Burnout Among Oncology Nurses: The Effects of Providing a Primary Palliative Care Intervention Using CONNECT Protocol
Background: Palliative care clinicians display less burnout than oncology clinicians. Little is known about the impact of providing both oncology care and primary palliative care in the same setting.
Objectives: The aim was to determine whether nurses providing primary palliative care in addition to oncology care would experience less burnout over time than nurses providing oncology care only.
Methods: The authors performed secondary analysis of the CONNECT study. Three groups of nurses were evaluated: primary palliative care, non–primary palliative care, and standard care. On study enrollment and after one year, nurses completed the Maslach Burnout Inventory. Multivariable regression analyses were performed to test differences in follow-up burnout scores between groups.
Findings: Overall burnout rates were low at enrollment for all groups. There were no differences in burnout scores at one year between nurses who provided palliative care and nurses in the other two groups.
Jump to a section
Burnout is the feeling of exhaustion associated with work-related chronic stress and is highly prevalent and problematic among all healthcare providers, including nurses (de Lima Garcia et al., 2019; Shah et al., 2021). The syndrome was first recognized and studied among workers in human services and education in the 1970s and was subsequently characterized using the following three dimensions: emotional exhaustion, depersonalization, and decreased personal accomplishment (Maslach et al., 1986; Schaufeli et al., 2009). Burnout has serious implications for patients and nurses and has been linked with worsened patient safety and quality of care (Jun et al., 2021; Maslach et al., 1986; Schaufeli et al., 2009). For healthcare providers, burnout is associated with poor psychological and physical health, including sleep disorders (Al Maqbali et al., 2021), anxiety and depression (Koutsimani et al., 2019), health-related quality of life (Gomez-Urquiza et al., 2016; Ruiz-Fernández et al., 2020), substance use disorders (Murali et al., 2018), and work–life imbalance (Boamah et al., 2017).
In clinical oncology nursing practice, high exposure to life-limiting illness has been associated with increased emotional exhaustion and burnout (Cañadas-de la Fuente et al., 2018). Although provider burnout may be expected in palliative care settings, palliative care clinicians appear to be at lower risk for burnout than those in other fields, such as critical care and oncology (Parola et al., 2017; Pereira et al., 2016). Communication training and support for engaging in difficult conversations about end-of-life issues are possible protective factors against burnout for palliative care and oncology clinicians and are valued by nurses who receive specialized training (Dijxhoorn et al., 2021; Kubota et al., 2016). However, little is known about the impact on clinician burnout of providing both oncology care and primary palliative care in the same setting.
This trial provides a unique opportunity to examine the impact of providing nurse-led primary palliative care in addition to oncology care on burnout scores among oncology nurses. The authors hypothesized that nurses providing primary palliative care in addition to standard oncology care would experience decreased burnout over time when compared to nurses providing standard oncology care only.
Methods
This is a secondary analysis of data from the Care Management by Oncology Nurses to Address Supportive Care Needs (CONNECT) study, a cluster randomized trial of a primary palliative care intervention for patients with advanced cancer (ClinicalTrials.gov identifier NCT02712229). Details of the primary study design have been published previously (Becker et al., 2017; Cohen et al., 2021; Robbins-Welty et al., 2018). Seventeen oncology practices were randomized to either implement primary palliative care in addition to standard oncology care (n = 9) or to continue to provide standard oncology care alone (n = 8). The hypothesis was that nurses who were asked to integrate primary palliative care into routine oncology care would experience lower levels of burnout than those who did not have this additional training and skill. The study was approved by the University of Pittsburgh Institutional Review Board.
Participants and Setting
For this study, all oncology nurses were enrolled from general medical oncology practices in western Pennsylvania from July 2016 through October 2020. Practices were community-based in suburban and rural areas within a larger cancer care network. Among oncology practices randomized to implement the primary palliative care intervention, select nurses were trained to provide primary palliative care in addition to their main roles as oncology infusion room nurses for patients with advanced cancer. Participating sites nominated nurses based on strong relationships with clinicians and staff, communication and interpersonal skills, interest in learning new skills, and a commitment to palliative oncology care.
Nurses were categorized into three groups as follows: (a) nurses who provided primary palliative care via the CONNECT intervention (PPC RNs), (b) nurses who worked at primary palliative care sites but did not implement the intervention (non-PPC RNs), and (c) nurses at standard care sites (SC RNs). Standard care sites provided oncology care according to best practices; this included supportive measures as deemed appropriate by the oncology team. These groups were selected to determine if implementing primary palliative care decreased nurse burnout and if the provision of primary palliative care may have affected other nurses at intervention sites.
Intervention: CONNECT Protocol
PPC RNs were oncology infusion room nurses chosen by clinic leadership to participate as CONNECT nurses. They attended an intensive three-day, in-person training covering the following four key domains of primary palliative care: symptom assessment and management, emotional support, engaging patients and caregivers in advance care planning, and care coordination. The training included didactic content as well as role-playing scenarios with standardized patients. In addition, PPC RNs had at least monthly one-on-one check-in sessions with the study’s nurse project manager and attended half-day booster education sessions twice yearly to refresh and practice primary palliative care skills.
Primary palliative care visits were scheduled with PPC RNs either before or after regularly scheduled oncology visits and were designed to occur at least monthly for three months. The first visit focused on establishing rapport, addressing symptom needs, and choosing a surrogate decision maker. Subsequent visits focused on treatment preferences, discussions with family, questions for the oncologist, and goals for the future. Visits were guided by patient-reported outcomes, including distress and symptom scores. After all visits, the PPC RN coordinated treatment recommendations with the patient’s oncologist (either in person, by telephone, or by email) and followed up with the patient or caregiver by telephone to ensure the care plan was working and to answer any questions. PPC RNs provided primary palliative care to one to four patients at any one time, with schedules adjusted so that the other clinic RNs were assigned to allow the PPC RNs to fill this role.
Data Collection
Data for the nurses enrolled in the study were collected at the time of nurse enrollment into CONNECT (baseline) and one year later. Surveys were administered via email or on paper, with as many as four email reminders to maximize completion rates. All study documents (electronic and paper) identified patients using only their study IDs to maintain confidentiality. Paper documents were stored securely in the research office in locked cabinets and entered into a secure web-based data management system by staff using a two-step data verification process.
Measures
The Maslach Burnout Inventory (MBI) was used to evaluate nurse burnout. The MBI is a 22-item survey that has been validated across multiple occupational settings in the evaluation of burnout and takes about 15 minutes to complete (Maslach et al., 1986). The 22 items are measured on a Likert-type scale ranging from 0 to 6. Three subscores correspond to each burnout dimension as follows: emotional exhaustion (feelings of energy depletion), depersonalization (increased mental distance from one’s job or feelings of negativism), and decreased personal accomplishment (reduced personal efficacy). Each subscale is scored differently. Emotional exhaustion scores range from 0 to 54, with 27 or more considered high, 17–26 considered moderate, and less than 17 considered low. Depersonalization scores range from 0 to 30, with 13 or more considered high, 7–12 considered moderate, and less than 7 considered low. Personal accomplishment scores range from 0 to 48, with 39 or more considered high, 32–38 considered moderate, and less than 32 considered low. High emotional exhaustion and depersonalization scores correlate with increased burnout. In contrast, low personal accomplishment scores correlate with higher burnout.
For all study groups, demographic information captured at baseline included age, gender, race, years practicing in oncology, and amount of time spent in the clinic.
Statistical Methods
Baseline characteristics of the nurses were reported as means and standard deviations for continuous variables and frequencies (percentages) for categorical variables; comparisons of the baseline characteristics between nurse groups were performed using analysis of variance for continuous variables and Fisher’s exact tests for categorical variables. Baseline burnout scores were reported as means and standard deviations overall and by intervention group. All statistical analyses were performed using SAS, version 9.4.
To explore the hypothesis that burnout would be lower among nurses providing primary palliative care in addition to standard oncology care, comparisons between baseline and one-year scores were performed. Multivariable regression analyses were performed to test differences in follow-up burnout scores between nurse groups while adjusting for the baseline score. This was performed among the following three groups of nurses: PPC RNs, non-PPC RNs, and SC RNs. The analysis was performed in this manner to detect any effect of performing the primary palliative care intervention or being employed at a center where the intervention took place. The alpha of 0.05 threshold was used to test for statistical significance; no adjustments were made for multiple comparisons. A p value less than 0.05 was considered statistically significant.
Results
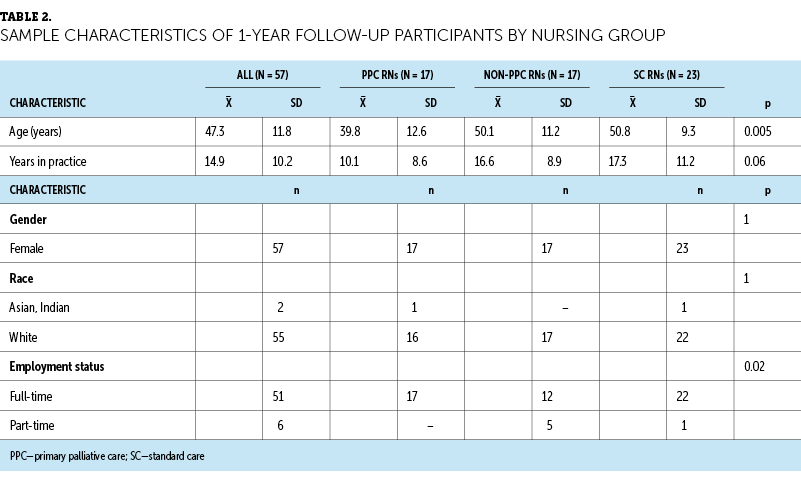
At baseline, 89 RNs from the 17 sites completed the MBI survey. The average age was 46.1 years (SD = 12), and 99% were female. The average number of years practicing in oncology was 13.2 (SD = 10.1), and 88% of RNs worked full-time. PPC RNs were younger than non-PPC and SC RNs at 38.6 years (SD = 12.2) compared to 49.8 years (SD = 12) and 47.4 years (SD = 10.5), respectively (p = 0.003) (see Table 1). Fifty-seven RNs completed the follow-up MBI survey at one year, with similar demographics presented in Table 2. The average age was 47.3 years (SD = 11.8), all were female, the average years in oncology practice was 14.9 (SD = 10.2), and 90% worked full-time. PPC RNs were again younger than nurses in the other two groups (PPC RNs: mean = 39.8 years, SD = 12.6; non-PPC RNs: mean = 50.1 years, SD = 11.2; and SC RNs: mean = 50.8 years, SD = 9.3).
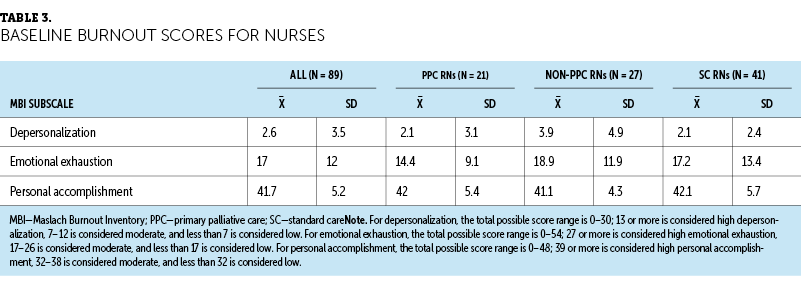
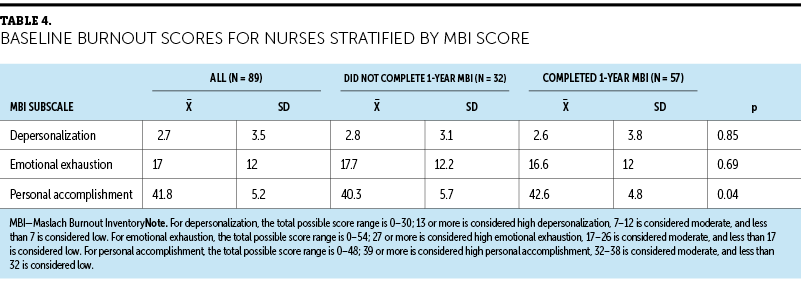
Burnout scores of nurses on enrollment into the study are presented in Table 3. The mean baseline score of emotional exhaustion for all nurses was 17 (SD = 12), which is on the border of low and moderate levels of burnout. PPC RNs had low baseline emotional exhaustion scores (mean = 14.4, SD = 9.1), and non-PPC RNs (mean = 18.9, SD = 11.9) and SC RNs (mean = 17.2, SD = 13.4) scored moderately. All three groups of nurses scored low on depersonalization (mean = 2.6, SD = 3.5) and high on personal accomplishment (mean = 41.7, SD = 5.2). Overall, these groups of nurses did not appear to experience high levels of burnout. There were no significant differences among baseline burnout scores of nurses who completed the follow-up MBI at one year and those who did not (see Table 4).
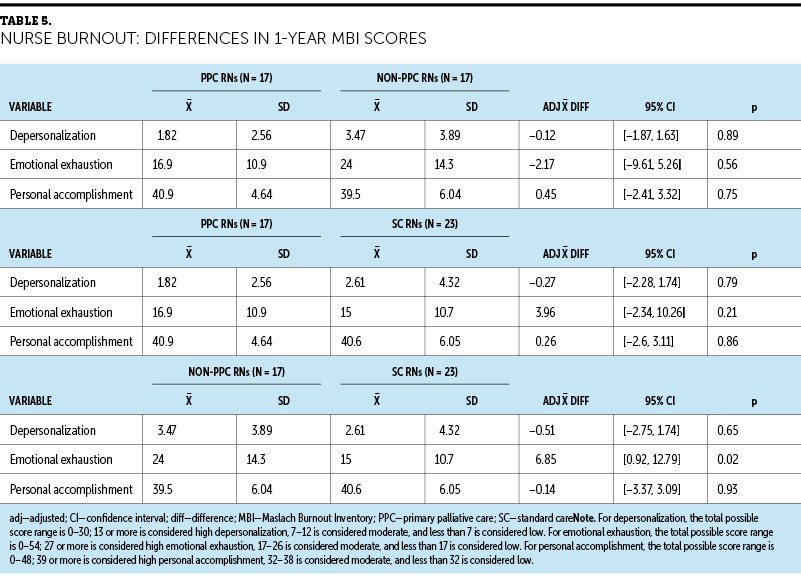
No significant decreases in burnout scores were observed among nurses after one year of implementation of the primary palliative care intervention (see Table 5). Emotional exhaustion scores remained borderline low to moderate among all groups. PPC RNs reported mean emotional exhaustion scores of 16.9 (SD = 10.9), compared to 24 (SD = 14.3) reported by non-PPC RNs (adjusted mean difference = –2.17; 95% confidence interval [CI] [–9.61, 5.26]; p = 0.56) and 15 (SD = 10.7) by SC RNs (adjusted mean difference = 3.96; 95% CI [–2.34, 10.26]); p = 0.21). Non-PPC RNs reported greater emotional exhaustion than SC RNs (adjusted mean difference = 6.85; 95% CI [0.92, 12.79]; p = 0.02). Depersonalization remained low and personal accomplishment high among all three groups, with no statistical significance. PPC RNs did not report a greater decrease in burnout scores than nurses in the other two groups.
Discussion
Studies have not evaluated the effect of providing primary palliative care and oncology care on nurse burnout. In this analysis, implementation of a primary nurse–led palliative care intervention (CONNECT protocol) did not affect burnout scores among nurses in community oncology clinics. Nurses’ scores did not indicate high levels of burnout on the MBI in any group at baseline or one year after the intervention; personal accomplishment remained high, and emotional exhaustion and depersonalization remained low.
This study hypothesized that the additional communication training (supporting the CONNECT protocol) the PPC RNs received would be protective against burnout, as had been observed in previous studies (Clayton et al., 2019; Dijxhoorn et al., 2021). Nurses have numerous hours of contact, communication, and physical interaction with patients throughout the patient’s diagnosis and treatment, and lacking resources to act on patient suffering can lead to more distress among nurses (Murali et al., 2018; Wu et al., 2016). The challenge of these situations and witnessing of patients’ difficulties during the cancer experience can lead to emotional exhaustion and depersonalization (Brady et al., 2020; Gomez-Urquiza et al., 2016; Parola et al., 2017). The CONNECT intervention empowered and supported nurses to act on patient distress by providing a protocol to communicate symptom needs and patient concerns to providers. In addition, the twice-yearly booster sessions allowed nurses to come together, formally debrief, and receive further coaching.
However, these effects may have been offset by the additional tasks required of the nurses who implemented the CONNECT protocol intervention on top of their typical duties. The roles of infusion room nurses are normally task-oriented and time-constrained. The CONNECT protocol intervention necessitated increased focus on the psychosocial needs of patients, and although nurses reported satisfaction with this role, they also discussed feeling pulled in multiple directions by their responsibilities (Feldenzer et al., 2019). In addition, emotional exhaustion was significantly higher at one year at the CONNECT protocol intervention sites among nurses who did not implement the intervention than among nurses at control sites. Although it is not possible to claim that this was a direct result of the intervention, nurses who were not chosen to be PPC nurses had to absorb some of the PPC RNs’ workload to allow time for the PPC RNs to practice the CONNECT protocol intervention.
Ultimately, results from the primary CONNECT protocol intervention did not show improved patient-reported outcomes at three months, although there was an improvement in patient symptoms among those who received more frequent primary palliative care visits (Schenker et al., 2021). An increased “dose intensity” of primary palliative care delivery may be needed to see improvement in patient outcomes (Schenker et al., 2021). If primary palliative care protocol interventions are added to RNs’ responsibilities, consideration will need to be given for how best to protect RNs’ time and ensure they are not merely being tasked with additional work.
Limitations
This study has several limitations. First, this is a secondary analysis that does not allow for inferences of causality. Other efforts to improve staff morale and wellness may have been in place at the study sites, confounding burnout effects of the CONNECT protocol intervention. Of note, MBI scores for all groups did not indicate high baseline levels of burnout. Another consideration is whether the MBI was the appropriate assessment tool given low levels of burnout; nurses may have experienced distress that was not captured by the MBI. Second, this was a small sample size with a lack of diversity. Nearly all the nurses included in this analysis were White and female. Third, study sites were largely rural/suburban and community-oriented, as opposed to sites situated in urban, academic-affiliated oncology practices. Therefore, these results may not generalize to nurses from other backgrounds or in other clinical settings. In addition, fewer nurses completed the MBI at one year than at baseline. Possibly, nurses experiencing higher burnout chose not to complete an additional survey or did not have time to do so amid their other duties. However, baseline burnout scores between those who followed up and those who did not were not significantly different. Staff turnover also may have been a factor because nurses may have chosen to seek employment elsewhere to relieve themselves from burnout (Shah et al., 2021). Finally, this study only measured two time points during the course of one year. Burnout scores could have increased with the initial burden of the CONNECT protocol intervention and subsequently leveled over time. The long-term effects of providing primary palliative care in addition to standard oncology care require further study.
Implications for Nursing
Findings from this study can support clinical oncology nurses in practice. The American Society of Clinical Oncology updated its guidelines in 2016 to recommend early, concurrent palliative care for patients with advanced cancer (Ferrell et al., 2017). Because specialty palliative care providers are limited, research to identify strategies for extending palliative care to more patients is ongoing, with this study as part of these efforts. Oncology nurses are at high risk for burnout, yet findings from this study indicate that levels of burnout in oncology infusion room nurses are low at baseline. It also suggests that providing primary palliative care in addition to oncology care does not appear to affect burnout. If adding primary palliative care to nursing practice is intended to increase patient access to palliative care, clinical practice models can prioritize nurse well-being. Adding palliative care to nursing practice can also extend palliative care to more patients with advanced cancer.
Conclusion
Burnout is a serious and increasingly common problem among healthcare providers involved in cancer care. Increased workload, extensive working hours, and significant patient acuity place nurses at risk for burnout, which negatively affects patient outcomes, quality care, and personal health. Oncology nurses who participated in this study using the primary CONNECT protocol intervention reported low levels of burnout before and after implementation of the intervention. As oncology practice evolves to encompass primary palliative care, nursing delivery models require limiting additional stress for nursing staff. These findings suggest that a strategy to provide primary palliative care may be implemented by oncology nurses safely with regards to burnout.
About the Authors
Jessica B. Cohen, MD, is an internal medicine resident physician in the Division of General Internal Medicine at the University of Pittsburgh Medical Center (UPMC), Victoria L. Reiser, AG-ACDNP, is a nurse practitioner in the Division of Hematology Oncology at the UPMC Hillman Cancer Center (HCC), Andrew D. Althouse, PhD, is an assistant professor of medicine in the Division of Internal General Medicine and the Center for Clinical Trials and Data Coordination, and Judith M. Resick, MSN, MPH, RN, is a nurse research program manager in the Palliative Research Center (PaRC) and Section of Palliative Care and Medical Ethics in the Division of General Internal Medicine, all at the University of Pittsburgh in Pennsylvania; Edward Chu, MD, MMS, is the director of the Albert Einstein Cancer Center at the Albert Einstein College of Medicine and vice president of cancer medicine at Montefiore Medical Center in Bronx, NY; Thomas J. Smith, MD, FACP®, FASCO, FAAHPM, is the director of palliative medicine in the Division of General Internal Medicine in the Section of Palliative Medicine in the School of Medicine at Johns Hopkins University and the Sidney Kimmel Comprehensive Cancer Center in Baltimore, MD; and Robert M. Arnold, MD, FACP®, FAAHPM, is a distinguished professor of medicine in the Section of Palliative Care and Medical Ethics in the PaRC and Section of Palliative Care and Medical Ethics in the Division of General Internal Medicine in the School of Medicine, Margaret Q. Rosenzweig, PhD, FNP-BC, AOCNP®, FAAN, is a professor in the School of Nursing, and Yael Schenker, MD, MAS, FAAHPM, is a professor of medicine in the Section of Palliative Care and Medical Ethics in the Division of General Internal Medicine and the director of the PaRC, all at the University of Pittsburgh. Rosenzweig and Schenker are dual senior authors. This study was supported by National Cancer Institute grant R01CA197103 and National Institute on Aging grant K24AG070285. This trial also used resources provided through the UPMC HCC Clinical Protocol and Data Management and HCC Protocol Review and Monitoring System, which are supported, in part, by award P30CA047. This study was also supported by the PaRC at the University of Pittsburgh. The authors have no conflicts of interest to disclose. The authors take full responsibility for this content. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias. Cohen can be reached at cohenjb@upmc.edu, with copy to CJONEditor@ons.org. (Submitted February 2022. Accepted April 20, 2022.)
References
Al Maqbali, M., Al Sinani, M., & Al-Lenjawi, B. (2021). Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Psychosomatic Research, 141, 110343. https://doi.org/10.1016/j.jpsychores.2020.110343
Becker, C.L., Arnold, R.M., Park, S.Y., Rosenzweig, M., Smith, T.J., White, D.B., . . . Schenker, Y. (2017). A cluster randomized trial of a primary palliative care intervention (CONNECT) for patients with advanced cancer: Protocol and key design considerations. Contemporary Clinical Trials, 54, 98–104. https://doi.org/10.1016/j.cct.2017.01.005
Boamah, S.A., Read, E.A., & Spence Laschinger, H.K. (2017). Factors influencing new graduate nurse burnout development, job satisfaction and patient care quality: A time-lagged study. Journal of Advanced Nursing, 73(5), 1182–1195. https://doi.org/10.1111/jan.13215
Brady, K.J.S., Ni, P., Sheldrick, R.C., Trockel, M.T., Shanafelt, T.D., Rowe, S.G., . . . Kazis, L.E. (2020). Describing the emotional exhaustion, depersonalization, and low personal accomplishment symptoms associated with Maslach Burnout Inventory subscale scores in US physicians: An item response theory analysis. Journal of Patient-Reported Outcomes, 4(1), 42. https://doi.org/10.1186/s41687-020-00204-x
Cañadas-de la Fuente, G.A., Gómez-Urquiza, J.L., Ortega-Campos, E.M., Cañadas, G.R., Albendín-García, L., & De la Fuente-Solana, E.I. (2018). Prevalence of burnout syndrome in oncology nursing: A meta-analytic study. Psycho-Oncology, 27(5), 1426–1433. https://doi.org/10.1002/pon.4632
Clayton, M.F., Iacob, E., Reblin, M., & Ellington, L. (2019). Hospice nurse identification of comfortable and difficult discussion topics: Associations among self-perceived communication effectiveness, nursing stress, life events, and burnout. Patient Education and Counseling, 102(10), 1793–1801. https://doi.org/10.1016/j.pec.2019.06.013
Cohen, M.G., Althouse, A.D., Arnold, R.M., Bulls, H.W., White, D., Chu, E., . . . Schenker, Y. (2021). Is advance care planning associated with decreased hope in advanced cancer? JCO Oncology Practice, 17(2), e248–e256. https://doi.org/10.1200/OP.20.00039
de Lima Garcia, C., de Abreu, L.C., Ramos, J.L.S., de Castro, C.F.D., Smiderle, F.R.N., dos Santos, J.A., & Bezerra, I.M.P. (2019). Influence of burnout on patient safety: Systematic review and meta-analysis. Medicina, 55(9), 553. https://doi.org/10.3390/medicina55090553
Dijxhoorn, A.-F.Q., Brom, L., van der Linden, Y.M., Leget, C., & Raijmakers, N.J. (2021). Prevalence of burnout in healthcare professionals providing palliative care and the effect of interventions to reduce symptoms: A systematic literature review. Palliative Medicine, 35(1), 6–26. https://doi.org/10.1177/0269216320956825
Feldenzer, K., Rosenzweig, M., Soodalter, J.A., & Schenker, Y. (2019). Nurses’ perspectives on the personal and professional impact of providing nurse-led primary palliative care in outpatient oncology settings. International Journal of Palliative Nursing, 25(1), 30–37. https://doi.org/10.12968/ijpn.2019.25.1.30
Ferrell, B.R., Temel, J.S., Temin, S., Alesi, E.R., Balboni, T.A., Basch, E.M., . . . Smith, T.J. (2017). Integration of palliative care into standard oncology care: American Society of Clinical Oncology clinical practice guideline update. Journal of Clinical Oncology, 35(1), 96–112. https://doi.org/10.1200/JCO.2016.70.1474
Gomez-Urquiza, J.L., Aneas-Lopez, A.B., De la Fuente-Solana, E.I., Albendin-Garcia, L., & Diaz-Rodriguez, L. (2016). Prevalence, risk factors, and levels of burnout among oncology nurses: A systematic review—ProQuest. Oncology Nursing Forum, 43(3), E104–E120. https://doi.org/10.1188/16.ONF.E104-E120
Jun, J., Ojemeni, M.M., Kalamani, R., Tong, J., & Crecelius, M.L. (2021). Relationship between nurse burnout, patient and organizational outcomes: Systematic review. International Journal of Nursing Studies, 119, 103933. https://doi.org/10.1016/j.ijnurstu.2021.103933
Koutsimani, P., Montgomery, A., & Georganta, K. (2019). The relationship between burnout, depression, and anxiety: A systematic review and meta-analysis. Frontiers in Psychology, 10, 284. https://doi.org/10.3389/fpsyg.2019.00284
Kubota, Y., Okuyama, T., Uchida, M., Umezawa, S., Nakaguchi, T., Sugano, K., . . . Akechi, T. (2016). Effectiveness of a psycho-oncology training program for oncology nurses: A randomized controlled trial. Psycho-Oncology, 25(6), 712–718. https://doi.org/10.1002/pon.4000
Maslach, C., Jackson, S., Leiter, M.P., Schaufeli, W.B., & Schwab, R. (1986). Maslach Burnout Inventory (vol. 21). Consulting Psychologists Press.
Murali, K., Makker, V., Lynch, J., & Banerjee, S. (2018). From burnout to resilience: An update for oncologists. American Society of Clinical Oncology Educational Book, 38, 862–872. https://doi.org/10.1200/EDBK_201023
Parola, V., Coelho, A., Cardoso, D., Sandgren, A., & Apóstolo, J. (2017). Prevalence of burnout in health professionals working in palliative care: A systematic review. JBI Evidence Synthesis, 15(7), 1905–1933. https://doi.org/10.11124/JBISRIR-2016-003309
Pereira, S.M., Teixeira, C.M., Carvalho, A.S., & Hernández-Marrero, P. (2016). Compared to palliative care, working in intensive care more than doubles the chances of burnout: Results from a nationwide comparative study. PLOS ONE, 11(9), e0162340. https://doi.org/10.1371/journal.pone.0162340
Robbins-Welty, G.A., Mueser, L., Mitchell, C., Pope, N., Arnold, R., Park, S., . . . Schenker, Y. (2018). Interventionist training and intervention fidelity monitoring and maintenance for CONNECT, a nurse-led primary palliative care in oncology trial. Contemporary Clinical Trials Communications, 10, 57–61. https://doi.org/10.1016/j.conctc.2018.03.006
Ruiz-Fernández, M.D., Ortega-Galán, Á.M., Fernández-Sola, C., Hernández-Padilla, J.M., Granero-Molina, J., & Ramos-Pichardo, J.D. (2020). Occupational factors associated with health-related quality of life in nursing professionals: A multi-centre study. International Journal of Environmental Research and Public Health, 17(3), 982. https://doi.org/10.3390/ijerph17030982
Schaufeli, W.B., Leiter, M.P., & Maslach, C. (2009). Burnout: 35 years of research and practice. Career Development International, 14(3), 204–220. https://doi.org/10.1108/13620430910966406
Schenker, Y., Althouse, A.D., Rosenzweig, M., White, D.B., Chu, E., Smith, K.J., . . . Arnold, R.M. (2021). Effect of an oncology nurse–led primary palliative care intervention on patients with advanced cancer: The CONNECT cluster randomized clinical trial. JAMA Internal Medicine, 181(11), 1451–1460. https://doi.org/10.1001/jamainternmed.2021.5185
Shah, M.K., Gandrakota, N., Cimiotti, J.P., Ghose, N., Moore, M., & Ali, M.K. (2021). Prevalence of and factors associated with nurse burnout in the US. JAMA Network Open, 4(2), e2036469. https://doi.org/10.1001/jamanetworkopen.2020.36469
Wu, S., Singh-Carlson, S., Odell, A., Reynolds, G., & Su, Y. (2016). Compassion fatigue, burnout, and compassion satisfaction among oncology nurses in the United States and Canada. Oncology Nursing Forum, 43(4), E161–E169. https://doi.org/10.1188/16.ONF.E161-E169