Adverse Childhood Experiences and Preventive Cervical Cancer Screening Behavior
Objectives: To examine associations between a history of adverse childhood experiences (ACEs) and receiving preventive cervical cancer screening and to investigate whether number and type of ACE exposures were predictive of cervical cancer screening uptake.
Sample & Setting: Data were from 11,042 adults who completed the 2020 Texas Behavioral Risk Factor Surveillance System survey. The U.S. Preventive Services Task Force guidelines were used to indicate whether individuals had received cervical cancer screening at recommended intervals.
Methods & Variables: Multiple logistic regression analysis was used to predict the likelihood of not having received the recommended preventive cancer screening by number and type of ACE exposures. Chi-square analysis was used to determine associations among demographic characteristics, cancer screening uptake, and ACE number and type.
Results: Individuals with one to three ACEs and those with six or more ACEs were statistically more likely not to have received the recommended cervical cancer screenings compared to those with zero ACEs. A history of physical ACEs was associated with 3.88 times the likelihood of not having received the recommended cervical cancer screening.
Implications for Nursing: To promote timely cervical cancer screening and prevent retraumatization of patients with a history of ACEs, providers should implement trauma-informed care principles in their healthcare settings.
Jump to a section
Cancer is the second leading cause of death in the United States (Centers for Disease Control and Prevention [CDC], 2020). Early screening reduces overall cancer risks through early detection (American Cancer Society, 2022). However, barriers persist and contribute to suboptimal cancer screening rates (Akinlotan et al., 2017). Exposure to adverse childhood experiences (ACEs) may be a barrier to cancer screening uptake. ACEs include exposure to physical, sexual, or emotional abuse or neglect, or household dysfunction (e.g., substance use disorder, mental health problems, domestic violence, parental separation, an incarcerated household member) (Felitti et al., 1998). According to the CDC (2021a), 5 of the 10 leading causes of death are associated with ACEs; in addition, women and individuals from underrepresented racial and ethnic groups are at greater risk for experiencing multiple ACEs. Documented links among ACEs, health behaviors, and subsequent health outcomes exist; adults exposed to ACEs may engage in increasingly risky behaviors that contribute to a greater likelihood of health issues across the life span (CDC, 2021a; Petruccelli et al., 2019; Ports et al., 2019).
Despite evidence linking ACEs to increased cancer risk (Holman et al., 2016), there is limited evidence of associations between ACEs and cancer screening behavior (Alcalá, Mitchell, & Keim-Malpass, 2017). This study used the Texas Behavioral Risk Factor Surveillance System (BRFSS) survey data to (a) describe demographic factors according to number of reported ACEs, (b) examine demographic differences between individuals who did and did not receive recommended cervical cancer screening, (c) examine whether individuals with exposure to ACEs were more likely not to have received cervical cancer screening than those without exposure, and (d) investigate whether the number and type of ACE exposures were predictive of having received screening.
Background
Cervical cancer is a significant health concern. The National Cancer Institute ([NCI], 2022) reported that 296,381 individuals in the United States had a cervical cancer diagnosis in 2020. In data from 2016 to 2020, 7.8 per 100,000 individuals reported new cervical cancer cases per year, and 2.2 per 100,000 individuals died per year (NCI, 2022; U.S. Cancer Statistics Working Group, 2023). These statistics additionally highlight that Hispanic women (10 per 100,000) and non-Hispanic American Indian and Alaska Native women (10.1 per 100,000) had the highest rates of cervical cancer and that Black, non-Hispanic women (3.4 deaths per 100,000) had the highest mortality (NCI, 2022).
Early screening can reduce cervical cancer risk by detecting the disease at an early stage. The U.S. Preventive Services Task Force ([USPSTF], 2018) recommends cervical cancer screening for individuals with a cervix aged 21–29 years every three years using cervical cytology (i.e., Papanicolaou [Pap] test) alone, and for individuals with a cervix aged 30–65 years every three years using cervical cytology alone or every five years using high-risk human papillomavirus (HPV) testing alone or in combination with cervical cytology (Curry et al., 2018). However, personal and structural obstacles may create barriers to receiving timely cervical cancer screenings (Akinlotan et al., 2017; Plourde et al., 2016), including a history of ACEs (Alcalá, Mitchell, & Keim-Malpass, 2017; Farley et al., 2002).
ACEs are powerful predictors of health behaviors in adults and potentially contribute to cancer screening behaviors (Holman et al., 2016; Hu et al., 2021). Physical and psychological abuse have been shown to be significant predictors of cancer risk in adulthood (Holman et al., 2016). ACEs can have severe negative effects on well-being, including psychological stress, use of inadequate coping mechanisms, and development of neglectful or risky health behaviors, which may contribute to chronic health conditions and even premature death (Ports et al., 2019). Numerous studies support the relationship between ACEs and various adult health-related outcomes, including cancer; the type and number of ACE exposures play a significant role in overall risk (Hu et al., 2021; Hughes et al., 2017; Petruccelli et al., 2019). Exposure to four or more ACEs is strongly linked to a higher risk of negative health outcomes including substance use, mental illness, risky sexual behavior, obesity, and disease (Felitti et al., 1998). Individuals with a history of ACEs are at significantly greater risk for cervical and other cancers (Holman et al., 2016; Modesitt et al., 2006; Van der Meer et al., 2012). A variety of ACE types, such as emotional, physical, or sexual abuse, are associated with risky behaviors that contribute to an increased risk of sexually transmitted infections, including HPV (Hillis et al., 2001). HPV is associated with 95% of all cervical cancers (Bosch et al., 2002), which underscores the need to examine the relationship between ACEs and cervical cancer risk (Farrow et al., 2018).
For individuals who have experienced ACEs, the effect of social determinants of health on cervical cancer prevention and control is particularly significant. It is widely recognized that social determinants of health, including where an individual lives, learns, works, and plays, as well as access to a healthy and safe environment, are important factors affecting risk and outcomes for cancer (CDC, 2021b). Socioeconomic status, education, and race and ethnicity, combined with exposure to ACEs, may be linked to cancer outcomes (Holman et al., 2016) via behaviors like cancer screening uptake. It is imperative to prioritize addressing these determinants when examining the associations between exposure to ACEs and cervical cancer screening behaviors.
Women who have experienced abuse may feel mental and physical discomfort during cervical cancer screenings (Coker et al., 2009). This has led to some women delaying or declining to receive this important preventive screening (Kohler et al., 2021). Adopting a trauma-informed approach to cervical cancer screening may be highly beneficial. The Substance Abuse and Mental Health Services Administration (2014) outlined the following six principles of trauma-informed care: (a) safety; (b) trustworthiness and transparency; (c) peer support; (d) collaboration and mutuality; (e) empowerment, voice, and choice; and (f) cultural, historic, and gender issues. Practicing trauma-informed care involves the following four key assumptions, referred to as the four Rs: (a) realizing that trauma is common; (b) recognizing signs and symptoms of trauma; (c) responding to trauma by integrating knowledge about trauma into policies, procedures, and practices; and (d) resisting retraumatizing patients (Substance Abuse and Mental Health Services Administration, 2015). Implementing a trauma-informed approach to caring for women who have had exposure to ACEs has the potential to positively affect cervical cancer screening behavior and uptake.
Statewide BRFSS surveys provide an opportunity to use data to identify potential public health issues that can be addressed through practice and policy. This study used data from the Texas BRFSS survey to evaluate the likelihood that individuals with exposure to ACEs received preventive cervical cancer screening. It also investigated whether exposure to ACEs can accurately predict cervical cancer screening uptake and analyzed associations among sociodemographic traits, ACEs, and cervical cancer screening. In this research, ACEs refer to negative occurrences experienced by an individual before the age of 18 years. Also, this article uses had the recommended screening or did not have the recommended screening instead of compliance and noncompliance to align with trauma-informed care best practices and to avoid the stigmatization and shaming associated with the latter terms (Kleinsinger, 2003).
Theoretical Framework
The perspective of ecologic theory (DeCandia & Guarino, 2015) can provide a deeper understanding of the relationships between ACEs and cervical cancer screening behaviors. This can provide insight into how individuals are affected by their surroundings, which is important in identifying the key contributors to childhood trauma. Understanding the dynamic relationship between risk and protective factors can lead to more effective interventions and support health-promoting behaviors (DeCandia & Guarino, 2015; Harvey, 2007). Trauma-informed care and interventions, delivered through an ecologic approach, recognize the effects of these factors on well-being and health. An ecologic framework emphasizes targeting individual, interpersonal, and community systems to address childhood trauma (DeCandia & Guarino, 2015; Harvey, 2007). Examining the effect of ACEs through this lens enables researchers to better understand the complex interactions among these factors and how they affect health behaviors.
Methods
Study Design
This study is a retrospective secondary data analysis using data from 11,042 adults who participated in the 2020 Texas BRFSS survey. The Texas A&M University Institutional Review Board determined that this secondary data analysis of publicly available deidentified data was not classified as human subjects research (IRB2022-0724). BRFSS surveys are administered annually in all 50 states, the District of Columbia, and certain territories working in conjunction with the CDC to formulate population-specific questions. The BRFSS surveys collect data from noninstitutionalized adults aged 18 years or older via randomly selected landline and cellular telephone surveys about a wide range of health-related information. Survey data represent a diverse population in terms of age, race, education, and socioeconomic status and are intended to be used in public health research and to develop and monitor programs that influence health policies (Mokdad et al., 2003).
Variables
Demographic data from the Texas BRFSS survey analyzed in this study included gender, age, race and ethnicity, marital status, education, and annual household income. In addition, number and type of ACEs and cervical cancer screening data from the Texas BRFSS survey were used.
ACEs: Every five years, Texas updates the ACEs measure used in the BRFSS survey, with the most recent update being in 2020. The 2020 Texas BRFSS survey ACEs measure consisted of 11 questions about ACEs before the age of 18 years. Four questions about household dysfunction assessed whether an individual lived with anyone who exhibited the following traits or behaviors: (a) was depressed, mentally ill, or suicidal; (b) misused alcohol; (c) used illegal street drugs or misused prescription medications; or (d) served time or was sentenced to serve time in a prison, jail, or correctional facility. Participants were asked one question regarding whether they had parents who were separated or divorced. Exposure to domestic violence was assessed with one question about how often parents or other adults in the home slapped, hit, kicked, punched, or beat up each other.
Participants were asked to reply how often they experienced sexual, physical, or emotional abuse before age 18 years with the following answer choices: never, once, more than once, do not know or not sure, and refuse to answer. Physical abuse was assessed using the following question: “Not including spanking (before age 18), how often did a parent or adult in your home ever hit, beat, kick, or physically hurt you in any way?” Emotional abuse was assessed using the following question: “How often did a parent or adult in your home ever swear at you, insult you, or put you down?” Sexual abuse was assessed with the following three questions: (a) “How often did anyone at least five years older than you or an adult ever touch you sexually?” (b) “How often did anyone at least five years older than you or an adult try to make you touch them sexually?” and (c) “How often did anyone at least five years older than you or an adult force you to have sex?” A “yes” response to questions about household dysfunction, parental separation/divorce, and exposure to domestic violence, and a response of “once” or “more than once” to questions about physical, emotional, and sexual abuse were each counted as one ACE. Total ACE scores ranged from 0 to 11.
Cervical cancer screening: USPSTF guidelines were used to indicate whether individuals had received cervical cancer screening at recommended intervals according to their age. The Texas BRFSS survey includes the following four questions about cervical cancer screening: (a) “Have you ever had a Pap test?” (b) “How long has it been since your last Pap test?” (c) “Have you ever had an HPV test?” and (d) “How long has it been since your last HPV test?” Individuals aged 21–29 years were coded as having had USPSTF-recommended cervical cancer screening if they reported having a Pap test within the past three years. Individuals aged 30–65 years were coded as having had USPSTF-recommended cervical cancer screening if they reported having either a Pap test in the past three years or an HPV test alone or in combination with a Pap test within the past five years.
Statistical Analyses
Demographic data were described using frequencies and weighted percentages. Chi-squares were used to examine differences in demographic variables by number of ACEs (zero, one to three, four to five, and six or more). Multiple logistic regression analysis was used to examine the likelihood of not having received recommended preventive cancer screening by number and type of ACEs (i.e., sexual, physical, or emotional abuse). Multiple logistic regression analysis is an appropriate method to examine relationships among risk factors and outcomes when there are multiple predictors (Nick & Campbell, 2007). The reference in all logistic regression models was the group of individuals who experienced zero ACEs.
Adjusted odds ratios considered gender, age, race and ethnicity, marital status, education level, and annual household income. When looking at each type of abuse individually, analyses also considered the other types of abuse. All statistical analyses were corrected to generate population estimates using sampling weights. The threshold for statistical significance was p = 0.05. Statistical analyses were performed using SAS, version 9.4.
Results
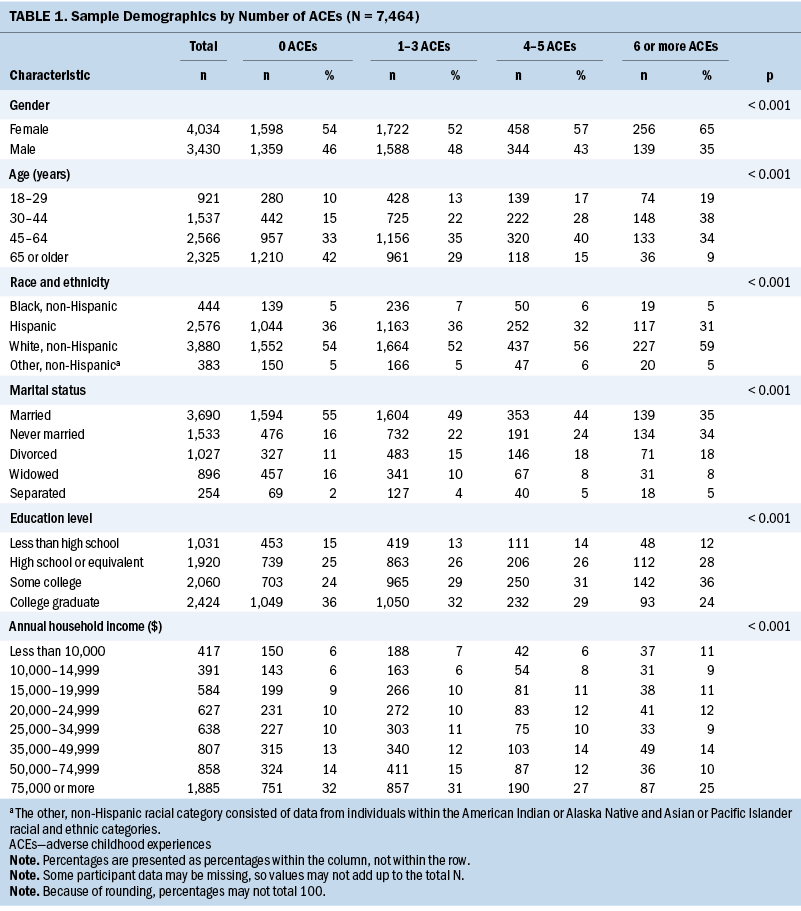
Demographic data by number of ACEs are shown in Table 1. ACEs data were available for 3,430 men and 4,034 women. Of these, 60% of men (n = 2,071) and 60% of women (n = 2,436) had experienced at least one ACE before age 18 years. Although more women had experienced zero ACEs than men (54% and 46%, respectively), a higher proportion of women than men had experienced four or more ACEs (n = 714 of 4,034 [18%] and n = 483 of 3,430, [14%], respectively). Greater proportions of individuals with more ACEs were in the 30–44 years and 45–64 years age brackets, had not graduated college, were never married, and were in lower income brackets at the time of the BRFSS survey. Higher percentages of White, non-Hispanic individuals were in the groups with zero ACEs and with six or more ACEs.
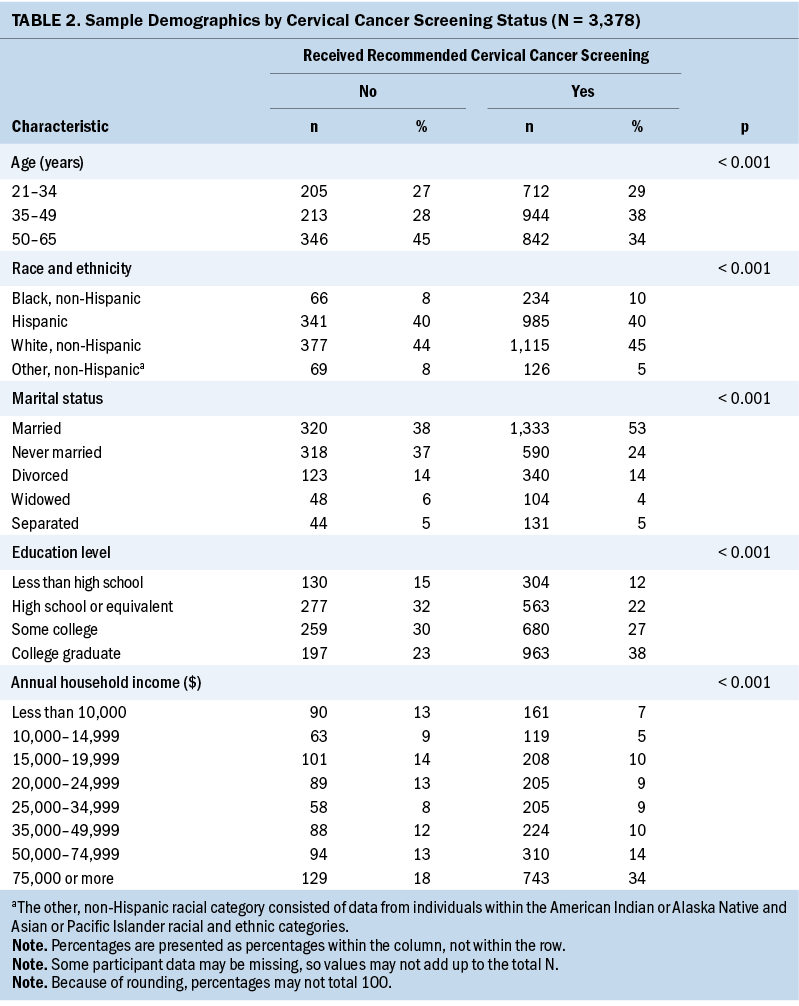
Data regarding cervical cancer screening behavior for 3,378 female individuals aged 21–65 years were available for analysis. Data were missing from 588 participants and thus not available for analysis. Of individuals with available data, 2,514 (74%) had received USPSTF-recommended cervical cancer screening and 864 (26%) had not. This consisted of 75% of White, non-Hispanic women (n = 1,115 of 1,492), 78% of Black, non-Hispanic women (n = 234 of 300), 74% of Hispanic women (n = 985 of 1,326), and 65% of women in the other, non-Hispanic racial category (consisting of individuals within the American Indian or Alaska Native and Asian or Pacific Islander racial and ethnic categories) (n = 126 of 195). Demographic data for women aged 21–65 years who had and did not have USPSTF-recommended cervical cancer screening are compared in Table 2. A higher proportion of women aged 35–49 years had received the recommended cervical cancer screening compared to older and younger women. The proportions of women who had received and not received recommended cervical cancer screening were similar among all racial groups except for the other, non-Hispanic group, which had a higher proportion of women who did have screening. In terms of education, a higher proportion of individuals who were college graduates had received cervical cancer screening compared with individuals with some college or less. Individuals in the highest income brackets (annual income of $50,000 or higher) were more likely to have received cervical cancer screening compared with those with annual incomes of less than $50,000.
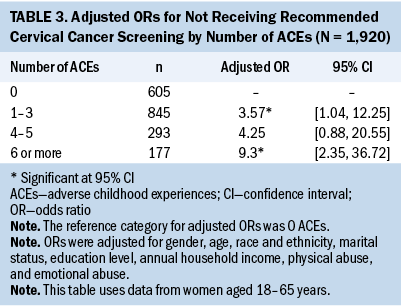
Multiple regression analyses identified a trend of increased likelihood of not having received recommended cervical cancer screening as number of ACEs increased (see Table 3). Individuals with a history of one to three ACEs and those with six or more ACEs were, respectively, 3.57 and 9.3 times more likely not to have had recommended cervical cancer screenings compared to those with zero ACEs. Although a history of four to five ACEs was associated with 4.25 times the likelihood of not having had the recommended screenings, this result was not statistically significant.
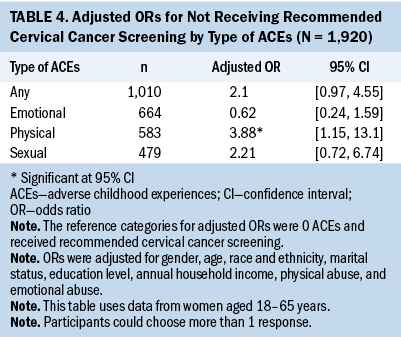
Regarding associations between ACE abuse types and likelihood of having had USPSTF-recommended cervical cancer screening, multiple logistic regression analysis results identified a 3.88 times the likelihood of not having had recommended screening for individuals with history of physical abuse (see Table 4). The odds of not having had screening were 2.1 times higher for individuals with any ACEs than for individuals with zero ACEs and approached significance (95% confidence interval [0.97, 4.55]).
Discussion
Data from this analysis indicate that a history of ACEs affects cervical cancer screening behavior in adult women. In examining demographics, 2020 Texas BRFSS survey data identified significant gender differences in relation to ACEs history. Although a higher proportion of women had zero ACEs compared with men, a higher proportion of women also had four or more ACEs. These findings are consistent with past ACEs studies (Petruccelli et al., 2019). This gender difference is critical to explore because prior research has found that associations between ACEs and cancer diagnosis are greater in women than in men (Alcalá, Tomiyama, & von Ehrenstein, 2017). In the current study, a lower proportion of individuals with six or more ACEs were college graduates, and a higher proportion were in lower income brackets. A higher proportion of individuals with six or more ACEs were also divorced or never married. These findings suggest that a history of ACEs may have long-term impacts on functioning that affect earning potential, although these associations may be complex and moderated by other factors (Giano et al., 2020; Merrick et al., 2018) not examined in the current analysis. This study’s findings of a higher percentage of individuals with four or more ACEs in the younger age brackets were consistent with studies that showed similar age-related patterns (Giano et al., 2020; Merrick et al., 2018).
Findings from this study are consistent with prior Texas Cancer Registry (2019) data showing similar trends comparing individuals who had and had not received recommended cervical cancer screenings. The rate of cervical cancer screening in this study’s sample was similar to the national average of 74%, and rates for Hispanic women and Black, non- Hispanic women in this study’s sample were slightly higher than the national averages of 70% and 75%, respectively (NCI, 2023). The relatively low screening rate for women in the other, non-Hispanic racial category in this study is concerning. Considering that Texas has a cervical cancer annual mortality rate higher than that in the United States overall (2.8 per 100,000 versus 2.2 per 100,000) (American Cancer Society, 2023), these findings highlight the importance of increasing the awareness of cervical cancer, risk factors, and screening recommendations and making cervical cancer screening more affordable and accessible in Texas. Targeted education and screening events for women aged 21–34 years and 50-65 years in underrepresented racial and ethnic groups and with lower educational attainment and income are potential ways to increase screening uptake.
In women with a history of ACEs, additional interventions may be necessary to increase cervical cancer screening uptake. This study indicated a greater likelihood of not having had recommended cervical cancer screening as number of ACEs increased. Although the adjusted odds ratio for the group with four to five ACEs of 4.25 was not significant, this might be because of the low number of women aged 21–65 years in the BRFSS survey sample with four to five ACEs (n = 293), compared to those with one to three ACEs (n = 845). Therefore, the study might have lacked the power to detect a significant difference in this group. These group cutoffs were purposeful based on prior studies that found significant differences in health-related outcomes in individuals with four or more ACEs (Hughes et al., 2017) and increased risk of premature death for individuals with six or more ACEs (Brown et al., 2009). Consistent with this study’s findings, a study involving a large cohort in the Southern Community Cohort Study found that women with three or more ACEs were less likely to have received recommended cervical cancer screening (Mouton et al., 2016).
When examining associations with ACE abuse types (sexual, physical, and emotional), this study found that only exposure to physical abuse ACEs was associated with greater likelihood not to have received recommended cervical cancer screening. Findings that exposure to sexual abuse ACEs was not associated with a greater likelihood of not having received recommended cervical cancer screening were unexpected, considering the invasive nature of cervical cancer screening and some prior studies that identified this association. Prior studies using state-level BRFSS survey data found varied associations between ACEs and cancer screening behavior. A study using 2014 Kansas BRFSS survey data (Alcalá, Mitchell, & Keim- Malpass, 2018) found that childhood physical and emotional abuse were associated with significantly reduced odds of following age- and physiology-related recommendations for cervical cancer screening; consistent with the findings from the current study, sexual abuse was not associated with reduced odds of cervical cancer screening. However, the same research group found that only sexual abuse was associated with decreased odds of having received cervical cancer screening using data from the 2009 Tennessee BRFSS survey (Alcalá, Mitchell, & Keim- Malpass, 2017). A study that did not measure ACEs but asked about history of childhood sexual abuse using a smaller sample from a large health maintenance organization found that sexual abuse was associated with a lower likelihood for women to have had recommended cervical cancer screening (Farley et al., 2002). Data involving larger national samples could provide additional support for identifying associations between ACEs and cervical cancer screening behavior.
Although not statistically significant, the finding that individuals with a history of emotional ACEs were more likely to have received recommended cervical cancer screening was unexpected. This finding highlights the importance of examining the differential effects of types of child abuse on adult cancer screening behavior. Health anxiety, for example, is a potential mediator that could be explored because childhood emotional abuse has been associated with adult anxiety (Taillieu et al., 2016). A systematic review by Horenstein and Heimberg (2020) found conflicting effects of anxiety and health anxiety on healthcare use, with most studies indicating that increased anxiety and health anxiety were associated with greater healthcare use. This research also highlighted preliminary but limited evidence that, in some cases, anxiety can be associated with delayed, irregular, or inconsistent use of healthcare services (Horenstein & Heimberg, 2020). More research involving individuals with a history of exposure to ACEs is needed to identify potential mediators, such as health anxiety, of the relationships among types of child abuse and cervical cancer screening uptake, which could suggest ways to overcome barriers to screening and help in designing trauma-informed interventions.
Prior studies examining the associations between ACEs and cancer screening behavior examined ACE exposure as bivariate (i.e., exposed or not exposed) or by categories of number of ACEs, with four or more ACEs as the maximum. In this study, categories of number of ACEs were used; six or more ACEs was included as a category. Examining data in this manner revealed a formerly unidentified pattern related to cervical cancer screening behavior. The significantly increased likelihood of women with six or more ACEs not having received recommended cervical cancer screenings is concerning, considering the association between a history of child abuse and a higher risk of cervical cancer (Coker et al., 2009). This association may be mediated by increased levels of smoking, perceived stress, risky sexual behavior, and lower screening rates in individuals with a history of child physical or sexual abuse (Hindin et al., 2019).
Cervical cancer mortality is reduced by early detection through routine cervical cancer screening (Curry et al., 2018). Methods of cervical cancer screening include cervical cytology, or a Pap test, which is performed in a lithotomy position with the insertion of a lighted vaginal speculum for visualization of the cervix and collection of cervical cells using a brush rotated at 360 degrees. Some women report hesitancy to receive this screening because of discomfort with the intrusiveness of the procedure (Kohler et al., 2021). Women who have experienced sexual violence may experience feelings of revictimization. Mouton et al. (2016) also reported that a greater number of ACEs was associated with decreased cervical cancer screening rates. A qualitative study found that women with a history of child sexual abuse reported barriers to cervical cancer screening, including low self-worth, embarrassment, self-consciousness, concern for their genital appearance, shame, and guilt (Cadman et al., 2012).
A trauma-informed approach to cervical cancer screening using the four Rs (realizing, recognizing, responding, and resisting) may help to improve screening behavior in individuals with a history of child abuse (Substance Abuse and Mental Health Services Administration, 2015). Data from this study support the assumption that trauma is common, because almost two-thirds of men and more than half of women had experienced at least one ACE, and women were more likely to experience four or more ACEs (realizing). Not adhering to cervical cancer screening recommendations might be a sign and symptom of trauma (recognizing). Healthcare providers should consider implementing policies, procedures, and practices to mitigate barriers for patients who are at higher risk for not receiving cervical cancer screening (responding). Implementing universal trauma-informed care practices, including for cervical cancer screening, may increase patient comfort and reduce the risk of additional trauma (resisting) (Owens et al., 2022). This includes training all staff in creating a safe environment from the time a patient checks in until they leave (Purtle, 2020).
Strengths and Limitations
These findings add additional context to the evaluation of timely cancer screening. They emphasize the importance of considering the type, number, and frequency of ACEs when examining associations between ACE history and adult cancer screening behavior. The primary limitation of this analysis is that data were provided by individuals via telephone survey, which may contribute to recall bias and social desirability bias in survey responses. Participants may not accurately remember or may not want to report whether they received timely cancer screening. The age at which ACEs occurred was not collected in the Texas BRFSS survey, which might differentially affect health behaviors (Harada et al., 2021). This study also did not control for insurance status or mental health diagnosis, both of which are associated with a history of child abuse (Alcalá, Valdez-Dadia, & von Ehrenstein, 2018; Petruccelli et al., 2019) and differences in likelihood of cervical cancer screening (Alcalá, Mitchell, & Keim-Malpass, 2017, 2018; Farley et al., 2002). Some data collection from the 2020 Texas BRFSS survey might have occurred during the COVID-19 pandemic social distancing regulations, which may have inhibited access to cervical cancer screening. Nevertheless, these access restrictions would have applied to all individuals. Despite these limitations, this study identified differences among individuals by number and type of ACEs. Texas is a non–Medicaid-expansion state and may have unique demographic, social, and political factors that potentially affect cancer screening behaviors, which makes generalization of these findings to other states more difficult.
Implications for Practice
About 95% of all cervical cancer is caused by 15 subtypes of HPV infections (Bosch et al., 2002). Pap testing can include HPV testing, known as a cotest, for early detection and risk stratification. No treatment for HPV currently exists, but vaccination has demonstrated as much as 86% effectiveness in preventing HPV infection (CDC, 2022). However, the median age at which childhood sexual abuse occurs is reported to be 9 years (Putnam, 2003), which is younger than the recommended age of 11–12 years for HPV vaccination, although the CDC states that vaccination may begin at age 9 years (CDC, 2021c). Cancer prevention should take precedence in coordination with cervical cancer screening. Lowering cancer risk through age-appropriate vaccination may mitigate anxiety associated with the pelvic examination and Pap test for survivors of child abuse.
Healthcare providers need to be aware of the potential impacts of child abuse on cervical cancer screening behavior. Even with universal trauma-informed care practices, additional responses may be necessary to support some patients in receiving timely cervical cancer screening. Although more than 80% of obstetricians and gynecologists strongly agreed that past child abuse is relevant to the care they provided, more than 70% reported that time was a significant barrier to screening patients, and fewer than one-third reported screening most of the time or all the time (Farrow et al., 2018). Therefore, targeting screening recommendations to patients who frequently delay or miss recommended screenings might be more feasible, in addition to applying universal trauma-informed care practices. Screening for child abuse history is now a reimbursable activity (Centers for Medicare and Medicaid Services, 2019), which can eliminate one identified barrier. Fewer than half of obstetricians and gynecologists reported having ever received training in screening for child abuse history, and many stated that they did not feel comfortable doing so (Farrow et al., 2018). Regular training might be beneficial in increasing healthcare provider comfort with screening for a history of child abuse.
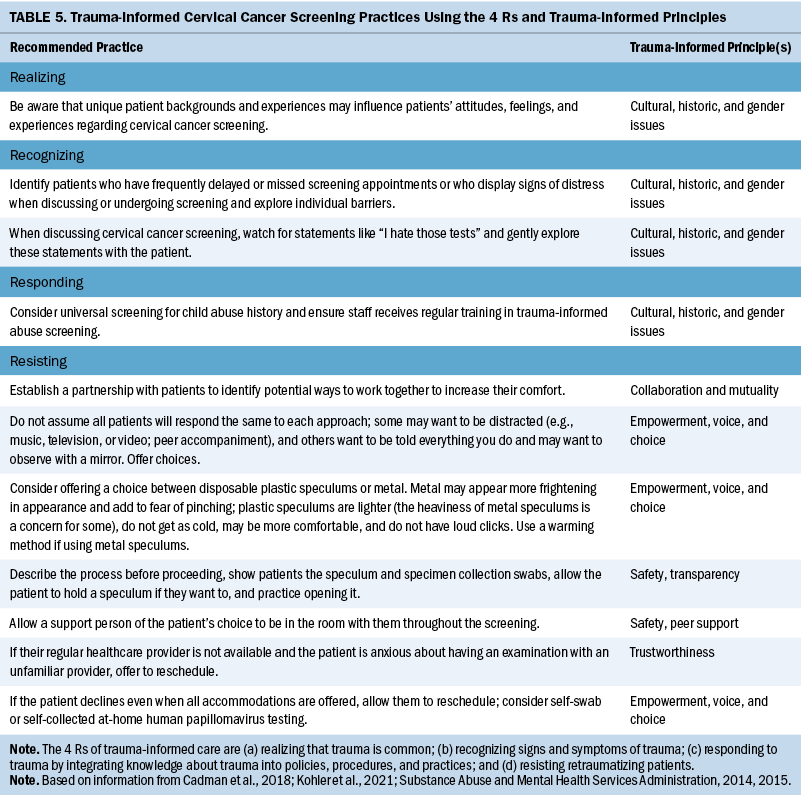
To prevent retraumatization of patients with a history of ACEs receiving cervical cancer screening, providers should follow the six principles of trauma-informed care. These include creating a safe space, having a transparent discussion of barriers to cervical cancer screening, encouraging peer support during the consultation, taking a posture of mutual problem-solving and collaboration, listening to and empowering patients by presenting choices, and considering unique historic, cultural, and gender-related factors that may affect cancer screening behavior. Table 5 provides additional recommendations for trauma-informed cervical cancer screening practices.
Conclusion
Data from BRFSS surveys can be used to identify trends in cervical cancer screening and factors associated with screening behavior. Links among exposure to ACEs, increased risk of poor health outcomes, and cancer screening and prevention behaviors have previously been established. In this study, a higher number of ACEs and a history of physical child abuse were associated with increased odds that women had not received recommended cervical cancer screening. Additional precautions and considerations regarding cervical cancer screening must be implemented for individuals with a history of child abuse. A trauma-informed care approach can be used to increase cervical cancer screening uptake rates in individuals exposed to ACEs.
About the Authors
Arica A. Brandford, PhD, JD, RN, is an assistant professor in the School of Nursing at Texas A&M University in Bryan; Elizabeth Nancy Williams, MPH, is a student research assistant and Gang Han, PhD, is a professor, both in the School of Public Health at Texas A&M University in College Station; Cynthia Weston, DNP, APRN, FNP-BC, CHSE, is dean of the College of Nursing in the Health Science Center at the University of North Texas in Fort Worth; and Nancy R. Downing, PhD, RN, SANE-A, SANE-P, FAAN, is an associate professor in the Texas A&M Health Center of Excellence in Forensic Nursing in the School of Nursing at Texas A&M University in Bryan. No financial relationships to disclose. Brandford, Williams, Weston, and Downing contributed to the conceptualization and design and the manuscript preparation. Brandford, Williams, Han, and Downing completed the data collection and provided statistical support. All authors provided the analysis. Brandford can be reached at arica.brandford@tamu.edu, with copy to ONFEditor@ons.org. (Submitted October 2022. Accepted June 29, 2023.)
References
Akinlotan, M., Bolin, J.N., Helduser, J., Ojinnaka, C., Lichorad, A., & McClellan, D. (2017). Cervical cancer screening barriers and risk factor knowledge among uninsured women. Journal of Community Health, 42(4), 770–778. https://doi.org/10.1007/s10900-017-0316-9
Alcalá, H.E., Mitchell, E.M., & Keim-Malpass, J. (2017). Adverse childhood experiences and cervical cancer screening. Journal of Women’s Health, 26(1), 58–63. https://doi.org/10.1089/jwh.2016.5823
Alcalá, H.E., Mitchell, E.M., & Keim-Malpass, J. (2018). Heterogeneous impacts: Adverse childhood experiences and cancer screening. Cancer Causes and Control, 29(3), 343–351. https://doi.org/10.1007/s10552-018-1007-2
Alcalá, H.E., Tomiyama, A.J., & von Ehrenstein, O.S. (2017). Gender differences in the association between adverse childhood experiences and cancer. Women’s Health Issues, 27(6), 625–631. https://doi.org/10.1016/j.whi.2017.06.002
Alcalá, H.E., Valdez-Dadia, A., & von Ehrenstein, O.S. (2018). Adverse childhood experiences and access and utilization of health care. Journal of Public Health, 40(4), 684–692. https://doi.org/10.1093/pubmed/fdx155
American Cancer Society. (2022). Cancer risk and prevention. https://www.cancer.org/cancer/risk-prevention.html
American Cancer Society. (2023). Cervix: At a glance. https://cancerstatisticscenter.cancer.org/#!/cancer-site/Cervix
Bosch, F.X., Lorincz, A., Muñoz, N., Meijer, C.J., & Shah, K.V. (2002). The causal relation between human papillomavirus and cervical cancer. Journal of Clinical Pathology, 55(4), 244–265.
Brown, D.W., Anda, R.F., Tiemeier, H., Felitti, V.J., Edwards, V.J., Croft, J.B., & Giles, W.H. (2009). Adverse childhood experiences and the risk of premature mortality. American Journal of Preventive Medicine, 37(5), 389–396. https://doi.org/10.1016/j.amepre.2009.06.021
Cadman, L., Waller, J., Ashdown-Barr, L., & Szarewski, A. (2012). Barriers to cervical screening in women who have experienced sexual abuse: An exploratory study. Journal of Family Planning and Reproductive Health Care, 38(4), 214–220. https://doi.org/10.1136/jfprhc-2012-100378
Centers for Disease Control and Prevention. (2020). An update on cancer deaths in the United States. https://www.cdc.gov/cancer/dcpc/research/update-on-cancer-deaths/index…
Centers for Disease Control and Prevention. (2021a). Adverse childhood experiences (ACEs): Preventing early trauma to improve adult health. https://www.cdc.gov/vitalsigns/aces/index.html
Centers for Disease Control and Prevention. (2021b). Equity in cancer prevention and control. https://www.cdc.gov/cancer/health-equity/equity.htm
Centers for Disease Control and Prevention. (2021c). HPV vaccination recommendations. https://www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html
Centers for Disease Control and Prevention. (2022). Genital HPV infection—Basic fact sheet. https://www.cdc.gov/std/hpv/stdfact-hpv.htm
Centers for Medicare and Medicaid Services. (2019). ICD-10-CM/PCS MS-DRG v37.0 definitions manual. https://www.cms.gov/icd10m/version37-fullcode-cms/fullcode_cms/P0960.ht…
Coker, A.L., Hopenhayn, C., DeSimone, C.P., Bush, H.M., & Crofford, L. (2009). Violence against women raises risk of cervical cancer. Journal of Women’s Health, 18(8), 1179–1185. https://doi.org/10.1089/jwh.2008.1048
Curry, S.J., Krist, A.H., Owens, D.K., Barry, M.J., Caughey, A.B., Davidson, K.W., . . . Wong, J.B. (2018). Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA, 320(7), 674–686. https://doi.org/10.1001/jama.2018.10897
DeCandia, C., & Guarino, K. (2015). Trauma-informed care: An ecological response. Journal of Child and Youth Care Work, 25, 7–32. https://doi.org/10.5195/jcycw.2015.69
Farley, M., Golding, J.M., & Minkoff, J.R. (2002). Is a history of trauma associated with a reduced likelihood of cervical cancer screening? Journal of Family Practice, 51(10), 827–831.
Farrow, V.A., Bosch, J., Crawford, J.N., Snead, C., & Schulkin, J. (2018). Screening for history of childhood abuse: Beliefs, practice patterns, and barriers among obstetrician-gynecologists. Women’s Health Issues, 28(6), 559–568. https://doi.org/10.1016/j.whi.2018.09.001
Felitti, V.J., Anda, R.F., Nordenberg, D., Williamson, D.F., Spitz, A.M., Edwards, V., . . . Marks, J.S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258. https://doi.org/10.1016/s0749-3797(98)00017-8
Giano, Z., Wheeler, D.L., & Hubach, R.D. (2020). The frequencies and disparities of adverse childhood experiences in the U.S. BMC Public Health, 20, 1327. https://doi.org/10.1186/s12889-020-09411-z
Harada, M., Guerrero, A., Iyer, S., Slusser, W., Szilagyi, M., & Koolwijk, I. (2021). The relationship between adverse childhood experiences and weight-related health behaviors in a national sample of children. Academic Pediatrics, 21(8), 1372–1379. https://doi.org/10.1016/j.acap.2021.05.024
Harvey, M.R. (2007). Towards an ecological understanding of resilience in trauma survivors: Implications for theory, research, and practice. Journal of Aggression, Maltreatment and Trauma, 14(1–2), 9–32. https://doi.org/10.1300/J146v14n01_02
Hillis, S.D., Anda, R.F., Felitti, V.J., & Marchbanks, P.A. (2001). Adverse childhood experiences and sexual risk behaviors in women: A retrospective cohort study. Family Planning Perspectives, 33(5), 206–211. https://doi.org/10.2307/2673783
Hindin, P., Btoush, R., & Carmody, D.P. (2019). History of childhood abuse and risk for cervical cancer among women in low-income areas. Journal of Women’s Health, 28(1), 23–29. https://doi.org/10.1089/jwh.2018.6926
Holman, D.M., Ports, K.A., Buchanan, N.D., Hawkins, N.A., Merrick, M.T., Metzler, M., & Trivers, K.F. (2016). The association between adverse childhood experiences and risk of cancer in adulthood: A systematic review of the literature. Pediatrics, 138(Suppl. 1), S81–S91. https://doi.org/10.1542/peds.2015-4268L
Horenstein, A., & Heimberg, R.G. (2020). Anxiety disorders and healthcare utilization: A systematic review. Clinical Psychology Review, 81, 101894. https://doi.org/10.1016/j.cpr.2020.101894
Hu, Z., Kaminga, A.C., Yang, J., Liu, J., & Xu, H. (2021). Adverse childhood experiences and risk of cancer during adulthood: A systematic review and meta-analysis. Child Abuse and Neglect, 117, 105088. https://doi.org/10.1016/j.chiabu.2021.105088
Hughes, K., Bellis, M.A., Hardcastle, K.A., Sethi, D., Butchart, A., Mikton, C., . . . Dunne, M.P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health, 2(8), e356–e366. https://doi.org/10.1016/S2468-2667(17)30118-4
Kleinsinger, F. (2003). Understanding noncompliant behavior: Definitions and causes. Permanente Journal, 7(4), 18–21.
Kohler, R.E., Roncarati, J.S., Aguiar, A., Chatterjee, P., Gaeta, J., Viswanath, K., & Henry, C. (2021). Trauma and cervical cancer screening among women experiencing homelessness: A call for trauma-informed care. Women’s Health, 17, 17455065211029238. https://doi.org/10.1177/17455065211029238
Merrick, M.T., Ford, D.C., Ports, K.A., & Guinn, A.S. (2018). Prevalence of adverse childhood experiences from the 2011–2014 Behavioral Risk Factor Surveillance System in 23 states. JAMA Pediatrics, 172(11), 1038–1044. https://doi.org/10.1001/jamapediatrics.2018.2537
Modesitt, S.C., Gambrell, A.C., Cottrill, H.M., Hays, L.R., Walker, R., Shelton, B.J., . . . Ferguson, J.E., II. (2006). Adverse impact of a history of violence for women with breast, cervical, endometrial, or ovarian cancer. Obstetrics and Gynecology, 107(6), 1330–1336. https://doi.org/10.1097/01.AOG.0000217694.18062.91
Mokdad, A.H., Stroup, D.F., & Giles, W.H. (2003). Public health surveillance for behavioral risk factors in a changing environment: Recommendations from the Behavioral Risk Factor Surveillance Team. MMWR Recommendations and Reports, 52(RR09), 1–12. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5209a1.htm
Mouton, C.P., Hargreaves, M.K., Liu, J., Fadeyi, S., & Blot, W.J. (2016). Adult cancer risk behaviors associated with adverse childhood experiences in a low income population in the southeastern United States. Journal of Health Care for the Poor and Underserved, 27(1), 68–83. https://doi.org/10.1353/hpu.2016.0027
National Cancer Institute. (2022). Cancer stat facts: Cervical cancer. https://seer.cancer.gov/statfacts/html/cervix.html
National Cancer Institute. (2023). Cervical cancer screening. https://progressreport.cancer.gov/detection/cervical_cancer
Nick, T.G., & Campbell, K.M. (2007). Logistic regression. In W.T. Ambrosius (Ed.), Topics in biostatistics (pp. 273–301). Humana Press. https://doi.org/10.1007/978-1-59745-530-5_14
Owens, L., Terrell, S., Low, L.K., Loder, C., Rhizal, D., Scheiman, L., & Seng, J. (2022). Universal precautions: The case for consistently trauma-informed reproductive healthcare. American Journal of Obstetrics and Gynecology, 226(5), 671–677. https://doi.org/10.1016/j.ajog.2021.08.012
Petruccelli, K., Davis, J., & Berman, T. (2019). Adverse childhood experiences and associated health outcomes: A systematic review and meta-analysis. Child Abuse and Neglect, 97, 104127. https://doi.org/10.1016/j.chiabu.2019.104127
Plourde, N., Brown, H.K., Vigod, S., & Cobigo, V. (2016). Contextual factors associated with uptake of breast and cervical cancer screening: A systematic review of the literature. Women and Health, 56(8), 906–925. https://doi.org/10.1080/03630242.2016.1145169
Ports, K.A., Holman, D.M., Guinn, A.S., Pampati, S., Dyer, K.E., Merrick, M.T., . . . Metzler, M. (2019). Adverse childhood experiences and the presence of cancer risk factors in adulthood: A scoping review of the literature from 2005 to 2015. Journal of Pediatric Nursing, 44, 81–96. https://doi.org/10.1016/j.pedn.2018.10.009
Purtle, J. (2020). Systematic review of evaluations of trauma-informed organizational interventions that include staff trainings. Trauma, Violence, and Abuse, 21(4), 725–740. https://doi.org/10.1177/1524838018791304
Putnam, F.W. (2003). Ten-year research update review: Child sexual abuse. Journal of the American Academy of Child and Adolescent Psychiatry, 42(3), 269–278. https://doi.org/10.1097/00004583-200303000-00006
Substance Abuse and Mental Health Services Administration. (2014). SAMHSA’s concept of trauma and guidance for a trauma-informed approach. https://ncsacw.acf.hhs.gov/userfiles/files/SAMHSA_Trauma.pdf
Substance Abuse and Mental Health Services Administration. (2015). TIP 57: Trauma-informed care in behavioral health services. https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4816.pdf
Taillieu, T.L., Brownridge, D.A., Sareen, J., & Afifi, T.O. (2016). Childhood emotional maltreatment and mental disorders: Results from a nationally representative adult sample from the United States. Child Abuse and Neglect, 59, 1–12. https://doi.org/10.1016/j.chiabu.2016.07.005
Texas Cancer Registry. (2019). Cervical cancer in Texas. Texas Department of State Health Services. https://www.dshs.texas.gov/sites/default/files/tcr/data/screening/Cervi…
U.S. Cancer Statistics Working Group. (2023). U.S. cancer statistics data visualizations tool [based on 2021 submission data (1999–2019)]. https://www.cdc.gov/cancer/dataviz
U.S. Preventive Services Task Force. (2018). Cervical cancer: Screening. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/cer…
Van der Meer, L.B., van Duijn, E., Wolterbeek, R., & Tibben, A. (2012). Adverse childhood experiences of persons at risk for Huntington’s disease or BRCA1/2 hereditary breast/ovarian cancer. Clinical Genetics, 81(1), 18–23. https://doi.org/10.1111/j.1399-0004.2011.01778.x


