Effects of the Use of the Provider Resilience Mobile Application in Reducing Compassion Fatigue in Oncology Nursing
Background: Oncology nurses have increased exposure to the prolonged illness, tragedy, loss, and premature death of patients. As a result, they are at higher risk for developing compassion fatigue.
Objectives: The aim of this study was to examine if use of the Provider Resilience mobile application (PRMA) will improve oncology nurses’ professional quality of life.
Methods: The quasiexperimental design was comprised of a longitudinal approach to evaluate the effect of an intervention program, PRMA, on professional quality of life between two nonrandomized groups (intervention and control) using pre- and post-tests in a sample of oncology RNs.
Findings: The findings of this study demonstrated no significant relationships between the intervention and control groups on secondary traumatic stress, compassion satisfaction, and burnout among oncology nurses.
Jump to a section
Oncology nurses are at particular risk for a type of secondary traumatic stress (STS) known as compassion fatigue (CF). Nurses with compassion fatigue have been reported to experience psychological, emotional, and, eventually, physical symptoms. Without intervention, CF can lead to nurses changing jobs or careers (Boyle, 2011). This study explores the effect of a convenient, low-cost, and accessible mobile application on professional quality of life of oncology nurses at risk for CF.
Literature Review
A review of the professional literature provided descriptions of CF among nurses and other members of helping professions. In Table 1, comparisons between CF and professional burnout illustrate the particular predisposition of nurses to CF related to the nature of their professional caring roles. 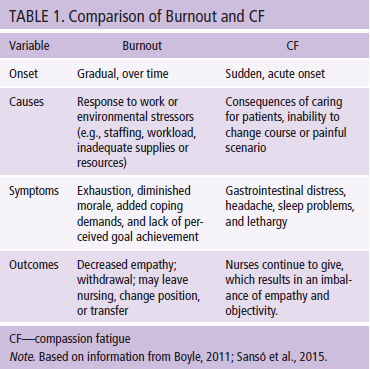
Potter et al. (2010) defined CF as “the traumatization of helpers through their effort at helping others” and as “a relational source of stress that also weighs heavily on oncology nurses” (p. E56). Several other definitions exist, and the nursing community has yet to reach a formal definition (Boyle, 2011). However, other definitions of CF share common descriptions of physical exhaustion and emotional distress resulting from close contact with patients and families. Nurses’ internalization of this suffering, combined with the inability to alleviate it, contributes to feelings of professional futility or self-blame. If these scenarios repeat without alleviation or attention, nurses begin to experience emotional detachment from patients and apathy toward the patient and family.
Similarities exist between CF and professional burnout, namely exhaustion, diminished morale, and lack of perceived goal achievement. Professional burnout arises from frustration when personal goals are not met, whereas CF evolves from perceived failure of rescue caretaking strategies (Valent, 2002). Nurses are particularly vulnerable to CF because they are partners, rather than observers, in patients’ healthcare journeys (Boyle, 2011). Oncology nurses have the added stress of working with a patient base in which survivorship is not guaranteed, contributing to “failure” of rescue caretaking strategies. In addition, oncology nurses working in mixed-model structures (serving curative and end-of-life patients) experience value conflicts that are confusing and taxing (Fillion et al., 2009).
Coetzee and Klopper (2010) suggested that, because CF has not been formally defined within nursing practice, the phenomenon has not been explored, described, or explained in a manner that would allow nurses to identify and combat CF effectively. However, long-term sequelae of unrecognized CF can be severe and lead to career changes. Radziewicz (2001) discussed the various domains in which CF symptoms are manifested. Symptoms are physical, behavioral, and spiritual, with spiritual being at the furthest end of the spectrum and the most severe and damaging (see Figure 1). 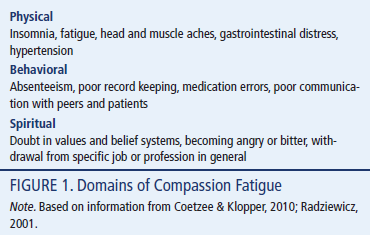
Aycock and Boyle (2009) surveyed national Oncology Nursing Society (ONS) members on the presence of workplace resources to combat CF. The most common reported resource (60%) was the employer-provided employee assistance program, but one can argue that this is not specifically aimed at CF for oncology nurses.
Other nurses reported simple unit-based practices to deal with staff bereavement, such as having memory walls, having quiet spaces, and sending sympathy cards to families after patient deaths have occurred. Potter, Deshields, and Rodriguez (2013) described more intense strategies involving provision of a comprehensive education program to staff in 90-minute sessions lasting five weeks (later modified to one-day workshops).
Although these extended studies succeeded in educating nurses on CF and its risks, not much data exist to support increased professional quality of life for nurses. Studies were also small (most with fewer than 50 participants) and used convenience samplings that limit generalization of findings. No published studies could be located in which technology was used as an intervention to combat CF or burnout.
Methods
Study Design
A prospective, quasiexperimental study was conducted in a 26-bed oncology unit at a medical center in California. The quasiexperimental design was comprised of a longitudinal approach to evaluate the effect of an intervention program, the Provider Resilience mobile application (PRMA), on professional quality of life between two nonrandomized groups (intervention and control) using pre- and post-tests in a sample of oncology RNs. At baseline, the intervention and control groups received CF education. The intervention group used the PRMA for six consecutive weeks. Both groups were evaluated at baseline and after completion of the six-week intervention. The institutional review board approved the study and study flyers. Informed consent was obtained from all participants.
Sample
Participants were recruited via advertisements asking for volunteers. Inclusion criteria were being aged 18 years and older, being fluent in English, being employed full-time as an oncology nurse, and owning a smartphone. A convenience sample was comprised of 25 clinical RNs from an inpatient oncology unit who attended the CF group education session. Participants were nonrandomly allocated to the intervention or control group, with 16 in the intervention group and 9 in the control group.
Data Collection
An educational inservice was given to all staff members to define CF and raise awareness. RN investigators then provided an accessible and convenient intervention to staff members in the intervention group via PRMA, which was developed by the Department of Defense to aid in alleviating CF among the social workers, nurses, and physicians who treat military service members (Bonanno, 2004). RN investigators invited staff members to download and use PRMA. PRMA use was monitored for a six-week period via tracking software, which participants downloaded onto their phones.
All participants in the control and intervention groups completed the Professional Quality of Life Scale (ProQOL) as a measurement tool pretest (prior to education and PRMA download) and post-test (following the six-week monitoring period).
Instrument
Professional Quality of Life Scale: The ProQOL 5 (http://bit.ly/1OWPcbA) is a 30-item instrument that uses a five-point Likert-type scale ranging from 1 (never) to 5 (very often) to assess the positive and negative quality-of-life elements that those in the helping professions experience in relation to their work (Stamm, 2010). The ProQOL 5 is comprised of three subscales: STS, compassion satisfaction, and burnout. STS and burnout are components of CF. STS addresses an individual’s exposure to extreme or stressful traumatic events in the workplace (Stamm, 2010).
Burnout is characterized by feelings of hopelessness and difficulty coping with work or performing one’s job effectively. Compassion satisfaction assesses the degree of pleasure derived from performing one’s job effectively (Stamm, 2010). Each subscale is comprised of 10 items, which asks participants to reflect on how frequently they experienced situations in their current work setting in the past 30 days. Higher scores on the compassion satisfaction subscale reflect greater work satisfaction, whereas higher scores on the burnout and STS subscales reflect greater difficulty related to feelings of job effectiveness (Stamm, 2010). Construct validity has been previously established (Stamm, 2010). Reliabilities (Cronbach alpha) are reported to range from 0.75–0.9 across all three subscales (Neville & Cole, 2013; Young, Derr, Cicchillo, & Bressler, 2011).
Provider Resilience mobile application: The goal of PRMA is to serve as a tool to increase provider resilience in the face of the demands on healthcare providers’ personal resources. PRMA provides the following:
• Psychoeducation about the risks of burnout, CF, and STS
• A method to evaluate healthcare providers’ level of burnout, CF, compassion satisfaction, and STS using a standardized assessment and a visual analog scale, which can be used to track symptoms and document change
• Tools that serve as reminders to healthcare providers to engage in self-care and brief interventions to increase resilience and reduce burnout
The resilience rating is based on the last ProQOL score, burnout rating, resilience builders and killers responses, and the last self-recorded vacation day.
The burnout rating is found through the burnout visual analog scale, which allows participants to rate themselves on 10 affective domains, including happy, trapped, satisfied, preoccupied, connected, worn out, caring, on edge, valued, and traumatized. The rating gives the participant a simple way to track his or her feelings in each of these areas over time.
The resilience builders and killers questionnaire is a short survey of different resilience builders and killers in which the participant may have engaged. In addition to affecting the resilience rating, this questionnaire can serve as a regular reminder of things to do—or not to do—to help the participant stay emotionally resilient.
If a participant’s overall resilience rating is low, he or she may be under a great deal of work-related stress. The participant is encouraged to use some of the built-in tools, like physical exercises, videos, and daily affirmations, to help the participant reconnect with the positive impact of his or her work.
The R&R Clock is an important feature of PRMA. PRMA reminds the participant to use vacation time. The R&R Clock counts the years, months, weeks, days, hours, minutes, and seconds since the user took a day off work.
Results
Sample Characteristics
Demographic and work-related characteristics of oncology nurse participants in the total sample and by treatment group are presented in Table 2. In the total sample, on average, most oncology nurses were aged 18–35 years, were female, and had five or fewer years of experience as an RN. More than half of all participants were ONS–certified and had five or fewer years of experience in oncology. 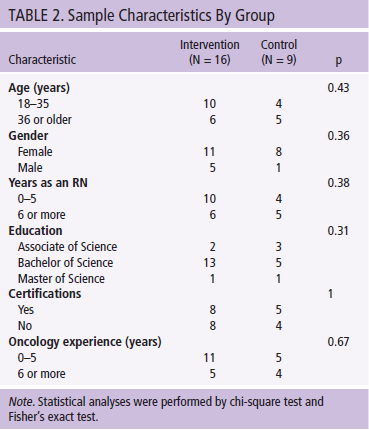
Bivariate analyses revealed that both groups were comparable in terms of age, gender, number of years as an RN, education level, certifications, and oncology experience. Of note, the topic of CF produced reported feelings of anxiety in one participant during the initial administration of the ProQOL. The participant chose to leave the study prior to using PRMA. The individual was given a list of referrals to follow up on potential negative results of CF. No other study participants reported negative effects of PRMA use.
According to the ProQOL suggested cutoffs, 14 of the 25 participants indicated that they had average STS at pretest, 17 reported high compassion satisfaction, and 15 reported low burnout.
At post-test, 8 participants indicated that they had low STS, 14 reported high compassion satisfaction, and 12 reported low burnout. No statistically significant differences were found when comparing levels of STS, compassion satisfaction, and burnout between intervention and control groups (see Table 3). 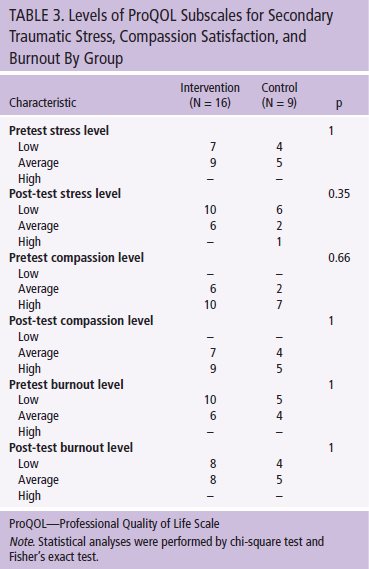
Differences between treatment groups for the ProQOL STS subscale from baseline (pretest) to week 6 (post-test) were not significant. In addition, no significant differences were found in the mean scores between the intervention and control groups for compassion satisfaction and burnout subscales. Improvements in ProQOL, as assessed by arithmetic mean change scores (mean difference) in overall ProQOL subscales for STS, compassion satisfaction, and burnout, were not significantly different between the intervention and control groups (see Table 4 and Figure 2). 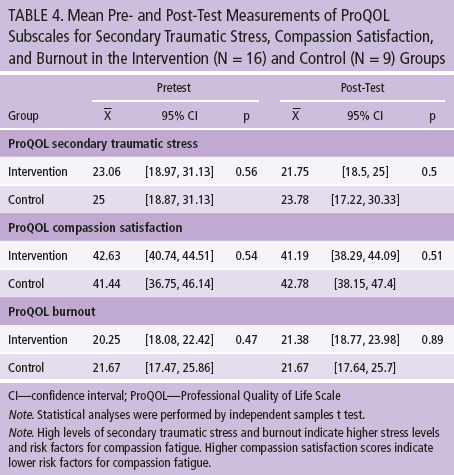
Discussion
The findings of the current study demonstrated no statistically significant relationships between the intervention and control groups on STS, compassion satisfaction, and burnout among oncology nurses. The study investigators hypothesized an inverse relationship in the intervention group between the pre- and post-test scores for STS. Such a relationship would indicate effectiveness of PRMA in reducing nurses’ stress.
Another expected outcome would have been a positive correlation in the intervention group between pretest burnout and STS scores. This relationship would indicate effectiveness of PRMA in improving the professional QOL of participants who had reported high stress and burnout levels prior to the intervention. In addition, investigators evaluated scores to determine whether the intervention group experienced higher levels of compassion satisfaction with lower levels of stress and burnout after six-week PRMA use when compared to the control group.
[[{"type":"media","view_mode":"media_original","fid":"27256","attributes":{"alt":"","class":"media-image","height":"258","typeof":"foaf:Image","width":"370"}}]]
Analysis
The current study was not statistically significant because no changes were seen in the pre- and post-test scores of the intervention group, control group, or sample as a whole. Changes in the numbers showed a nonsignificant relationship between pretest STS and pretest burnout, which could be argued as qualitative evidence of the relationship between STS and increased burnout in oncology nurses; conversely, nurses already suffering from burnout would be more susceptible to STS. Although the data neither support nor negate the hypothesis, not enough data demonstrated any difference between groups, and the investigators believe a larger study is warranted.
The results of this pilot feasibility study are preliminary and should be interpreted with caution. The sample was relatively small, and the post-hoc power analysis suggested low statistical power to detect significant differences. Participants were not randomized into the intervention or control group. Therefore, the difference in sample size between the two groups may have factored into the lack of differences because of the lack of power. Much of the information provided via the tracking software also focused on the technical aspects of PRMA, and such data were not related to the current study’s goals. The tracking software provided information regarding the amount of time each user spent on PRMA; however, time (measured in minutes) varied greatly among participants. In the end, these data were unreliable.
In addition to statistical and software limitations, logistical limitations were also discovered. The convenience sample of oncology nurses was derived from the same unit, which enforces a policy that prohibited cell phone use during work time (excluding breaks). No feasible methods were available to measure external sources of self-care used by the participants in conjunction with PRMA, which may have influenced their pre- and post-test scores. The ProQOL, although useful in theory because of its record of validity, was ultimately a challenging instrument to implement in the current study. The tool was challenging because it did not provide enough data to power the analysis. In addition, the authors hand-scored the scales, which was time consuming.
Implications for Practice
Lessons may be learned from the results of this pilot study. Because PRMA has not been previously studied in oncology nurses, the results of this pilot feasibility study can be used to inform a larger one. The lack of variability in pre- and post-test data may be an indicator that this particular application does not have an effect on professional quality of life among oncology nurses. However, testing the PRMA intervention requires a larger study, with a greater number of participants and data that could be more thoroughly analyzed. Additional investigations should clarify how to access more information about the PRMA application, how it works, and what information can be extracted from the tracking software’s study logs prior to initiating another study.
[[{"type":"media","view_mode":"media_original","fid":"27261","attributes":{"alt":"","class":"media-image","height":"231","typeof":"foaf:Image","width":"370"}}]]
Conclusion
Additional studies are needed to explore the use of technology to prevent CF and burnout and build resilience. A review of the literature revealed several studies that focused on the use of mobile applications for patient care, such as health prevention (Vodopivec-Jamsek, de Jongh, Gurol-Urganci, Atun, & Car, 2012), cancer pain management (Agboola et al., 2014), and use of a mobile application as a post-traumatic stress disorder (PTSD) coach (Owen et al., 2015). At the time of print, no new publications explored the use of technology to decrease CF, burnout, and PTSD in healthcare providers.
In conclusion, the literature suggests that CF is a significant problem among oncology nurses and that few interventions are effective in addressing it. Multiple intervention styles are needed to meet the varying needs of nurses, and the current study explored whether PRMA could be included in the arsenal of tools to combat the threat of CF. The small sample size in the current pilot study limited the generalizability of the findings; therefore, a larger sample is needed to explore potential effects of a mobile application on CF and burnout in this high-risk nursing population. Further research of PRMA and other technology-based tools is needed to prevent CF from subverting the dedication of oncology nurses.
[[{"type":"media","view_mode":"media_original","fid":"27456","attributes":{"alt":"","class":"media-image","height":"194","typeof":"foaf:Image","width":"768"}}]]
References
Agboola, S., Kamdar, M., Flanagan, C., Searl, M., Traeger, L., Kvedar, J., & Jethwani, K. (2014). Pain management in cancer patients using a mobile app: Study design of a randomized controlled trial. JMIR Research Protocols, 3, e76. doi:10.2196/resprot.3957
Aycock, N., & Boyle, D. (2009). Interventions to manage compassion fatigue in oncology nursing. Clinical Journal of Oncology Nursing, 13, 183–191. doi:10.1188/09.CJON.183-191
Bonanno, G.A. (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist, 59, 20–28. doi:10.1037/0003-066X.59.1.20
Boyle, D.A. (2011). Countering compassion fatigue: A requisite nursing agenda. Online Journal of Issues in Nursing, 16, 2. doi:10.3912/OJIN.Vol16No01Man02
Coetzee, S.K., & Klopper, H.C. (2010). Compassion fatigue within nursing practice: A concept analysis. Nursing and Health Sciences, 12, 235–243. doi:10.1111/j.1442-2018.2010.00526.x
Fillion, L., Duval, S., Dumont, S., Gagnon, P., Tremblay, I., Bairati, I., & Breitbart, W.S. (2009). Impact of a meaning-centered intervention on job satisfaction and on quality of life among palliative care nurses. Psycho-Oncology, 18, 1300–1310. doi:10.1002/pon.1513
Neville, K., & Cole, D.A. (2013). The relationships among health promotion behaviors, compassion fatigue, burnout, and compassion satisfaction in nurses practicing in a community medical center. Journal of Nursing Administration, 43, 348–354. doi:10.1097/NNA.0b013e3182942c23
Owen, J.E., Jaworski, B.K., Kuhn, E., Makin-Byrd, K.N., Ramsey, K.M., & Hoffman, J.E. (2015). mHealth in the wild: Using novel data to examine the reach, use, and impact of PTSD coach. JMIR Mental Health, 2, 1–9. doi:10.2196/mental.3935
Potter, P., Deshields, T., Divanbeigi, J., Berger, J., Cipriano, D., Norris, L., & Olsen, S. (2010). Compassion fatigue and burnout: Prevalence among oncology nurses. Clinical Journal of Oncology Nursing, 14, E56–E62. doi:10.1188/10.CJON.E56-E62
Potter, P., Deshields, T., & Rodriguez, S. (2013). Developing a systematic program for compassion fatigue. Nursing Administration Quarterly, 37, 326–332.
Radziewicz, R.M. (2001). Self-care for the caregiver. Nursing Clinics of North America, 36, 855–869.
Sansó, N., Galiana, L., Oliver, A., Pascual, A., Sinclair, S., & Benito, E. (2015). Palliative care professionals’ inner life: Exploring the relationships among awareness, self-care, and compassion satisfaction and fatigue, burnout, and coping with death. Journal of Pain and Symptom Management, 50, 200–207. doi:10.1016/j.jpainsymman.2015.02.013
Stamm, B.H. (2010). The concise ProQOL manual (2nd ed.). Pocatello, ID: ProQOL.org
Valent, P. (2002). Diagnosis and treatment of helper stresses, trauma and illnesses. In C.R. Figley (Ed.), Treating compassion fatigue (pp. 17–37). New York, NY: Brunner-Routledge.
Vodopivec-Jamsek, V., de Jongh, T., Gurol-Urganci, I., Atun, R., & Car, J. (2012). Mobile phone messaging for preventive health care. Cochrane Database of Systematic Reviews, 12, CD007457. doi:10.1002/14651858.CD007457.pub2
Young, J.L., Derr, D.M., Cicchillo, V.J., & Bressler, S. (2011). Compassion satisfaction, burnout, and secondary traumatic stress in heart and vascular nurses. Critical Care Nursing Quarterly, 34, 227–234. doi:10.1097/CNQ.0b013e31821c67d5
About the Author(s)
Patricia Jakel, RN, MN, AOCN®, is an advanced practice nurse, Jillian Kenney, RN, BSN, OCN®, is a clinical nurse II, and Natalia Ludan, RN, BSN, OCN®, is a clinical nurse III, all in the Solid Tumor Program at the University of California–Los Angeles (UCLA) Santa Monica Medical Center; Pamela S. Miller, PhD, RN, ACNP, CNS, is a nurse scientist in the Research and Evidence-Based Practice Program at UCLA Health System in Los Angeles; Norma McNair, PhD, RN, ACNS-BC, is a clinical nurse specialist at the Ronald Reagan UCLA Medical Center in Los Angeles; and Edith Matesic, DNP, RN, NEA-BC, is former chief nursing officer at UCLA Health System, all in California. The authors take full responsibility for the content of the article. The authors did not receive honoraria for their work. The content of this article has been reviewed by independent peer reviewers to ensure that it is balanced, objective, and free from commercial bias. No financial relationships relevant to the content of this article have been disclosed by the authors, planners, independent peer reviewers, or editorial staff. Jakel can be reached at pjakel@mednet.ucla.edu, with copy to editor at CJONEditor@ons.org. (Submitted November 2015. Revision submitted February 2016. Accepted for publication March 10, 2016.)




