An Integrative Review of Patient Education During Inpatient Hematopoietic Stem Cell Transplantation
Problem Identification: Patients undergoing hematopoietic stem cell transplantation (HSCT) have significant learning needs that nurses must provide. The review question was “What teaching methods and strategies have been examined to deliver education to patients undergoing HSCT?”
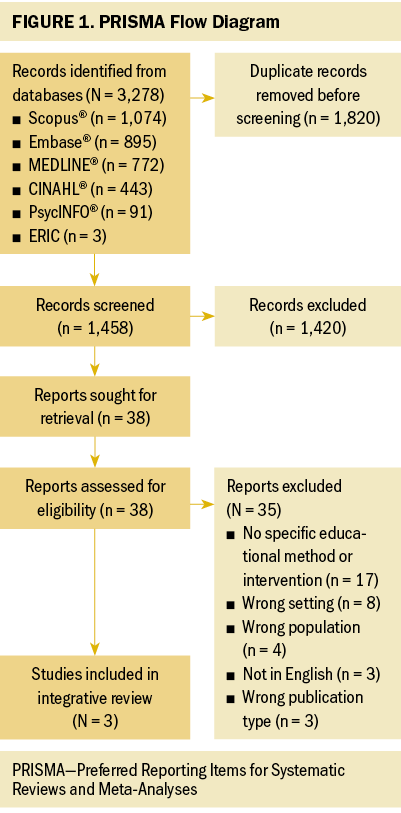
Literature Search: The review was conducted in November 2022 using the following databases: Scopus®, Embase®, MEDLINE®, CINAHL®, PsycINFO®, and ERIC. The search comprised two main concepts: HSCT and patient education.
Data Evaluation: The search yielded 1,458 records after duplicates were removed, and 3 studies were included in this review. The studies were critically appraised using the Mixed Methods Appraisal Tool and deemed to be of moderate quality.
Synthesis: Problem-solving training was the teaching method used in all three studies. Satisfaction was noted among patients and those delivering the intervention. The effect of the training on information retention or application was not measured.
Implications for Practice: Additional research is needed to explore how to best educate patients undergoing HSCT while hospitalized. Structured teaching methods may have a sound theoretical basis and warrant additional investigation using more rigorous research methods.
Jump to a section
Hematopoietic stem cell transplantation (HSCT) is a curative treatment for hematologic malignancies and nonhematologic diseases (Galgano et al., 2023). The process involves high-dose chemotherapy followed by the infusion of a donor’s (allogeneic) or a patient’s own (autologous) stem cells. HSCT involves lengthy hospitalization, significant side effects, and changes to a patient’s ability to care for themselves, and requires lifelong follow-up (de Azevedo et al., 2017; Schoemans et al., 2019). Given that undergoing HSCT is a high-risk and complex process, the patient must understand their treatment to be involved in their care (Schoemans et al., 2019).
Patient Education
Patient education is the process of teaching, counseling, and training the patient on aspects of their care (Strupeit et al., 2013). The delivery of information requires consideration of timing, delivery format, content, and setting (Schoemans et al., 2019). Successful patient education has many positive outcomes. A systematic review by Husson et al. (2011) revealed that survivors of cancer whose informational needs were satisfied had less anxiety, less depression, and better health-related quality of life. Addressing patients’ needs for knowledge can also positively affect their ability to cope and improve their health and treatment-related decision-making (de Azevedo et al., 2017). Patients are expected to have a dedicated caregiver during the HSCT process, and education can shift caregivers from having a passive role to playing an active role in the patient’s care (Bergkvist et al., 2020). As many HSCT centers move to complete more care in the outpatient setting, patients are discharged from the hospital earlier, which creates additional pressure for patients and their families to be prepared for self-management (Schmit-Pokorny et al., 2003).
The intensity of the HSCT process is understood by healthcare providers but is difficult to communicate to patients and their families (Liso et al., 2017). Patients may struggle to understand medical terminology and feel surprised by the impact of the treatment they are undergoing and its need for long-term follow-up (Cohen et al., 2013). In the hospital setting, challenges such as stress, anxiety, depression, and fear, which are prevalent among patients undergoing cancer treatments, increase mental stress, which can negatively affect learning (Inott & Kennedy, 2011). Systemic barriers that affect how nurses teach include time constraints, a lack of preparation to teach, and limited teaching resources (Livne et al., 2017). Nurses may lack the training and ability to accurately assess and often overestimate their patients’ health literacy, leaving these patients at risk for educational gaps (Foster et al., 2016).
Using Theory-Based Interventions in Adult Learning
Theory provides an explanation of how and why phenomena occur (Sidani & Braden, 1997). When developing an intervention, theory can be used to (a) identify and describe the problem of interest, including factors and causes, which can inform the intervention design; (b) describe the anticipated or desired mechanism of change and the outcome of interest in the development of the intervention; and (c) inform the implementation and application of the intervention to target the specific problems, factors, mechanisms of change, and outcomes (Bartholomew & Mullen, 2011). Therefore, interventions guided by theory can be more effective because they are developed using comprehensive knowledge of phenomena, context, outcomes, and implementation factors often explained by the theory (Bartholomew & Mullen, 2011). In addition, outcomes from studies that use theory-guided interventions are more applicable to practice because the intervention was developed for a specific situation or context (Sidani & Braden, 2021).
Numerous adult learning theories exist and reflect varying educational contexts and perspectives. Andragogy, the foundation for adult learning, can be described as the “art and science of helping adults learn” (Knowles, 1980, p. 43). Knowles (1980) characterized adult learners and distinguished their needs and motivations when learning relative to those of children. These principles are important for educators to understand how adults approach learning and gaining knowledge, and the specific needs that may exist. Educational interventions based on adult learning theory provide an avenue to approach the specific needs of learners within complex contexts, such as adults undergoing HSCT.
Review Question
This integrative review explored how nurses can effectively deliver patient education to patients undergoing HSCT. The review question was “What teaching methods and strategies have been examined to deliver education to patients undergoing HSCT?”
Methods
An integrative literature review was done to answer the review question. An integrative review allows for the inclusion of broad data sources including experimental and nonexperimental research, as well as theoretical and empirical literature to fully understand a phenomenon or concern of interest (Whittemore & Knafl, 2005). The integrative review methodology was selected because it enables inclusion of diverse data sources (Toronto & Remington, 2020). The integrative review was conducted using the following six steps outlined by Toronto and Remington (2020): (a) formulation of purpose and review question, (b) literature search and selection, (c) quality appraisal, (d) analysis and synthesis, (e) discussion and conclusion, and (f) dissemination of findings.
Search Methods
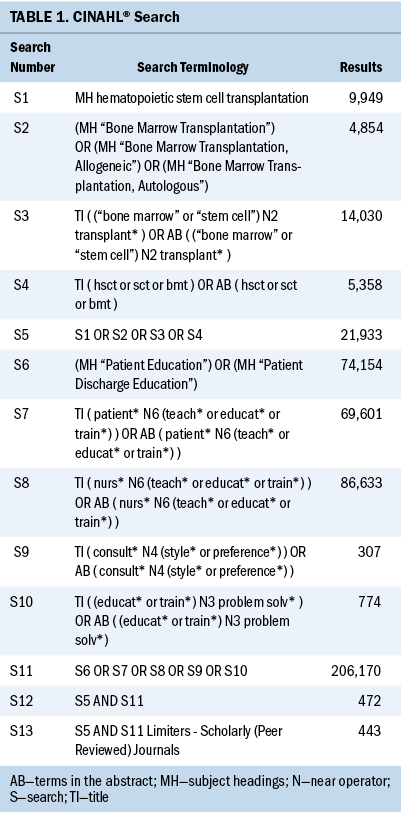
A comprehensive systematic search was developed with guidance from a health sciences research librarian (K.A.H.). The following databases were searched: Scopus®, Embase®, MEDLINE®, CINAHL®, PsycINFO®, and ERIC. The six databases were searched for articles published from the time of the database’s inception to November 22, 2022. The search included two main search categories for keywords and subject headings: HSCT and patient education. Keywords remained constant across the databases; however, subject headings were adapted to each database’s controlled terms. CINAHL search strategies are listed in Table 1. Full search strategies are presented in the appendices. When possible in each database, limitations were applied to the search to include only peer-reviewed sources and to exclude sources of evidence outlined in the exclusion criteria. Covidence software was used for data management of data and the screening process, as well as duplicate removal.
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: Patients underwent autologous or allogeneic HSCT; patients were aged 18 years or older; the teaching occurred in an inpatient setting; the article was published in English; experimental or nonexperimental research was conducted; and a specific teaching approach, method, or intervention was used. The exclusion criteria were as follows: The patient population was not isolated to those who underwent HSCT; patients were aged younger than 18 years; articles did not use a specific teaching method; teaching occurred in an outpatient setting; and content was published as a dissertation, a conference abstract, a book, a chapter in a book, an editorial, or a letter.

Study Selection
Prior to screening, an inter-rater exercise was undertaken, with 50 records randomly selected from the full search results. Inter-rater agreement was 96% between C.B. and K.M.K.-S. and 92% between C.B. and K.S. After this calibration exercise, C.B. first screened the titles and abstracts for all records. K.M.K.-S. and K.S. reviewed half of the title and abstract records. Disagreements in the first level of screening were resolved by discussion between C.B., K.M.K.-S., and K.S. Full-text screening was then independently undertaken by C.B. and K.S., and disagreements were resolved by discussion between C.B., K.M.K.-S., and K.S.
Data Extraction
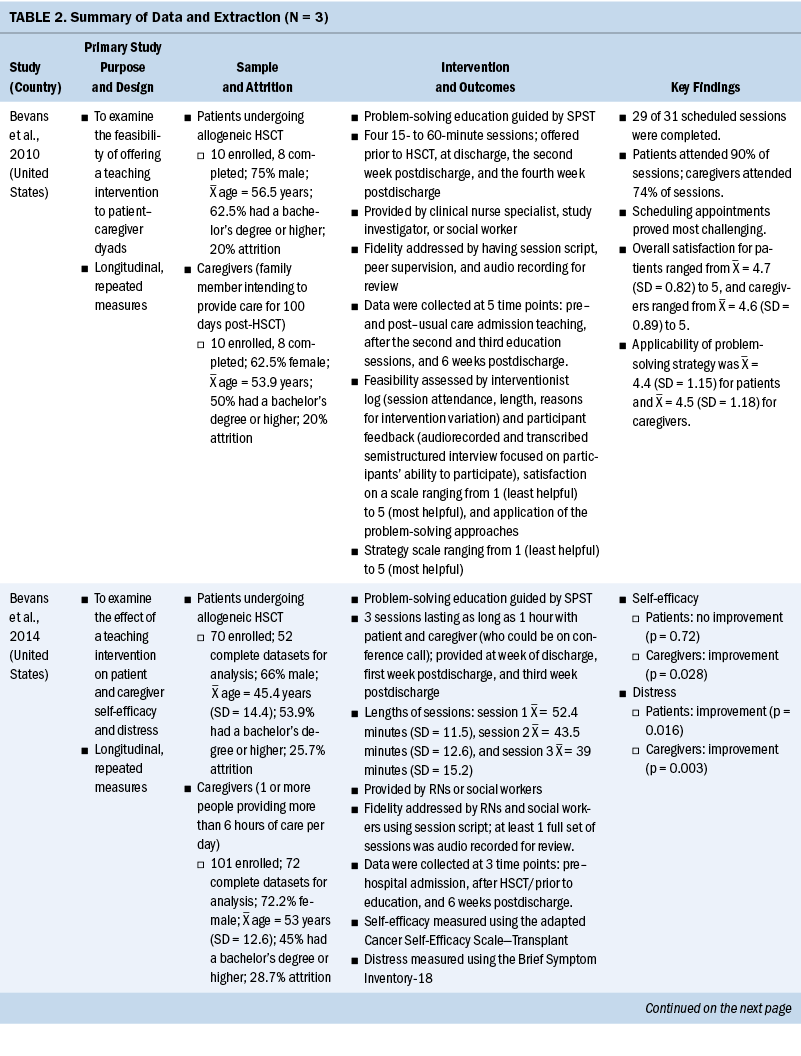
A data extraction table was developed based on the Template for Intervention Description and Replication checklist (Hoffmann et al., 2014) and used to organize data (see Table 2). Data were manually extracted by C.B. and K.M.K.-S. The inclusion of adult learning theory in each study was also assessed and included in the data extraction table.
Critical Appraisal
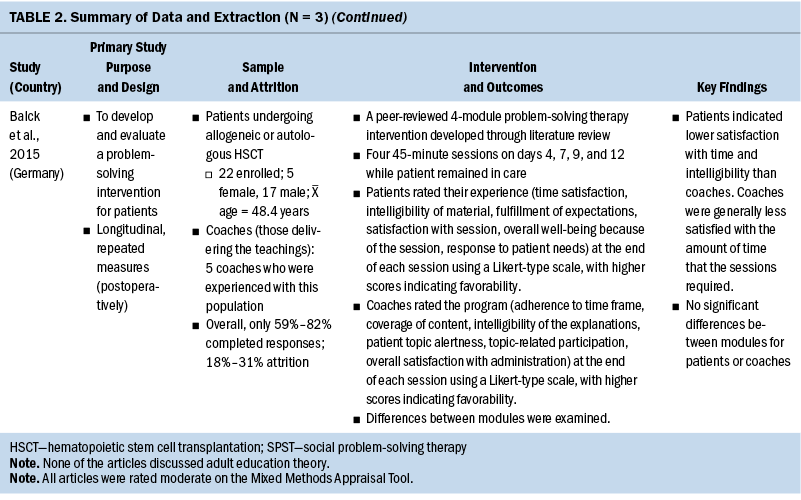
The included studies were appraised using the Mixed Methods Appraisal Tool (Hong et al., 2018), which is a tool for appraising qualitative, quantitative, and mixed-methods studies for reviews including mixed study designs (Hong et al., 2018). Studies were deemed to be of high quality if there were five “yes” answers out of five evaluative questions, moderate quality if there were three to four “yes” answers, and low quality if there were fewer than three “yes” answers. The critical appraisal was undertaken by C.B. and was verified by K.M.K.-S. for all studies. The critical appraisal is outlined in Table 3. Studies were not excluded based on the results of the critical appraisal.
Results
Search Outcomes
The search yielded 3,278 records. After 1,820 records were removed because of duplication, 1,458 records were screened by title and abstract, and 38 articles were included for full-text review. The full-text screening yielded three articles for inclusion in this review. Studies were excluded because they lacked a specific educational method or intervention (n = 17), took place outside of the inpatient setting (n = 8), did not include the correct population (n = 4), were published in a non-English language (n = 3), or were not published in the correct format (n = 3). The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Flow Diagram is represented in Figure 1 (Page et al., 2021).
Study Characteristics
Two of the studies were conducted in the United States, and one in Germany. For two studies, the teaching intervention was delivered to dyads that included a patient undergoing allogenic HSCT and their caregiver (Bevans et al., 2010, 2014). The remaining study delivered teaching to patients undergoing allogeneic or autologous HSCT (Balck et al., 2015). All studies were published in 2010 or later. All three studies used a longitudinal repeated-measures design measuring quantitative data (Balck et al., 2015; Bevans et al., 2010, 2014). The sample sizes were 20 participants (Bevans et al., 2010), 22 participants (Balck et al., 2015), and 171 participants (Bevans et al., 2014). The teaching intervention in all three studies was a problem-solving intervention (Balck et al., 2015; Bevans et al., 2010, 2014); none of the studies based the teaching interventions on adult learning theory.
Problem-Solving Training
The most common educational intervention was a problem-solving therapy (PST) intervention. PST coaches participants to understand the nature of their problems and then directs them to alter or react to their situation (Nezu et al., 1999). The aims of the PST were to prepare patients to implement solutions after discharge (Balck et al., 2015), to empower patients to cope with cancer and cancer treatments (Bevans et al., 2010), and to teach a systematic approach to solve problems that arise from intense treatment (Bevans et al., 2014). The PST intervention was delivered to a patient–caregiver dyad in two studies (Bevans et al., 2010, 2014). Clinicians guided the dyad to identify a problem, review information related to the problem, and then develop a plan to address the problem (Bevans et al., 2010).
Similarly, Balck et al. (2015) used problem-solving guides that were designed for a population of patients with general cancers and adapted to the needs of patients undergoing HSCT. The guides contained the following five problem-solving steps: “(a) problem orientation, (b) problem definition, (c) generation of alternatives, (d) decision-making, and (e) implementation of the selected solution and verifications,” which were implemented in one of four training sessions delivered solely to the patient (Balck et al., 2015, p. 239).
PST was delivered by trained clinical nurse specialists, nurse scientists, or social workers (Bevans et al., 2010), a trained nurse or social worker (Bevans et al., 2014), or a coach (unknown discipline) who had received six hours of training (Balck et al., 2015). The PST interventions were assigned to certain points during the HSCT; however, there was variance between studies regarding when the sessions took place. The intervention in one study took place only in the inpatient setting (Balck et al., 2015), and the interventions in two studies took place in inpatient and outpatient settings (Bevans et al., 2010, 2014). The interventions were delivered as four one-hour sessions pretransplantation, at discharge, two weeks postdischarge, and four weeks postdischarge (Bevans et al., 2010), or as three one-hour sessions during the week of discharge, one week postdischarge, and three weeks postdischarge (Bevans et al., 2014). The interventions in one study took place entirely in the inpatient setting and were delivered as four 45-minute sessions on days 4, 7, 9, and 12 of HSCT (Balck et al., 2015). Bevans et al. (2014) adjusted the intervention based on findings from Bevans et al. (2010). In the study by Bevans et al. (2014), the intervention was reduced from four to three sessions based on feedback from the 2010 pilot study in which patients reported the pretransplantation session as less helpful amid the complex time before hospital admission. Patients were also found to have more than one caregiver by Bevans et al. (2010); therefore, Bevans et al. (2014) included as many as three caregivers per patient.
PST Outcomes
Two of the PST articles were pilot studies with a focus on determining the feasibility of offering the intervention (Balck et al., 2015; Bevans et al., 2010). Feasibility was determined by sufficient participation satisfaction, sufficient attendance (Bevans et al., 2010), and patient and coach satisfaction and intelligibility of the sessions (Balck et al., 2015). Helpfulness of the sessions was measured and deemed to be higher among caregivers than patients (Bevans et al., 2010). The intervention was deemed feasible in the studies (Balck et al., 2015; Bevans et al., 2010).
In the Bevans et al. (2010) pilot study, distress was measured as a secondary outcome. Distress was higher postintervention for patients and lower for caregivers (Bevans et al., 2010). The study’s authors found that participants who had more distress at baseline had improved problem-solving skills after the intervention, suggesting that individuals with more distress may experience more benefits from PST.
In Bevans et al. (2014), the primary outcome of interest was caregiver self-efficacy and distress, although these outcomes were also reported for the patients. The patient–caregiver dyad-directed PST intervention increased caregiver self-efficacy but had no effect on patient self-efficacy. In contrast to the pilot study, the intervention decreased distress among caregivers and patients. Of note, the caregivers who demonstrated less response to the intervention were caring for patients who were deemed to have worse acuity than the patients whose caregivers had more response.
Challenges with delivering PST included scheduling and the length of time required from the healthcare providers to add these sessions to their existing workload (Bevans et al., 2010, 2014). In contrast, some coaches felt that the time frame was limited, so some sessions were not sufficiently covered (Balck et al., 2015). Uncertainty regarding the required dose in contrast to the timing of the sessions remains unknown; however, Bevans et al. (2014) used data from Bevans et al. (2010) to adjust the timing of the sessions.
Critical Appraisal
Overall, the quality of the included studies was moderate. No study had complete outcome data. The lowest attrition rates were 20% (Bevans et al., 2010) and ranged as high as 28.7% (Bevans et al., 2014). The risk of attrition bias represents a threat to the validity of the results and may be a result of small sample sizes. In addition, a lack of account for confounding factors was noted. These limitations are taken with consideration that two of the studies were identified as pilot studies, with the objective of testing intervention feasibility.
Discussion
PST was the only studied teaching approach and was determined to be a possible teaching method for educating patients undergoing HSCT and their caregivers. PST has been used in various settings and populations, largely to address psychological disorders such as anxiety and depression (Nezu et al., 2013). Patients undergoing HSCT experience high anxiety and depression at baseline—issues that are exacerbated during HSCT; therefore, PST is a relevant intervention for this population (Seo et al., 2019).
Whether the intervention was effective in patients acquiring and applying desired learnings was not explored in any of the studies included in this review. This leaves uncertainty about the utility of PST in the acquisition of specific skills and knowledge that patients undergoing HSCT require. Outcomes such as patient-reported distress and self-efficacy were used to assess the effectiveness of PST. Although addressing the psychosocial needs of patients undergoing HSCT is an important aspect of care, measuring how well PST facilitates learning would require evaluating how well the participants retained the content and how they were able to apply it to their lives.
A systematic review across various patient populations by Friedman et al. (2011) revealed that verbal and discussion-based teaching strategies were the least effective. The studies in the review by Friedman et al. (2011) were published between 1995 and 2009, and the applicability of the included methods to current teaching practices may be considered. For example, the use of technology is an emerging patient teaching strategy that has shown efficacy in other medical settings (Halldorsdottir et al., 2020). Advantages exist to verbal teaching because oral instruction can help overcome issues of health literacy (Parnell, 2014). Nevertheless, even recently in a surgical setting, the provision of written information improved recall when compared to verbal information only (Aslam et al., 2023). Of note, in all three of the included studies, there is no documentation of teaching types aside from verbal or discussion. Although PST is a unique teaching strategy, the basis in discussion may present a limitation if patients do not receive other forms of teaching resources such as written, video, lecture, or audiorecorded materials.
The approach used by Bevans et al. (2010) and Bevans et al. (2014) to deliver the training to the patient and caregiver raises consideration for who should be included as the subject of patient teaching. Given how treatment-related distress and effects can negatively affect a patient’s learning, the inclusion of a caregiver presents another consideration when delivering patient education. In the hospital and after discharge, family caregivers are expected to provide complex care to patients, often with little preparation or help (van Ryn et al., 2011). To engage in these patient care activities, caregivers require access to information, training, and support (Northouse et al., 2012). Therefore, involving family in patient education seems to be a sensible consideration to patient teaching. This does add additional workload for nurses who are engaging in patient teaching because they must shift their attention from one learner to two. As additional research emerges regarding the role that caregivers play in patient care outcomes, the inclusion of family caregivers as an extension of the patient requiring education may be appropriate.
Delivering education in the inpatient setting was the focus of this review. Subsequent studies that took place exclusively outside of this setting were not included. This may be relevant because the care of patients undergoing HSCT is shifting toward outpatient care, and care teams must provide more coordinated care along the treatment trajectory (Schmit-Pokorny et al., 2003). Therefore, education is taking place in several settings throughout the HSCT process. This is reflected in this review because the entire intervention was delivered in an inpatient setting in only one study, and the intervention in the other two studies took place within inpatient and outpatient settings. Viewing the care of patients undergoing HSCT on a continuum may prompt additional consideration of coordinated education across inpatient and outpatient settings to ensure that teaching content is aligned and that the teachers use similar techniques to maintain continuity in teaching approaches.
Implementing an individual learning assessment has been found to be a critical component of patient teaching (Friedman et al., 2011). The learning assessment forms the basis of tailoring education to meet the individual patient’s needs, and it should take into consideration certain factors such as literacy, motivation, cultural background, and preferred learning styles (Schoemans et al., 2019). None of the PST interventions included a clear patient assessment prior to starting the intervention; however, a learning assessment may provide greater insight into a patient’s baseline knowledge and motivations regarding the patient-perceived problems targeted by PST. The objective of PST is not to teach patients the solutions to problems, but rather to teach patients problem-solving skills (Lorig & Holman, 2003). Although the steps of PST are structured, the orientation of steps (such as how patients orient and define problems), which solutions would be reasonable and applicable to their circumstance, and what resources or approaches they would undertake to implement solutions are highly personal and may vary among patients. As such, the applicability and helpfulness of the PST instruction to patients may hinge on the values, beliefs, and preferences revealed from the learner’s assessment.
None of the included studies were underpinned by a specific learning theory. Aspects of adult learning theory can be integrated into these teaching opportunities with patients and families. For example, Mezirow’s (2000) transformative learning theory states, “Learning is understood as the process of using a prior interpretation to construe a new or revised interpretation of the meaning of one’s experience as a guide to future action” (p. 5). Similarly, one assumption from Knowles (1980) about adult learners is that adults use previous life experience when acquiring new knowledge. The use of PST can be situated within these adult learning theories and principles because learners may draw from previous life experience to situate their problems and perspectives about possible solutions along with the reflection brought on by the introduction of other possible approaches to their problems.
PST is a structured approach to teaching that is more effective than unstructured or improvised approaches to teaching that, without training on how to effectively teach, nurses may naturally employ (Friedman et al., 2011). Within the principles of andragogy, adult learners seek information that they can apply directly to their lives, and, as such, learning activities should be organized around developing specific and clear competencies (Knowles, 1980). In the context of adult learning, this may represent a shift from informal to nonformal learning, whereby learners use programs or other structured tools to meet specific learning goals (Merriam & Baumgartner, 2020). In contrast, patients may partake in informal learning by observing or conversing with nursing staff during daily activities; however, these encounters lack intention and assessment to ensure that necessary education points were retained. Future interventions may be developed using PST by framing teaching objectives within applicable contexts and problems and using applicable scenarios to work through potential issues that patients would be required to manage.
Strengths and Limitations
One strength of this review is that it included a comprehensive search across several health and teaching databases overseen by a research librarian to ensure that the search was systematic and complete. Given the highly specific review question, the number of included studies was limited. This can be seen as a strength because this review highlights the gap in the evidence base of this topic, and as a limitation because the results lack the strength to make practice recommendations (Slyer, 2016). Likewise, the age of the available studies is also a limitation and reflects the lack of recent evidence. Other limitations are that articles were only included if the full text was available in English and that gray literature was not included in the search. In addition, studies that took place only in outpatient settings were excluded, which may have omitted meaningful methods or strategies for educating patients undergoing HSCT.
Implications for Practice
Because of the few studies on this topic, of which two were pilot studies, it is difficult to translate results into recommendations for nursing practice. This review highlights that there is a significant need for additional research to investigate how to best educate patients undergoing HSCT while in the hospital. To generate recommendations about best practice, additional research is needed using methods that can generate higher levels of evidence (Polit & Beck, 2017). For example, a multisite randomized controlled trial with objective outcomes to evaluate the effect on patient learning as well as clinical outcomes, such as patient information and skill retention, hospital readmission rates, adherence to treatments, and patient satisfaction, would allow for better evaluation of the effectiveness of a specific approach to patient teaching.
Conclusion
Patient education is a critical element to the care of patients undergoing HSCT. This review revealed that structured approaches to patient education, such as the use of PST, may be worthwhile approaches to patient education and may be effective in reducing symptoms of distress. Ultimately, the body of knowledge regarding how to best teach patients undergoing HSCT is limited and would benefit from additional high-quality studies to broaden and strengthen the evidence base that nurses can use to approach patient teaching.
About the Authors
Claire Beaton, RN, MN, is an RN and Kara Sealock, RN, BN, MEd, EdD, CCNC(C)®, CCNE, is an associate professor, both in the Faculty of Nursing; K. Alix Hayden, MLIS, MSc, PhD, is a librarian for Libraries and Cultural Resources; and Kathryn M. King-Shier, RN, PhD, FESC, is a professor and the associate dean of graduate programs in the Faculty of Nursing, all at the University of Calgary in Canada. No financial relationships to disclose. Beaton, Sealock, Hayden, and King-Shier contributed to the conceptualization and design and completed the data collection. Beaton, Sealock, and King-Shier provided the analysis. All authors contributed to the manuscript preparation.Beaton can be reached at cmbeaton@alumni.ucalgary.ca with copy to ONFEditor@ons.org. (Submitted June 2023. Accepted October 20, 2023.)
References
Aslam, A.M., Kennedy, J., Seghol, H., Khisty, N., Nicols, T.A., & Adie, S. (2023). A randomized controlled trial of patient recall after detailed written consent versus standard verbal consent in adults with routine orthopaedic trauma. Bone and Joint Open, 4(2), 104–109.
Balck, F., Zimmermann, A., & Neumann, A. (2015). Conception and associated evaluation of a problem-solving training (PST) for patients in the hospital context of hematopoietic stem cell transplantation (HSCT). Journal of Psychosocial Oncology, 33(3), 232–249.
Bartholomew, L.K., & Mullen, P.D. (2011). Five roles for using theory and evidence in the design and testing of behavior change interventions. Journal of Public Health Dentistry, 71(Suppl. 1), S20–S33.
Bergkvist, K., Winterling, J., & Kisch, A.M. (2020). Support in the context of allogeneic hematopoietic stem cell transplantation—The perspectives of family caregivers. European Journal of Oncology Nursing, 46, 101740.
Bevans, M., Castro, K., Prince, P., Shelburne, N., Prachenko, O., Loscalzo, M., . . . Zabora, J. (2010). An individualized dyadic problem-solving education intervention for patients and family caregivers during allogeneic hematopoietic stem cell transplantation: A feasibility study. Cancer Nursing, 33(2), E24–E32.
Bevans, M., Wehrlen, L., Castro, K., Prince, P., Shelburne, N., Soeken, K., . . . Wallen, G.R. (2014). A problem-solving education intervention in caregivers and patients during allogeneic hematopoietic stem cell transplantation. Journal of Health Psychology, 19(5), 602–617. https://doi.org/10.1177/1359105313475902
Cohen, M.Z., Jenkins, D., Holston, E.C., & Carlson, E.D. (2013). Understanding health literacy in patients receiving hematopoietic stem cell transplantation. Oncology Nursing Forum, 40(5), 508–515. https://doi.org/10.1188/13.ONF.508-515
de Azevedo, I.C., Cassiano, A.d.N., de Carvalho, J.B.L., & Ferreira Júnior, M.A. (2017). Nursing care for hematopoietic stem cell transplant recipients and their families. Rev Rene, 18(4), 559–566.
Foster, J., Idossa, L., Mau, L.-W., & Murphy, E. (2016). Applying health literacy principles: Strategies and tools to develop easy-to-read patient education resources. Clinical Journal of Oncology Nursing, 20(4), 433–436. https://doi.org/10.1188/16.CJON.433-436
Friedman, A.J., Cosby, R., Boyko, S., Hatton-Bauer, J., & Turnbull, G. (2011). Effective teaching strategies and methods of delivery for patient education: A systematic review and practice guideline recommendations. Journal of Cancer Education, 26(1), 12–21.
Galgano, L., Hutt, D., & Mekelenkamp, H. (2023). HSCT: How does it work? In M. Kenyon & A. Babic (Eds.), The European blood and marrow transplantation textbook for nurses: Under the auspices of EBMT (pp. 25–43). Springer.
Halldorsdottir, H., Thoroddsen, A., & Ingadottir, B. (2020). Impact of technology-based patient education on modifiable cardiovascular risk factors of people with coronary heart disease: A systematic review. Patient Education and Counseling, 103(10), 2018–2028.
Hoffmann, T.C., Glasziou, P.P., Boutron, I., Milne, R., Perera, R., Moher, D., . . . Michie, S. (2014). Better reporting of interventions: Template for Intervention Description and Replication (TIDieR) checklist and guide. BMJ, 348, g1687.
Hong, Q.N., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., Dagenais, P., . . . Pluye, P. (2018). The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Education for Information, 34(4), 285–291.
Husson, O., Mols, F., & van de Poll-Franse, L.V. (2011). The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: A systematic review. Annals of Oncology, 22(4), 761–772.
Inott, T., & Kennedy, B.B. (2011). Assessing learning styles: Practical tips for patient education. Nursing Clinics of North America, 46(3), 313–320.
Knowles, M.S. (1980). The modern practice of adult education: From pedagogy to andragogy. Association Press.
Liso, A., Neri, M., Maglietta, F., La Russa, R., & Turillazzi, E. (2017). Hematopoietic stem cell transplantation: A bioethical lens. Stem Cells International, 2017, 1286246.
Livne, Y., Peterfreund, I., & Sheps, J. (2017). Barriers to patient education and their relationship to nurses’ perceptions of patient education climate. Clinical Nursing Studies, 5(4), 65.
Lorig, K.R., & Holman, H. (2003). Self-management education: History, definition, outcomes, and mechanisms. Annals of Behavioral Medicine, 26(1), 1–7.
Merriam, S.B., & Baumgartner, L.M. (2020). Learning in adulthood: A comprehensive guide (4th ed.). John Wiley and Sons.
Mezirow, J. (2000). Learning as transformation: Critical perspectives on a theory in progress. Jossey-Bass.
Nezu, A.M., Nezu, C.M., & D’Zurilla, T.J. (2013). Problem-solving therapy: A treatment manual. Springer.
Nezu, A.M., Nezu, C.M., Houts, P.S., Friedman, S.H., & Faddis, S. (1999). Relevance of problem-solving therapy to psychosocial oncology. Journal of Psychosocial Oncology, 16(3–4), 5–26.
Northouse, L., Williams, A.-L., Given, B., & McCorkle, R. (2012). Psychosocial care for family caregivers of patients with cancer. Journal of Clinical Oncology, 30(11), 1227–1234.
Page, M.J., McKenzie, J.E., Bossuyt, P.M., Boutron, I., Hoffmann, T.C., Mulrow, C.D., . . . Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71.
Parnell, T.A. (2014). Health literacy in nursing: Providing person-centered care. Springer.
Polit, D.F., & Beck, C.T. (2017). Resource manual for nursing research: Generating and assessing evidence for nursing practice (10th ed.). Wolters Kluwer.
Schmit-Pokorny, K., Franco, T., Frappier, B., & Vyhlidal, R.C. (2003). The cooperative care model: An innovative approach to deliver blood and marrow stem cell transplant care. Clinical Journal of Oncology Nursing, 7(5), 509–514, 556.
Schoemans, H.M., Finn, L., Foster, J., Roche-Green, A., Bevans, M., Kullberg, S., . . . Schmit-Pokorny, K. (2019). A conceptual framework and key research questions in educational needs of blood and marrow transplantation patients, caregivers, and families. Biology of Blood and Marrow Transplantation, 25(7), 1416–1423.
Seo, H.-J., Baek, Y.-G., Cho, B.-S., Kim, T.-S., Um, Y.H., & Chae, J.-H. (2019). Anxiety and depression of the patients with hematological malignancies during hospitalization for hematopoietic stem cell transplantation. Psychiatry Investigation, 16(10), 751–758.
Sidani, S., & Braden, C.J. (1997). Evaluating nursing interventions: A theory-driven approach. Sage.
Sidani, S., & Braden, C.J. (2021). Nursing and health interventions: Design, evaluation, and implementation (2nd ed.). John Wiley and Sons.
Slyer, J.T. (2016). Unanswered questions: Implications of an empty review. JBI Database of Systematic Reviews and Implementation Reports, 14(6), 1–2.
Strupeit, S., Buß, A., & Dassen, T. (2013). Effectiveness of nurse-delivered patient education interventions on quality of life in outpatients: A systematic review. Applied Nursing Research, 26(4), 232–238.
Toronto, C.E., & Remington, R. (Eds.). (2020). A step-by-step guide to conducting an integrative review. Springer.
van Ryn, M., Sanders, S., Kahn, K., van Houtven, C., Griffin, J.M., Martin, M., . . . Rowland, J. (2011). Objective burden, resources, and other stressors among informal cancer caregivers: A hidden quality issue? Psycho-Oncology, 20(1), 44–52.
Whittemore, R., & Knafl, K. (2005). The integrative review: Updated methodology. Journal of Advanced Nursing, 52(5), 546–553.

