The Impact of Chemotherapy-Related Cognitive Impairment on Social Roles and Well-Being in Breast Cancer Survivors
Purpose: To explore the impact of disruptions in information processing (DIPs) on social roles, well-being, and quality of life (QOL) in breast cancer survivors after chemotherapy.
Participants & Setting: Experiences of DIPs were explored in eight breast cancer survivors aged 53–70 years, 12–60 months post-treatment, referred from a National Cancer Institute–designated cancer center and a nonprofit breast cancer support organization from January 6 to August 31, 2020.
Methodologic Approach: This study used a mixed-methods approach. Participants journaled and answered questionnaires sent via mail that asked them about changes in their cognition, QOL, and social roles. Qualitative data were thematically analyzed using constant comparative analysis, and questionnaire scores were compared with qualitative data.
Findings: Journals revealed problems with functioning in occupational roles and increased stress, anxiety, and frustration. Women with more DIPs tended to have lower role satisfaction and QOL. Greater role satisfaction was associated with higher QOL and social role participation.
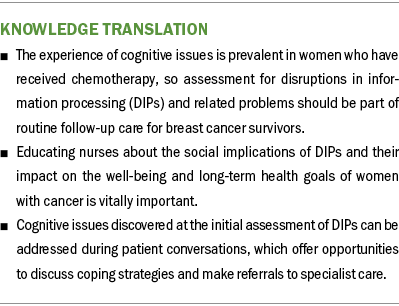
Implications for Nursing: Mitigating the effects of DIPs on social function may allow women to continue in important roles, which has the potential to affect QOL.
Jump to a section
Breast cancer is the form of cancer with the highest incidence in women, with more than 80% of new diagnoses occurring in women aged older than 50 years (American Cancer Society, 2022a). Because of the improved effectiveness of current treatment regimens and early detection, there were over four million survivors in the United States in early 2022 (American Cancer Society, 2022b). Because the incidence of breast cancer is highest in women aged older than 50 years, the focus of survivorship care must encompass problems most important to women in this age group, including issues that may lead to early retirement, changes in family responsibilities, and impacts of disease or treatment on social roles.
Research Problem
Background
Among the most common complaints of breast cancer survivors are episodes of disruptions in information processing (DIPs), or episodic disruptions in memory, attention, processing speed, language, and executive function. DIPs often persist for years following chemotherapy (Bolton & Isaacs, 2018; Henderson et al., 2019; Lange et al., 2019; Rodríguez Martín et al., 2020). Although many with DIPs describe episodes of forgetfulness and problems finding the right word, the most common hallmark of DIPs is an inability to concentrate, think, and multitask. Like delirium, these cognitive symptoms are described as unpredictable and subtle, but reversible. Because of the transient presentation of these symptoms following chemotherapy treatment, women with complaints of DIPs often have healthy results on neuropsychological tests (Bray et al., 2018), yet find it difficult to engage in activities essential for maintaining roles that contribute to a meaningful life and sense of well-being and quality of life (QOL).
Social roles consist of the actions and behaviors deemed necessary to fulfill positions held within a group. Multiple social roles are held by each individual and include those associated with family or friend relationships, work, school, volunteerism, and leisure or discretionary activities (e.g., religion, community participation, sports). Depending on life circumstances, women typically acquire, change, and lose roles as they progress through life. Social roles are an important source of well-being in women because they provide a positive sense of identity and purpose (Chen et al., 2014; Krause, 1994; Reid & Hardy, 1999).
Identity is the meaning one ascribes to oneself in relation to a position held in society and provides a standard or guide for behavior and interaction with others (Burke, 1991; Marcussen et al., 2004). Roles that are important or salient to the individual provide personal meaning and are tied to a person’s self-identity. In relation to a position or role held in society, the importance assigned to that role by the individual affects the degree to which it becomes a part of their self-concept or self-identity. Competent performance and satisfaction in roles deemed essential to self-identity and of high salience is an important source of psychological and physical well-being in women (Talley et al., 2012). Conversely, the loss of important social roles of high salience can lead to feelings of identity loss (Chen et al., 2014). Common social roles of women aged older than 50 years include spouse, mother, grandmother, worker, homemaker, friend, and volunteer. Occupational roles provide women with financial stability.
Significance
Middle-aged to older women may experience transitions in their social roles. Many may begin to experience adult children leaving home, older parents needing care, or career transitioning. In a 12-year longitudinal study of 493 women aged 45–55 years, women reported a sense of loss in their lives when transitioning from midlife to later life as they experienced changes in social roles around parenting and employment (Burn et al., 2016). Health problems and mid- to late-life experiences, such as the loss of parents, spouse, or friends, may trigger new, shifting, or diminished social roles. Often, lost roles may be replaced by other social activities, such as volunteering, social activities with friends, and spending time with grandchildren.
DIPs are pervasive and unpredictable; as a result, they often lead to disruptions in a person’s ability to perform their roles. Although some roles can be delegated to others, many are deeply tied to one’s identity, and delegation can cause significant emotional distress or negative evaluation of self-worth. These feelings can lead to additional negative perceptions of cognitive function because of worries about future DIPs, and this heightened anxiety may lead to withdrawing from highly valued roles that are central to one’s identity.
Conceptual Framework
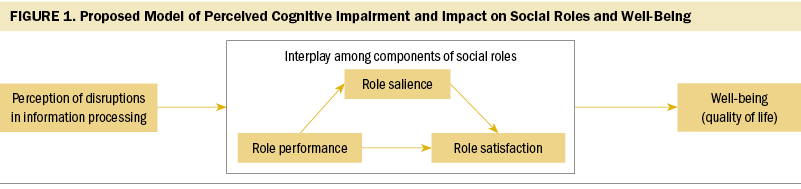
The model in Figure 1 illustrates the proposed mechanism by which DIPs can affect women’s performance of and satisfaction in social roles and lead to an alteration in well-being. Problems functioning in important roles can lead to emotional distress. The impact this distress may have on psychological well-being is influenced by the saliency of the role for the individual (Talley et al., 2012). If the role is important to one’s identity, the level of emotional distress that results when one is unable to satisfactorily perform that role will affect psychological well-being outcomes more significantly (Talley et al., 2012).
Problem Statement
The aim of this mixed-methods pilot study was to explore and elucidate the impact of DIPs on the relationships among the components of social roles (role salience, role performance, role satisfaction), well-being, and QOL in breast cancer survivors aged older than 50 years following chemotherapy.
Design
Participants and Setting
This study was approved by the institutional review board at the University of Oklahoma Health Sciences Center in Oklahoma City. The sample consisted of eight White women aged 53–70 years (mean = 60.6, SD = 5.1), referred from the Stephenson Cancer Center, a National Cancer Institute–designated cancer center, and from Project 31, a nonprofit breast cancer support organization in Oklahoma, from January 6 to August 31, 2020. Of the 20 individuals who expressed interest, 3 were lost during follow-up. Of the remaining 17, 12 did not meet one or more of the following study inclusion criteria: (a) being aged 50 years or older (n = 1), (b) being free of metastasis (n = 2), and (c) being 12–60 months from last chemotherapy treatment (n = 9). A telephone screening verified that participants did not have a diagnosis of dementia and were able to provide informed consent, as measured by a total score on the telephone version of the Montreal Cognitive Assessment of more than 19 points (Nasreddine et al., 2005; Pendlebury et al., 2013).
Data Sources
Participants received a mailed study packet that included (a) study consent and Health Insurance Portability and Accountability Act forms; (b) a sociodemographic and health questionnaire; (c) key study questionnaires; (d) a journal; and (e) a self-addressed, stamped envelope. Verbal instructions were given during the telephone interview, and written instructions were included in the packet. All elements of the study packet were completed by participants at home. The packets were mailed back to the primary investigator (L.R.B.) within one to six days.
Severity of DIPs: The participants’ perception of their cognition, as compared to their pre–breast cancer cognitive performance, was measured using the Everyday Cognition scale (ECog) (Farias et al., 2013). The ECog contains 39 questions that ask about events that reflect difficulties across the following four cognitive domains: memory, language, visuospatial abilities, and executive functions (planning, organization, divided attention). Participants were asked to compare their performance in each domain to their pre–breast cancer performance. Items on the ECog are scored using a four-point Likert-type scale with responses ranging from 1 (better or no change) to 4 (consistently much worse). The ECog was validated using several clinical groups consisting of older adults with mild cognitive impairment or dementia and a healthy group (Farias et al., 2008). Psychometric properties were shown to be very good on the ECog, with test–retest reliability of 0.82, and good content, construct, convergent, and divergent validity (Farias et al., 2008).
Role salience, limitations, and satisfaction: The Social Role Participation Questionnaire (SRPQ) assesses role participation along the following three dimensions: role importance (salience), limitations to role participation, and satisfaction with role performance (van Genderen et al., 2016). The following 11 types of roles are addressed by the SRPQ: intimate relationships, relationships with children, relationships with other family, employment, planning or engaging in social activities, physical leisure activities, hobbies, travel or vacationing, community/ cultural/religious activities, casual or informal contact with others, and educational pursuits. Items are rated on five-point Likert-type scales. For role importance (salience), scores range from 1 (not at all important) to 5 (extremely important) (Gignac et al., 2008), regardless of whether the participant is actively engaged in the role. The limitations to role participation dimension rating addresses the level of physical difficulty in participating in each role, with scores ranging from 1 (no difficulty) to 4 (unable to do) or 0 = not applicable. For satisfaction (with time spent in roles or with role performance), scores range from 1 (not at all satisfied) to 5 (extremely satisfied). In a sample of patients with osteoarthritis, internal consistency for each dimension of the SRPQ was good, with a Cronbach’s alpha of 0.74 for role importance (salience), 0.83 for satisfaction with time spent in roles, and 0.85 for satisfaction with role performance (Gignac et al., 2008).
QOL: The Functional Assessment of Cancer Therapy–Breast (FACT-B) measures multidimensional QOL and well-being specific to breast cancer survivorship. The FACT-B consists of the following two subscales: the Functional Assessment of Cancer Therapy–General and the breast cancer subscale (Brady et al., 1997). It assesses physical (seven items), social (seven items), emotional (five items), and functional (seven items) well-being, relationship with doctor (two items), and breast cancer–specific QOL (nine items). Reliability of the FACT-B is very good, with a Cronbach’s alpha of 0.9, and test–retest reliability of 0.85. (Brady et al., 1997).
Impact of DIPs on roles and QOL captured through journaling: Journaling was used to obtain a broader perspective of the experience of DIPs and the impact they have on women’s daily life and well-being. Expressive writing through journaling is a powerful tool used to capture the essence of important life events by offering participants the opportunity to tell their story in their own words and from their personal perspectives (Pennebaker & Seagal, 1999). Participants were asked to write for 20–30 minutes per day on four consecutive days about their experiences with DIPs and any changes or problems in their social roles. The focus of each day’s writing was guided by a specific question that varied as follows:
- Day 1: “How has your ability to fulfill important roles and duties in your life changed since you completed chemotherapy? What factors led to these changes?”
- Day 2: “Describe how your ability to think has changed since chemotherapy and what factors contributed to these changes.”
- Day 3: “Talk about how changes in your ability to think have affected important roles in your life.”
- Day 4: “What have you done to cope with changes in your roles and duties?”
Participants were instructed not to worry about grammar, spelling, or their writing and sentence structure (Pennebaker & Seagal, 1999).
Data Analysis
This mixed-methods pilot study involved the sequential use of qualitative and quantitative designs to explore the impact of DIPs on components of social roles. The main objective was explored with the qualitative data collected via journals, and the quantitative data collected by the questionnaires were used to corroborate and/or expand on insights gained.
Themes were generated using constant comparative analysis, a qualitative method that involves various levels of coding, including initial, axial, and selective coding (Kolb, 2012; Ridolfo & Schoua- Glusberg, 2011). Initial coding involved identifying concepts and categories in each journal entry with the aim of understanding the experience of each participant. Coding then proceeded by combining subcategories and breaking down categories to form common elements that were categorized into person-centered, relevant themes. As an iterative process, themes were verified by linking them back to the subcategories. Categories and themes were discussed to validate findings. Experts in expressive writing (M.C. and L.R.B.) and mixed methods (S.S.C.B., B.W.C., and L.R.B.) were involved in the analysis of the journals.
Following completion of the journal analysis, the results were also shared with two participants, who were given the opportunity to offer additional input. The participants verified that the analysis captured the essence of their experience with DIPs. The questionnaire scores were analyzed graphically using Microsoft Excel to illustrate the interactive effects of role salience and cognitive loss on the relationship between role limitation and satisfaction. The sample size of this study was very small with few missing data. Handling of missing data was based on pairwise deletion to optimize use of the data provided (Kang, 2013).
Findings
Sample Characteristics
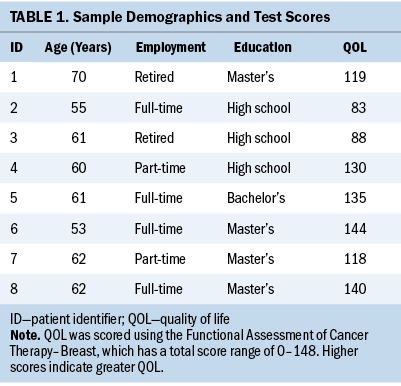
The sample consisted of eight White women aged 53–70 years (mean = 60.6, SD = 5.1); five were college educated, and three had a high school diploma or GED (see Table 1). All but one were married and living with their spouse, and six were employed either full-or part-time.
Role Salience and the Relationship Among Components of Social Roles
Higher levels of role salience: Women with higher levels of role salience tended to describe themselves as people who held multiple roles and were adept at efficiently managing several tasks prior to their breast cancer diagnosis. Participants with the highest role salience were women who, prior to their diagnosis, maintained multiple salient roles in areas like careers, social organizations, and leadership positions, and they led active social lives. Family support during their recovery phase was mentioned as being very important by two of the three women with the highest role salience.
One participant listed employment as being a highly valuable role. Having been in the same career for 36 years, she eased back into this role post-treatment. Although it was difficult, she worked her way back to full-time employment, stating, “I’m not willing to try a brand new job that is totally outside my comfort zone. I’m not sure my brain can learn a completely new routine or job.” Returning to important roles was of great value to this participant, as evidenced by her following statement:
I have gone back to my roles of mom, wife, friend, nurse, leader in my nursing organization, leader in a support group, and secretary of our association. I haven’t changed any roles. It keeps me busy and my mind open. If I quit some of the things I do, I think my mind would not be as sharp.
Another participant with a high score for salience had one of the lowest scores for role satisfaction. Employment became overwhelming for this participant, and she left her position for a time, stating, “Although I continued to work, the quality of my writing and thinking declined. My roles as wife, mother, and competent employee declined until I felt as if I was holding on by a thread.” She also stated, “I was really unable to deal with stress and the fast pace of work. I took two years off and am now back working part-time for three institutions.” Although the participant highly valued these roles, her ability to maintain a satisfactory level of participation was reduced because of DIPs, which affected the satisfaction she felt in her most highly valued roles.
Lower levels of role salience: Participants with the lowest salience scores spoke less about having multiple roles; instead, they identified one or two that were of the greatest importance to them. Participants with only one main salient role experienced more dissatisfaction and less QOL when DIPs interfered with performance in that role.
A participant with the lowest score for salience, whose most salient role was her employment, returned to work three months after chemotherapy but was laid off several months later. She experienced challenges performing her job duties because of experiencing DIPs following her return to work, in addition to an increase in feelings of anxiety and depression. Describing the situation, she stated the following:
I feel like I was very scatterbrained, and it took me a lot longer to do my work. I feel that I was not able to perform my job as well as I had in the past. It was a struggle, and 10 months after I returned to work full-time, I was laid off. The reason was reduction in workforce, but deep down, I feel that it was related to my cancer and my inability to do the job as well, and I couldn’t take the high pressure.
Eventually, the company rehired her, but into a position with less pay.
Based on participants with the highest and lowest levels of role salience, those with less social involvement and only one salient role fared worse when their ability to perform in that role became compromised. Those with numerous roles that were important to them who were able to maintain some level of performance in some of the roles tended to report more satisfaction and greater QOL.
Perceived Change in Cognition and its Relationship to Social Roles and QOL
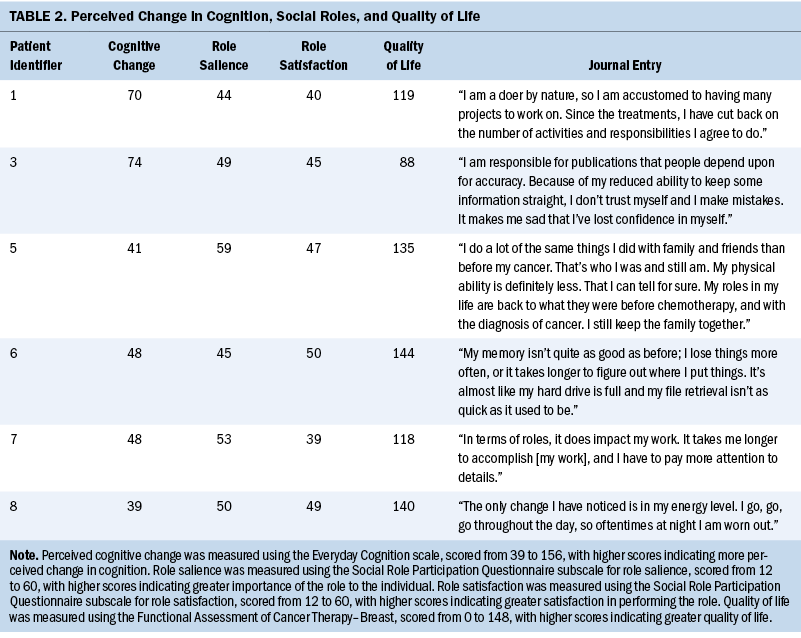
Table 2 shows the relationships between role salience and satisfaction according to level of perceived cognitive loss. Changes in cognition, as measured by the ECog, were not linearly associated with any of the components of social roles. However, participants with the highest perceived levels of change in cognition had lower levels of satisfaction and role salience.
Higher perceived levels of DIPs: A participant who had the highest level of perceived cognitive change, but ranked lower in role salience, satisfaction, and QOL (FACT-B score of 88), had maintained an active social life before being diagnosed with breast cancer and readily volunteered to take on projects. After chemotherapy, DIPs compromised her ability to perform various duties. She stated the following:
I have always been a multitasker, but now I know that if I do more than two things at once, I will fail at one or both. This is so obvious to me that when I perform even a simple task, I become so anxious about what I’m trying to accomplish that I make mistakes. I believe that a combination of [chemotherapy] and anxiety contributes to my difficulties.
One participant, who had retired from her career after treatment and had the second highest level of perceived change in cognition, said the following:
Thinking doesn’t seem to be primary, although sometimes it seems that I have to use mental cues to figure certain things out. Examples include names, lists, and sequential numbers. But the frustrating part is retention. Some days it becomes a struggle to pull information out of my head. Information I know is there, but I can’t find the right door to open to retrieve it.
In addition to low role salience and low satisfaction, this participant reported moderate QOL (FACT-B score of 119) as well as a high score for role limitations.
Lower salience and satisfaction in important roles may be a factor in women’s perception of the changes in their cognition. With fewer salient roles, the inability to perform satisfactorily may have a greater impact on perceived cognitive change.
Lower perceived level of DIPs: One participant who had previously described herself as being a resilient person and who scored with a high level of satisfaction and low salience stated, “Even if those roles had changed, I’m not sure I would notice; I would just adjust or compensate. It is not in my nature to whine or complain. I’m much more likely to find a way.” The situation was the opposite for another participant with low QOL (FACT-B score of 118) and very low satisfaction scores. She stated the following:
I also notice, because I have to focus more intently, that I feel more anger and frustration than I did before chemotherapy. I think it does impact some of my interpersonal relationships. I get frustrated easier by people who do get off-task and even with family members over small issues.
The participant with the least perceived change in cognition stated the following:
I’m still working a full-time job, so maybe that has helped. I am very organized, [I] always was; I can still remember things, et cetera. My boss depends on me, so I work to stay on top of things so he doesn’t have to.
Having helped her sister care for their aging mother, she also stated, “That’s probably why I will work until I’m in my late 60s, because I see how important it is to stay active and try to keep as sharp as I can.” Two participants with the least change in cognition focused on maintaining important roles and remaining active and functional throughout their treatment.
Discussion
The findings from this pilot study of eight older breast cancer survivors demonstrated the unpredictability of DIPs and their effects on social roles. DIPs may also induce feelings of anxiety, agitation, and embarrassment that erode the woman’s confidence in conducting her normal everyday activities. Women have reported similar experiences in findings from other qualitative studies that showed the inconsistent yet persistent manner of cognitive changes resulting in problems functioning in social roles (Kanaskie & Loeb, 2015; Player et al., 2014). The pervasive manner of DIPs can lead to episodes that range from being embarrassing to posing a danger to aspects of women’s performance of everyday roles. Women have reported feeling frustration and distress over memory lapses and the inability to focus, as well as feelings of danger when overwhelmed and confused in the midst of traffic or hectic situations (Bolton & Isaacs, 2018). DIPs that appear particularly problematic are those that affect skills and abilities essential to proficiency at work and home, such as organization, planning, and multitasking. The decline in these functions is associated with the loss of roles and strain in relationships, which may lead to having lower self-esteem, feeling undervalued, and feeling less confident in the ability to function competently in society. In one study, women described how these deficits in their abilities led to them feeling less capable than they were prior to chemotherapy treatment and described the need to adjust to a new normal (Henderson et al., 2019). This pilot study found that salience, or the importance the women assign to their roles, was a key mediating factor in determining whether limitations or declines in performance led to distress and declines in self-worth and QOL. There is a dearth of literature focused on this relationship between the importance of a given role to a woman and the distress associated with declines in being able to perform this role.
Engaging in important roles is a source of validation for women and provides a sense of self-worth (Chen et al., 2014). Conversely, the inability to perform in roles that have become an integral part of a woman’s life can cause emotional and psychosocial issues. This was evident by statements made in participants’ journals and is consistent with findings from other studies (Bolton & Isaacs, 2018; Boykoff et al., 2009; Henderson et al., 2019; Player et al., 2014).
Described in detail in the journal narratives and confirmed through scores on standard clinical assessment tools, satisfaction in performing salient social roles is associated with higher QOL. Women with higher role salience described themselves prior to their cancer diagnosis as “go-getters,” women who valued their careers and social involvement and who were not afraid to take on leadership roles. These women also had multiple salient roles that contributed to their overall social identity. The three participants with the highest saliency were able to maintain moderate levels of well-being and QOL. However, it is not necessarily the number of roles but the ability to maintain satisfaction in performing those important roles that made the difference. Women with few salient roles or minimal social involvement may experience a greater perception of cognitive disruption if performance is disrupted by DIPs in those few important roles.
Implications for Practice and Research
Interplay of Salience and Satisfaction
It is important to recognize that the impact of DIPs on the lives of women cannot be fully defined by measuring cognitive function because satisfaction is multifaceted, encompassing social, emotional, and functional issues. Role saliency mediates the relationship between a woman’s limitations and her satisfaction in her roles. This pilot study revealed that women can have one very salient role that can cause a greater decline in satisfaction when limitations prevent participation in that role. However, women with several salient roles are likely to experience less of a decline in satisfaction when limitations do not affect most of these salient roles.
Occupational Role and Other Issues
For most, DIPs began during chemotherapy, with some experiencing improvements on treatment completion. Despite that fact, problems that affect daily living persisted 12–60 months beyond completion of treatment for seven of the eight participants. The type of role most often affected was occupational, with women retiring, changing jobs, or struggling to compensate for the occurrence of DIPs while maintaining employment. Other research studies have also found that women’s challenges functioning in occupational roles are among the most common complaints, as well as challenges with family and other social roles (Bolton & Isaacs, 2018; Henderson et al., 2019; Player et al., 2014; Von Ah et al., 2013).
Financial distress cannot be ignored by nurses when addressing disruptions to occupational roles in women receiving treatment for cancer. Cognitive changes following chemotherapy can cause women to leave long-standing employment, opting to retire or pursue less demanding jobs, which not only has a negative impact on their identity but can also lead to financial loss (Becker et al., 2015; Boykoff et al., 2009; Kanaskie & Loeb, 2015; Player et al., 2014; Von Ah et al., 2013). Consistent with these findings, some women in this study were forced to leave employment. Because of difficulties at work, a few participants had retired, were laid off, or gave up employment altogether. Others developed coping strategies that allowed them to return to occupational roles, although in some instances with less pay. Adding to the cost of treatment, these shifts in employment may contribute to additional financial hardships, as well as the loss of health insurance and other important benefits.
Limitations
Generalizability of this study is limited because of the small size and homogeneous nature of the study sample. The participants were all White and had minimal cognitive impairment, and most had education levels of some college or higher. Additional research is needed in a more diverse sample of older women to evaluate the effect of DIPs on the various components of social roles, psychological well-being, and QOL.
Conclusion
The impact of role loss depends on multiple factors, such as occupational status, level of involvement in various roles, importance of each role, ability to maintain active involvement in important roles, emotional well-being, and role functionality. To date, there is no single tool that sufficiently addresses all of these issues to provide an accurate assessment or measurement of DIPs and the impact they have on a woman’s life. Ongoing work in this area is warranted.
The authors gratefully acknowledge the support of Project 31 in the completion of this project and in advocating for breast cancer survivors.
About the Authors
Lisa R. Bailey, PhD, RN, was, at the time of this writing, a PhD student and Melissa Craft, PhD, APRN-CNS, AOCN®, FCNS, FAAN, is the associate dean for clinical affairs, outreach, and practice innovation, both in the Fran and Earl Ziegler College of Nursing at the University of Oklahoma Health Sciences Center in Oklahoma City; Shannon S.C. Bert, PhD, is an associate professor in the Department of Human Relations at the University of Oklahoma in Norman; and Barbara W. Carlson, RN, PhD, FGSA, is a professor in the School of Nursing at the University of North Carolina, Wilmington. This research was funded, in part, by the Donald W. Reynolds Foundation and Sigma Theta Tau Beta Delta At-Large Chapter. Bailey completed the data collection. Craft, Bert, and Carlson provided statistical support. Bailey, Craft, and Bert provided the analysis. All authors contributed to the conceptualization and design and the manuscript preparation. Bailey can be reached at lisabailey945@gmail.com, with copy to ONFEditor@ons.org. (Submitted July 2023. Accepted December 19, 2023.)
References
American Cancer Society. (2022a). Breast cancer: Facts and figures, 2022–2024. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
American Cancer Society. (2022b). Cancer treatment and survivorship: Facts and figures, 2022–2024. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and…
Becker, H., Henneghan, A., & Mikan, S.Q. (2015). When do I get my brain back? Breast cancer survivors’ experiences of cognitive problems. Clinical Journal of Oncology Nursing, 19(2), 180–184. https://doi.org/10.1188/15.CJON.180-184
Bolton, G., & Isaacs, A. (2018). Women’s experiences of cancer-related cognitive impairment, its impact on daily life and care received for it following treatment for breast cancer. Psychology, Health and Medicine, 23(10), 1261–1274. https://doi.org/10.1080/13548506.2018.1500023
Boykoff, N., Moieni, M., & Subramanian, S.K. (2009). Confronting chemobrain: An in-depth look at survivors’ reports of impact on work, social networks, and health care response. Journal of Cancer Survivorship: Research and Practice, 3(4), 223–232. https://doi.org/10.1007/s11764-009-0098-x
Brady, M.J., Cella, D.F., Mo, F., Bonomi, A.E., Tulsky, D.S., Lloyd, S.R., . . . Shiomoto, G. (1997). Reliability and validity of the Functional Assessment of Cancer Therapy–Breast quality-of-life instrument. Journal of Clinical Oncology, 15(3), 974–986. https://doi.org/10.1200/JCO.1997.15.3.974
Bray, V.J., Dhillon, H.M., & Vardy, J.L. (2018). Systematic review of self-reported cognitive function in cancer patients following chemotherapy treatment. Journal of Cancer Survivorship: Research and Practice, 12(4), 537–559. https://doi.org/10.1007/s11764-018-0692-x
Burke, P.J. (1991). Identity processes and social stress. American Sociological Review, 56(6), 836–849. https://doi.org/10.2307/2096259
Burn, K., Dennerstein, L., Browning, C., & Szoeke, C. (2016). Patterns of social engagement in the transition to later life. Maturitas, 88, 90–95. https://doi.org/10.1016/j.maturitas.2016.03.016
Chen, B.Q.P., Parmar, M.P., & Gartshore, K. (2014). Supporting women with advanced breast cancer: The impact of altered functional status on their social roles. Canadian Oncology Nursing Journal, 24(3), 194–203. https://doi.org/10.5737/1181912x243194198
Farias, S.T., Mungas, D., Reed, B.R., Cahn-Weiner, D., Jagust, W., Baynes, K., & DeCarli, C. (2008). The measurement of Everyday Cognition (ECog): Scale development and psychometric properties. Neuropsychology, 22(4), 531–544. https://doi.org/10.1037/0894-4105.22.4.531
Farias, S.T., Park, L.Q., Harvey, D.J., Simon, C., Reed, B.R., Carmichael, O., & Mungas, D. (2013). Everyday cognition in older adults: Associations with neuropsychological performance and structural brain imaging. Journal of the International Neuropsychological Society, 19(4), 430–441. https://doi.org/10.1017/S1355617712001609
Gignac, M.A.M., Backman, C.L., Davis, A.M., Lacaille, D., Mattison, C.A., Montie, P., & Badley, E.M. (2008). Understanding social role participation: What matters to people with arthritis? Journal of Rheumatology, 35(8), 1655–1663. https://www.jrheum.org/content/jrheum/35/8/1655.full.pdf
Henderson, F.M., Cross, A.J., & Baraniak, A.R. (2019). ‘A new normal with chemobrain’: Experiences of the impact of chemotherapy-related cognitive deficits in long-term breast cancer survivors. Health Psychology Open, 6(1), 2055102919832234. https://doi.org/10.1177/2055102919832234
Kanaskie, M.L., & Loeb, S.J. (2015). The experience of cognitive change in women with breast cancer following chemotherapy. Journal of Cancer Survivorship, 9(3), 375–387. https://doi.org/10.1007/s11764-014-0387-x
Kang, H. (2013). The prevention and handling of the missing data. Korean Journal of Anesthesiology, 64(5), 402–406. https://doi.org/10.4097/kjae.2013.64.5.402
Kolb, S.M. (2012). Grounded theory and the constant comparative method: Valid research strategies for educators. Journal of Emerging Trends in Educational Research and Policy Studies, 3(1), 83–86.
Krause, N. (1994). Stressors in salient social roles and well-being in later life. Journal of Gerontology, 49(3), P137–P148. https://doi.org/10.1093/geronj/49.3.p137
Lange, M., Licaj, I., Clarisse, B., Humbert, X., Grellard, J.-M., Tron, L., & Joly, F. (2019). Cognitive complaints in cancer survivors and expectations for support: Results from a web-based survey. Cancer Medicine, 8(5), 2654–2663. https://doi.org/10.1002/cam4.2069
Marcussen, K., Ritter, C., & Safron, D.J. (2004). The role of identity salience and commitment in the stress process. Sociological Perspectives, 47(3), 289–312. https://doi.org/10.1525/sop.2004.47.3.289
Nasreddine, Z.S., Phillips, N.A., Bédirian, V., Charbonneau, S., Whitehead, V., Collin, I., . . . Chertkow, H. (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53(4), 695–699. https://doi.org/10.1111/j.1532-5415.2005.53221.x
Pendlebury, S.T., Welch, S.J.V., Cuthbertson, F.C., Mariz, J., Mehta, Z., & Rothwell, P.M. (2013). Telephone assessment of cognition after transient ischemic attack and stroke: Modified telephone interview of cognitive status and telephone Montreal Cognitive Assessment versus face-to-face Montreal Cognitive Assessment and neuropsychological battery. Stroke, 44(1), 227–229. https://doi.org/10.1161/STROKEAHA.112.673384
Pennebaker, J.W., & Seagal, J.D. (1999). Forming a story: The health benefits of narrative. Journal of Clinical Psychology, 55(10), 1243–1254. https://doi.org/10.1002/(sici)1097-4679(199910)55:10<1243::aid-jclp6>3…
Player, L., Mackenzie, L., Willis, K., & Loh, S.Y. (2014). Women’s experiences of cognitive changes or ‘chemobrain’ following treatment for breast cancer: A role for occupational therapy? Australian Occupational Therapy Journal, 61(4), 230–240. https://doi.org/10.1111/1440-1630.12113
Reid, J., & Hardy, M. (1999). Multiple roles and well-being among midlife women: Testing role strain and role enhancement theories. Journals of Gerontology: Series B, 54B(6), S329–S338. https://doi.org/10.1093/geronb/54b.6.s329
Ridolfo, H., & Schoua-Glusberg, A. (2011). Analyzing cognitive interview data using the constant comparative method of analysis to understand cross-cultural patterns in survey data. Field Methods, 23(4), 420–438. https://doi.org/10.1177/1525822X11414835
Rodríguez Martín, B., Fernández Rodríguez, E.J., Rihuete Galve, M.I., & Cruz Hernández, J.J. (2020). Study of chemotherapy-induced cognitive impairment in women with breast cancer. International Journal of Environmental Research and Public Health, 17(23), 8896. https://doi.org/10.3390/ijerph17238896
Talley, A.E., Kocum, L., Schlegel, R.J., Molix, L., & Bettencourt, B.A. (2012). Social roles, basic need satisfaction, and psychological health: The central role of competence. Personality and Social Psychology Bulletin, 38(2), 155–173. https://doi.org/10.1177/0146167211432762
van Genderen, S., Plasqui, G., Lacaille, D., Arends, S., van Gaalen, F., van der Heijde, D., . . . Boonen, A. (2016). Social role participation questionnaire for patients with ankylosing spondylitis: Translation into Dutch, reliability and construct validity. RMD Open, 2(1), e000177. https://doi.org/10.1136/rmdopen-2015-000177
Von Ah, D., Habermann, B., Carpenter, J.S., & Schneider, B.L. (2013). Impact of perceived cognitive impairment in breast cancer survivors. European Journal of Oncology Nursing, 17(2), 236–241. https://doi.org/10.1016/j.ejon.2012.06.002




