Pediatric Patients and Dietary Choices: Examining Alternative Options, Decision Making, and Misinformation
Background: Nutrition is a key component of oncologic therapies and treatments. Patients and families are interested in the integration of alternative diets to promote therapy response as well as counteract the cancer. With the expansion of online and social media presence comes the endorsement of nonscientific claims.
Objectives: The purpose of this article is to review alternative diets and discuss the basis of good nutrition in pediatric patients with cancer. This article will also explore where patients and families are likely to seek their information and assess their level of trust in the information.
Methods: Five alternative diets and two supplements were assessed through a literature review for their effect on pediatric patients with cancer.
Findings: Additional research is needed to prove consistent and definitive dietary benefits for pediatric patients with cancer; however, some diets have demonstrated promising results. A general diet for pediatric patients with cancer consists of an appropriate distribution of nutritious carbohydrates, proteins, and fats. However, unregulated sources of information remain a risk.
Jump to a section
Well-balanced nutrition is a key component of oncology supportive care. It is associated with enhanced tolerance to therapies, improved survival, increased quality of life, and decreased adverse events during cancer treatments (Ladas et al., 2005). Alternative diets have been an ongoing, continually changing trend for decades. In the community of pediatric patients with cancer, patients and their families may explore alternative therapies and nutritional options. In addition, families of pediatric patients with cancer have expressed an interest in receiving detailed materials about nutrition (Arpaci et al., 2014) and have demonstrated obsessive and painstakingly close monitoring of their child’s eating habits after their child’s cancer diagnosis (Williams et al., 2015).
The 2018 Food and Health Survey, implemented by the International Food Information Council Foundation (IFICF, 2018), examined popular sources of nutrition information among Americans. Although participants reported that they have more trust in healthcare professionals and registered dietitians for nutrition information, their actual sources tended to be more socially based versus scientific; they often sought the advice of friends or family members, television, or information via social media (IFICF, 2018). Another study (Thomas et al., 2018) found that a similar percentage of participants had a comparable trust in information about cancer from watching television as they did from speaking with a physician. One of the major concerns with using media sources for nutrition or medical information is that there is little to no regulation for statements or claims. Korownyk et al. (2014) reviewed the quality of medical recommendations and claims made on daytime television shows. These television shows, combined, had an average of more than five million viewers daily; however, only about half of the claims on the shows had scientific evidence to support them (Korownyk et al., 2014).
According to Pennycook and Rand (2019), another obstacle in diminishing misinformation is that professional fact-checking mainly targets outright false material; it may miss content that is more biased or misleading. In addition, families may be unaware that what is being promoted may not be beneficial, or may be potentially harmful, to their child or adolescent with cancer. Nursing and clinical staff can support patients and their family members by understanding current diet trends in the oncology community, the potential for exposure to nonscientific information, and how to guide them to evidence-based decisions.
Current Diet Trends and Research
Plant-Based Diet
The two major diets that are most often considered as plant-based diets are vegetarian and vegan. Vegetarian diets are regarded as a diet that does not include meat, poultry, or fish (Academy of Nutrition and Dietetics, 2018). A vegan diet only includes foods from plants and eliminates all animal products, such as meat, animal fats, dairy, and eggs (American Institute for Cancer Research [AICR], 2019). There has been strong evidence that a plant-based diet can decrease the chance of developing many types of cancer, including female-specific cancers and adult cancers of the gastrointestinal tract (Tantamango-Bartley et al., 2013). There is limited research specifically on plant-based diets in pediatric patients with cancer. However, an article by Madigan and Karhu (2018) emphasizes that plant-based nutrition is associated with better overall health and prevention of chronic diseases in children. The article also highlights an important concept: the development of healthy habits at a young age may persist into adulthood and may prevent future disorders (Madigan & Karhu, 2018).
There are no published trials, studies, or case reports about the efficacy of a plant-based diet while a patient is undergoing cancer treatment and experiencing related symptoms (National Cancer Institute, 2019). However, there also are no data that any individual who was already following a plant-based diet before diagnosis should abandon it when beginning treatment (National Cancer Institute, 2019). Recommendations stress involving a dietitian to ensure that calorie, protein, and nutrient needs are adequate during and following cancer treatment (AICR, 2019; American Cancer Society [ACS], 2018; National Cancer Institute, 2019). Multiple nutrients are often lacking in a plant-based diet, such as calcium, vitamins D and B12, zinc, iron, and protein, and may require supplementation and appropriate planning (Mayo Clinic, 2019). Adopting a plant-based diet may provide benefits against a number of cancers, but additional research to establish the safety of this type of diet in pediatric patients must be examined.
Fasting or Calorie Restriction
Fasting, or food deprivation without water restriction, was a common practice in therapies for chronic illnesses, such as heart disease, as well as religious practices (UCSF Osher Center for Integrative Medicine, 2018). The concept of starving the cancer stems from the idea of denying the malignant cells with energy and resources to continue to grow and divide rapidly (Cathcart et al., 2017). Malignant cells have a higher metabolic rate and use glucose as their main source of energy (Cathcart et al., 2017). Some cancers express higher concentrations of insulin growth factor; fasting can decrease insulin growth factor concentrations, which ultimately leads to cell death (Cathcart et al., 2017). In addition, it has been suggested that fasting can reduce the levels of anabolic hormones, growth factors and inflammatory cytokines, oxidative stress, and cell proliferation while enhancing cell destruction and DNA repair (UCSF Osher Center for Integrative Medicine, 2018). A case study of 10 patients in Cathcart et al. (2017) revealed that intermittent fasting along with a chemotherapy regimen demonstrated decreased gastrointestinal side effects and fatigue. However, there are several serious concerns with fasting. Restricting food and calorie intake often requires extended periods of time (weeks to months) to generate the metabolic changes depicted (UCSF Osher Center for Integrative Medicine, 2018). It is widely recognized that calorie restriction or fasting is never recommended in certain populations, such as those who are underweight, seriously ill, or younger than age 18 years. Pediatric patients with cancer often fit these descriptions and, therefore, fasting is contraindicated.
Ketogenic Diet
A ketogenic diet consists of high fat, low carbohydrates, and adequate proteins (Weber et al., 2018). The ketogenic diet has gained popularity as a weight-loss diet and has had previous uses in controlling epilepsy. The idea behind incorporating a ketogenic diet into cancer treatment is to reduce blood glucose levels and induce ketosis so that cancer cells are starved of energy while normal cells adapt to use ketones and survive (Weber et al., 2018). In addition, decreased blood glucose causes insulin and insulin-like growth factor to drop, which are important drivers of cancer cell proliferation (Weber et al., 2018). Ketogenic diets have been applied to other neurologic disorders, such as epilepsy, which has inspired research in patients with brain tumors. In addition, some research has shown that normal brain cells may be able to metabolize ketones better in comparison to malignant cells (Oliveira et al., 2018).
A study by van der Louw et al. (2019) reported that a ketogenic diet used by three patients with diffuse intrinsic pontine gliomas, with no other treatment options, was safe for use in patients younger than age 18 years. However, the article mentions that patients’ prolonged survival cannot be attributed solely to the addition of a ketogenic diet (van der Louw et al., 2019). A study by Nebeling et al. (1995) examined glucose availability and uptake by neurologic tumors, specifically astrocytomas. Blood glucose levels were able to remain below normal to normal while increasing blood ketone levels 20- to 30-fold (Nebeling et al., 1995). Two patients demonstrated decreased glucose uptake at the tumor site on their positron-emission tomography scans (Nebeling et al., 1995). One of the patients displayed clinical improvement and did not have disease progression for 12 months (Nebeling et al., 1995). Data have shown the ketogenic diet’s potential in adjuvant therapies in brain tumors. However, most research to date has been conducted with small sample sizes, which does not provide definitive evidence to alter policies and treatment plans.
Macrobiotic Diet
The macrobiotic diet promotes a balance between life and nutrition while based on specifics from person to person; this includes level of activity, climate, and a person’s biological sex (National Cancer Institute, 2019). A macrobiotic diet focuses on whole grains, vegetables, and beans (Kushi Institute, 2020). Other foods, such as fish, fruits, and nuts, are permitted for occasional consumption (Kushi Institute, 2020). The diet discourages meats, animal products, dairy, sugars, and processed or refined foods (Kushi Institute, 2020). There is little data on the efficacy of the macrobiotic diet for patients with cancer, making its benefits and risks difficult to characterize (Rezash, 2008). The macrobiotic diet may be beneficial in decreasing the risk of some cancers in adults based on its limitation of red meats and refined foods in addition to the promotion of fibers and vegetables (Rezash, 2008). However, because the diet discourages fruit, meats, and dairy, patients may have insufficient calorie intake or necessary nutrients for growth and development (Dagnelie et al., 1994). Therefore, the diet may be unsuitable for infants and young children. In addition, if maintaining nutrition through adequate caloric intake and essential vitamins is of concern, this diet may be considered inappropriate and potentially harmful.
Paleolithic Diet
The concept of the Paleolithic diet, or paleo diet, is to mimic what humans presumably hunted, gathered, and ate during the Paleolithic Era: meat, animal products, fish and shellfish, fruits, vegetables, eggs, and nuts while excluding grains, dairy products, salt, or refined fats and sugar (Patel & Suleria, 2017). The theory supporting the paleo diet is to minimize processed food—a mainstay in modern diets—because those foods may increase chronic illness, including cancer (Zick et al., 2018). Research on the paleo diet targets adults; however, results from studies may inform diet recommendations in pediatrics. A study by Whalen et al. (2017), focusing on generalized chronic diseases, observed that diets more closely resembling paleo were conversely associated with disease-related mortality. A second study conducted by Whalen et al. (2016) described how paleo diet patterns may be associated with lower levels of systemic inflammation and oxidative stress. Although the data may suggest a benefit in preventing chronic illnesses, the diet does not adhere to ACS dietary recommendations. Paleo diets can lack whole grains, calcium, and vitamin D, which are important for growth and bone development in children (Rubio-López et al., 2017).
Probiotics
Probiotics may accompany regimens that include frequent antibiotics or gastrointestinal irritants to assist with side effects, boost immunity, and replenish the normal flora (Patel & Goyal, 2013). Studies indicate that probiotics may be helpful in reducing chemotherapy- and radiation-induced diarrhea and other gastrointestinal side effects (Du et al., 2018; Redman et al., 2014). A study by Du et al. (2018) reported the effects of probiotics, specifically Bacillus licheniformis, on pediatric patients with neurologic cancer undergoing radiation therapy. Patients who received probiotics had increased relief of gastrointestinal upset symptoms, such as mucositis, nausea and vomiting, diarrhea, and abdominal pain (Du et al., 2018). The study also measured inflammatory cytokine levels, which were lower in the patients who received probiotics (Du et al., 2018). Although rare, the introduction of microorganisms to an immunocompromised patient can increase the risk of probiotic-related sepsis (Redman et al., 2014). Ladas et al. (2016) examined the safety and efficacy of probiotics in pediatric patients receiving allogeneic bone marrow transplantation. The patients were given Lactobacillus plantarum during their myeloablative conditioning and after they were no longer considered neutropenic. No Lactobacillus plantarum–associated bacteremia presented in any of the patients (Ladas et al., 2016). In addition, about 70% of the patients did not develop acute graft-versus-host disease (Ladas et al., 2016). Finally, a study by Wada et al. (2010) demonstrated that the addition of probiotics, specifically Bifidobacterium breve strain Yakult, had several positive effects: decreased fevers, decreased need for IV antibiotics, maintained intestinal microflora, and reduced bacterial translocation. Patel and Goyal (2013) also focused on the possible anti-cancer properties of probiotics.
Melatonin
Melatonin is a natural hormone secreted by the pineal gland that regulates sleep–wake and reproductive cycles, as well as inhibits melanin formation (Talib, 2018). It is used as a natural sleep aid, but also has been studied for its tumor-targeting activity and ability to diminish treatment-related side effects (Talib, 2018). Talib (2018) found that adding melatonin to chemotherapy and/or radiation treatment may add to tumor response, perhaps because of the hormone’s inhibitory effects. By triggering cell differentiation, melatonin may impede and eliminate early-stage neuroblastoma (Lee at al., 2019). Studies have reported that melatonin may contribute to improved quality of life (National Cancer Institute, 2019). Johnston et al. (2019) examined the safety, tolerability, and response to high-dose melatonin administration in pediatric patients with relapsed solid tumors and found that the melatonin protocol was well tolerated. Lower incidences of cachexia, anorexia, and depression were reported (Johnston et al., 2019). These positive findings support further investigation of melatonin as a contributor to anticancer treatment.
Considerations
Most scientific claims and research are based on results in adult patients with cancer. The nutritional needs of adults are different from those of children and, therefore, should be taken into consideration when making any dietary decisions. In addition, with any supplements or herbals, there are no U.S. Food and Drug Administration (FDA) regulations that examine purity or safety. Supplements do not need to show safety before they are marketed to the public (FDA, 2015). Manufacturers do not need to prove that supplement claims are accurate and truthful before products are in the marketplace (FDA, 2015). Therefore, providers and/or dietitians can advise patients with cancer whether diet changes or the addition of supplements or herbals may negatively interact with their treatment.
The Basis of Appropriate Nutrition
Good nutrition is essential to tolerate an illness and associated treatments, but also critical in children to facilitate normal development. During chemotherapy, surgery, and radiation therapy, the patient is under increased levels of distress. To support activity, organ function, and energy, children in treatment require more calories. Rich proteins, carbohydrates, and fat are sources of calories. Protein is used to grow, rebuild, and repair tissues. These tissues include skin, the gastrointestinal lining, and hematopoietic cells (Wu, 2016). Protein malnutrition can lead to growth stunting, edema, vascular dysfunction, anemia, weakness, and impaired immunity (Wu, 2016). Carbohydrates are the body’s leading source of energy and help to maintain cellular structure (ACS, 2014). Therefore, carbohydrates are essential for proper organ function. Fats are another source of energy, in addition to insulating tissues and making certain vitamins available for use in the body (Harvard Medical School, 2019). Another benefit of fat is its high calorie per gram ratio, which is 9 for fat compared to 4 for proteins and carbohydrates (Harvard Medical School, 2019). This means that it is easier to ingest a larger number of calories in a smaller portion, which is helpful to patients with decreased appetite and wanting to gain weight. The percentages of each element should be based on the patient’s needs and agreed on by their provider and dietitian (ACS, 2014). Table 1 provides more information about each diet and how it compares to ACS recommendations. 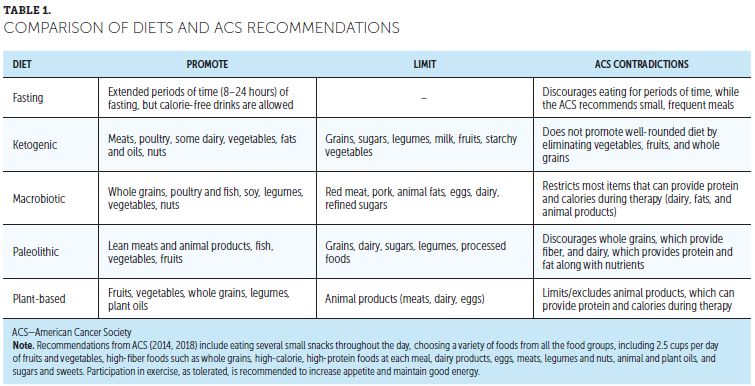
Discussion
The ACS (2014) provides dietary guidance for patients with cancer that can be achieved with an assortment of different dietary patterns. However, it should be noted that these alternative diets are not entirely consistent with recommendations; some restrict key elements that provide balanced nutrition, promote growth, and maintain a healthy weight during therapies. In addition, it should be considered that most research, if any, has insufficient qualitative and quantitative evidence while making clinical recommendations.
Consumers are at risk for not being able to differentiate between reputable, authentic information and falsified, discreditable claims. To make the best health and nutrition decisions, patients and family members should be aware of common red flags for misinformation. False claims can often guarantee a quick fix or simply sound too good to be true (Cleveland Clinic, 2017). Some statements claim that they are supported by research; however, the findings may be from a single study, have been refuted by reputable scientific organizations, or suggest simple conclusions made from complex research (Cleveland Clinic, 2017). Lastly, an immediate red flag should be any claim that promotes a specific product, plan, or person for likely financial gain (Cleveland Clinic, 2017).
It has been demonstrated that familiarity and well-known sources are preferred when retrieving information (Pennycook & Rand, 2019). Highly rigorous and precise resources that are less recognizable, despite their reputability, are often perceived as less trustworthy (Pennycook & Rand, 2019). However, as described in the 2018 Food and Health Survey (IFICF, 2018), there is expressed trust and interest in healthcare professionals and dietitians when obtaining nutrition information. Patients and families who have a strong and dependable bond with their medical team report more beneficial health behaviors and higher levels of satisfaction (Birkhäuer et al., 2017). Trust between patients and providers should encourage open discussion and education about nutrition.
Implications for Nursing
One of the most effective ways that nurses and practitioners can assist their patients’ nutrition concerns is to provide scientific, evidence-based education. Surveys have suggested that people appreciate the advice and input of healthcare professionals. In addition, strong and positive relationships between healthcare professionals and patients lead to better health outcomes (Birkhäuer et al., 2017). The nurse and the practitioner play a vital role in patient care by providing nutrition education (Arkansas State University, 2018). It is important to take advantage of opportunities to instruct patients and families on how to make better nutritional choices during all phases of therapy. By providing direction on how to identify questionable claims, as well as stressing vital nutrition for patients with cancer, healthcare providers can help to ease patient confusion and anxieties. To best educate patients and family members about healthy diet decisions without bias, nurses can have open conversations and provide direction to appropriate resources, such as the ACS guidelines (Zick et al., 2018). If patients or family members are receptive, nurses can provide informative and accurate scientific diet information (Arkansas State University, 2018). Consulting the dietitian is always warranted for patients and families who have questions about nutrition throughout the duration of therapy. Dietitians can provide appropriate nutrition choices and options for pediatric patients with cancer. Lastly, praise is key. Provide commendation to patients and family members for taking an interest in their health and asking questions to their healthcare team versus addressing their concerns alone or through less-credible sources. 
Conclusion
There has yet to be consistent and conclusive research demonstrating benefits for pediatric patients with cancer; however, some diets and supplements have produced encouraging results. Despite the benefits of online information and social media sources, it has become increasingly difficult to differentiate dietary claims that are scientifically proven or fabricated by non–research-based groups. Healthcare providers should use evidence-based information, such as the ACS guidelines, when discussing nutrition with pediatric patients with cancer and their families. 
About the Author(s)
Rebecca Zanecosky, MSN, CRNP, PNP-AC, is a pediatric nurse practitioner in the Division of Blood and Marrow Transplantation at the Children’s Hospital of Pittsburgh in Pennsylvania. The author takes full responsibility for this content and did not receive honoraria or disclose any relevant financial relationships. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Zanecosky can be reached at bzanecosky@gmail.com, with copy to CJONEditor@ons.org. (Submitted June 2019. Accepted November 26, 2019.)


