancer Center and a breast oncology clinical research manager in the Clinical Protocol and Data Management Office; Samrawit Solomon, BA, is a research associate in the School of Nursing; and Dawn L. Hershman, MD, MS, is an American Cancer Society Professor of Medicine and Epidemiology, the director of breast oncology, and co-leader of the cancer population sciences program in the Herbert Irving Comprehensive Cancer Center, and the interim chief of the Division of Hematology/Oncology in the Department of Medicine, all at Columbia University Irving Medical Center in New York, NY. This research was supported, in part, by the National Cancer Institute and the National Institutes of Health (3P30CA013696-45S2). Beauchemin, Raghunathan, and Hershman contributed to the conceptualization and design and provided the analysis. Beauchemin, Taboada, and Harden completed the data collection. Raghunathan provided statistical support. Beauchemin, Raghunathan, Taboada, Solomon, and Hershman contributed to the manuscript preparation. Beauchemin can be reached at mmp2123@cumc.columbia.edu, with copy to ONFEditor@ons.org. (Submitted June 2023. Accepted October 25, 2023.)
References
Banegas, M.P., Guy, G.P., Jr., de Moor, J.S., Ekwueme, D.U., Virgo, K.S., Kent, E.E., . . . Yabroff, K.R. (2016). For working-age cancer survivors, medical debt and bankruptcy create financial hardships. Health Affairs, 35(1), 54–61. https://doi.org/10.1377/hlthaff.2015.0830
Beauchemin, M.P., DeStephano, D., Raghunathan, R., Harden, E., Accordino, M., Hillyer, G.C., . . . Hershman, D.L. (2023). Implementation of systematic financial screening in an outpatient breast oncology setting. JCO Clinical Cancer Informatics, 7, e2200172. https://doi.org/10.1200/cci.22.00172
Bradley, C.J., Yabroff, K.R., Zafar, S.Y., & Shih, Y.-C.T. (2021). Time to add screening for financial hardship as a quality measure? CA: A Cancer Journal for Clinicians, 71(2), 100–106.
Damschroder, L.J., Reardon, C.M., Widerquist, M.A.O., & Lowery, J. (2022). The updated consolidated framework for implementation research based on user feedback. Implementation Science, 17(1), 75.
de Souza, J.A., Aschebrook-Kilfoy, B., Grogan, R., Yap, B.J., Daugherty, C., & Cella, D. (2016). Grading financial toxicity based upon its impact on health-related quality of life (HRQol). Journal of Clinical Oncology, 34(Suppl. 3), 16. https://doi.org/10.1200/jco.2016.34.3_suppl.16
de Souza, J.A., Yap, B.J., Hlubocky, F.J., Wroblewski, K., Ratain, M.J., Cella, D., & Daugherty, C.K. (2014). The development of a financial toxicity patient-reported outcome in cancer: The COST measure. Cancer, 120(20), 3245–3253. https://doi.org/10.1002/cncr.28814
de Souza, J.A., Yap, B.J., Wroblewski, K., Blinder, V., Araújo, F.S., Hlubocky, F.J., . . . Cella, D. (2017). Measuring financial toxicity as a clinically relevant patient-reported outcome: The validation of the Comprehensive Score for Financial Toxicity (COST). Cancer, 123(3), 476–484.
Donovan, K.A., Deshields, T.L., Corbett, C., & Riba, M.B. (2019). Update on the implementation of NCCN Guidelines for distress management by NCCN member institutions. Journal of the National Comprehensive Cancer Network, 17(10), 1251–1256. https://doi.org/10.6004/jnccn.2019.7358
Han, X., Zhao, J., Zheng, Z., de Moor, J.S., Virgo, K.S., & Yabroff, K.R. (2020). Medical financial hardship intensity and financial sacrifice associated with cancer in the United States. Cancer Epidemiology, Biomarkers and Prevention, 29(2), 308–317.
Laganà, L., & Prilutsky, R.R. (2016). A pilot psychometric study on the validation of the older women’s non-medical stress scale (OWN-MSS) on an ethnically diverse sample. Journal of Geriatrics and Palliative Care, 4(1).
Lambert, C., Legleitner, S., & LaRaia, K. (2019). Technology unlocks untapped potential in a financial navigation program. Oncology Issues, 34(1), 38–45.
Maldonado, J.A., Fu, S., Chen, Y.-S., Acquati, C., Yabroff, K.R., Banegas, M.P., . . . Smith, G.L. (2021). Sensitivity of psychosocial distress screening to identify cancer patients at risk for financial hardship during care delivery. JCO Oncology Practice, 17(12), e1856–e1865. https://doi.org/10.1200/op.20.01009
Marmot, M., & Allen, J.J. (2014). Social determinants of health equity. American Journal of Public Health, 104(Suppl. 4), S517–S519. https://doi.org/10.2105/ajph.2014.302200
Meropol, N.J., Schrag, D., Smith, T.J., Mulvey, T.M., Langdon, R.M., Jr., Blum, D., . . . Schnipper, L.E. (2009). American Society of Clinical Oncology Guidance Statement: The cost of cancer care. Journal of Clinical Oncology, 27(23), 3868–3874. https://doi.org/10.1200/jco.2009.23.1183
Morris, N.S., MacLean, C.D., Chew, L.D., & Littenberg, B. (2006). The Single Item Literacy Screener: Evaluation of a brief instrument to identify limited reading ability. BMC Family Practice, 7, 21. https://doi.org/10.1186/1471-2296-7-21
Pangestu, S., & Rencz, F. (2023). Comprehensive Score for Financial Toxicity and health-related quality of life in patients with cancer and survivors: A systematic review and meta-analysis. Value in Health, 26(2), 300–316.
Pelletier, W., & Bona, K. (2015). Assessment of financial burden as a standard of care in pediatric oncology. Pediatric Blood and Cancer, 62(Suppl. 5), S619–S631.
Ramsey, S.D., Bansal, A., Fedorenko, C.R., Blough, D.K., Overstreet, K.A., Shankaran, V., & Newcomb, P. (2016). Financial insolvency as a risk factor for early mortality among patients with cancer. Journal of Clinical Oncology, 34(9), 980–986. https://doi.org/10.1200/JCO.2015.64.6620
Rotter, J., Spencer, J.C., & Wheeler, S.B. (2019). Financial toxicity in advanced and metastatic cancer: Overburdened and underprepared. Journal of Oncology Practice, 15(4), e300–e307. https://doi.org/10.1200/jop.18.00518
Shah, K., Zafar, S.Y., & Chino, F. (2022). Role of financial toxicity in perpetuating health disparities. Trends in Cancer, 8(4), 266–268. https://doi.org/10.1016/j.trecan.2021.12.007
Smith, G.L., Banegas, M.P., Acquati, C., Chang, S., Chino, F., Conti, R.M., . . . Yabroff, K.R. (2022). Navigating financial toxicity in patients with cancer: A multidisciplinary management approach. CA: A Cancer Journal for Clinicians, 72(5), 437–453.
Smith, G.L., Lopez-Olivo, M.A., Advani, P.G., Ning, M.S., Geng, Y., Giordano, S.H., & Volk, R.J. (2019). Financial burdens of cancer treatment: A systematic review of risk factors and outcomes. Journal of the National Comprehensive Cancer Network, 17(10), 1184–1192. https://doi.org/10.6004/jnccn.2019.7305
Tucker-Seeley, R.D., & Thorpe, R.J., Jr. (2019). Material–psychosocial–behavioral aspects of financial hardship: A conceptual model for cancer prevention. Gerontologist, 59(Suppl. 1), S88–S93. https://doi.org/10.1093/geront/gnz033
Watabayashi, K., Steelquist, J., Overstreet, K.A., Leahy, A., Bradshaw, E., Gallagher, K.D., . . . Shankaran, V. (2020). A pilot study of a comprehensive financial navigation program in patients with cancer and caregivers. Journal of the National Comprehensive Cancer Network, 18(10), 1366–1373.
Wheeler, S.B., Biddell, C.B., Manning, M.L., Gellin, M.S., Padilla, N.R., Spees, L.P., . . . Rosenstein, D.L. (2022). Lessening the Impact of Financial Toxicity (LIFT): A protocol for a multi-site, single-arm trial examining the effect of financial navigation on financial toxicity in adult patients with cancer in rural and non-rural settings. Trials, 23(1), 839.
Yabroff, K.R., Bradley, C.J., & Shih, Y.-C.T. (2021). Improving the process of screening for medical financial hardship in oncology practice. Cancer Epidemiology, Biomarkers and Prevention, 30(4), 593–596. https://doi.org/10.1158/1055-9965.Epi-21-0111
Yabroff, K.R., Zhao, J., Han, X., & Zheng, Z. (2019). Prevalence and correlates of medical financial hardship in the USA. Journal of General Internal Medicine, 34(8), 1494–1502. https://doi.org/10.1007/s11606-019-05002-w
Zafar, S.Y., Peppercorn, J.M., Schrag, D., Taylor, D.H., Goetzinger, A.M., Zhong, X., & Abernethy, A.P. (2013). The financial toxicity of cancer treatment: A pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist, 18(4), 381–390.

